Abstract
Background:
Corneal collagen cross-linking with riboflavin, also known as collagen cross-linking (CXL), involves the application of riboflavin solution to the eye that is activated by illumination with ultraviolet A (UVA) light. We survey here the topographic corneal changes one year after CXL in patients with corneal keratoconus.
Materials and Methods:
This prospective randomized clinical trial study comprised 66 patients with progression of keratoconus during one year who were enrolled at Feiz University Referral Eye Center in Isfahan. Before and after the operation, patients were examined with slit lamp and funduscopic examinations and measurement of uncorrected visual acuity (UCVA), and best spectacle-corrected visual acuity (BSCVA) was done with a logarithm of minimal angle of resolution (logMAR) scale. Corneal topographic and pachymetry values were derived from Orbscan II. The paired t-test test was used for statistical analyses with SPSS software version 20 (SPSS Inc., Chicago, IL, USA).
Results:
All 66 patients completed postoperative follow-up at 12 months. The mean age of the patients was 22.4 ± 5.4 years (range: 18-29 years). Thirty-six (54.55%) subjects were men and 30 (45.45%) were women. The mean preoperative sphere was −2.66 ± 2.14 diopter (D), the mean cylinder was −3.97 ± 2.29, and the mean spherical equivalent (SE) was −4.64 ± 2.56. Postoperatively, the mean sphere was −2.22 ± 2.57 D, the mean cylinder was −3.60 ± 2.40 D, and SE was −4.02 ± 2.93 D (P = 0.037). SE also demonstrated a mean difference of 0.62 ± 0.37 D significantly (P = 0.006). The mean diameter of preoperative posterior best-fit sphere (BFS) was 6.33 ± 0.35mm (range: 5.51-7.73 mm) before operation, and it improved to 6.28 ± 0.34mm (range: 4.36-6.13 mm) after operation; the difference was significant (P = 0.039).
Conclusion:
Our study showed a significant improvement in topographic corneal changes and refractive results in patients with corneal ectasia after CXL.
Keywords: Collagen cross-linking, progressive keratoconus, ultraviolet irradiation
INTRODUCTION
Keratoconus is an eye disorder that causes the corneal tissue to become abnormally thin and the central area to protrude in a cone shape, distorting the vision. It is typically diagnosed in the adolescent years of the patient and attains its most severe state between the ages of 20 and 40. If afflicting both eyes, the deterioration in vision can affect the ability of the patient to drive a car or read normal print.[1] The incidence of keratoconus is reported to be 1 in 2,000 in the general population;[2] reported rates vary with the criteria used for diagnosis. Although usually a progressive disease, recent data suggests that it stabilizes after time in most patients, and that treatment with rigid contact lenses is successful for many; 10 to 20% of keratoconus patients in the United States eventually receive corneal transplants to restore their vision.[3]
Corneal cross-linking (CXL) treatment of keratoconus was first introduced by Wollensak et al. in 2003.[4] Corneal collagen cross-linking with riboflavin, also known as CXL, CCR, CCL, and KXL, involves a one-time application of riboflavin solution to the eye that is activated by illumination with ultraviolet A (UVA) light for approximately 30 minutes.[5,6] The riboflavin causes new bonds to form across adjacent collagen strands in the stromal layer of the cornea, which recovers and preserves some of the mechanical strength of the cornea. The corneal epithelial layer is generally removed to increase penetration of the riboflavin into the stroma.[7] CXL increases the resistance to the digestion of pepsin by enhancing corneal anticollagenase activity, and induces a thicker diameter of collagen fiber.[8] Confocal microscopy studies have also shown apoptosis of keratocytes in the anterior and intermediate stroma followed by a gradual keratocyte repopulation.[9]
We performed this study because of the small number of studies on the treatment of Iranian patients with CXL method and the unknown impact of this procedure on the cornea of Iranian patients with keratoconus.
The aim of this study was to evaluate topographic corneal changes one year after CXL in patients with corneal keratoconus at Feiz Hospital of Isfahan, 12 months after treatment.
MATERIALS AND METHODS
Randomized clinical trial and study criteria
In this prospective study, 66 patients with progression of keratoconus during one year were enrolled at Feiz University Referral Eye Center in Isfahan from December 2010 to December 2011. Inclusion criteria in this study were corneal ectasia and corneal thickness of ≥400 μm at the thinnest point.[10,11]
All procedures were performed by a single surgeon. Informed consent was obtained from all subjects.
Exclusion criteria included pregnancy, a history of herpetic keratitis, severe eye dry, concurrent corneal infections, concomitant autoimmune diseases, and any previous corneal surgery such as corneal ring insertion. Also, patients with diabetes mellitus, patients with poor compliance, and patients with corneal transplantation were excluded.
Preoperative examinations
Before the operation, patients were examined with slit lamp and funduscopic examinations, and measurement of uncorrected visual acuity (UCVA) and best spectacle-corrected visual acuity (BSCVA) with a logarithm of minimal angle of resolution (logMAR) scale was performed. Corneal topographic and pachymetry values were derived from Orbscan II (Bausch and Lomb, Rochester, NY). Keratometry values reported are the simulated keratometric values obtained with Orbscan II.
Surgical procedure
After topical anesthesia (tetracaine 0.5% ophthalmic drops, Darou Pakhsh Phama Co., Iran), with a surgical blade (≠15) under sterile conditions, mechanical epithelium removal of the central 8 mm area of the cornea was performed. Riboflavin 0.1% (Medio-Haus Medizinprodukte GmbH, Neudorf, Germany) solution was instilled in the eye every three minutes for 30 minutes. Then, examination under slit lamp was performed for ensuring penetration of riboflavin into the cornea.
After this procedure, cornea UVA irradiation was performed with a UV-X device (IROC Innocross, Zürich, Switzerland). The device was set at a safe working distance of 5 cm from the corneal surface with a medium-sized UV ray aperture at a wavelength of 370 nm. Irradiation was performed for 30 minutes and along with this procedure, riboflavin 0.1% solution was instilled every three minutes.
After treatment, the patient received topical ciprofloxacin 0.30% and betamethasone 0.1% with an extended-wear night and day bandage contact lens for seven days.
Postoperative management
All patients were given topical ciprofloxacin 0.30% and betamethasone (four times a day) for seven days. On the first and seventh day after the procedure, the patients were examined for survey epithelial healing and absence of postoperative infection. Then 12 months later, postoperative examinations were carried out in the same way as the preoperative examinations: Slit lamp examination, visual acuity, refraction, and corneal topography with Orbscan II.
Statistical analysis
The paired sample t-test was used for statistical analyses with SPSS software version 20 (SPSS Inc., Chicago, IL, USA). Results are presented as mean ± standard deviation or error where applicable. The threshold for statistical significance was set at a P value less than 0.05.
RESULTS
All 66 patients completed a postoperative follow-up at 12 months. The mean age of the patients was 22.4 ± 5.4 years (range: 18-29 years). Thirty-six (54.55%) subjects were men and 30 (45.45%) were women.
Change in UCVA 12 months after CXL with riboflavin for progressive keratoconus was measured. Patients were compared before operation and after operation [Table 1].
Table 1.
Comparison of pre-op and post-op BSCVA
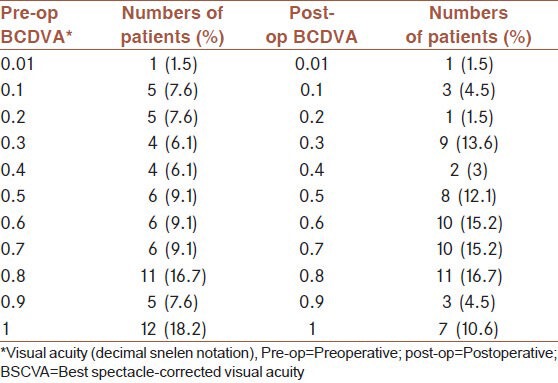
Subject reports of deteriorating best corrected visual acuity (BCVA or BSCVA) shows an increase in maximum keratometry (K) of 1.00 diopter (D) in one year.
The results regarding refractive changes preoperative and postoperative corneal cross-linking (CXL) are presented in Table 2.
Table 2.
Comparison of refractive values before and after CXL
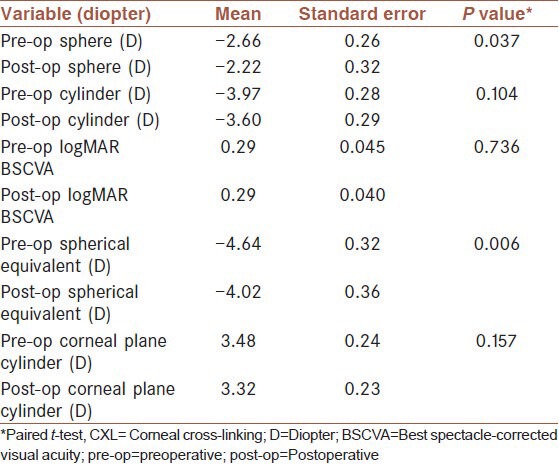
The mean UCVA was not significantly improved 12 months after surgery [0.29 ± 0.36 logMAR to 0.29 ± 0.32 logMAR (P = 0.736)] [Table 3].
Table 3.
Comparison of topographic values before and after CXL
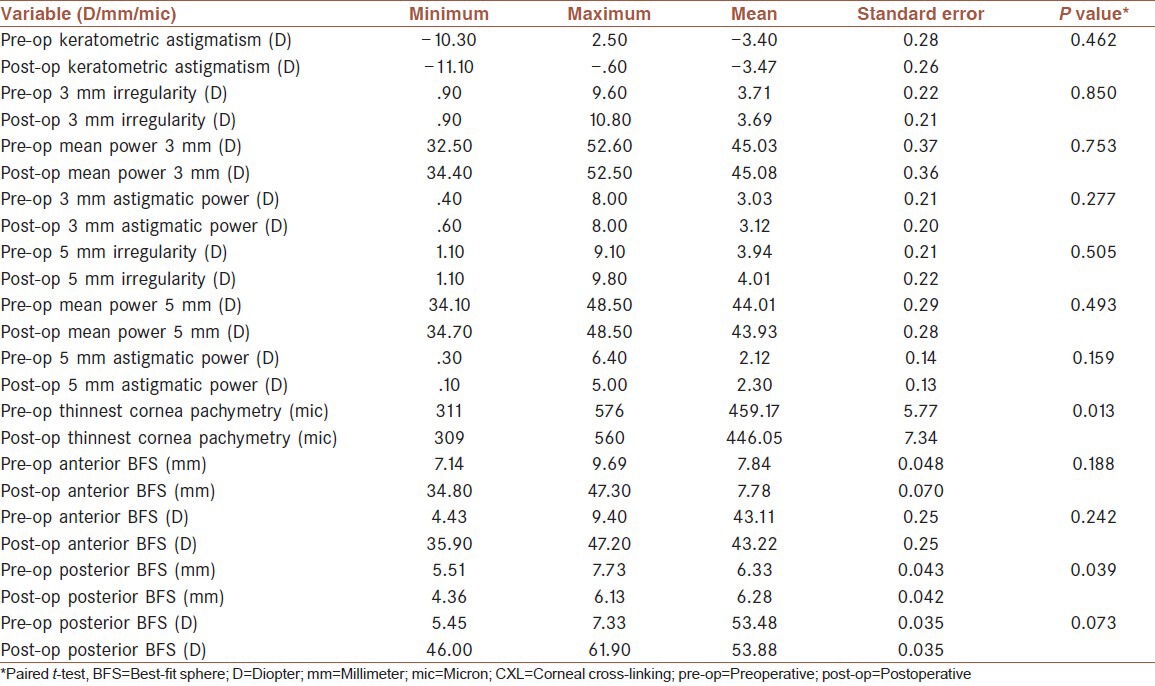
The mean of preoperative posterior BFS was 6.33 ± 0.35 mm (range: 5.51 to 7.73 mm) before operation and it improved to 6.28 ± 0.34 mm (range: 4.36 to 6.13 mm) after operation; the difference was significant (P = 0.039) but the difference between the mean of preoperative anterior BFS (7.84 ± 0.39 mm) and postoperative anterior BFS (7.78 ± 0.56 mm) was not significant (P = 0.188)
Except the decreasing of the thickness of cornea, all the other results were status quo or improved, indicating that the CXL may be a good method for arresting the progression of keratoconus.
DISCUSSION
The CXL technique, developed in recent years, is under study for the treatment of several eye disorders. In keratoconus patients, drops containing riboflavin, a B-complex vitamin, are applied to the cornea which is then exposed to UVA light; this stimulates collagen fibers to connect to one another or cross-link. Collagen is the primary protein constituent of the connective tissues of the body. The procedure helps restore appropriate curvature and structure to the cornea, and makes it possible for most patients, who need them, to wear rigid contact lenses again.[12]
CXL is a new treatment for patients with keratoconus;[4] so, response to treatment maybe different among different racial and ethnic groups. In this research, we survey topographic corneal changes one year after CXL in Iranian patients with corneal keratoconus in Isfahan.
Kohlhaas and colleagues, in an animal study, showed a significant increase in corneal rigidity of porcine and rabbit corneas after corneal cross-linking.[7] Studies on humans with keratoconus have demonstrated satisfactory short-term and long-term findings with substantial topographic and refractive improvement following treatment.[13] A considerable decline in topographic parameters such as keratometry, apical gradient curvature, inferior-superior index, cone area, and corneal aberrations after CXL has been reported.[14]
Greenstein and colleagues showed changes in corneal thickness one year after CXL for keratoconus and corneal ectasia.[15]
Our study, like other previous studies shows that CXL with riboflavin is effective in halting the progression of keratoconus.[16] For example, our study showed that the mean of preoperative posterior best-fit sphere (BFS) was 6.33 ± 0.35mm (range: 5.51 to 7.73 mm) before operation and that it improved to 6.28 ± 0.34 mm (range: 4.36 to 6.13 mm) after operation; the difference was significant. Our results are similar to the research of Saffarian and colleagues.[17] The study mentioned was also done on the Iranian population in 2010. This study showed a statistically significant decrease in cylindrical power (P < 0.001) and decline of −0.18 ± 0.79 diopter (D) in spherical power (P > 0.05).[17]
In 2008, Raiskup-Wolf et al.[18] described what remains the largest published series comprising 241 eyes followed in Dresden for up to six years after cross-linking. This uncontrolled, retrospective study confirmed earlier findings with statistically significant improvements in astigmatism, best-corrected visual acuity (BCVA), and maximum simulated keratometry values (Kmax) at 12 months. Flattening was observed in 54% of eyes with a mean change in Kmax of -1.91 D (P < 0.01). The effects of cross-linking were maintained over the duration of follow-up with progression of the disease documented in only two patients (which responded to retreatment). Subsequent published reports from several other centers have described similar results.[18]
Our study showed that the mean baseline corneal pachymetry was 459.17 ± 45.92 μm (range: 311 to 576 μm). One year postoperatively, the mean corneal thickness decreased significantly to 446.05 ± 59.63 μm (range: 309 to 560 μm) (P = 0.013).
Saffarian and colleagues[17] reported that the mean baseline corneal pachymetry was 460.68 ± 46.59 μm (range: 400 to 576 μm). One year postoperatively, the mean corneal thickness decreased significantly to 445.07 ± 41.57 μm (range: 395 to 570 μm) (P < 0.05). Their results are similar to our study.
Caporossi et al.[19] illustrated that the mean spherical equivalent (SE) declined 2.5 D, postoperatively. These results were topographically confirmed by a reduction in mean keratometry. In our study, the mean preoperative SE was −4.64 ± 2.56 D and the mean postoperative SE was −4.02 ± 2.93 D. Our study also demonstrated a mean difference of 0.62 ± 0.37 D significantly (P = 0.006).
Koller et al.[20] found a significant improvement in four of seven Pentacam topography indices (central keratoconus index, keratoconus index, index of height asymmetry, minimum radius of curvature) one year after CXL. In this study, we also found an improvement in the mean baseline corneal pachymetry, including the mean corneal thickness, as in the Koller study. Thus, although the two studies found an improvement in topography after CXL, it is unclear why some of the improvements were in different topography indices.
Wollensak et al.[8] reported that the riboflavin/UVA treatment leads to a dose-dependent keratocyte damage that can be expected in human corneas down to a depth of 300 μm using a surface UVA dose of 5.4 J/cm2. They reported that a standard surface UVA dose of 3 mW/cm has a toxic effect on the endothelial cells of corneas thinner than 400 μm. But in our study, we had no significant adverse effects among the patients with corneas thinner than 400 μm. Similarly, studies with more than 400 μm pachymetry subjects had no significant adverse effects.[17]
CXL has some benefits compared with other methods of keratoconus treatment. There are no cuts in the body of the cornea. It is much safer than a corneal graft which was very successful in the past, and than even a gas-permeable contact lens, and also there is no chance of rejection (some grafts tend to last around 10-15 years). The transplant carries risks such as infection, rejection, cataracts, glaucoma, and astigmatism. At 15 years, there is no difference in the survival rate between penetrating corneal transplants performed for keratoconus and those performed for all other indications. Young keratoconus patients are likely to need one or more repeated grafts during their lifetime. Cross-linking avoids the removal of any corneal structural tissue (only the surface epithelial cells are removed and these grow back mostly within two days).[21]
In conclusion, our study showed a significant improvement in topographic corneal changes and refractive results in patients with corneal ectasia after CXL. These results can illustrate the efficacy and usage of CXL for keratoconus among Iranian patients. However, there are still few clinical trials on the efficacy and safety of CXL in the Iranian population, and future studies are necessary.
Footnotes
Source of Support: School of Medicine of Isfahan University of Medical Science, Isfahan, Iran
Conflict of Interest: This research supported with School of Medicine of Isfahan University of Medical Science, Isfahan, Iran.
REFERENCES
- 1.Pantanelli S, MacRae S, Jeong TM, Yoon G. Characterizing the wave aberration in eyes with keratoconus or penetrating keratoplasty using a high-dynamic range wavefront sensor. Ophthalmology. 2007;114:2013–21. doi: 10.1016/j.ophtha.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 2.Kennedy RH, Bourne WM, Dyer JA. A 48-year clinical and epidemiologic study of keratoconus. Am J Ophthalmol. 1998;101:267–73. doi: 10.1016/0002-9394(86)90817-2. [DOI] [PubMed] [Google Scholar]
- 3.Tuft SJ, Moodaley LC, Gregory WM, Davison CR, Buckley RJ. Prognostic factors for progression of keratoconus. Ophthalmology. 1994;101:439–47. doi: 10.1016/s0161-6420(94)31313-3. [DOI] [PubMed] [Google Scholar]
- 4.Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-A-induced collagen cross-linking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–7. doi: 10.1016/s0002-9394(02)02220-1. [DOI] [PubMed] [Google Scholar]
- 5.Spoerl E, Wollensak G, Seiler T. Increased resistance of crosslinked cornea against enzymatic digestion. Current Eye Research. 2004;29:35–40. doi: 10.1080/02713680490513182. [DOI] [PubMed] [Google Scholar]
- 6.Spoerl E, Wollensak G, Dittert DD, Seiler T. Thermomechanical behavior of collagen-cross-linked porcine cornea. Ophthalmologica. 2004;218:136–40. doi: 10.1159/000076150. [DOI] [PubMed] [Google Scholar]
- 7.Kohlhaas M, Spoerl E, Schilde T, Unger G, Wittig C, Pillunat LE. Biomechanical evidence of the distribution of cross-links in corneas treated with riboflavin/ultraviolet A light. J Cataract Refract Surg. 2006;32:279–83. doi: 10.1016/j.jcrs.2005.12.092. [DOI] [PubMed] [Google Scholar]
- 8.Wollensak G, Spoerl E, Wilsch M, Seiler T. Keratocyte apoptosis after corneal collagen cross-linking using riboflavin/UVA treatment. Cornea. 2004;23:43–9. doi: 10.1097/00003226-200401000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Mazzotta C, Balestrazzi A, Traversi C, Baiocchi S, Caporossi T, Tommasi C, et al. Treatment of progressive keratoconus by riboflavin-UVA-induced cross-linking of corneal collagen ultrastructural analysis by Heidelberg retinal tomograph II in vivo confocal microscopy in humans. Cornea. 2007;26:390–7. doi: 10.1097/ICO.0b013e318030df5a. [DOI] [PubMed] [Google Scholar]
- 10.Agrawal VB. Corneal collagen cross-linking with riboflavin and ultraviolet - A light for keratoconus: Results in Indian eyes. Indian J Ophthalmol. 2009;57:111–4. doi: 10.4103/0301-4738.44515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spoerl E, Mrochen M, Sliney D, Trokel S, Seiler T. Safety of UVA – riboflavin cross-linking of the cornea. Cornea. 2007;26:385–9. doi: 10.1097/ICO.0b013e3180334f78. [DOI] [PubMed] [Google Scholar]
- 12.American Academy of Ophthalmology. Corneal Collagen Crosslinking: Treatment Results In Keratoconus Patients. Science Daily. 2008. Nov 9, [Last accessed on 2012 May 25]. Available from: http://www.sciencedaily.com/releases/2008/11/081109074606.htm .
- 13.Caporossi A, Mazzotta C, Baiocchi S, Caporossi T. Long-term results of riboflavin ultraviolet a corneal collagen cross-linking for keratoconus in Italy: The Siena eye cross study. Am J Ophthalmol. 2010;149:585–93. doi: 10.1016/j.ajo.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 14.Vinciguerra P, Albè E, Trazza S, Rosetta P, Vinciguerra R, Seiler T, et al. Refractive, topographic, tomographic, and aberrometric analysis of keratoconic eyes undergoing corneal cross-linking. Ophthalmology. 2009;116:369–78. doi: 10.1016/j.ophtha.2008.09.048. [DOI] [PubMed] [Google Scholar]
- 15.Greenstein SA, Shah VP, Fry KL, Hersh PS. Corneal thickness changes after corneal collagen crosslinking for keratoconus and corneal ectasia: One year results. J Cataract Refract Surg. 2011;37:691–700. doi: 10.1016/j.jcrs.2010.10.052. [DOI] [PubMed] [Google Scholar]
- 16.Wollensak G. Corneal collagen crosslinking: New horizons. Expert Rev Ophthalmol. 2010;5:201–15. [Google Scholar]
- 17.Saffarian L, Khakshoor H, Zarei-Ghanavati M, Esmaily H. Corneal Crosslinking for Keratoconus in Iranian Patients: Outcomes at 1 year following treatment. Middle East Afr J Ophthalmol. 2010;17:365–8. doi: 10.4103/0974-9233.71600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raiskup-Wolf F, Hoyer A, Spoerl E, Pillunat LE. Collagen crosslinking with riboflavin and ultraviolet-A light in keratoconus: Long-term results. J Cataract Refract Surg. 2008;34:796–801. doi: 10.1016/j.jcrs.2007.12.039. [DOI] [PubMed] [Google Scholar]
- 19.Caporossi A, Mazzotta C, Baiocchi S, Caporossi T. Long-term results of riboflavin ultraviolet a corneal collagen cross-linking for keratoconus in Italy: The Siena eye cross study. Am J Ophthalmol. 2010;149:585–93. doi: 10.1016/j.ajo.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 20.Koller T, Iseli HP, Hafezi F, Vinciguerra P, Seiler T. Scheimpflug imaging of corneas after collagen cross-linking. Cornea. 2009;28:510–5. doi: 10.1097/ICO.0b013e3181915943. [DOI] [PubMed] [Google Scholar]
- 21.Snibson GR. Collagen cross-linking: A new treatment paradigm in corneal disease-a review. Clin Experiment Ophthalmol. 2010;38:141–53. doi: 10.1111/j.1442-9071.2010.02228.x. [DOI] [PubMed] [Google Scholar]


