Abstract
Objective:
To study the problems faced during the surgery and follow-up of modified complete primary repair of exstrophy (CPRE) technique. Initial experience with CPRE and its short- and long-term outcomes with respect to continence status and psychosocial impact are reported.
Materials and Methods:
A retrospective review of the hospital case records from March 2008 to September 2012 was performed. Data of patients with bladder exstrophy managed by a single paediatric surgeon using modified CPRE technique were analysed. Quality of life and psychosocial impact of the surgery were assessed using Pediatric Quality of Life Inventory (PedsQL 4.0) and compared with those of typical peers.
Results:
Eight children (age 4 days-12 years) underwent CPRE using modified Mitchell's technique. Two patients (25%) experienced early postoperative complications, with infection and fistula developing in one each. All the patients were doing well on follow-up, with variable continence rates and good cosmesis. Mean duration of follow-up was 18.5 months (range 6 months-4 years). Five out of seven (71%) children were continent or partially continent. One case was lost to follow-up. PedsQL scores were comparable with those of age-matched peers in all domains except the social functioning domain in 8-12 years age group (83.53 ± 9.70 vs. 77.86 ± 10.22, P < 0.05).
Conclusion:
Our preliminary results with modified CPRE in neonates and children have been encouraging. No major complications were observed. Continence rate was satisfactory and cosmetic results were good. Though the technique is being practiced at several Indian centres, there is a paucity of comprehensive Indian data on CPRE.
KEY WORDS: Bladder exstrophy, complete primary repair, urinary continence
INTRODUCTION
Surgical management of bladder exstrophy has evolved tremendously over the last several decades.[1,2] Although the modern staged repair of exstrophy (MSRE) currently savours widespread popularity, complete primary repair of exstrophy (CPRE) potentially provides socially acceptable continence in a single surgery. Primary closure of bladder exstrophy without lower limb immobilisation and osteotomies has been recently demonstrated.[3] However, according to Gearhart, CPRE in the neonatal period is a formidable task fraught with complications even in experienced hands.[4] There are very few reports on complete primary repair in the newborn period from Indian centres.[5,6] We report our initial experience with CPRE in paediatric patients, all treated by a single surgeon at a tertiary care centre located in northern Karnataka.
MATERIALS AND METHODS
Hospital records of patients with bladder exstrophy operated by a single paediatric surgeon were analysed. Children with only epispadias and those previously operated for exstrophy were excluded. Ethical clearance for the study was obtained from the hospital authority.
CPRE was done employing the modified Mitchell's technique. The Mitchell's procedure[7] incorporates the three goals of staged reconstruction performed in a single-stage surgery: Bladder closure, epispadias repair and achievement of urinary continence, preferably in the neonatal period. The bladder, bladder neck and urethra are moved posteriorly within the pelvis facilitating re-approximation of the pubic symphysis and this reproduces the normal morphology with improved urinary continence. Total penile disassembly reduces anterior tension on the urethra, which decreases the risk of bladder dehiscence and dorsal chordee. Also, separation of urethra from corpora cavernosa allows adequate exposure and proximal dissection of inter-symphyseal ligament located posterior to the urethra, allowing posterior placement of the bladder without tension. Proper identification of the bladder neck, which lies proximal to the verumontanum in boys and just distal to the trigone in girls, is crucial.
Our operative technique included extraperitoneal mobilisation of urinary bladder [Figure 1a] with ureteric catheters in situ and bladder closure in two layers over suprapubic Malecot's catheter. Bladder capacity was assessed after closure using the suprapubic catheter [Table 1]. Near-complete penile disassembly [Figure 1b], division of inter-symphyseal bands and wrapping around bladder neck, and bilateral superior pubic ramus osteotomies were done under general with epidural anaesthesia in all patients including the two newborns. Epispadias repair was done using modified Cantwell–Ransley (corporal bodies medially rotated and fixed to each other by sutures and Ipgam procedure) technique. Ipgam (or reverse Duckett) denotes the reversal of the technique Meatal Advancement and Glanuloplasty (MAGPI). Catheters were sequentially removed by 12-18 days following surgery. Following discharge, patients were followed prospectively for clinical outcome, radiological data on the progression of vesicoureteric reflux (using voiding cystourethrogram) and scarring on dimercapto succinic acid (DMSA) scan. Urodynamic status (yearly), urinary continence status (during each visit) and episodes of urinary tract infections (3-monthly urine cultures) were documented [Figure 2]. Continence was defined as a dry interval >2 h and spontaneous voiding without catheterisation, and partial continence as dry for a period between 1 and 2 h.
Figure 1.

(a) Extraperitoneal bladder mobilisation. (b) Near-complete penile disassembly. (c) Neurovascular bundle dissection in newborn. (d) Postoperative cosmetic appearance
Table 1.
Demographic and baseline characteristics of our subjects

Figure 2.

(a) Voiding cystourethrogram showing bilateral vesicoureteric reflux. (b) Urodynamic study showing good capacity, compliance and flow pressures
Pediatric quality of life inventory (PedsQL 4.0), a 15-item questionnaire for children, was used to assess the quality of life.[8] The PedsQL 4.0 English version was translated into vernacular language (Kannada). The scores were calculated for physical functioning (5 items), emotional functioning (4 items), social functioning (3 items) and school functioning (3 items). Answering options were never (0), almost never (1), sometimes (2), often (3) and almost always (4). Each answer was reverse scored and rescaled to 0-100 scale (0 = 100, 1 = 75, 2 = 50, 3 = 25 and 4 = 0). The mean scores for each domain were then calculated and compared with the scores of age-matched healthy peers attending the paediatric out-patient department. Scoring scale ranged from zero to 100, with zero reflecting the worst quality of life and higher psychosocial morbidity and 100 reflecting excellent quality of life. Parent proxy-report was used in children aged less than 8 years. To study the psychosocial impact of the condition on parents, a questionnaire was prepared using pediatric inventory for parents (PIP) as the reference. Rating was done on a 5-point Likert scale for subjective difficulty faced by the parents. The maximum score of 60 represented higher psychosocial morbidity. Statistical methods included quantitative variables summarised by mean and standard deviation. Wilcoxon signed rank test was used for comparing the scores in various domains of the questionnaire (per age group) using SPSS 16.0 software package.
RESULTS
Between March 2008 and September 2012, eight children with classic bladder exstrophy underwent complete primary repair. Table 1 shows the baseline and demographic data of our cases. Two out of eight patients were females. CPRE was performed within the first 4 days of life in two cases. CPRE with osteotomy was done in six cases at a mean age of 5.6 years (range 2-8 years). None of our patients had other major congenital malformations; Two had bilateral undescended testes with inguinal herniae which were operated during the same surgery. Three of our patients had gross polypoid changes of bladder at the time of surgery. One patient developed fluid overload and pulmonary oedema postoperatively and recovered with fluid restriction and diuretics. Postoperative vesicocutaneous fistula in another child closed spontaneously before discharge from the hospital.
The mean duration of follow-up was 18.5 months (range 6 months-4 years). Long-term outcomes including the duration of follow-up and urinary continence status are shown in Table 2. All patients voided in stream during follow-up [Figure 3]. Five out of seven (71%) children were continent or partially continent, which were reported by the parents as socially acceptable. One case was lost to follow-up. Four patients had gaping of symphysis pubis at 1 year. Five out of eight patients underwent urodynamic studies 1 year after surgery. All had small to moderate capacity bladders, moderate pressures and moderate flow rates. Vesicoureteric reflux of low grade was present in all seven patients who underwent voiding cystourethrogram studies, but none had progressive hydronephrosis. Two of our patients had febrile urinary tract infection (UTI) during follow-up. None of our patients had hypospadias or penile loss. Bladder neck reconstruction (BNR) was done in one female child. Persistence of penoscrotal dissociation was observed in all boys.
Table 2.
Outcome of modified complete primary repair of exstrophy in the present series
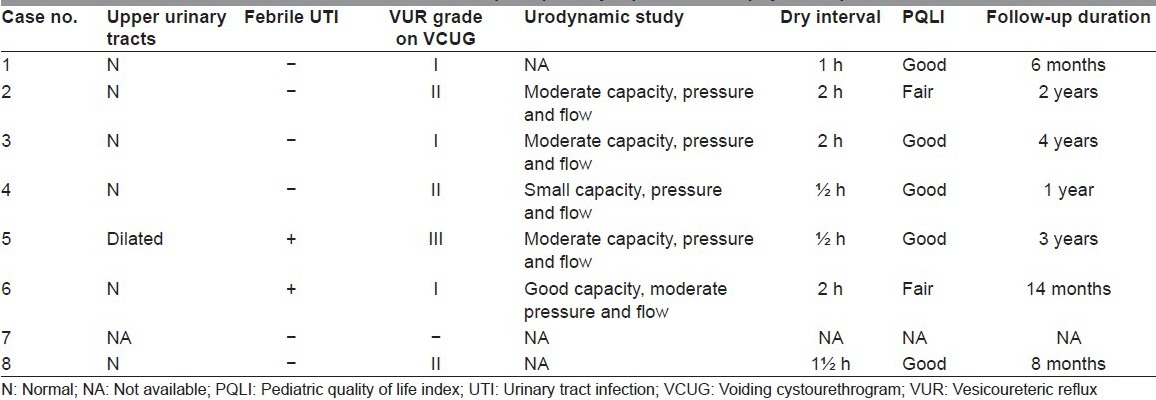
Figure 3.

Photograph taken during the follow-up of a 7-year-old boy, displaying voiding with good stream
PedsQL scores in our patients in all domains were similar when compared with their age-matched typical peers, except in the social functioning subscale in 8-12 years age group (83.53 ± 9.70 vs. 77.86 ± 10.22, P < 0.05). The overall parents’ perceived difficulty (mean score = 112.8 ± 12) of parenting stress was moderate with a mean PIP frequency of 96.4 ± 18.
DISCUSSION
The current emphasis in the management of exstrophy bladder is on limiting the frequency and morbidity of surgical procedures.[9] In our series, we had performed exstrophy and epispadias repairs in a single stage to reduce the costs and morbidity associated with multiple operations. We opted for near-complete penile disassembly, a modification of the “total penile disassembly” technique of Mitchell, wherein the distal-most attachment of the urethral plate to the glans is left intact, thereby achieving a glandular meatus and avoiding necrosis of glans penis and corporal bodies. This technique can avoid hypospadias, but may result in reduced penile length and persistence of penoscrotal dissociation as seen in our series. We did superior pubic ramus osteotomy (SPRO) in all cases, except the newborns. The advantages of SPRO are the ease of the procedure, minimal blood loss, and no need for another skin incision or turning the patient on the operating table. Though re-diastasis was observed in four of our patients during follow-up, it is stated to be common to all osteotomy techniques.[10] In three of our patients, the bladder had gross polypoid changes, which are considered by some authors as difficult bladders to close.[2] However, in our experience, these patients also had good outcomes and the results were comparable with others without such changes.
CPRE results in normal bladder cycling, optimises capacity and compliance, and may obviate the need for augmentation. However, it may not consistently achieve the goal of normal voiding in most of the patients. In the longest follow-up study of CPRE from Seattle,[11] 76% of 29 patients who underwent CPRE developed continence (dry interval >2 h) compared with 27% of 77 staged repairs requiring augmentation in the same institution. In our series, five out of seven (71%) children were either continent or partially continent (dry interval 1-2 h) during a mean follow-up period of 18.5 months. Though CPRE proposes to establish continence without the need for bladder neck repair (BNR), recent studies have demonstrated the need for an outlet procedure in most patients.[11,12] However, if CPRE is successful, BNR results tend to be favourable without the need for bladder augmentation.[13] One female child in our series had persistent incontinence secondary to inadequate bladder outlet resistance. We performed Young-Dees-Leadbetter-Politano BNR which led to good bladder capacity post-BNR.
Schaeffer et al. recently reported that post-CPRE complications in females include dehiscence, prolapse and stricture, and in males include dehiscence, prolapse, pubic separation and stricture. Out of 27 patients who underwent BNR, 15 (56%) were subsequently continent, 5 (19%) were daytime continent with nocturnal incontinence and 7 (26%) were continuously incontinent.[14] Hypospadias following CPRE is reported in two-thirds of boys, whereas we had no hypospadias due to the modification in epispadias repair. The most feared complication following CPRE has been the partial or complete hemiglans and corporal loss (incidence 5-12%), which may be seen in any bladder exstrophy closure method; it was avoided by incomplete penile disassembly technique in our series. Comparing the urodynamic findings, Borer et al. reported that CPRE patients ubiquitously had better bladder stability and compliance than those undergoing modern staged repair, whereas bladder capacity in the two groups was comparable.[15] Urodynamic studies done in five of our patients revealed small- to moderate-capacity bladders, moderate pressures and good flow rates. Only one patient had progression of hydronephrosis in the current series. Febrile UTI observed in two of our patients was due to drug non-compliance; none had pyelonephritis. The reported incidence of progressive or severe hydronephrosis and/or renal scarring ranges from 0 to 30%.[1,2]
Despite widespread practice, long-term outcome of modern reconstructive technique of the exstrophy bladder remains controversial.[16] Lack of long-term follow-up has been the major drawback in the assessment of superiority of one technique over the other.
Reiner and Gearhart have previously reported that children with bladder exstrophy are more vulnerable to anxiety disorder ontogenesis than their peers and experience clinically significant anxiety disorders.[17] In a recent study, health-related quality of life scores on the Child Health Questionnaire Form-87 among adolescents with bladder exstrophy were reported as “good” when descriptively compared with a reference population.[18] We assessed the psychosocial impact of the condition on parents and the quality of life of children, which is one of the strengths of our study. However, we did not compare them with other children managed with alternative exstrophy repair techniques. Nonetheless, our findings may evoke the need for developing targeted interventions to help parents cope with their child's illness.
In India, over the years, authors at several paediatric centres have demonstrated expertise in diverse bladder reconstruction techniques.[19,20] However, considering the recent literature on CPRE, there is a conspicuous absence of published Indian data on CPRE results, especially the long-term outcome. With regard to bladder exstrophy management, the current Indian scenario has been elucidated in a recent editorial.[20] Though it has been claimed that expertise in comprehensive management of bladder exstrophy is available at select Indian centres, none of these have reported the comparative outcomes of CRPE and other techniques. Ray et al., in 2002, reported 10 cases of single-stage repair out of 37 cases with exstrophy — epispadias complex and found that it was “more successful” than staged repair.[5] However, their reporting of individual patient data on continence and urodynamic studies was brief. In a recent study from Chandigarh, the authors quantified the outcome of exstrophy repair in terms of quality of life using the scoring system.[6]
CONCLUSION
Successful primary closure provides the exstrophic bladder the best opportunity to progress through normal bladder development. We feel that it is one of the major determinants of eventual bladder capacity and compliance. Our preliminary experience suggested that CPRE decreases the number of surgeries and is safe and efficacious even in newborns. We found the urinary continence difficult to achieve, but it was possible to accomplish socially acceptable continence.
Our literature review indicated that though various approaches are being practiced at several centres in India, comprehensive Indian data on complete primary repair are lacking. Further long-term follow-up studies are necessary to compare the results of CPRE with modern staged repair in Indian setting.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Husmann DA. Surgery insight: Advantages and pitfalls of surgical techniques for the correction of bladder exstrophy. Nat Clin Pract Urol. 2006;3:95–100. doi: 10.1038/ncpuro0407. [DOI] [PubMed] [Google Scholar]
- 2.Gearhart JP, Mathews RI. Exstrophy-epispadias complex. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 6th ed. Philadelphia: Saunders Elsevier; 2012. pp. 3325–78. [Google Scholar]
- 3.Mushtaq I, Garriboli M, Smeulders N, Cherian A, Desai D, Eaton S, et al. Primary neonatal bladder exstrophy closure- challenging the traditions. J Urol. 2013 Jul 18; doi: 10.1016/j.juro.2013.07.020. E-pub Ahead of Print. [DOI] [PubMed] [Google Scholar]
- 4.Gearhart JP. Complete primary repair of bladder exstrophy: Complications and management. J Urol. 2001;165:2431–3. doi: 10.1016/S0022-5347(05)66222-2. [DOI] [PubMed] [Google Scholar]
- 5.Ray AK, Mukherjee NN, Mukherjee S, Mukharjee P. Total correction of bladder exstrophy- our experience in 37 patients. Indian J Urol. 2002;18:117–9. [Google Scholar]
- 6.Kanojia RP, Agrawal S, Rathod KK, Bawa M, Menon P, Mahajan JK, et al. Quantified outcome for patients with bladder exstrophy. J Pediatr Urol. 2013;9:298–302. doi: 10.1016/j.jpurol.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 7.Grady RW, Mitchell ME. Complete primary repair of exstrophy. J Urol. 1999;162:1415–20. [PubMed] [Google Scholar]
- 8.Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: Feasibility, reliability, and validity. Ambul Pediatr. 2003;3:329–41. doi: 10.1367/1539-4409(2003)003<0329:tpaapp>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 9.Mahajan JK, Rao KL. Exstrophy-epispadias complex- Issues beyond the initial repair. Indian J Urol. 2012;28:382–7. doi: 10.4103/0970-1591.105747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chiari G, Avolio L, Bragheri R. Bilateral anterior pubic osteotomy in bladder exstrophy repair: Report of increasing success. Pediatr Surg Int. 2001;17:160–3. doi: 10.1007/s003830000470. [DOI] [PubMed] [Google Scholar]
- 11.Shnorhavorian M, Grady RW, Andersen A, Joyner BD, Mitchell ME. Long-term follow up of complete primary repair of exstrophy: The Seattle experience. J Urol. 2008;180:1615–9. doi: 10.1016/j.juro.2008.04.085. [DOI] [PubMed] [Google Scholar]
- 12.Gargollo PC, Borer JG, Diamond DA, Hendren WH, Rosoklija I, Grant R, et al. Prospective follow up in patients after complete primary repair of bladder exstrophy. J Urol. 2008;180:1665–70. doi: 10.1016/j.juro.2008.05.076. [DOI] [PubMed] [Google Scholar]
- 13.Gearhart JP, Baird A, Nelson CP. Results of bladder neck reconstruction after newborn complete primary repair of exstrophy. J Urol. 2007;178:1619–22. doi: 10.1016/j.juro.2007.03.175. [DOI] [PubMed] [Google Scholar]
- 14.Schaeffer AJ, Stec AA, Purves JT, Cervellione RM, Nelson CP, Gearhart JP. Complete primary repair of bladder exstrophy: A single institution referral experience. J Urol. 2011;186:1041–6. doi: 10.1016/j.juro.2011.04.099. [DOI] [PubMed] [Google Scholar]
- 15.Borer JG, Gargollo PC, Hendren WH, Diamond DA, Peters CA, Atala A, et al. Early outcome following complete primary repair of bladder exstrophy in the newborn. J Urol. 2005;174:1674–8. doi: 10.1097/01.ju.0000175942.27201.59. [DOI] [PubMed] [Google Scholar]
- 16.Gobet R. Alternative management of bladder exstrophy. Curr Opin Urol. 2009;19:424–6. doi: 10.1097/MOU.0b013e32832c90af. [DOI] [PubMed] [Google Scholar]
- 17.Reiner WG, Gearhart JP. Anxiety disorders in children with the epispadias-exstrophy complex. Urology. 2006;68:172–4. doi: 10.1016/j.urology.2006.01.056. [DOI] [PubMed] [Google Scholar]
- 18.Schaeffer AJ, Yenokyan G, Alcon K, Furth SL, Diener-West M, Wu A, et al. Health related quality of life in adolescents with bladder exstrophy- epispadias as measured by the child health questionnaire-child form 87. J Urol. 2012;188:1924–9. doi: 10.1016/j.juro.2012.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kulkarni B, Chaudhary N, Yadav S, Oak SN. A new technique for repair of exstrophy-epispadias complex. Pediatr Surg Int. 2002;18:559–62. doi: 10.1007/s00383-002-0777-4. [DOI] [PubMed] [Google Scholar]
- 20.Bhatnagar V. The management of bladder exstrophy: Indian scenario. J Indian Assoc Pediatr Surg. 2011;16:43–4. doi: 10.4103/0971-9261.78128. [DOI] [PMC free article] [PubMed] [Google Scholar]


