Abstract
As well as craniofacial synostosis, complex syndactyly of hands is a distinctive feature of Apert syndrome. Consideration of blood flow to the digits is very important in separation surgery. Several reports offer information about arterial distribution in Apert's hands. Though, venous pattern has not been well discussed. Infrared venography offers a real-time image with minimal invasion. An Apert syndrome patient underwent a series of finger splitting surgeries. Infrared venography was carried out to assess veins. There was a palmar venous arch, placing distally to the metacarpophalangeal joint. The arch had to be cut to divide fused fingers sufficiently. As well as arterial abnormality, venous uniqueness should be noted in Apert syndactyly surgeries. Infrared venography, which can be carried out easily, offers good information that surgeon require.
KEY WORDS: Anomaly, Apert syndrome, hand, infrared, syndactyly, vein
INTRODUCTION
The hands in Apert syndrome often demonstrate so-called spoon hand or mitten hand deformity, including syndactyly, symphalangism and soft-tissue anomalies. Consideration of blood flow to the digits of each patient, not only arterial supply but also venous drainage, is very important in the division surgery. Infrared venography is one of the most less-invasive modalities. A 1-year-old boy with Apert syndrome underwent finger separation surgeries. Infrared venography was performed on the table, just prior to the surgeries.
CASE REPORT
An Apert syndrome infant with Upton's Type II[1] hands underwent a series of surgeries. At the age of 14 months, separation between the middle and ring fingers was done. Under general anaesthesia, just prior to the operation, infrared venography was done with Genial-Viewer® (Genial Light Co. Ltd., Hamamatsu, Japan) [Figure 1] and recorded in a laptop computer. Simple straight line separation with dorsal rectangular flap was performed. Full thickness skin graft was taken from the lower abdomen and replanted to cover the defect. Separation of index-middle and ring-little fingers was performed 5 months after [Figure 2]. Infrared venography was carried out again. Arterial or venous insufficiency of digits was not observed through both surgeries.
Figure 1.

Genial-Viewer® is consisted of measuring module (front), power supply unit (back right) and a laptop computer for data processing and storage
Figure 2.
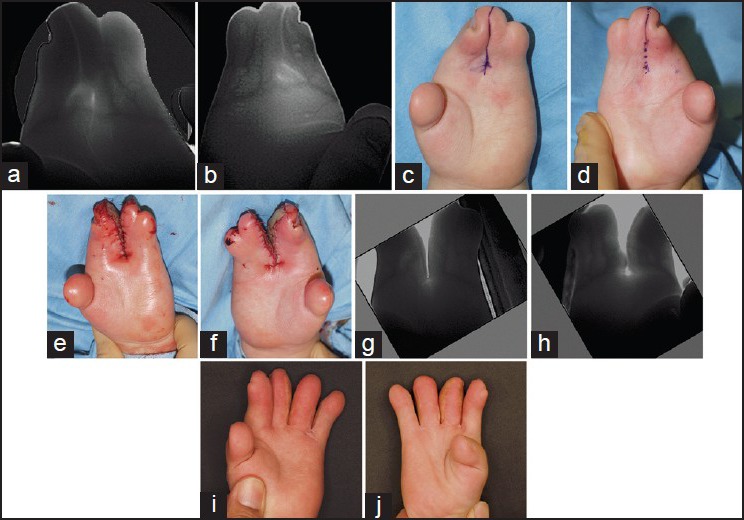
Infrared venography through finger splitting surgeries for an Apert patient. Volar venous arch placed distally to the metacarpophalangeal joint, where incision had to be performed to divide fingers sufficiently. (a, b) Snap shots of palmar side venogram, immediately before the separation surgery. (c, d) Designs for the first separation surgery, (e and f) Immediately after the first separation surgery. (g, h) Snap shots of venogram, immediately before the second separation surgery. Volar venous arch was severed between the middle and ring fingers. (I, j) Fifteen months after the second separation surgery
Infrared venogram
Infrared venography was able to visualise superficial veins, which could not be seen with bare eyes. The veins were recognised as dark lines. Real-time venogram was able to be seen through display of a laptop computer. The images were captured and recorded. Furthermore, video could be recorded. At the time before the separation procedures, vein of digits flows into venous arch on the volar aspect. The arch placed distally to the metacarpophalangeal joint, where incision has to be done to divide fingers sufficiently. Longitudinal vein of palm was observed very thin. On the dorsal aspect, for his left hand, veins could be observed on the radial margin of index, radial side of middle and ulnar margin of little finger. No proper dorsal vein of the ring finger could be identified at that moment. On the dorsum of his right hand, a vein runs on the index finger supplying branches to the middle finger. The other runs slightly radial side of ring-little inter-digital space, which seemed likely to be damaged by separation procedure [Figure 3]. At the time of immediately before secondary splitting surgery, palmar venous arch revealed to be severed by the first surgery [Figure 2].
Figure 3.
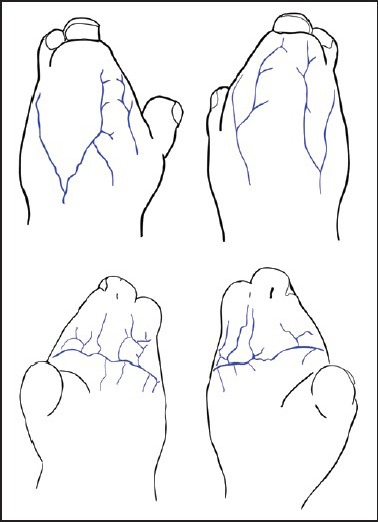
Venogram of the Apert patient's hands, based on infrared video and snap shots. Not all of the fingers had their own proper dorsal vein. There were palmar venous arches on both hands, which placed distally to the metacarpophalangeal joint
DISCUSSION
To perform separation surgery for syndactyly, understanding of vascular distribution is very important. Several reports offer information about arterial anatomy of Apert syndrome hands. With angiography, absence of superficial palmar arch and mono arterialisation of all fingers were pointed out.[2,3] Upton reported,[1] based on his operative records, that a dominant deep palmar arch was present usually abnormally far into webspaces before digital bifurcation was demonstrated. With three-dimensional computed tomography (CT) and magnetic resonance imaging, Holten et al. reported that common digital arteries tended to bifurcate after the metacarpophalyngeal joint.[4] Description about venous distribution was scarcely seen. Only writing could be found was a report with digital video angiography, stating “normal venous return”.[3] This is the first report of venous abnormality in hands of an Apert syndrome patient.
Light transmission through tissues is greatest within the red and near infrared wavelength.[5] At near infra-red band, haemoglobin has lower absorbance than at visible band, though it is relatively high in comparison with other protein in the tissue. Therefore, absorbance contrast between vessels and surrounding tissue can be used to visualise vascular pattern.[6] No contrast agent has to be administered [Figure 4].
Figure 4.
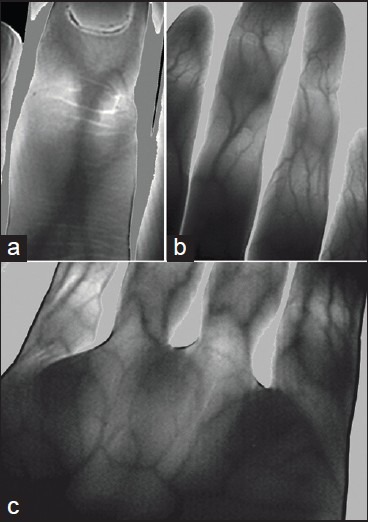
Infrared venogram of an author's hand
Nowadays, infrared venography of finger[7] or palm[8] has been widely used for personal identification in automated teller machines. Based on the same theory, Genial-Viewer® was designed to visualise vasculature beneath skin. It is consisted of measuring module, power supply unit and lap-top computer for data processing and storage. Measuring module is composed of infrared submission table and camera, connected with an arm. It is light and handy. Real-time image can be seen. Both still image and moving picture can be recorded. The recorded data can be processed and analysed digitally. It can be used in the operative field only have to be wrapped with an ordinal sterile plastic bag. As infrared ray has strong diffusional scattering character through tissue, it cannot penetrate thick part of the body. It is suitable to observe superficial veins. In finger replantation surgery, it is useful to find vessels to anastomose. It is also helpful in designing vascularized flaps. Digital arteries can also be observed with certain setting. With software, pulsation speed and acceleration can be analysed. It may be a good tool to evaluate peripheral blood flow. Indocyanine green venography and lymphography can also be performed with the system.
There are several tools to visualise vasculature. X-ray angiography, including three-dimensional CT, offers extensive information, but requires complicated sequence and time. Radiation exposure is inevitable. Magnetic resonance angiography also gives precise image, but requires contrast agent and time. Vascular ultrasonography is a representative example of minimum invasive modality. Though, information obtained is fragmented with a view by view. In the market there are a few infra-red imaging systems, utilising reflected infrared light while Genial-Viewer® employs transmitted light. For visualising blood vessels of hand, transmitted light gives sharper image.
Early surgical intervention is recommended for hand in Apert syndrome,[1,9,10] to minimise progressive growth deformity and influence on patients’ psychological development. Though, splitting all fingers by one stage, performing surgery on both sides of the same digit should be avoided. By means of ultra-red venography, abnormal venous distribution was detected. We have been doing the staged separation surgery for Apert syndactyly hands. Hence, it has not changed our surgery plan. Though, it was confirmed that it is safer to perform staged separation for Apert hand, not only because of the arterial abnormality, but also the abnormal venous distribution.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Upton J. Apert syndrome. Classification and pathologic anatomy of limb anomalies. Clin Plast Surg. 1991;18:321–55. [PubMed] [Google Scholar]
- 2.Mantero R, Ferrari GL, Ghigliazza GB, Auxilia E. Syndactyly: An angiographic study. Ann Chir Main. 1983;2:62–5. doi: 10.1016/s0753-9053(83)80083-0. [DOI] [PubMed] [Google Scholar]
- 3.Mantero R, Auxilia E, de Albertis P, Ferro C. Digital videoangiography of the hand. Ann Chir Main. 1984;3:160–4. doi: 10.1016/s0753-9053(84)80029-0. [DOI] [PubMed] [Google Scholar]
- 4.Holten IW, Smith AW, Isaacs JI, Moore MH, David DJ. Imaging of the Apert syndrome hand using three-dimensional CT and MRI. Plast Reconstr Surg. 1997;99:1675–80. [PubMed] [Google Scholar]
- 5.Hammel HT, Hardy JD, Murgatroyd D. Spectral transmittance and reflectance of excised human skin. J Appl Physiol. 1956;9:257–64. doi: 10.1152/jappl.1956.9.2.257. [DOI] [PubMed] [Google Scholar]
- 6.Kaneko M, Shimizu K, Yamamoto K, Mikami T, Tamura M. Basic study for visualization of blood vessels using near-infrared light. MBE. 1989;89:25–30. [Google Scholar]
- 7.Kono M, Ueki H, Umemura S. Near-infrared finger vein patterns for personal identification. Appl Opt. 2002;41:7429–36. doi: 10.1364/ao.41.007429. [DOI] [PubMed] [Google Scholar]
- 8.Watanabe M, Endoh T, Shiohara M, Sasaki S. Arlington, VA, USA: The proceeding of the conference; 2005. Palm vein authentication technology and its applications. The Biometric Consortium Conference. can be seen on a website: http://www.biometrics.org/bc2005/bc2005.php . [Google Scholar]
- 9.Barot LR, Caplan HS. Early surgical intervention in Apert's syndactyly. Plast Reconstr Surg. 1986;77:282–7. doi: 10.1097/00006534-198602000-00020. [DOI] [PubMed] [Google Scholar]
- 10.Chang J, Danton TK, Ladd AL, Hentz VR. Reconstruction of the hand in Apert syndrome: A simplified approach. Plast Reconstr Surg. 2002;109:465–70. doi: 10.1097/00006534-200202000-00008. [DOI] [PubMed] [Google Scholar]


