Abstract
We aimed to compare the clinical outcome and cost of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Sixty patients with acute cholecystitis were randomized into early (within 24 hours of admission) or delayed (after 6–8 weeks of conservative treatment) laparoscopic cholecystectomy groups. There was no significant difference between study groups in terms of operation time and rates for conversion to open cholecystectomy. On the other hand, total hospital stay was longer (5.2 ± 1.40 versus 7.8 ± 1.65 days; P = 0.04) and total costs were higher (2500.97 ± 755.265 versus 3713.47 ± 517.331 Turkish Lira; P = 0.03) in the delayed laparoscopic cholecystectomy group. Intraoperative and postoperative complications were recorded in 8 patients in the early laparoscopic cholecystectomy group, whereas no complications occurred in the delayed laparoscopic cholecystectomy group (P = 0.002). Despite intraoperative and postoperative complications being associated more with early laparoscopic cholecystectomy compared with delayed intervention, early laparoscopic cholecystectomy should be preferred for treatment of acute cholecystitis because of its advantages of shorter hospital stay and lower cost.
Key words: Acute cholecystitis, Laparoscopic cholecystectomy, Outcome assessment, Cost and cost analysis
Elective laparoscopic cholecystectomy has become the gold standard for treatment of symptomatic gallstones.1 However, in the early days, acute cholecystitis was a contraindication of laparoscopic cholecystectomy, and patients with acute cholecystitis were managed conservatively and discharged for re-admission in order to have elective surgery performed for the definitive treatment.2,3 Then, randomized controlled trials and meta-analyses had shown the benefits of early surgery (within the acute admission period, which is 24 to 72 hours) compared with delayed cholecystectomy with respect to hospital stay and costs, with no significant difference in morbidity and mortality.2,4,5 Thus, in the late 1980s early surgery for acute cholecystitis had gained popularity. The updated Tokyo Guidelines announced in 2013 by the Japanese Society of Hepato-Biliary-Pancreatic Surgery suggested that early laparoscopic cholecystectomy is the first-line treatment in patients with mild acute cholecystitis, whereas in patients with moderate acute cholecystitis, delayed/elective laparoscopic cholecystectomy after initial medical treatment with antimicrobial agent is the first-line treatment.6
With the increased experience in laparoscopy, surgeons started to attempt early laparoscopic cholecystectomy for acute cholecystitis.2 However, early laparoscopic cholecystectomy is still performed by only a minority of surgeons.7–9 Furthermore, the exact timing, potential benefits, and cost-effectiveness of laparoscopic cholecystectomy in the treatment of acutely inflamed gallbladder have not been clearly established and continue to be controversial.1,10
The aim of this study was to compare the intra-operative and postoperative outcomes, and cost of early versus delayed laparoscopic cholecystectomy for acute cholecystitis.
Patients and Methods
Study design and population
This was a prospective, randomized, 2-arm clinical study. Between January 2011 and March 2012, 60 patients whose physical, laboratory, and ultrasound findings suggested acute cholecystitis, and who were operated on by laparoscopy, were included in the study. Acute cholecystitis diagnosis was based on a combination of clinical and radiologic criteria. All of the following criteria together constituted an acute episode: right subcostal tenderness; positive Murphy sign; leukocytosis; thickened, edematous distended gallbladder; presence of gallstones; and pericholecystic fluid collection on ultrasound examination. Patients with common bile duct stones, acute pancreatitis, previous upper abdominal surgery, or severe concomitant medical problems deeming them unfit for laparoscopic surgery were excluded from the study.
Each patient gave written informed consent before participation in the study. Approval for this study was obtained from the ethics committee of the Atatürk Training and Research Hospital. The study was conducted in accordance with the latest version of the Declaration of Helsinki and local regulations.
Patients were randomized to the early or delayed operation group using the closed-envelope method. The early operation group was operated on within 24 hours of admission (30 patients), whereas the late operation group was operated on after 6 to 8 weeks following the initial treatment (30 patients). Patients in the delayed group were treated with intravenous fluids, antibiotics, and analgesics. Patients who responded to conservative treatment were discharged after a complete relief of symptoms. They were called for laparoscopic cholecystectomy after 6 or 8 weeks, when the acute episode had subsided.
Laparoscopic cholecystectomy
Laparoscopic cholecystectomy operations were performed by competent trainees under the supervision of a consultant. The surgical procedure was in line with the literature.1 The surgery was done with the patient under general anesthesia using endotracheal intubation. Pneumoperitoneum was created by blind puncture with a Veress needle through a subumbilical incision. Four laparoscopic ports were used: 10-mm umbilical for the optical instrument (0 degrees), 10-mm subxiphoidal for working instruments, 5-mm right subcostal along the midclavicular line also for working instruments, and 5 mm on the right flank for retraction instruments. Adhesion release and exposure of Calot triangle were undertaken first. If necessary, the gallbladder was emptied through a laterally inserted Veress needle to allow better grasping. The cystic pedicle was detected to isolate the cystic duct and the artery separately. Both were then clipped and divided. The gallbladder was dissected off of its bed with a monopolar cautery hook. At completion of the surgery, the gallbladder was placed in a retrieval bag and extracted through the subxiphoidal incision, which was enlarged if necessary. Hemostasis was achieved in the gallbladder bed, and after a through saline lavage, a suction drain was placed if clinically indicated and the incisions closed. When required, a conversion to open surgery was performed through a right subcostal incision.
Evaluation criteria
Demographics, clinical data, and findings for medical history, physical examination, laboratory tests, and ultrasonography were recorded for all patients. The patients were followed up during postoperative hospitalization. The primary evaluation criteria of the study were operative and postoperative variables, such as operation time, hospitalization duration, intraoperative and postoperative complications, and rate of conversion to open cholecystectomy. For the late operation group, hospitalization duration was considered as total length of stay for both first and second hospitalizations (for initial treatment and operation, respectively) added together. The secondary evaluation criterion was treatment-related cost, including costs of surgery, hospitalization, and conservative treatment. The costs of hospitalization include first hospitalization, second hospitalization (for the late operation group), and outpatient visits in between and after the hospitalizations.
For the costs, the price list of medical treatment and intervention defined by the Turkish Ministry of Health was used.
Statistical analysis
The study data were summarized with descriptive statistics (mean, SD, frequency, and percentage). The comparisons between study groups were performed using Student t test for continuous variables and χ2 test for categoric variables. The treatment-related costs were expressed as Turkish Lira (TL), which is the currency of Turkey. As of March 12, 2013, the exchange rate was 1.0 TL = $0.55 as announced by the Central Bank of the Republic of Turkey. The statistical analyses were performed using a commercially available software (Statistical Package for Social Sciences version 15.0, SPSS Inc, Chicago, Illinois). The statistical level of significance was set to P < 0.05.
Results
Study groups
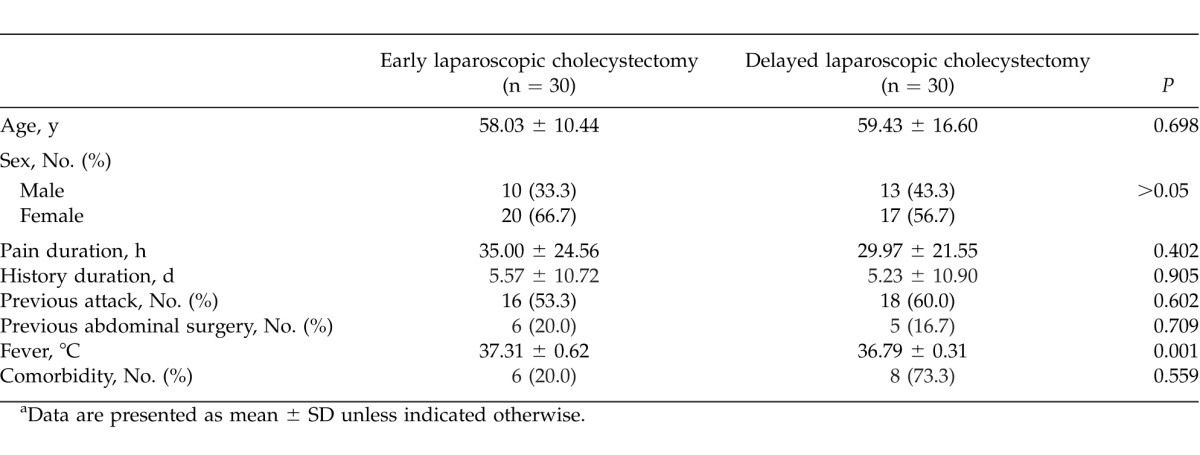
The study groups, which underwent early or delayed laparoscopic cholecystectomy, showed no difference in age and sex distribution. Initial clinical findings and medical history were also similar between groups, except for fever, which was significantly higher in the early laparoscopic cholecystectomy group (37.31°C ± 0.62°C versus 36.79°C ± 0.31°C; P = 0.001). The basic clinical and demographic findings of study patients are summarized in Table 1.
Table 1.
Basic clinical and demographic data of patients in the early and delayed laparoscopic cholecystectomy groupsa
Clinical findings
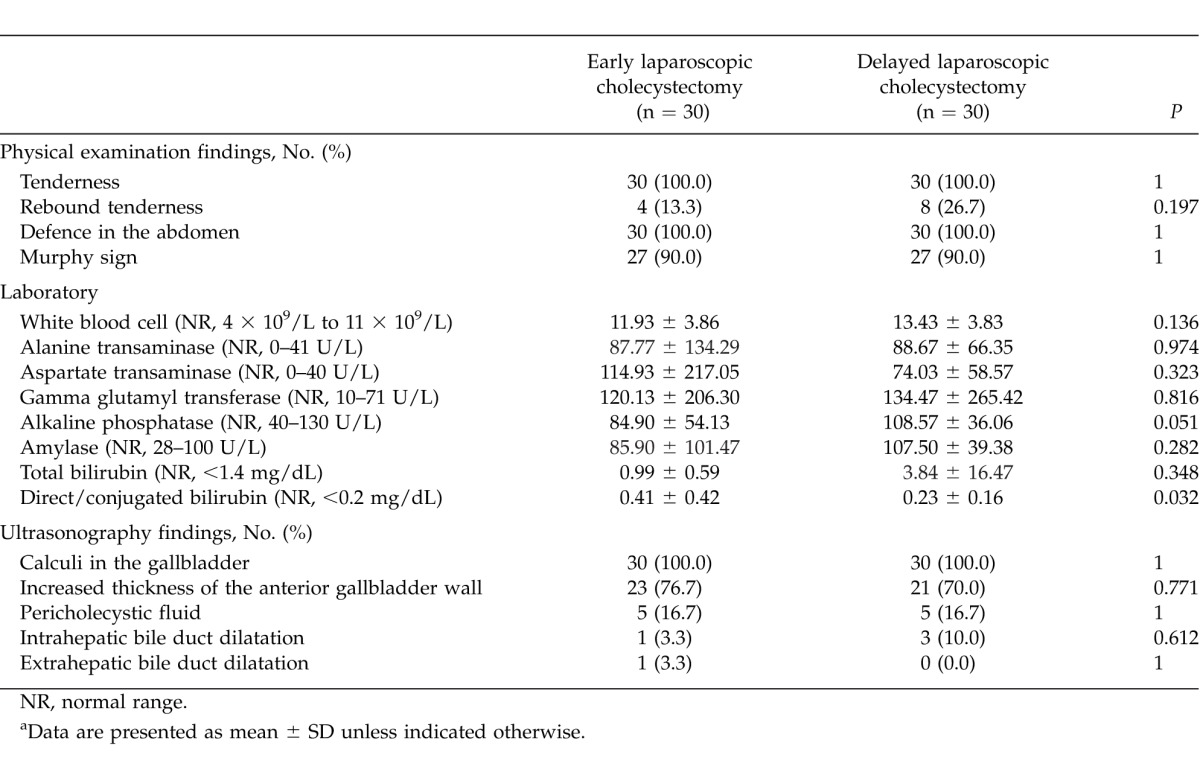
Both groups revealed similar physical examination findings: all patients had tenderness and defense in the abdominal area (this term means tensing the muscles in the abdominal area, a clinical finding that may present when the internal organs are inflamed in some manner) and 90% had Murphy sign, and 13.3% in the early and 26.7% in the late laparoscopic cholecystectomy groups had rebound tenderness. Blood count and liver function results were not different between groups. On ultrasonography, calculi in the gallbladder were detected in all of the patients, and thickness of the anterior gallbladder wall was increased in 23 and 21 patients in the early and delayed laparoscopic cholecystectomy groups, respectively. Other ultrasonography findings were pericholecystic fluid (5 patients each from the early and delayed laparoscopic cholecystectomy groups), and intrahepatic (1 patient in the early and 3 patients in the delayed laparoscopic cholecystectomy groups) and extrahepatic (1 patient in the early laparoscopic cholecystectomy group) bile duct dilatation. Ultrasonographic findings were similar between groups (Table 2).
Table 2.
Physical, laboratory, and radiologic findings of patients in the early and delayed laparoscopic cholecystectomy groupsa
Intraoperative and postoperative findings
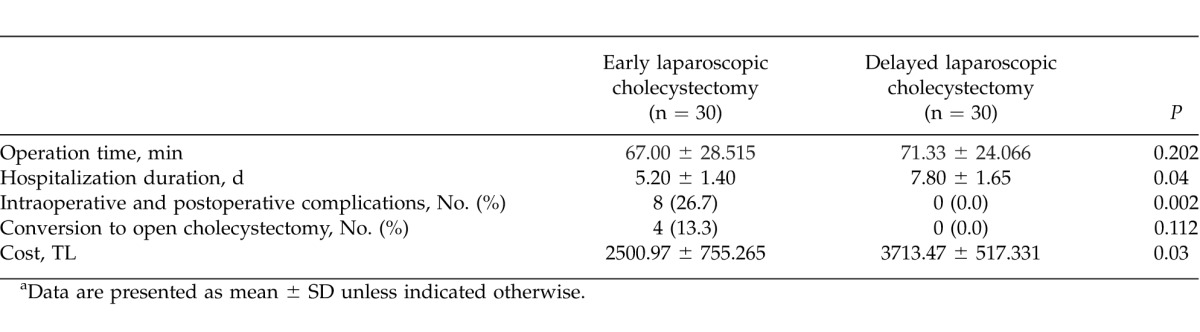
There was no significant difference between the early and the delayed laparoscopic cholecystectomy groups in terms of operation time and rates for conversion to open cholecystectomy (Table 3). On the other hand, total hospital stay was longer (5.2 ± 1.40 versus 7.8 ± 1.65 days; P = 0.04) and total costs were higher (2500.97 ± 755.265 versus 3713.47 ± 517.331 TL; P = 0.03) in the delayed laparoscopic cholecystectomy group than in the early laparoscopic cholecystectomy group. Intraoperative and postoperative complications were recorded in 8 patients in the early laparoscopic cholecystectomy group, whereas no complications occurred in the delayed laparoscopic cholecystectomy group (P = 0.002; Table 3). Of these complications, 3 were intraoperative—bile duct injury, bleeding, and gallbladder perforation—and 5 were postoperative—lung infection, atelectasis, surgical site infection, bleeding from umbilical trocar site, and leakage from a Luschka canal.
Table 3.
Intraoperative and postoperative findings of patients in the early and delayed laparoscopic cholecystectomy groupsa
Discussion
In this prospective, randomized study, we confirmed that early laparoscopic cholecystectomy has the advantage of shorter hospital stay and lower cost compared with delayed laparoscopic cholecystectomy for the treatment of acute cholecystitis due to gallstones.
In the past, the optimal timing for laparoscopic cholecystectomy for patients with acute cholecystitis had generally been considered to be 6 to 8 eight weeks after the acute phase to allow for resolution of the acute inflammation of the gallbladder.8 However, several clinical trials—albeit mostly small and retrospective studies—proved that early laparoscopic cholecystectomy is safe and shortens hospital stay, with morbidity and mortality similar to those of elective delayed cholecystectomy.2,4,8,9,11 In a retrospective analysis of 100 patients, Ohta et al11 compared 4 timing groups of laparoscopic cholecystectomy (≤72 hours, 4–14 days, 3–6 weeks, and >6 weeks after onset of symptoms) and found that the best timing for laparoscopic cholecystectomy for acute cholecystitis is within 72 hours, which provides the shortest total hospital stay versus operations performed later. Falor et al8 performed early laparoscopic cholecystectomy (within 48 hours of admission) in 117 of 303 patients with mild gallstone pancreatitis; for the rest of the patients, operation was delayed until the normalization of laboratory values. They suggested that early laparoscopic cholecystectomy is safe, resulting in shortened hospital stay and decreased use of endoscopic retrograde cholangiopancreatography without increased morbidity and mortality. Chang et al4 reported that although early laparoscopic cholecystectomy is associated with a higher rate of wound infections compared with delayed intervention, it shortens the length of hospital stay and reduces the risk of repeat cholecystitis. In a randomized, controlled trial including 75 patients, early laparoscopic cholecystectomy (<24 hours) was found to decrease the morbidity during the waiting period for elective laparoscopic cholecystectomy, the rate of conversion to open cholecystectomy, operating time, and hospital stay.12 In a recent survey evaluating surgical approaches for acute gallbladder disease between 1989 and 2006 in Sweden, total hospital stay was found to be shorter for patients who had emergency cholecystectomy at first admission compared with patients with elective cholecystectomy.7
Similar to the above clinical studies, we found that hospitalization duration was significantly shorter and treatment-related costs were lower with early laparoscopic cholecystectomy compared with delayed laparoscopic cholecystectomy for acute cholecystitis. Furthermore, operation time and conversion rate were comparable between groups. It should be noted that physical, clinical, and radiologic characteristics of patients in both study groups were similar in our study, except for body temperature and blood direct/conjugated bilirubin level, which were significantly higher in the early laparoscopic cholecystectomy group.
In addition to the clinical studies, the meta-analyses of randomized clinical trials in the literature demonstrated that early laparoscopic cholecystectomy (24–72 hours of onset) provides benefit over delayed laparoscopic cholecystectomy (6–12 weeks later) in terms of total hospital stay, with conflicting results on conversion rates and postoperative complications.5,13–15 Siddiqui et al14 analyzed 4 clinical studies containing 375 patients and found shorter hospital stay and longer operation time in early laparoscopic cholecystectomy, but they found no significant difference in conversion rates between early and delayed laparoscopic cholecystectomy. In a best-evidence topic that analyzed 92 papers (meta-analyses, randomized control trials, prospective controlled study, and retrospective cohort studies), it was concluded that early laparoscopic cholecystectomy for acute cholecystitis is advantageous in terms of the length of hospital stay without increases in morbidity or mortality.15 Although the operating time in early laparoscopic cholecystectomy can be longer, the incidence of serious complications was found to be comparable to the delayed laparoscopic cholecystectomy. In the present study, similar to the findings of studies showing a high rate of wound infections and complications with early laparoscopic cholecystectomy, we found that intraoperative and postoperative complications were more common with early than delayed laparoscopic cholecystectomy. The higher rate of complications in the early laparoscopic cholecystectomy group may also be explained by the significantly higher initial body temperatures and blood direct/conjugated bilirubin levels in this group. However, considering the shorter hospitalization duration and lower treatment costs, early laparoscopic cholecystectomy still seems advantageous over late intervention.
We believe that inflammation associated with acute cholecystitis creates an edematous plane around the gallbladder, thus facilitating its dissection from the surrounding structures. Maturation of the surrounding inflammation, and thus organization of the adhesions, leading to scarring and contraction, occurs during the cool-down period.
A few recent studies have compared the costs of early and delayed laparoscopic cholecystectomy. In a decision-tree model on the cost-utility of early versus delayed laparoscopic cholecystectomy for acute cholecystitis, Wilson et al16 showed that early laparoscopic cholecystectomy is less costly and results in better quality of life. Another decision analytic model from Canada confirmed the better patient quality of life and substantial cost savings in association with early laparoscopic cholecystectomy.17 On the other hand, in a randomized, controlled trial of 72 patients, the cost-utility of early and elective laparoscopic cholecystectomies was found to be similar.2 In the present study, we showed that treatment-related costs were lower in the early laparoscopic cholecystectomy group. However, this may be due to a shorter hospitalization duration and lack of conservative treatment in early laparoscopic cholecystectomy.
The present study had some limitations. The sample size was considerably small, and cost analysis was not based on a systematic decision model. In spite of these limitations, this was the first prospective randomized study from Turkey comparing early versus delayed laparoscopic cholecystectomy for acute cholecystitis, which is among the most common operations in surgical practice. The findings of this study should provide a basis for larger-scale clinical studies and further cost analysis.
In conclusion, although intraoperative and postoperative complications are associated more with early laparoscopic cholecystectomy compared with delayed intervention, early laparoscopic cholecystectomy should be preferred by surgeons for treatment of acute cholecystitis with the advantage of shorter hospital stay and lower cost.
References
- 1.Kolla SB, Aggarwal S, Kumar A, Kumar R, Chumber S, Parshad R, et al. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a prospective randomized trial. Surg Endosc. 2004;18(9):1323–1327. doi: 10.1007/s00464-003-9230-6. [DOI] [PubMed] [Google Scholar]
- 2.Macafee DAL, Humes DJ, Bouliotis G, Beckingham IJ, Whynes DK, Lobo D. Prospective randomized trial using cost-utility analysis of early versus delayed laparoscopic cholecystectomy for acute gallbladder disease. Br J Surg. 2009;96(9):1031–1040. doi: 10.1002/bjs.6685. [DOI] [PubMed] [Google Scholar]
- 3.Cuschieri A. Approach to the treatment of acute cholecystitis: open surgical, laparoscopic or endoscopic? Endoscopy. 1993;25(6):397–398. doi: 10.1055/s-2007-1010349. [DOI] [PubMed] [Google Scholar]
- 4.Chang TC, Lin MT, Wu MH, Wang MY, Lee PH. Evaluation of early versus delayed laparoscopic cholecystectomy in the treatment of acute cholecystitis. Hepatogastroenterology. 2009;56(89):26–28. [PubMed] [Google Scholar]
- 5.Gurusamy K, Samraj K, Gluud C, Wilson E, Davidson BR. Meta-analysis of randomized controlled trials on the safety and effectiveness of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. 2010;97(2):141–150. doi: 10.1002/bjs.6870. [DOI] [PubMed] [Google Scholar]
- 6.Miura F, Takada T, Strasberg SM, Solomkin JS, Pitt HA, Gouma DJ, et al. TG13 flowchart for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2013;20(1):47–54. doi: 10.1007/s00534-012-0563-1. [DOI] [PubMed] [Google Scholar]
- 7.Sandzen B, Haapamaki MM, Nilsson E, Stenlund HC, Oman M. Surgery for acute gallbladder disease in Sweden 1989–2006 - a register study. Scand J Gastroenterol. 2013;48(4):480–486. doi: 10.3109/00365521.2012.763177. [DOI] [PubMed] [Google Scholar]
- 8.Falor AE, de Virgilio C, Stabile BE, Kaji AH, Caton A, Kokubun BA, et al. Early laparoscopic cholecystectomy for mild gallstone pancreatitis: time for a paradigm shift. Arch Surg. 2012;147(11):1031–1035. doi: 10.1001/archsurg.2012.1473. [DOI] [PubMed] [Google Scholar]
- 9.Panagiotopoulou IG, Carter N, Lewis MC, Rao S. Early laparoscopic cholecystectomy in a district general hospital: is it safe and feasible? Int J Evid Based Health. 2012;10(2):112–116. doi: 10.1111/j.1744-1609.2012.00260.x. [DOI] [PubMed] [Google Scholar]
- 10.Sankarankutty A, da Luz LT, De Campos T, Rizoli S, Fraga GP, Nascimento B., Jr Uncomplicated acute cholecystitis: early or delayed laparoscopic cholecystectomy? Rev Col Bras Cir. 2012;39(5):436–440. doi: 10.1590/s0100-69912012000500017. [DOI] [PubMed] [Google Scholar]
- 11.Ohta M, Iwashita Y, Yada K, Ogawa T, Kai S, Ishio T, et al. Operative timing of laparoscopic cholecystectomy for acute cholecystitis in a Japanese institute. JSLS. 2012;16(1):65–70. doi: 10.4293/108680812X13291597716023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gurusamy KS, Samraj K, Fusai G, Davidson BR. Early versus delayed laparoscopic cholecystectomy for biliary colic. Cochrane Database Syst Rev. 2008 doi: 10.1002/14651858.CD007196.pub2. 4):CD007196. [DOI] [PubMed] [Google Scholar]
- 13.Lau H, Lo CY, Patil NG, Yuen WK. Early versus delayed-interval laparoscopic cholecystectomy for acute cholecystitis: a metaanalysis. Surg Endosc. 2006;20(1):82–87. doi: 10.1007/s00464-005-0100-2. [DOI] [PubMed] [Google Scholar]
- 14.Siddiqui T, MacDonald A, Chong PS, Jenkins JT. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a meta-analysis of randomized clinical trials. Am J Surg. 2008;195(1):40–47. doi: 10.1016/j.amjsurg.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 15.Skouras C, Jarral O, Deshpande R, Zografos G, Habib N, Zacharakis E. Is early laparoscopic cholecystectomy for acute cholecystitis preferable to delayed surgery?: best evidence topic (BET) Int J Surg. 2012;10(5):250–258. doi: 10.1016/j.ijsu.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 16.Wilson E, Gurusamy K, Gluud C, Davidson BR. Cost-utility and value-of-information analysis of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. 2010;97(2):210–219. doi: 10.1002/bjs.6872. [DOI] [PubMed] [Google Scholar]
- 17.Johner A, Raymakers A, Wiseman SM. Cost-utility of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Surg Endosc. 2013;27(1):256–262. doi: 10.1007/s00464-012-2430-1. [DOI] [PubMed] [Google Scholar]


