Abstract
With loss of renal function and decreasing glomerula filtration rate the serum levels of 25-hydroxyvitamin D [25(OH)D] as well as 1,25-dihydroxyvitamin D [1,25 (OH)2 D] often decrease simultaneously. In representative groups of German patients on renal replacement therapy (hemodialysis, peritoneal dialysis, kidney transplantation) our group retrospectively analyzed the vitamin D status over a period of 12 y (1995‒2006). Only 11% of patients had a serum level of 25(OH)D that was > 30 ng/ml, more than 70% had a level of 25(OH)D < 20 ng/ml. In clinical trials we used sun-simulating artificial lamps to produce vitamin D3 in the skin. Partial-body irradiation (15% of body surface) was used during the routine hemodialysis treatment. Whole-body UV exposure was done in a standing position three times a week before the hemodialysis treatment. With both procedures we observed an increase of the serum level of 25(OH)2D3 by approx. 35–50% over a period of 2‒3 mo, maintenance of trabecular bone mineral density and a normalization of systolic and diastolic blood pressure. Heart rate variability improved during the whole-body radiation intervention period by 20‒25%. Patients who continued the whole-body irradiation regularly two or three times before starting the routine hemodialysis session had maintained normal levels of circulating 25(OH)D3 and of 1,25(OH)2D3. Therefore, from our data it can be recommended that intermittent suberythemal UVB exposure with a sun-simulation spectrum is effective to treat and/or protect against vitamin D deficiency in chronic and end-stage kidney disease patients.
Keywords: chronic kidney disease; vitamin D3; 25-Hydroxyvitamin D; 1,25-Dihydroxyvitamin D; bone mineral density; hypertension
Introduction
Normal kidney function is required for the maintenance of sufficient serum levels of 1,25(OH)2D. 25-hydroxyvitamin D3 [25(OH)D3, caldiol] is the precursor for the activation to 1,25-dihydroxyvitamin D [1,25(OH)2D3, calcitriol] in numerous non-renal cells and in the renal proximal tubular cell by the 1-α-hydroxylase. With loss of renal function and decreasing glomerula filtration rate the serum levels of 25(OH)D as well as 1,25(OH)2D decrease simultaneously because the endocytotic receptor megalin reduces the uptake of 25(OH)D from the vitamin D-binding protein (DBP) and the uptake of 25(OH)D3 from the glomerular ultrafiltrate.1Therefore the KDIGO Clinical Practice Guidelines recommend that for holding a normal status of vitamin D a serum level of 25(OH)D < 20‒32 ng/ml should be corrected using the same treatment strategies recommended for the general population2-4. As in the general population and in patients with CKD and ESKD there is an association of low 25(OH)D serum levels with increasing mortality.5-7
Vitamin D status in German Patients on Renal Replacement Therapy
Renal replacement therapy (RRT) has been established for more than 50 y, and the main focus is to prolong a high quality of life with a low rate of comorbidities. Up to now the majority of patients are older than 65 y, and the major consequences of RRT are essential hypertension, diabetes mellitus type II and metabolic syndrome.3,4 For these primary renal diseases vitamin D deficiency is a major risk factor.
In representative groups of patients on renal replacement therapy (hemodialysis, peritoneal dialysis, kidney transplantation) our group retrospectively analyzed the vitamin D status over a period of 12 y (1995‒2006).8-10 Only 11% of patients had a serum level of 25(OH)D > 30 ng/ml, whereas more than 70% had a level of 25(OH)D < 20 ng/ml. Over the 12 y period an increase of the median of serum level of 25(OH)D from 8.5 ng/ml to 21.0 ng/ml was seen9 (Fig. 1). Patients with Diabetes mellitus type I (50%), Diabetes mellitus type II (70%), patients with hypertensive nephropathy (42%) and with immune-systemic diseases (48%) had severe deficiency of 25(OH)D < 12.5 ng/ml.8
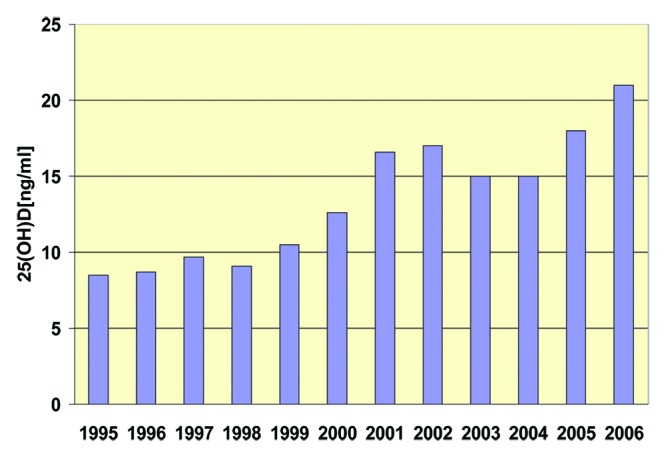
Figure 1. Vitamin D Status of German Hemodialysis Patients (Medians over the time course 1995 – 2006)
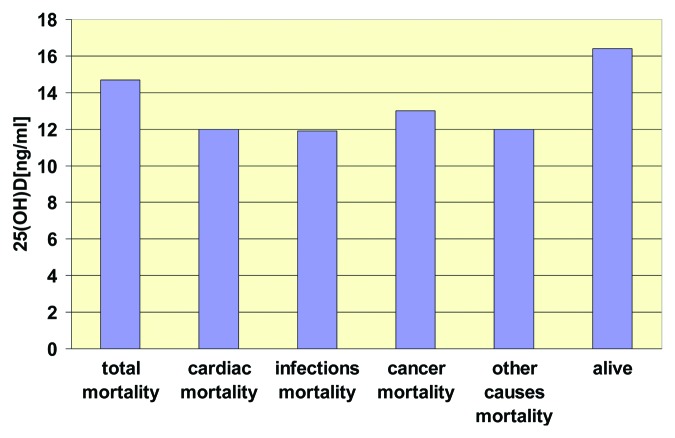
As reported for the general population the typical seasonal variation of the vitamin D status was observed in patients on renal replacement therapy and also in patients on hemo-dialysis.11-19 The KDIGO group2-4 reported a correlation between vitamin D status and mortality8,10 (Fig. 2) Also for mortality there was a seasonal variation with the highest rates during winter and early springtime and the lowest rates during summer and the early autumn months.20-27
Figure 2. Vitamin D Status and Mortality in German Hemodialysis Patients (Medians over the time course 1995–2006)
Exposure to UV Radiation in End-Stage Kidney Disease (ESKD) Patients
Treatment with vitamin D metabolites and analoges was been used nearly as long as chronic dialysis therapy was established. Due to the main goal of suppressing secondary hyperparathyroidism for improving renal bone disease the medication 1,25(OH)2D3, calcitriol was introduced in the early 1970s. Within the past 20 y it has become evident that many organs can synthesize 1,25(OH)2D3 by an autocrine mode via local activation of circulating 25(OH)D3 to 1,25(OH)2D3.13
The major source of vitamin D comes from exposure of the skin to sunlight and UV-B exposure.13,19 The capacity of the skin to produce vitamin D3 is dependent on skin pigmentation, latitude, season of the year and time of the day.19 Additionally, aging and alterations of the skin due to uremia with increased pigmentation and hyperkeratosis reduces the capacity of the skin to produce vitamin D3 when compared with younger and healthy people. It is well known that the skin itself is not only able to convert 7-dehydrocholesterol (7-DHC) to vitamin D3 (cholecalciferol), but is also able to convert vitamin D3 to 25(OH)D3 as well as to the hormonal active metabolite 1,25(OH)2D3 by cutenaous 25-hydroxylase [CYP27A, 1/CYP2R1] and 1-α-hydroxylase [CYP27B1], respectively.28-36 -
Therefore the hypothesis of our group was to expose the skin of ESKD patients to UVB radiation to improve serum levels of 25(OH)D and at the same time have the skin also produce 25(OH)D3 from cutaneous vitamin D which in turn could be converted in the skin to 1,25(OH)2D3.37-44 Moreover, the activation of the whole vitamin D metabolic pathway due to UV irradiation could additionally improve the residual capacity of the endocrine function of the kidneys in CKD patients to produce more of 1,25(OH)2D3 . Patients with advanced kidney disease stages 3–5 have been reported to need supra-physiological serum levels of > 100–250 ng/ml for converting 25(OH)D3 extra-renally to 1,25(OH)2D3.43
It is also known that in patients who were anephric had detectable serum levels of 1,25(OH)2D3.31
Medical Heliotherapy in ESKD Patients
For our clinical trials we used sun-simulating artificial lamps with two different procedures.
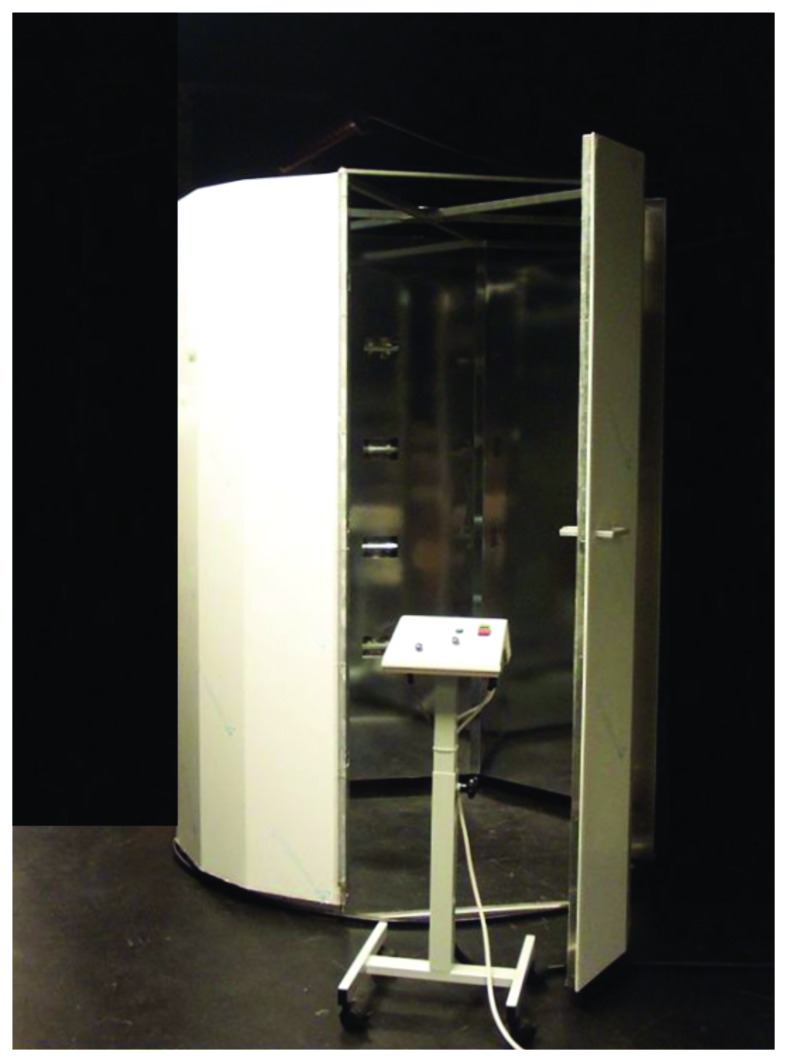
One procedure was partial-body irradiation during the routine hemodialysis treatment.48 We used a tripod-leg-based UV-device (Fig. 3) for irradiating only the ventral part of the legs (e.g., approximately 15% of body surface) with fluorescent lamps (FL) and an UVB output of approx. 3.5%.46,48 Whole-body UV exposure (Fig. 4) was done in a standing position three times a week before the hemodialysis treatment. The halogen lamps had an UVB output of ~11%, and there was a gap of 14 percent between EVitD and Eerythema for safe sub-erythemal activation of the vitamin D production in the skin; this gap we called the “Therapeutic Window”45-47. With both procedures we calculated a nonlinear correlation of the vitamin D weighted irradiance dose and the serum level of 25(OH)D3.46
Figure 3. Partial-body UV irradiation during a routine hemodialysis session (from 46, with permission)
Figure 4. Sun-simulating UV irradiation cabin (from 46, with permission)
During six months of the whole-body irradiation the medians of all vitamin D metabolites (vitamin D3, 25(OH)D3, 1,25(OH)2D3) increased, but with different time courses. Vitamin D3 increased 6-fold after seven weeks from 6 ng/ml to 36 ng/ml, and thereafter a stable plateau was observed over the following months. 25(OH)D3 increased continuously over the six month period by 100% from 43 ng/ml to 86 ng/ml and 1,25(OH)2D3 increased after seven weeks by 48% from 21 pg/ml to 33 pg/ml remaining stable within the normal range over the following time45. (Fig. 5) After partial-body irradiation we observed an increase of 25(OH)D levels reaching its maximum after ten weeks by ~36% from 25 ng/ml to 39 ng/ml.
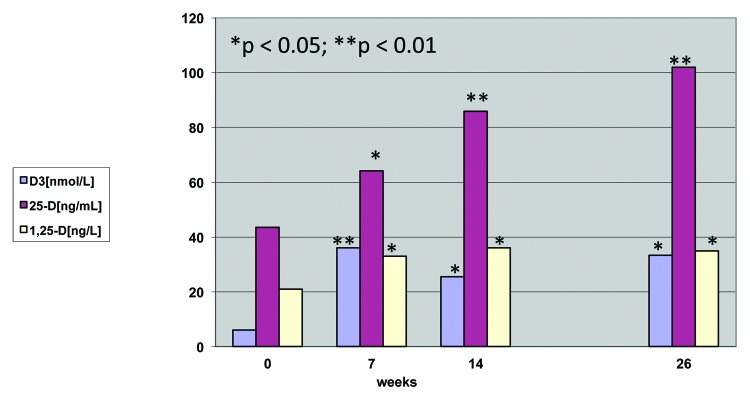
Figure 5. Vitamin D Metabolite Levels in Hemodialysis Patients after Whole-Body UV Irradiation
The serum level of circulating 1,25(OH)2D3 increased by 48% after 14 weeks from 10 pg/ml to 19 pg/ml remaining stable thereafter.46,48 (Fig. 6)
Figure 6. Vitamin D Metabolite Levels in Hemodialysis Patients after Partial-Body Irradiation (approx. 15% of Body Surface)
Whole-body irradiation was able to increase the serum level of 25(OH)D3 by ~50–65% over a period of 3–6 mo.45,46 Moreover, as documented in healthy people, regular partial-body UVB exposure of only ~15% of body surface was sufficient to guarantee a high-normal serum levels of 25(OH)D3 and was comparable with whole-body exposure. The exposures mimic the action of the natural sun producing previtamin D3 in the skin which converts to vitamin D3.19 Once formed it is converted in the liver to 25(OH)D3 which in turn is converted in the kidneys and by activated monocytes and possibly by keratinocytes to 1,25(OH)2D331,34,43.
The accumulation of each suberythemal radiation led to a total of 15–35 MEDII over the period of 2–3.5 mo, which is equal to between one-sixth and one-third of the recommended minimal erythemal dose per person over one year.46
Skeletal and Cardiocirculatory Effects of UV Exposure in ESKD Patients
Renal bone disease and bone mineral density (BMD)
Renal osteodystrophy and extraskeletal calcification are very frequent in CKD and ESKD patients. The established treatment is oral and/or intravenous active vitamin D. But, important side-effects are hypercalcemia and /or hyperphosphatemia. Therefore a vitamin D therapy without these side-effects is needed.
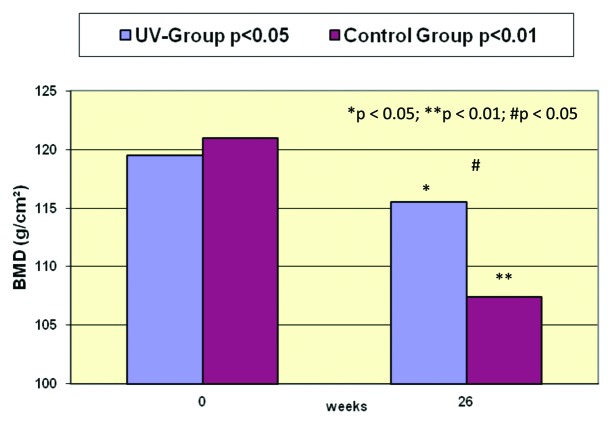
Before and after six months of whole-body exposure to UV radiation there was only a small decrease of 3.5% in the trabecular bone mass in comparison with 11% in the non-irradiated and non-treated control group.50-52 (Fig. 7) This is agreement with the literature reporting a decrease of BMD by ~3% over six months in patients treated with 1,25(OH)2D3 or analogs.54-62
Figure 7. Trabecular Bone Mineral Density (DE-QCT) of Hemodialysis Patients before and after 6 Months of Whole-Body UV Irradiation
Blood pressure regulation
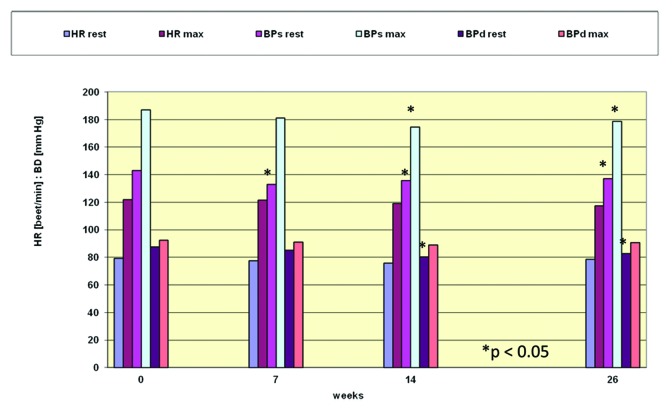
About 50 percent of patients with ESKD suffer from essential hypertension and/or diabetes mellitus type II and metabolic syndrome.63,64 Left ventricular hypertrophy, coronary heart disease and cardiomyopathy are very frequent co-morbidities in CKD and ESKD patients. After seven and 14 weeks of UVB exposure systolic and diastolic blood pressure decreased significantly at rest and also after maximum ergometric work load (Fig. 8). This was comparable with the maximum increases of circulating 25(OH)D3 and 1,25(OH)2D3. There was a decrease of resting heart rate of 3% and a significant reduction of systolic and diastolic blood pressure of 8% and 4%, respectively.47,49 This is also in line with the well-known seasonal and geographic differences of blood pressure with a decrease during summertime and and increase with higher latitude.65-68
Figure 8. Heart Rate, Systolic and Diastolic Blood Pressure at Rest and at Maximal Work Load of Hemodialysis Patients before and after 6 Months of Whole-Body UV Irradiation
Work load capacity
The physical capacity of CKD patients decrease due to, e.g., uremic myopathy, polyneuropathy or metabolic acidosis. Vitamin D deficiency also leads to muscle weakness and to a decrease of muscle strength and coordination. Confirming previous findings from our group and from the literature in healthy people and in cardiac patients submaximal and maximal ergometric work load increased significantly in the group exposed to UV radiation.47,49,53 After three months of serial UVB irradiation we found a significant increase of work load by 6% in the bicycle ergometer test, with a significant increase in oxygen uptake of 11% and a reduction of the accumulation of lactic acid of 9%.46
Heart rate variability
In dialysis patients the rate of cardiac death is more than doubled in comparison with the general population, and often they die from sudden death. The uremic neuropathy may be one risk factor for an increase of the sympathetic tone, and heart rate variability (HRV) is one marker of the sympathetic-parasympathetic balance.46,69-71
During the whole-body UV radiation intervention period we found an increase of the medians of the RR-interval time in ECG by 20% and of the means of the standard deviation of the RR-intervals (beat-to-beat difference) by 25%.46 (Fig. 9) These are measures of the cardiocirculatory rhythmicity and shows that the neuropatic induced stiffness of the heart frequency distribution decreased. The improvement of these parameters of HRV was observed at the time when the serum level of 1,25(OH)2D3 reached its maximum. Therefore serial sun(-like) UV exposure can improve the parasympathetic tone and can protect from arrhythmic dysregulation of the heart. Therefore UV exposure improved the cardio-circulatory adaptation in an equal manner as endurance training.69
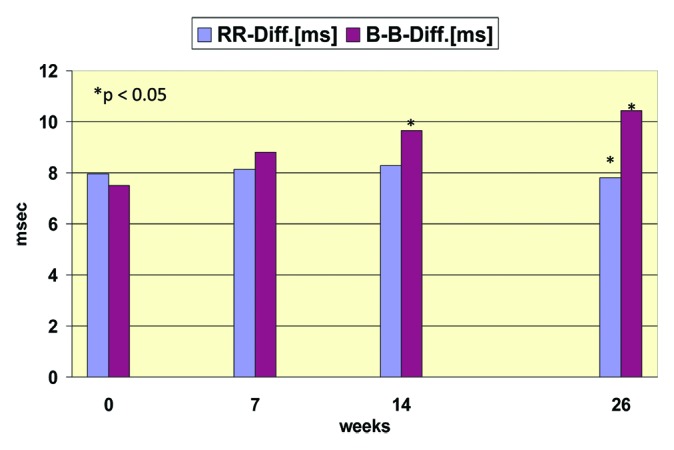
Figure 9. Heart Rate Variability (ECG-RR-Differences and SD(dRR)) of Hemodialysis Patients before and after 6 Months of Whole-Body UV Irradiation
Use of UVB radiation in Our Dialysis Unit
Following the clinical trials we had implemented serial UV-B irradiation for the treatment of the renal vitamin D deficiency instead of treatment with vitamin D3 orally and/or 1,25(OH)2D3 intravenously over the past 15 y in our dialysis unit.46
A number of patients were exposed intermittently to suberythemal whole-body UV-B radiation regularly two or three times before their routine hemodialysis session. These patients hold normal levels of circulating 25(OH)D3 (mean serum levels: 45.3 ng/ml) and also normal level of circulating 1,25(OH)2D3 (mean serum levels: 30.4 pg/ml).
Conclusion
The vitamin D deficiency in CKD patients and especially in patients on dialysis is an independent risk factor for the function of many organs and/or metabolic and enzymatic pathways, as well as for the overall and cardiovascular mortality. Additionally impairment of the vitamin D metabolism due to CKD causes a reduction of the physical capacity and multiple co-morbidities. People with renal insufficiency often are also sun deprived.72-76
As recommended in the K/DOQI guidelines improvement in vitamin D status can result to non-calcemic benefits of vitamin D by the autocrine production of 1,25(OH)2D3 . The K/DOQI guidelines recommend to normalize the basal vitamin D status.- The traditional therapy still used today in nephrology is the use of active vitamin D metabolites to treat secondary hyperparathyroidism. But, using active vitamin D metabolites however can have side-effects causing hypercalcemia, hyperphosphatemia and vascular calcification.2,3 Therefore our aim was to use the extrarenal capacity of the monocytes and possibly of the skin to produce 1,25(OH)2D3. From our results uremic skin is able to produce a sufficient amount of vitamin D3 which is metabolized in the liver to 25(OH)D or possibly by the skin and/or other organs and cells to both 25(OH)D and 1,25(OH)D2, then sending it into the circulation and stimulating the well-known positive protective effects in bone, blood pressure regulation, heart rate rhythmicity, as well as on muscle metabolism and physical capacity.From our data it can be recommended that intermittent suberythemal UVB exposure with a sun-simulation spectrum to treat and/or protect the vitamin D deficiency in chronic and end-stage kidney disease patients. We had found no (major) side effects from this therapy over the past 20 y.
Therefore, regular outdoor sun exposure during summertime (April to September / October in latitudes > 45° N/S) and / or serial suberythemal sun-simulating UV-B irradiation should also be recommended as measures of prevention and treatment of patients with all stages of chronic kidney disease.
Glossary
Abbreviations:
- UV
Ultraviolet
- DE-QCT
Double-Electron Quantitative Computed Tomography
- ECG
Electrocardiography
- RR
Interval of successive R’s
- R
Peak of the QRS Complex of ECG
- B-B-Diff
SD(dRR), standard deviation of RR intervals
- HR
Heart Rate
- BP
Blood Pressure
- BPs
systolic BP
- BPd
diastolic BP
- max
maximum Work Load
Disclosure of Potential Conflicts of Interest
No potential conflict of interest was disclosed.
Footnotes
Previously published online: www.landesbioscience.com/journals/dermatoendocrinology/article/24539
References
- 1.Dusso AS. Kidney disease and vitamin D levels: 25-hydroxyvitamin D, 1,25-dihydroxyvitamin D, and VDR activation. Kidney Inter Suppl. 2011;1:136–41. doi: 10.1038/kisup.2011.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Kidney Foundation K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003;42(Suppl 3):S1–201. doi: 10.1016/S0272-6386(03)00905-3. [DOI] [PubMed] [Google Scholar]
- 3.Kidney Disease. Improving Global Outcomes (KDIGO) CKD-MBD Work Group KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease- Mineral and Bone Disorder (CKD-MBD) Kidney Int. 2009;113:S1–130. doi: 10.1038/ki.2009.188. [DOI] [PubMed] [Google Scholar]
- 4.Kidney Disease. Improving Global Outcomes (KDIGO) CKD-MBD Work Group KDIGO clinical practice guideline for the evaluation and management of Chronic Kidney Disease. Kidney Int Suppl. 2013;3:1–163. doi: 10.1038/kisup.2012.73. [DOI] [PubMed] [Google Scholar]
- 5.Wolf M, Shah A, Gutierrez O, Ankers E, Monroy M, Tamez H, et al. Vitamin D levels and early mortality among incident hemodialysis patients. Kidney Int. 2007;72:1004–13. doi: 10.1038/sj.ki.5002451. [DOI] [PubMed] [Google Scholar]
- 6.Krause R, Roth HJ, Edenharter G. Vitamin D deficiency and cardiac mortality in patients on renal replacement therapy (RRT) J Am Soc Nephrol. 2008;19:74A. [Google Scholar]
- 7.Jean G, Souberbielle JC, Chazot C. Monthly cholecalciferol administration in haemodialysis patients: a simple and efficient strategy for vitamin D supplementation. Nephrol Dial Transplant. 2009;24:3799–805. doi: 10.1093/ndt/gfp370. [DOI] [PubMed] [Google Scholar]
- 8.Schober-Halstenberg HJ. Vitamin-D-Status (25(OH)D3) und Mortalität von Hämodialysepatienten. [MD-Thesis]. Berlin: Charité 2010. [Google Scholar]
- 9.Krause R, Roth HJ, Haas K, Edenharter G, Schober-Halstenberg HJ. Vitamin-D-Status bei terminal Nierenkranken in Deutschland. Nieren- Hochdruckkr. 2008;37:463. [Google Scholar]
- 10.Krause R, Schober-Halstenberg HJ, Edenharter G, Haas K, Roth HJ, Frei U. Vitamin D status and mortality of German hemodialysis patients. Anticancer Res. 2012;32:391–5. [PubMed] [Google Scholar]
- 11.Hollis BW. Assessment of vitamin D status and definition of a normal circulating range of 25-hydroxyvitamin D. Curr Opin Endocrinol Diabetes Obes. 2008;15:489–94. doi: 10.1097/MED.0b013e328317ca6c. [DOI] [PubMed] [Google Scholar]
- 12.Heaney RP. Optimal vitamin D status. J Bone Miner Res. 2009;24:755–, author reply 756. doi: 10.1359/jbmr.081219. [DOI] [PubMed] [Google Scholar]
- 13.Holick MF. Vitamin D for health and in chronic kidney disease. Semin Dial. 2005;18:266–75. doi: 10.1111/j.1525-139X.2005.18402.x. [DOI] [PubMed] [Google Scholar]
- 14.Tentori F, Hunt WC, Stidley CA, Rohrscheib MR, Bedrick EJ, Meyer KB, et al. Medical Directors of Dialysis Clinic Inc Mortality risk among hemodialysis patients receiving different vitamin D analogs. Kidney Int. 2006;70:1858–65. doi: 10.1038/sj.ki.5001868. [DOI] [PubMed] [Google Scholar]
- 15.Stavroulopoulos A, Cassidy MJ, Porter CJ, Hosking DJ, Roe SD. Vitamin D status in renal transplant recipients. Am J Transplant. 2007;7:2546–52. doi: 10.1111/j.1600-6143.2007.01978.x. [DOI] [PubMed] [Google Scholar]
- 16.Del Valle E, Negri AL, Aguirre C, Fradinger E, Zanchetta JR. Prevalence of 25(OH) vitamin D insufficiency and deficiency in chronic kidney disease stage 5 patients on hemodialysis. Hemodial Int. 2007;11:315–21. doi: 10.1111/j.1542-4758.2007.00186.x. [DOI] [PubMed] [Google Scholar]
- 17.Chandra P, Binongo JN, Ziegler TR, Schlanger LE, Wang W, Someren JT, et al. Cholecalciferol (vitamin D3) therapy and vitamin D insufficiency in patients with chronic kidney disease: a randomized controlled pilot study. Endocr Pract. 2008;14:10–7. doi: 10.4158/EP.14.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tokmak F, Quack I, Schieren G, Sellin L, Rattensperger D, Holland-Letz T, et al. High-dose cholecalciferol to correct vitamin D deficiency in haemodialysis patients. Nephrol Dial Transplant. 2008;23:4016–20. doi: 10.1093/ndt/gfn367. [DOI] [PubMed] [Google Scholar]
- 19.Holick MF. Photosynthesis of vitamin D in the skin: effect of enviromental and life-style variables. Fed Proc. 1987;146:1876–82. [PubMed] [Google Scholar]
- 20.Simon JA. Review: vitamin D supplementation decreases all-cause mortality in adults and older people. Evid Based Med. 2008;13:47. doi: 10.1136/ebm.13.2.47. [DOI] [PubMed] [Google Scholar]
- 21.Halloran BP, Schaefer P, Lifschitz M, Levens M, Goldsmith RS. Plasma vitamin D metabolite concentrations in chronic renal failure: effect of oral administration of 25-hydroxyvitamin D3. J Clin Endocrinol Metab. 1984;59:1063–9. doi: 10.1210/jcem-59-6-1063. [DOI] [PubMed] [Google Scholar]
- 22.Noordzij M, Korevaar JC, Boeschoten EW, Dekker FW, Bos WJ, Krediet RT, Netherlands Cooperative Study on the Adequacy of Dialysis (NECOSAD) Study Group The Kidney Disease Outcomes Quality Initiative (K/DOQI) Guideline for Bone Metabolism and Disease in CKD: association with mortality in dialysis patients. Am J Kidney Dis. 2005;46:925–32. doi: 10.1053/j.ajkd.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 23.Tentori F, Albert JM, Young EW, Blayney MJ, Robinson BM, Pisoni RL, et al. The survival advantage for haemodialysis patients taking vitamin D is questioned: findings from the Dialysis Outcomes and Practice Patterns Study. Nephrol Dial Transplant. 2009;24:963–72. doi: 10.1093/ndt/gfn592. [DOI] [PubMed] [Google Scholar]
- 24.Wolf M, Shah A, Gutierrez O, Ankers E, Monroy M, Tamez H, et al. Vitamin D levels and early mortality among incident hemodialysis patients. Kidney Int. 2007;72:1004–13. doi: 10.1038/sj.ki.5002451. [DOI] [PubMed] [Google Scholar]
- 25.Naves-Díaz M, Alvarez-Hernández D, Passlick-Deetjen J, Guinsburg A, Marelli C, Rodriguez-Puyol D, et al. Oral active vitamin D is associated with improved survival in hemodialysis patients. Kidney Int. 2008;74:1070–8. doi: 10.1038/ki.2008.343. [DOI] [PubMed] [Google Scholar]
- 26.Wolf M, Betancourt J, Chang Y, Shah A, Teng M, Tamez H, et al. Impact of activated vitamin D and race on survival among hemodialysis patients. J Am Soc Nephrol. 2008;19:1379–88. doi: 10.1681/ASN.2007091002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kovesdy CP, Kalantar-Zadeh K. Vitamin D receptor activation and survival in chronic kidney disease. Kidney Int. 2008;73:1355–63. doi: 10.1038/ki.2008.35. [DOI] [PubMed] [Google Scholar]
- 28.Krause R, Matulla B, Chen TC, Regular UV. B)-irradiation. An effective way to normalize calcitriol deficiency in hemodialysis patients. Clin Lab (Zaragoza) 1996;42:305–7. [Google Scholar]
- 29.Krause R, Matulla B, Albrecht C. UVB can normalize Vitamin D, 25 (OH) D3 and calcitriol in ESRD patients without side effects: Result of extrarenal synthesis of 1,25 (OH2) D3. J Am Soc Nephrol. 1999;10:621A. [Google Scholar]
- 30.Krause R, Matulla B, Albrecht C. UVB can normalize Vitamin D, 25 (OH) D3 and calcitriol in ESRD patients without side effects: Result of extrarenal synthesis of 1,25 (OH2) D3. J Am Soc Nephrol. 1999;10:621A. [Google Scholar]
- 31.Lambert PW, Stern PH, Avioli RC, Brackett NC, Turner RT, Greene A, et al. Evidence for extrarenal production of 1 α, 25-dihydroxyvitamin D in man. J Clin Invest. 1982;69:722–5. doi: 10.1172/JCI110501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jones G. Expanding role for vitamin D in chronic kidney disease: importance of blood 25-OH-D levels and extra-renal 1alpha-hydroxylase in the classical and nonclassical actions of 1alpha,25-dihydroxyvitamin D(3) Semin Dial. 2007;20:316–24. doi: 10.1111/j.1525-139X.2007.00302.x. [DOI] [PubMed] [Google Scholar]
- 33.Holick MF. Noncalcemic Actions of 1,25-Dihydroxyvitamin D3 and clinical Implications. In: Holick MF, ed. Vitamin D-Physiology, Molecular Biology, and Clinical Applications. Humana Press; Totowa/New Yersey 1999:207-16. [Google Scholar]
- 34.Lehmann B, Genehr T, Knuschke P, Pietzsch J, Meurer M. UVB-induced conversion of 7-dehydrocholesterol to 1α,25-dihydroxyvitamin D3 in an in vitro human skin equivalent model. J Invest Dermatol. 2001;117:1179–85. doi: 10.1046/j.0022-202x.2001.01538.x. [DOI] [PubMed] [Google Scholar]
- 35.Loomis WF. Skin-pigment regulation of vitamin-D biosynthesis in man. Science. 1967;157:501–6. doi: 10.1126/science.157.3788.501. [DOI] [PubMed] [Google Scholar]
- 36.Zehnder D, Bland R, Williams MC. Extrarenal expression of 25-hydroxyvitamin D3-1α-Hydroxylase. J Clin Endocrinol Metab. 2001;10:888–94. doi: 10.1210/jc.86.2.888. [DOI] [PubMed] [Google Scholar]
- 37.Hewison M, Burke F, Evans KN, Lammas DA, Sansom DM, Liu P, et al. Extra-renal 25-hydroxyvitamin D3-1alpha-hydroxylase in human health and disease. J Steroid Biochem Mol Biol. 2007;103:316–21. doi: 10.1016/j.jsbmb.2006.12.078. [DOI] [PubMed] [Google Scholar]
- 38.Jean G, Terrat JC, Vanel T, Hurot JM, Lorriaux C, Mayor B, et al. Evidence for persistent vitamin D 1-alpha-hydroxylation in hemodialysis patients: evolution of serum 1,25-dihydroxycholecalciferol after 6 months of 25-hydroxycholecalciferol treatment. Nephron Clin Pract. 2008;110:c58–65. doi: 10.1159/000151534. [DOI] [PubMed] [Google Scholar]
- 39.KDIGO Clinical Practice Guideline for the Diagnosis Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) Kidney Int. 2009;76:S1–130. doi: 10.1038/ki.2009.172. [DOI] [PubMed] [Google Scholar]
- 40.Vieth R. Vitamin D supplementation, 25-hydroxyvitamin D concentrations, and safety. Am J Clin Nutr. 1999;69:842–56. doi: 10.1093/ajcn/69.5.842. [DOI] [PubMed] [Google Scholar]
- 41.Palmer SC, McGregor DO, Macaskill P, Craig JC, Elder GJ, Strippoli GF. Meta-analysis: vitamin D compounds in chronic kidney disease. Ann Intern Med. 2007;147:840–53. doi: 10.7326/0003-4819-147-12-200712180-00004. [DOI] [PubMed] [Google Scholar]
- 42.Gal-Moscovici A, Sprague SM. Role of vitamin D deficiency in chronic kidney disease. J Bone Miner Res. 2007;22(Suppl 2):V91–4. doi: 10.1359/jbmr.07s203. [DOI] [PubMed] [Google Scholar]
- 43.Dusso AS, Brown AJ, Slatopolsky E, Vitamin D. Am J Physiol. 2005;289:F8–28. doi: 10.1152/ajprenal.00336.2004. [DOI] [PubMed] [Google Scholar]
- 44.MacLaughlin J, Holick MF. Aging decreases the capacity of human skin to produce vitamin D3. J Clin Invest. 1985;76:1536–8. doi: 10.1172/JCI112134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Krause R, Bennhold I, Matulla B. Regular UV(B) irradiation in prevention and therapy of vitamin D deficiency in hemodialysis patients. In: Holick MF, Jung EG (eds) Biologic Effects of Light 1995. de Gruyter, Berlin/New York 1996:64-6. [Google Scholar]
- 46.Krause R. Role of Vitamin D and Ultraviolet Radiation in Chronic Kidney Disease. In: Holick MF (Ed.) Vitamin D – Physiology, Molecular Biology, and Clinical Applications (2nd Ed.), pg. 967-983, Humana Press / Springer New York 2010:967-84. [Google Scholar]
- 47.Klamroth R. Der Einfluß serieller UVB-Exposition auf die körperliche Leistungsfähigkeit ambulanter Hämodialyse-Patienten unter besonderer Berücksichtigung des Vitamin D-Stoffwechsels. [MD-Thesis] Berlin: Freie Universität 1996. [Google Scholar]
- 48.Winter P. Teilkörperbestrahlung mit einem sonnenähnlichen Wellenspektrum (UVB + UVA) während der Hämodialyse und dessen Einfluss auf den Vitamin-D-Metabolismus [ MD-Thesis]. Berlin: Charité 2007. [Google Scholar]
- 49.Klamroth R, Krause R. Bühring. Ausdauertrainingsähnliche Kreislauf- und Stoffwechseleffekte unter serieller UV-Bestrahlung bei Dialysepatienten. Phys Rehab Kur Med. 1996;6:155. [Google Scholar]
- 50.Krause R, Albrecht C, Felsenberg D. Bone mineral density and vertebral morphometry after UV-therapy in hemodialysis patients. Nephrol Dial Transplant. 1996;1:1212. [Google Scholar]
- 51.Krause R, Bennhold I, Albrecht C. Bone mineral density, vitamin D metabolism and vitamin D receptor after UV(B) irradiation in hemodialysis patients. In: Holick MF, Jung EG (eds) Biologic Effects of Light 1995. de Gruyter, Berlin-New York 1996:67-9. [Google Scholar]
- 52.Albrecht C. Wirkungen serieller UV-B-Bestrahlung auf den Knochenmineralgehalt, die Knochenmorphometrie und die Vitamin D3-Synthese bei ambulanten chronischen Hämodialysepatienten [MD-Thesis] Berlin: Freie Universität 1998. [Google Scholar]
- 53.Matias PJ, Ferreira C, Jorge C, Borges M, Aires I, Amaral T, et al. 25-Hydroxyvitamin D3, arterial calcifications and cardiovascular risk markers in haemodialysis patients. Nephrol Dial Transplant. 2009;24:611–8. doi: 10.1093/ndt/gfn502. [DOI] [PubMed] [Google Scholar]
- 54.Moe S, Drüeke T, Cunningham J, Goodman W, Martin K, Olgaard K, et al. Kidney Disease: Improving Global Outcomes (KDIGO) Definition, evaluation, and classification of renal osteodystrophy: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO) Kidney Int. 2006;69:1945–53. doi: 10.1038/sj.ki.5000414. [DOI] [PubMed] [Google Scholar]
- 55.National Kidney Foundation K/DOQI clinical practice guidelines for bone metabolism and disease in children with chronic kidney disease. Am J Kidney Dis. 2005;46:S1–121. doi: 10.1053/S0272-6386(05)01244-8. [DOI] [PubMed] [Google Scholar]
- 56.Lindergård B, Johnell O, Nilsson BE, Wiklund PE. Studies of bone morphology, bone densitometry and laboratory data in patients on maintenance hemodialysis treatment. Nephron. 1985;39:122–9. doi: 10.1159/000183355. [DOI] [PubMed] [Google Scholar]
- 57.Wissing KM, Broeders N, Moreno-Reyes R, Gervy C, Stallenberg B, Abramowicz D. A controlled study of vitamin D3 to prevent bone loss in renal-transplant patients receiving low doses of steroids. Transplantation. 2005;79:108–15. doi: 10.1097/01.TP.0000149322.70295.A5. [DOI] [PubMed] [Google Scholar]
- 58.Rickers H, Nielsen AH, Smith Pederson R, Rødbro P. Bone mineral loss during maintenance hemodialysis. Acta Med Scand. 1978;204:263–7. doi: 10.1111/j.0954-6820.1978.tb08437.x. [DOI] [PubMed] [Google Scholar]
- 59.Lechleitner P, Krimbacher E, Genser N, Fridrich L, zur Nedden D, Helweg G, et al. Bone mineral densitometry in dialyzed patients: quantitative computed tomography versus dual photon absorptiometry. Bone. 1994;15:387–91. doi: 10.1016/8756-3282(94)90814-1. [DOI] [PubMed] [Google Scholar]
- 60.Taal MW, Masud T, Green D, Cassidy MJ. Risk factors for reduced bone density in haemodialysis patients. Nephrol Dial Transplant. 1999;14:1922–8. doi: 10.1093/ndt/14.8.1922. [DOI] [PubMed] [Google Scholar]
- 61.Barnas U, Schmidt A, Seidl G, Kaider A, Pietschmann P, Mayer G. A comparison of quantitative computed tomography and dual X-ray absorptiometry for evaluation of bone mineral density in patients on chronic hemodialysis. Am J Kidney Dis. 2001;37:1247–52. doi: 10.1053/ajkd.2001.24529. [DOI] [PubMed] [Google Scholar]
- 62.Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr. 2006;84:18–28. doi: 10.1093/ajcn/84.1.18. [DOI] [PubMed] [Google Scholar]
- 63.Dawson-Hughes B, Heaney RP, Holick MF, Lips P, Meunier PJ, Vieth R. Estimates of optimal vitamin D status. Osteoporos Int. 2005;16:713–6. doi: 10.1007/s00198-005-1867-7. [DOI] [PubMed] [Google Scholar]
- 64.Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Endocrine Society Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–30. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- 65.Krause R, Bennhold I, Britzke K. Reduction of cardiac risk factors in coronary and hemodialysis patients after UVB therapy. In: MF Holick, EG (eds) Jung Biologic Effects of Light 1995. de Gruyter, Berlin 1996:70-2. [Google Scholar]
- 66.Krause R, Klamroth R, Bennhold IUV. (B) irradiation reduces cardiac risk in hemodialysis patients. J Am Soc Nephrol. 1996;7:1452. [Google Scholar]
- 67.Krause R, Bühring M, Hopfenmüller W, Holick MF, Sharma AM. Ultraviolet B and blood pressure. Lancet. 1998;352:709–10. doi: 10.1016/S0140-6736(05)60827-6. [DOI] [PubMed] [Google Scholar]
- 68.Michos ED, Melamed ML. Vitamin D and cardiovascular disease risk. Curr Opin Clin Nutr Metab Care. 2008;11:7–12. doi: 10.1097/MCO.0b013e3282f2f4dd. [DOI] [PubMed] [Google Scholar]
- 69.Abel HH, Krause R, Klüssendorf D, Koepchen HP. Changed relations between cardiorespiratory parameters and heart rate variability in endurance-trained individuals at rest. In: Chronobiology & Chronomedicine. Ed. by G.Hildebrandt, R.Moog, F.Raschke, pg.187-192. Verlag Peter Lang, Frankfurt/Main-Bern-New York-Paris 1987. [Google Scholar]
- 70.Abel HH, Krause R, Klein B. Herzfrequenzvariabilität und Behandlung mit UV-Licht. Phys Rehab Kur Med. 1995;5:4546. [Google Scholar]
- 71.London GM, Guérin AP, Verbeke FH, Pannier B, Boutouyrie P, Marchais SJ, et al. Mineral metabolism and arterial functions in end-stage renal disease: potential role of 25-hydroxyvitamin D deficiency. J Am Soc Nephrol. 2007;18:613–20. doi: 10.1681/ASN.2006060573. [DOI] [PubMed] [Google Scholar]
- 72.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 73.Krause R, Bennhold I, Bühring M. Heliotherapie bei Dialysepatienten – eine Alternative in der Therapie der renalen Osteopathie. Nieren- Hochdruckkr. 1994;23:450. [Google Scholar]
- 74.Rojas-Rivera J, De La Piedra C, Ramos A, Ortiz A, Egido J. The expanding spectrum of biological actions of vitamin D. Nephrol Dial Transplant. 2010;25:2850–65. doi: 10.1093/ndt/gfq313. [DOI] [PubMed] [Google Scholar]
- 75.Bikle DD. Extrarenal synthesis pof 1,25-dihydroxyvitamin D and its health implications.; in: Holick MF (ed): Vitamin D – Physiology, Molecular Biology, and Clinical Application. New York, Springer 2010:277-96. [Google Scholar]
- 76.Grant WB. The health benefits of solar irradiance and vitamin D and the consequences of their deprivation.; in: Holick MF (ed): Vitamin D – Physiology, Molecular Biology, and Clinical Application. New York, Springer 2010:745-64. [Google Scholar]