Abstract
Anti-leucine-rich glioma inactivated-1 (LGI1) limbic encephalitis (LE) is a rare neurological disorder that has a subacute course of progressive encephalopathy and fasciobrachial dystonic seizures. We report a patient with anti-LGI1 LE that presented with atypical manifestations that complicated the diagnosis. A 62-year-old woman presented with a chronic course of memory disturbance and a subsequent relapse with an altered mental status after 10 months. The patient reported frequent chest pain of squeezing and dull nature, typically lasting 10-30 seconds. The chest pain was related to partial seizures, which were confirmed by video-EEG monitoring. Anti-LGI1 antibody was identified in serum and CSF. The patient's symptoms improved by immune modulation treatment. Patients with anti-LGI1 LE can experience atypical partial seizures, and a chronic relapsing course. Clinical suspicions and video-EEG monitoring are helpful for the early diagnosis and effective immune modulation.
Keywords: limbic encephalitis, chest pain, seizure, immune
INTRODUCTION
Limbic encephalitis (LE) is an uncommon neurological disorder characterized by a subacute and progressive altered consciousness, memory disturbance, and recurrent seizures. Classically, LE is considered as paraneoplastic disorder [1, 2]. Antibodies including anti-Hu, anti-Yo, anti-CV2/CRMP5, anti-Ri, anti-Ma2, and anti-amphiphysin are associated with paraneoplastic LE. Recently, new antibodies were identified that target neuronal cell surface antigens, ion channels (i.e., voltage-gated potassium channels [VGKC]), and ligand-gated ion channels (i.e., NMDA, AMPA, and GABAB receptor channels), which are not commonly related to tumors [3-5].
LE associated with antibodies against leucine-rich glioma inactivated-1 (LGI1), one of the specific targets of VGKC-complex antibodies, is characterized by faciobrachial dystonic seizures (FBDS) and memory loss with a subacute clinical course [5-7]. Usually, FBDS precedes other symptoms and prompts the diagnosis of anti-LGI1 LE [7]. However, here we report a case of anti-LGI1 LE that presented with atypical chest pain and spontaneous relapsing-remitting course that complicated the diagnosis.
CASE REPORT
A 62-year-old woman presented with confusion and memory loss in August 2012. She developed confusion with disorientation to the time and place and had no memory of a recent family trip before 2 days of admission. Upon admission, her serum sodium was 120 mmol/L, which was corrected to 134 mmol/L after 3 days. A brain MRI and EEG failed to indicate any abnormality, and no focal deficit was found on neurological examinations. After correction of hyponatremia, she was discharged without significant problems, except for memory disturbance. Her Korean Mini-Mental State Examination (K-MMSE) score was 25 at the time of discharge (8/10 on time and place orientation and 0/3 on memory recall).
The patient was readmitted to our hospital 12 months after her initial admission. Since two months before readmission, she was experiencing recurrent chest discomfort that she described as squeezing and dull in nature, typically lasting 10~30 seconds. The frequency of these episodes was initially once a day, but progressed to more than 20 times a day after 2 months. She reported that her memory disturbance was aggravated and she had developed intermittent confusion with disorientation. She repeatedly asked, "Where am I?" and, "Why am I here?" and sometimes lost her sense of direction. On the day before her readmission, she experienced chest discomfort and subsequently lost consciousness and collapsed with facial grimacing and abnormal arm-twisting movements. She regained consciousness a few minutes later, but was disoriented to the time and place. Definite convulsive movements were not observed. At admission, she was alert, oriented and showed no focal deficits on neurological examination. Her K-MMSE score was 24 (8/10 on time and place orientation, 4/5 on attention and calculation and 0/3 on memory recall), and she showed no difficulties with daily activity during her admission. Routine blood tests and a brain MRI were normal; a routine EEG failed to show definite abnormalities. For her chest discomfort, transthoracic echocardiography, CT coronary angiography, and 24-h electrocardiography were all normal. Supine blood pressure was 130/60 mmHg, and orthostatic blood pressure at 0, 1, 3, and 5 min was 120/60, 125/60, 130/60, and 125/65 mmHg, respectively. Esophagogastroduodenoscopy and esophagogram with esophageal manometry revealed normal findings.
Initially, we diagnosed the patient with anxiety disorder and administered a selective serotonin reuptake inhibitor and an anxiolytic. However, her chest discomfort persisted. On video-EEG monitoring, ictal discharges were observed in the right temporal area during her chest discomfort (Fig. 1), whereas FBDS or other seizures were not reproduced. FDG PET revealed no abnormalities. After administering oxcarbazepine, the frequency and duration of her chest discomfort reduced to a few times a day and lasted only a few seconds, whereas her memory disturbance persisted. Thus, we suspected autoimmune causes for the limbic encephalitis, and anti-LGI1 antibody was detected in both serum and CSF (Fig. 2). After treatments with IV immunogloblin (0.4 g/day for 5 days) and antiepileptic drugs (oxcarbazepine and levetiracetam), the chest discomfort and memory disturbance markedly improved. Her follow-up K-MMSE score was 27 (8/10 on time and place orientation and 4/5 on attention and calculation). She has been symptom free for a month after her discharge.
Fig. 1.
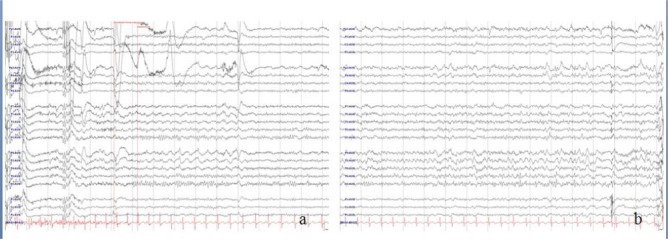
EEG revealed rhythmic sharp and slow waves (a) and rhythmic theta build-ups (b) in the right temporal area. The patient felt chest discomfort simultaneously with theseictal discharges.
Fig. 2.
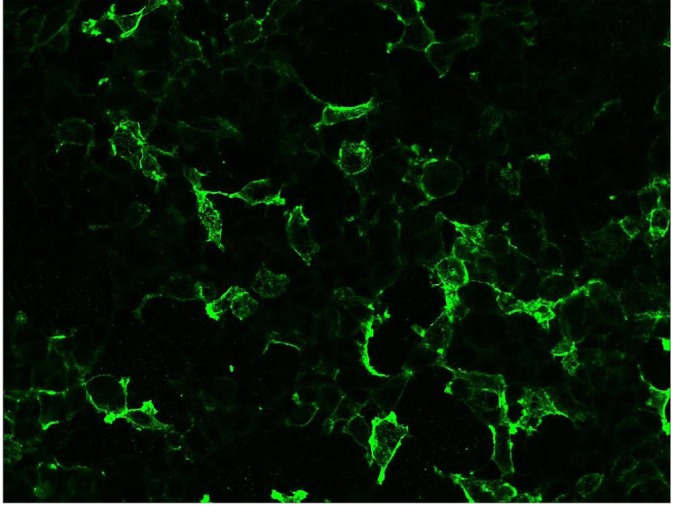
The patient's serum was reacted with an LGI1 antigen expressing cell line. Cell membranous immunofluorescence was detected on a cellbased indirect immunofluorescence test.
DISCUSSION AND CONCLUSIONS
Anti-LGI1 LE usually involves the medial temporal area, which causes memory dysfunction and seizures. This disorder was recently identified as an autoimmune encephalitis, which has distinctive clinical features, such as limbic dysfunction, seizures, and occasional hyponatremia [7-9]. The chest discomfort observed in our patients is an unusual manifestation. The cause of chest discomfort was identified as partial seizure in video-EEG, and thus it was related to the autoimmune activities.
Our patient showed spontaneous remission for 10 months after the initial manifestation of hyponatremia and memory disturbance. This spontaneous remission and relapse is very unusual in this autoimmune encephalitis, and delayed the diagnosis of the patient. In Anti-LGI1 LE, MRI may show signal changes in medial temporal lobes and basal ganglia [5-9], but PET is a more sensitive tool because it can detect abnormal glucose metabolism in these areas [7, 9, 10]. However, a number of patients do not show abnormalities on MRI or PET, and evidence of inflammation, including pleocytosis or protein elevation, can be absent from CSF [7-9]. Accordingly, typical clinical manifestations are necessary for prompt antibody diagnoses.
Chest tightness is usually documented in patients with cardiogenic or vasovagal syncope related to esophageal disorders such as esophageal spasm or gastroesophageal reflux [11]. Syncope is the first differential diagnosis in a patient with loss of consciousness without convulsive movements. In this patient, however, the possibility of cardiac or chest disease was excluded by thorough cardiac, chest and upper gastrointestinal work-ups, or with an orthostatic blood pressure examination. Instead, the symptom was related to parital seizures originating from right temporal lobe. Because her chest discomfort partially responded to an antiepileptic, this could be a clue to the proper diagnosis. However, until video-EEG monitoring, the cause of chest pain had been obscured.
Because of the atypical manifestations, only the previous history of hyponatremia and memory disturbance, in addition to a recent history of FBDS, could make us to suspect anti-LGI1 LE. Hyponatremia is commonly detected in patients with anti-LGI1 LE [5-9]. However, hyponatremia is a non-specific sign, because it is also caused by other medical conditions, such as decreased salt intake, salt loss by vomiting or diarrhea, or medical disorders including hypothyroidism or syndrome of inappropriate antidiuretic hormone secretion [12]. Cognitive impairment and confusion, which are cardinal manifestations of LE, are also found in patients with hyponatremia [12]. In our patient, memory disturbance, which is very common in the elderly, persisted after her plasma sodium level had normalized, whereas her other symptoms disappeared. Because these symptoms were similar to those of other medical disorders, we encountered difficulty with correctly diagnosing the patient on her first admission. Because the patient presented with the atypical manifestation of a spontaneous relapsing-remitting disease course with a 10-month interval, rather than a subacute progressive course, we encountered further difficulty with the diagnosis
Our patient showed normal neuroimaging and CSF findings, along with an atypical clinical presentation that mimicked other disorders with symptoms including anxiety, vasovagal, cardiogenic syncope, metabolic encephalopathy, psychiatric disorders, and geriatric cognitive impairment. A history of hyponatremia, pharmacoresistant partial seizures and early documentation of seizures by video-EEG monitoring could prompt the diagnosis. Nevertheless, it is notable that the atypical chest pain as well as the chronic remitting-relapsing condition were another manifestations of anti-LGI1 LE in our patient, and that early and optimal treatments are crucial for full recovery.
References
- 1.Corsellis JA, Goldberg GJ, Norton AR. "Limbic encephalitis" and its association with carcinoma. Brain. 1968;91:481–496. doi: 10.1093/brain/91.3.481. [DOI] [PubMed] [Google Scholar]
- 2.Bakheit AM, Kennedy PG, Behan PO. Paraneoplastic limbic encephalitis: clinico-pathological correlations. J Neurol Neurosurg Psychiatry. 1990;53:1084–1088. doi: 10.1136/jnnp.53.12.1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Graus F, Saiz A. Limbic encephalitis: a probably under-recognized syndrome. Neurologia. 2005;20:24–30. [PubMed] [Google Scholar]
- 4.Bien CG, Schulze-Bonhage A, Deckert M, Urbach H, Helmstaedter C, Grunwald T, Schaller C, Elger CE. Limbic encephalitis not associated with neoplasm as a cause of temporal lobe epilepsy. Neurology. 2000;55:1823–1828. doi: 10.1212/wnl.55.12.1823. [DOI] [PubMed] [Google Scholar]
- 5.Tüzün E, Dalmau J. Limbic encephalitis and variants: classification, diagnosis and treatment. Neurologist. 2007;13:261–271. doi: 10.1097/NRL.0b013e31813e34a5. [DOI] [PubMed] [Google Scholar]
- 6.Asztely F, Kumlien E. The diagnosis and treatment of limbic encephalitis. Acta Neurol Scand. 2012;126:365–375. doi: 10.1111/j.1600-0404.2012.01691.x. [DOI] [PubMed] [Google Scholar]
- 7.Irani SR, Michell AW, Lang B, Pettingill P, Waters P, Johnson MR, Schott JM, Armstrong RJ, S Zagami A, Bleasel A, Somerville ER, Smith SM, Vincent A. Faciobrachial dystonic seizures precede Lgi1 antibody limbic encephalitis. Ann Neurol. 2011;69:892–900. doi: 10.1002/ana.22307. [DOI] [PubMed] [Google Scholar]
- 8.Machado S, Pinto AN, Irani SR. What should you know about limbic encephalitis? Arq Neuropsiquiatr. 2012;70:817–822. doi: 10.1590/s0004-282x2012001000012. [DOI] [PubMed] [Google Scholar]
- 9.Lai M, Huijbers MG, Lancaster E, Graus F, Bataller L, Balice-Gordon R, Cowell JK, Dalmau J. Investigation of LGI1 as the antigen in limbic encephalitis previously attributed to potassium channels: a case series. Lancet Neurol. 2010;9:776–785. doi: 10.1016/S1474-4422(10)70137-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kamaleshwaran KK, Iyer RS, Antony J, Radhakrishnan EK, Shinto A. 18F-FDG PET/CT findings in voltagegated potassium channel limbic encephalitis. Clin Nucl Med. 2013;38:392–394. doi: 10.1097/RLU.0b013e318286b58b. [DOI] [PubMed] [Google Scholar]
- 11.Cheshire WP, Jr, Achem SR. The synchrony of syncope: chest pain, panic, and vasovagal convergence in the perfect autonomic storm. Clin Auton Res. 2004;14:44–48. doi: 10.1007/s10286-004-0161-7. [DOI] [PubMed] [Google Scholar]
- 12.Gulati S, Kumar L. 'Chest epilepsy' in a child. Postgrad Med J. 1992;68:369–370. doi: 10.1136/pgmj.68.799.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Devinsky O, Price BH, Cohen SI. Cardiac manifestations of complex partial seizures. Am J Med. 1986;80:195–202. doi: 10.1016/0002-9343(86)90009-4. [DOI] [PubMed] [Google Scholar]
- 14.Tzamaloukas AH, Malhotra D, Rosen BH, Raj DS, Murata GH, Shapiro JI. Principles of management of severe hyponatremia. J Am Heart Assoc. 2013;2:e005199. doi: 10.1161/JAHA.112.005199. [DOI] [PMC free article] [PubMed] [Google Scholar]


