Abstract
Transcranial direct current stimulation (tDCS) is an upcoming treatment modality for patients with schizophrenia. A series of recent observations have demonstrated improvement in clinical status of schizophrenia patients with tDCS. This review summarizes the research work that has examined the effects of tDCS in schizophrenia patients with respect to symptom amelioration, cognitive enhancement and neuroplasticity evaluation. tDCS is emerging as a safe, rapid and effective treatment for various aspects of schizophrenia symptoms ranging from auditory hallucinations-for which the effect is most marked, to negative symptoms and cognitive symptoms as well. An interesting line of investigation involves using tDCS for altering and examining neuroplasticity in patients and healthy subjects and is likely to lead to new insights into the neurological aberrations and pathophysiology of schizophrenia. The mechanistic aspects of the technique are discussed in brief. Future work should focus on establishing the clinical efficacy of this novel technique and on evaluating this modality as an adjunct to cognitive enhancement protocols. Understanding the mechanism of action of tDCS as well as the determinants and neurobiological correlates of clinical response to tDCS remains an important goal, which will help us expand the clinical applications of tDCS for the treatment of patients with schizophrenia.
Keywords: Transcranial direct current stimulation, Auditory hallucinations, Cortical plasticity, Schizophrenia
INTRODUCTION
Antipsychotics have been the mainstay of treatment in schizophrenia since the introduction of chlorpromazine in 1952. The advent of antipsychotics has revolutionized the treatment of schizophrenia.1) However, the conceptual paradigm for the treatment of schizophrenia has been largely unchanged since. Despite several attempts at theorizing schizophrenia as a disorder of neurotransmitters other than dopamine, there is no antipsychotic drug which does not have an anti-dopaminergic action.2) Nonetheless, antipsychotics continue to be the cornerstone and the gold standard for treatment of schizophrenia; but for them, we might have been stuck in the era of custodial care with the occasional electroconvulsive therapy.1) And yet, one cannot help but perceive an element of therapeutic stagnation-at least in terms of pharmacologic options, that has come to characterize the clinical management of this chronic disorder.3) This gap in our care drives us toward discovering and/or inventing new modalities of treatment; along these lines, for the treatment of schizophrenia symptoms that do not respond to antipsychotic medication, a host of add-on pharmacological choices have been described.4)
In this context, it is interesting to note that a series of recent observations have consistently demonstrated an immediate amelioration of persistent auditory verbal hallucinations in schizophrenia with transcranial direct current stimulation (tDCS). Application of tDCS for various psychiatric disorders including schizophrenia has been commented upon as an exciting area requiring further systematic exploration.5) Interestingly, application of transcranial electrical brain stimulation for the treatment of severe mental disorders like psychosis dates back to 1870s.6) Recently, there has been a re-emergent interest in the application of tDCS for the treatment of schizophrenia. In this review, we summarize the studies that have examined the effects of tDCS in schizophrenia patients. We identified these studies by performing a literature search in PubMed, PsycINFO and Google Scholar for published studies up until October 2013, with the following search terms and their combinations: transcranial direct current stimulation, tDCS, and schizophrenia.
MAIN DISCOURSE
Transcranial Direct Current Stimulation
tDCS is a noninvasive brain stimulation technique where direct current in the range of 0.5 to 2 mA is passed through the scalp by means of electrodes ranging in size, most commonly, from 25 to 35 cm2 over designated areas of interest in an attempt to modulate the activity of specific brain region(s).7-10) The historical roots of tDCS electrophysiology has been traced to the discovery of the biological effects of direct current; indeed, as early as two centuries ago, application of direct current to the scalp was possibly used to treat mental disorder.11) It is an offshoot from techniques of electro-stimulation and electro-anesthesia, where direct current bias was reliably employed in the 1950s.8) First clinical results using modern forms of tDCS were reported in the 1960s and 1970s motivated by the realization, in animal studies, that several minute long stimulation protocols had lasting changes on the cortical excitability.8) Since then, tDCS has been explored for efficacy in a multitude of disorders ranging from pain to depression to post stroke recovery with varying levels of success.12,13)
Though tDCS has been around for several decades, with regards to its application in treatment of schizophrenia, this therapeutic technique has had a rediscovery of sorts very recently, where it has been shown to have a relatively selective effect leading to rapid amelioration of auditory hallucinations in patients with schizophrenia (Table 1). Concurrently, researchers working on its effects on healthy individuals have been able to demonstrate stable, long lasting neuroplastic effects of this intervention in improving mathematical abilities.14) These interesting developments have led to newer questions in the area of "neuroethics".15,16) However, the debate on "neuroethics" is beyond the scope of this manuscript since the focus of this review is to critically evaluate the use of this emerging technique in patients with schizophrenia.
Table 1.
Studies using tDCS for symptom reduction in patients with schizophrenia
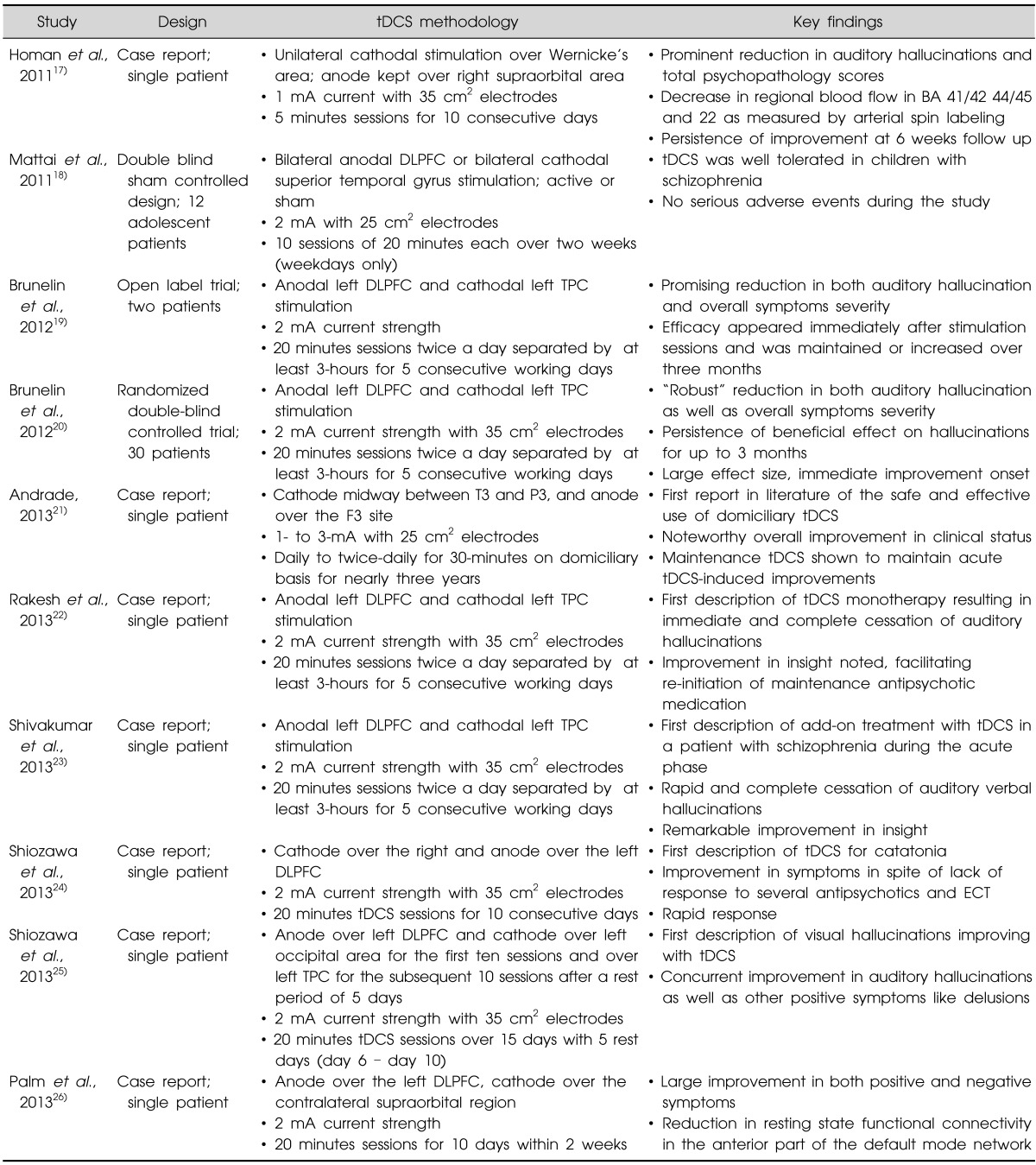
tDCS, transcranial direct current stimulation; DLPFC, dorsolateral prefrontal cortex; TPC, temporoparietal cortex; BA, Brodmann area; ECT, electroconvulsive therapy.
Application of tDCS in Schizophrenia
Research on tDCS in schizophrenia has been in three largely distinct directions. Several case reports, and one randomized controlled trial (RCT) have tested its effectiveness in symptom reduction and its tolerability (Table 1). Other studies have evaluated the effect of tDCS on various cognitive faculties in the context of schizophrenia (Table 2). A third line of enquiry has utilized tDCS in conjunction with transcranial magnetic stimulation (TMS) as an investigative approach to evaluate neuroplasticity changes in patients with this disorder (Table 3). Insights gleaned from these enquiries in discussed below.
Table 2.
Studies using tDCS for enhancement of cognition in patients with schizophrenia
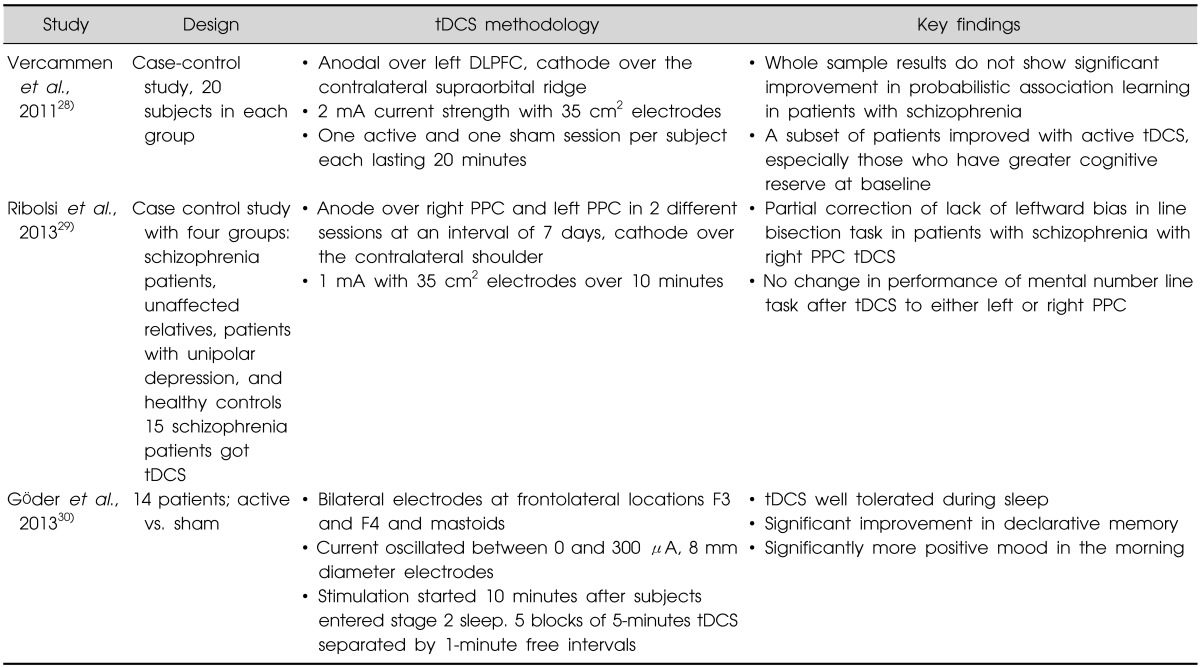
tDCS, transcranial direct current stimulation; DLPFC, dorsolateral prefrontal cortex; PPC, posterior parietal cortex.
Table 3.
Studies using tDCS to evaluate neuroplasticity in patients with schizophrenia
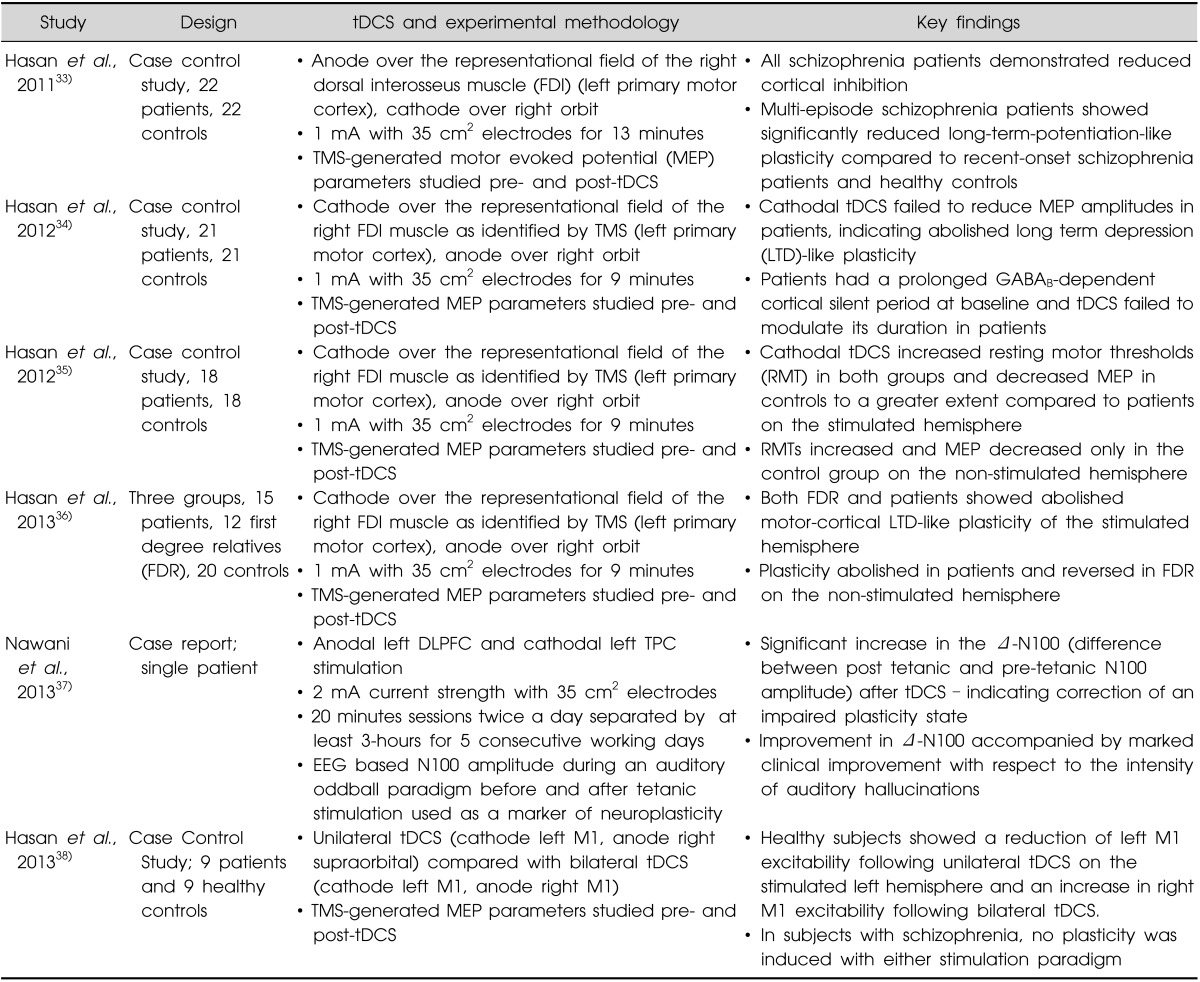
tDCS, transcranial direct current stimulation; DLPFC, dorsolateral prefrontal cortex; TPC, temporoparietal cortex; EEG, electroencephalography.
Safety of tDCS in Schizophrenia
A total of about 50 patients with schizophrenia have been reported in world literature to have received tDCS for therapeutic purposes (Table 1).17-26) One consistent observation is that tDCS appears to be remarkably safe in the short and medium term. Though the long term safety of the technique is yet to be evaluated through systematic long term studies (although it is encouraging to note that the single case report of safe and effective domiciliary use of daily to twice-daily, domiciliary, 30-minutes, 1- to 3-mA tDCS sessions across nearly 3 years for the treatment of continuous, disabling, clozapine-refractory auditory hallucinations in schizophrenia)21); moreover, there has not been a single published report where tDCS had to be stopped for safety reasons. In addition, it is reassuring to note that the study in pediatric sample has not reported any significant problems either.18) Even in a schizophrenia patient with a dermatological condition, tDCS could be applied safely on the region with vitiligo.27) In many of the earlier reports, side effects that are reported have been mild itching and burning sensation, or mild but tolerable levels of pain at the electrode placement site. Studies involving controls have been equally comforting on the safety issue.14)
tDCS in Schizophrenia: Clinical Impact
While the focus of most of the reports till date has been on hallucinations-the symptom cluster that has shown consistent improvement with tDCS-few reports also mention significant gains in negative symptoms. In the RCT by Brunelin et al.,20) the effect size for improvement of negative symptoms was 1.07. Most reports present a picture of overall improvement in the patient's general state, including functioning as well as social interaction. Another interesting observation from our group has been the improvement in insight that has accompanied decrease in hallucinatory experiences.22,23) With regard to cognitive symptoms, the three studies till date have been largely positive (Table 2).28-30) While two of them have found a clear improvement in cognitive faculties,29,30) the third observed improvement only in a subset of patients.28) These studies have only looked at select cognitive functions. Hemineglect bias (as evaluated by the line bisection studies) and defects in declarative memory are only two of the many cognitive deficits reported in patients with schizophrenia. Till the point when studies can demonstrate convincing improvement in a broad range of cognitive faculties, and these distill down to functional improvement in patients, one needs to be appropriately circumspect about the potential utility of this technique in ameliorating cognitive symptoms. Sample sizes in all these studies are modest but they open up an interesting possibility of helping patients with their cognitive symptoms. These findings, although preliminary, are quite exciting and make one wonder whether tDCS adaptively modulates certain critical component(s) in the pathophysiology of schizophrenia.
Effectiveness of tDCS on Auditory Hallucinations in Schizophrenia
With regard to clinical effectiveness, following features make tDCS quite distinctive and appealing as a novel therapeutic technique:
(i) Rapid onset of action: Most reports till date appear to suggest that clinical improvement begins quite early, in some cases just after the first couple of sessions of tDCS.19,22-24)
(ii) The persistence of response is another factor that most reports concur on. A five to ten day session can be expected to provide sustained improvement for two to three months. This is, perhaps, the most favorable aspect of treatment with tDCS, enabling patients to achieve symptom control which is not only fast but also long lasting. This opens up many therapeutic avenues and possibilities and is likely to increase the acceptability of treatment as a whole.
(iii) Considering the fact that most of these reports have looked at patients who have been on antipsychotics for a long time without appreciable response, the quantum of improvement is quite striking. The effect size reported in the only RCT by Brunelin et al.20) was 1.58, almost thrice the usual effect sizes with antipsychotic medication.
Of course, any discussion on the size of the effect has to be tempered by the knowledge that potential publication bias might operate to inflate apparent effect sizes during the initial periods whenever a new treatment is introduced.31) The same enthusiasm had greeted the introduction of TMS on the clinical scene with large effect sizes being reported initially. But over time it has fallen; the current understanding is that it is actually close to 0.3.32) Hence, one has to wait for studies with larger samples to get a true estimation of the impact tDCS has on symptoms of schizophrenia.
tDCS as an Investigative tool for Schizophrenia
The investigative potential of tDCS to understand the pathogenesis schizophrenia has been tapped by the series of research publications over the last two years; these research works have demonstrated altered neuroplasticity in patients with schizophrenia through tDCS based experiments (Table 3).33-38) They have shown that both long term potentiation (LTP) and long term depression (LTD) like neuroplasticity is deficient in patients with schizophrenia.39) This finding has further been extended to unaffected first degree relatives, suggesting a possible endophenotype for the disorder. In these studies, single session of tDCS has been used to induce real time, instantaneous plasticity changes which have been validated by alteration in the motor evoked potentials (MEPs), as studied by TMS. This line of research is quite exciting as it demonstrates, in a very direct and consistent manner, that tDCS causes real, measurable changes in the way neuronal circuits behave. Even more exciting, perhaps, is the finding that these changes are transferred across hemispheres, at least in healthy controls.35,36) This line of work has been taken a step further in a recent case report,37) where adaptive changes in this altered state of neuroplasticity were seen after a therapeutic trial of tDCS, and this improvement was in parallel with clinical improvement. This deserves further systematic exploration as an altered neuroplastic state has the potential to become both an endophenotype and a biomarker of clinical status in schizophrenia.
tDCS in Schizophrenia: Mechanism of Action
A good summary of the putative mechanisms of action by which tDCS causes benefits has been provided in a recent review.9) A lot remains unknown with many of the hypothesized mechanisms of action yet to be proven, and understanding these is an area of active research. What is clear; however, is that the effects of tDCS are highly polarity specific, at least at the neuronal level, and probably, by extension, at the circuit level. Anodal stimulation has been shown to enhance neuronal excitability while the reverse happens if cathode is used.40) This change in excitability is likely due to shift of the resting membrane potential and is understood to be the primary mechanism underlying the short term effects of tDCS.11,40) The longer term effects of tDCS are proposed to be due a combination of changes in the synaptic microenvironment-specifically-by NMDA and GABA receptor activity alterations,9,41) which can then lead to changes along the lines of LTP or LTD. tDCS can result in adaptive modulation of neuroplasticity through brain derived neurotrophic factor (BDNF) dependent mechanism,42,43) since BDNF abnormalities are linked with the pathogenesis of positive symptoms in schizophrenia including auditory hallucinations,44) it is possible this might have mechanistic relevance. A cascading butterfly effect of the resulting changes in local neuronal circuitry over longer range neuron networks by means of alteration in the intracellular and extracellular molecular and structural profile is plausible, and may underlie the long term effects of tDCS. Interestingly, it has been found that the effects of tDCS do not appear to be limited to the site of stimulation or to the local networks, even in the short term; in this context it is interesting to note that tDCS of the prefrontal cortex was demonstrated to activate the midbrain and this might have potential mechanistic basis in treating schizophrenia patients.45) Changes in the MEP parameters have been noted in the opposite hemisphere shortly after a single session of tDCS.35) Together, all these might be linked with the proposed mechanism of tDCS in altering cortical excitation/inhibition balance,46) since such cortical dis-inhibitory states have been proposed to underlie the genesis of auditory hallucinations in schizophrenia.47)
In the context of schizophrenia, the reduction in auditory hallucinations could be understood as hyper polarization in the region of Heschl's gyrus, or activation of an underperforming fronto-temporal circuitry or a combination of both.20) That the response is sometimes, almost immediate suggests that electrophysiological alterations are primarily at play.40) The persistence of the effect, as is reported in many studies, is likely to be due to longer lasting structural changes at the synaptic and network level.41)
FUTURE DIRECTIONS
The most immediate issue that needs to be addressed is perhaps, establishing further support for the effectiveness of tDCS for positive symptoms through further large scale systematic studies; in addition, the impact of tDCS on other symptom dimensions needs to be evaluated. Equally important are long-term studies to establish the safety of tDCS in schizophrenia. Contextually, understanding the predictors of clinical response, the specific symptoms that respond best to the intervention, and those that do not are very important and relevant clinical questions. Given the potential utility of tDCS to enhance cognition in neuropsychiatric disorders, the impact of tDCS monotherapy/combining tDCS with cognitive training to improve cognitive deficits in schizophrenia is another critical area for further research.48,49) Given the safety of tDCS, this might be considered as an important avenue to explore in ultra-high risk subjects with attenuated psychosis symptoms. Apart from tDCS, parallel techniques with variations in the stimulation parameter like transcranial random noise stimulation (tRNS) and similar others need to be examined systematically. In this context, it is interesting to note that tRNS has recently been reported to improve negative symptoms in schizophrenia.50) Further refinements in the technique of application of tDCS, like use of more focused application by means of high definition tDCS,51) or array based applications52) and their impact on clinical efficacy is another area which needs systematic enquiry. On a larger timeframe, one needs to understand the mechanism of action of tDCS in the context of schizophrenia. The size of the effect and the immediacy and persistence of response suggest that tDCS is altering a fundamental pathology in the diseased brain. Concurrent application of investigative tDCS to characterize the neurobiological aberrations in subjects with genetic risk for schizophrenia is another critical area for future research. Understanding this would be crucial from the pathophysiological point of view since it can provide important leads towards identifying a reliable biomarker for schizophrenia-something that has eluded the research community for several years. This will have far reaching impact on the diagnosis and treatment of this chronic and often difficult to manage disease.
Acknowledgments
This work is partially supported by the Wellcome Trust/DBT India Alliance Senior Fellowship Research Grant (500236/Z/11/Z) as well as the Department of Science and Technology (Government of India) Research Grant (SR/CSI/158/2012) to GV. SMA, AB, and SVK are supported by the Wellcome Trust/DBT India Alliance. VS is supported by the Indian Council of Medical Research. AS, HN, HC, and JCN are supported by the Department of Science & Technology, Government of India.
References
- 1.Tandon R, Nasrallah HA, Keshavan MS. Schizophrenia, "just the facts" 5. Treatment and prevention. Past, present, and future. Schizophr Res. 2010;122:1–23. doi: 10.1016/j.schres.2010.05.025. [DOI] [PubMed] [Google Scholar]
- 2.Kapur S, Mamo D. Half a century of antipsychotics and still a central role for dopamine D2 receptors. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27:1081–1090. doi: 10.1016/j.pnpbp.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 3.Abbott A. Schizophrenia: The drug deadlock. Nature. 2010;468:158–159. doi: 10.1038/468158a. [DOI] [PubMed] [Google Scholar]
- 4.Torrey EF, Davis JM. Adjunct treatments for schizophrenia and bipolar disorder: what to try when you are out of ideas. Clin Schizophr Relat Psychoses. 2012;5:208–216. [PubMed] [Google Scholar]
- 5.George MS, Padberg F, Schlaepfer TE, O'Reardon JP, Fitzgerald PB, Nahas ZH, et al. Controversy: Repetitive transcranial magnetic stimulation or transcranial direct current stimulation shows efficacy in treating psychiatric diseases (depression, mania, schizophrenia, obsessive-complusive disorder, panic, posttraumatic stress disorder) Brain Stimul. 2009;2:14–21. doi: 10.1016/j.brs.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 6.Steinberg H. A pioneer work on electric brain stimulation in psychotic patients. Rudolph Gottfried Arndt and his 1870s studies. Brain Stimul. 2013;6:477–481. doi: 10.1016/j.brs.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 7.Rajji TK, Rogasch NC, Daskalakis ZJ, Fitzgerald PB. Neuroplasticity-based brain stimulation interventions in the study and treatment of schizophrenia: a review. Can J Psychiatry. 2013;58:93–98. doi: 10.1177/070674371305800206. [DOI] [PubMed] [Google Scholar]
- 8.Guleyupoglu B, Schestatsky P, Edwards D, Fregni F, Bikson M. Classification of methods in transcranial electrical stimulation (tES) and evolving strategy from historical approaches to contemporary innovations. J Neurosci Methods. 2013;219:297–311. doi: 10.1016/j.jneumeth.2013.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brunoni AR, Nitsche MA, Bolognini N, Bikson M, Wagner T, Merabet L, et al. Clinical research with transcranial direct current stimulation (tDCS): challenges and future directions. Brain Stimul. 2012;5:175–195. doi: 10.1016/j.brs.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nitsche MA, Cohen LG, Wassermann EM, Priori A, Lang N, Antal A, et al. Transcranial direct current stimulation: State of the art 2008. Brain Stimul. 2008;1:206–223. doi: 10.1016/j.brs.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Priori A. Brain polarization in humans: a reappraisal of an old tool for prolonged non-invasive modulation of brain excitability. Clin Neurophysiol. 2003;114:589–595. doi: 10.1016/s1388-2457(02)00437-6. [DOI] [PubMed] [Google Scholar]
- 12.Fregni F, Pascual-Leone A. Technology insight: noninvasive brain stimulation in neurology-perspectives on the therapeutic potential of rTMS and tDCS. Nat Clin Pract Neurol. 2007;3:383–393. doi: 10.1038/ncpneuro0530. [DOI] [PubMed] [Google Scholar]
- 13.Nitsche MA, Boggio PS, Fregni F, Pascual-Leone A. Treatment of depression with transcranial direct current stimulation (tDCS): a review. Exp Neurol. 2009;219:14–19. doi: 10.1016/j.expneurol.2009.03.038. [DOI] [PubMed] [Google Scholar]
- 14.Hauser TU, Rotzer S, Grabner RH, Mérillat S, Jäncke L. Enhancing performance in numerical magnitude processing and mental arithmetic using transcranial Direct Current Stimulation (tDCS) Front Hum Neurosci. 2013;7:244. doi: 10.3389/fnhum.2013.00244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fitz NS, Reiner PB. The challenge of crafting policy for do-it-yourself brain stimulation. J Med Ethics. 2013 doi: 10.1136/medethics-2013-101458. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohen Kadosh C, Levy N, O'Shea J, Shea N, Savulescu J. The neuroethics of non-invasive brain stimulation. Curr Biol. 2012;22:R108–R111. doi: 10.1016/j.cub.2012.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Homan P, Kindler J, Federspiel A, Flury R, Hubl D, Hauf M, et al. Muting the voice: a case of arterial spin labeling-monitored transcranial direct current stimulation treatment of auditory verbal hallucinations. Am J Psychiatry. 2011;168:853–854. doi: 10.1176/appi.ajp.2011.11030496. [DOI] [PubMed] [Google Scholar]
- 18.Mattai A, Miller R, Weisinger B, Greenstein D, Bakalar J, Tossell J, et al. Tolerability of transcranial direct current stimulation in childhood-onset schizophrenia. Brain Stimul. 2011;4:275–280. doi: 10.1016/j.brs.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brunelin J, Mondino M, Haesebaert F, Saoud M, Suaud-Chagny MF, Poulet E. Efficacy and safety of bifocal tDCS as an interventional treatment for refractory schizophrenia. Brain Stimul. 2012;5:431–432. doi: 10.1016/j.brs.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 20.Brunelin J, Mondino M, Gassab L, Haesebaert F, Gaha L, Suaud-Chagny MF, et al. Examining transcranial directcurrent stimulation (tDCS) as a treatment for hallucinations in schizophrenia. Am J Psychiatry. 2012;169:719–724. doi: 10.1176/appi.ajp.2012.11071091. [DOI] [PubMed] [Google Scholar]
- 21.Andrade C. Once- to twice-daily, 3-year domiciliary maintenance transcranial direct current stimulation for severe, disabling, clozapine-refractory continuous auditory hallucinations in schizophrenia. J ECT. 2013;29:239–242. doi: 10.1097/YCT.0b013e3182843866. [DOI] [PubMed] [Google Scholar]
- 22.Rakesh G, Shivakumar V, Subramaniam A, Nawani H, Amaresha AC, Narayanaswamy JC, et al. Monotherapy with tDCS for Schizophrenia: a case report. Brain Stimul. 2013;6:708–709. doi: 10.1016/j.brs.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 23.Shivakumar V, Bose A, Rakesh G, Nawani H, Subramaniam A, Agarwal SM, et al. Rapid improvement of auditory verbal hallucinations in schizophrenia after add-on treatment with transcranial direct-current stimulation. J ECT. 2013;29:e43–e44. doi: 10.1097/YCT.0b013e318290fa4d. [DOI] [PubMed] [Google Scholar]
- 24.Shiozawa P, da Silva ME, Cordeiro Q, Fregni F, Brunoni AR. Transcranial direct current stimulation (tDCS) for catatonic schizophrenia: a case study. Schizophr Res. 2013;146:374–375. doi: 10.1016/j.schres.2013.01.030. [DOI] [PubMed] [Google Scholar]
- 25.Shiozawa P, da Silva ME, Cordeiro Q, Fregni F, Brunoni AR. Transcranial direct current stimulation (tDCS) for the treatment of persistent visual and auditory hallucinations in schizophrenia: A case study. Brain Stimul. 2013;6:831–833. doi: 10.1016/j.brs.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 26.Palm U, Keeser D, Blautzik J, Pogarell O, Ertl-Wagner B, Kupka MJ, et al. Prefrontal transcranial direct current stimulation (tDCS) changes negative symptoms and functional connectivity MRI (fcMRI) in a single case of treatment-resistant schizophrenia. Schizophr Res. 2013;150:583–585. doi: 10.1016/j.schres.2013.08.043. [DOI] [PubMed] [Google Scholar]
- 27.Shiozawa P, da Silva ME, Raza R, Uchida RR, Cordeiro Q, Fregni F, et al. Safety of repeated transcranial direct current stimulation in impaired skin: a case report. J ECT. 2013;29:147–148. doi: 10.1097/YCT.0b013e318279c1a1. [DOI] [PubMed] [Google Scholar]
- 28.Vercammen A, Rushby JA, Loo C, Short B, Weickert CS, Weickert TW. Transcranial direct current stimulation influences probabilistic association learning in schizophrenia. Schizophr Res. 2011;131:198–205. doi: 10.1016/j.schres.2011.06.021. [DOI] [PubMed] [Google Scholar]
- 29.Ribolsi M, Lisi G, Di Lorenzo G, Koch G, Oliveri M, Magni V, et al. Perceptual pseudoneglect in schizophrenia: candidate endophenotype and the role of the right parietal cortex. Schizophr Bull. 2013;39:601–607. doi: 10.1093/schbul/sbs036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Göder R, Baier PC, Beith B, Baecker C, Seeck-Hirschner M, Junghanns K, et al. Effects of transcranial direct current stimulation during sleep on memory performance in patients with schizophrenia. Schizophr Res. 2013;144:153–154. doi: 10.1016/j.schres.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 31.Sommer IE, Aleman A, Slotema CW, Schutter DJ. Transcranial stimulation for psychosis: the relationship between effect size and published findings. Am J Psychiatry. 2012;169:1211. doi: 10.1176/appi.ajp.2012.12060741. [DOI] [PubMed] [Google Scholar]
- 32.Slotema CW, Aleman A, Daskalakis ZJ, Sommer IE. Meta-analysis of repetitive transcranial magnetic stimulation in the treatment of auditory verbal hallucinations: update and effects after one month. Schizophr Res. 2012;142:40–45. doi: 10.1016/j.schres.2012.08.025. [DOI] [PubMed] [Google Scholar]
- 33.Hasan A, Nitsche MA, Rein B, Schneider-Axmann T, Guse B, Gruber O, et al. Dysfunctional long-term potentiation-like plasticity in schizophrenia revealed by transcranial direct current stimulation. Behav Brain Res. 2011;224:15–22. doi: 10.1016/j.bbr.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 34.Hasan A, Nitsche MA, Herrmann M, Schneider-Axmann T, Marshall L, Gruber O, et al. Impaired long-term depression in schizophrenia: a cathodal tDCS pilot study. Brain Stimul. 2012;5:475–483. doi: 10.1016/j.brs.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 35.Hasan A, Aborowa R, Nitsche MA, Marshall L, Schmitt A, Gruber O, et al. Abnormal bihemispheric responses in schizophrenia patients following cathodal transcranial direct stimulation. Eur Arch Psychiatry Clin Neurosci. 2012;262:415–423. doi: 10.1007/s00406-012-0298-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hasan A, Misewitsch K, Nitsche MA, Gruber O, Padberg F, Falkai P, et al. Impaired motor cortex responses in non-psychotic first-degree relatives of schizophrenia patients: a cathodal tDCS pilot study. Brain Stimul. 2013;6:821–829. doi: 10.1016/j.brs.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 37.Nawani H, Kalmady SV, Bose A, Shivakumar V, Rakesh G, Subramaniam A, et al. Neural basis of tDCS effects on auditory verbal hallucinations in schizophrenia: A case report evidence for cortical neuroplasticity modulation. J ECT. 2013 doi: 10.1097/YCT.0b013e3182a35492. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 38.Hasan A, Bergener T, Nitsche MA, Strube W, Bunse T, Falkai P, et al. Impairments of motor-cortex responses to unilateral and bilateral direct current stimulation in schizophrenia. Front Psychiatry. 2013;4:121. doi: 10.3389/fpsyt.2013.00121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hasan A, Wobrock T, Rajji T, Malchow B, Daskalakis ZJ. Modulating neural plasticity with non-invasive brain stimulation in schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2013;263:621–631. doi: 10.1007/s00406-013-0446-8. [DOI] [PubMed] [Google Scholar]
- 40.Nitsche MA, Paulus W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol. 2000;527(Pt 3):633–639. doi: 10.1111/j.1469-7793.2000.t01-1-00633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liebetanz D, Nitsche MA, Tergau F, Paulus W. Pharmacological approach to the mechanisms of transcranial DC-stimulation-induced after-effects of human motor cortex excitability. Brain. 2002;125:2238–2247. doi: 10.1093/brain/awf238. [DOI] [PubMed] [Google Scholar]
- 42.Antal A, Chaieb L, Moliadze V, Monte-Silva K, Poreisz C, Thirugnanasambandam N, et al. Brain-derived neurotrophic factor (BDNF) gene polymorphisms shape cortical plasticity in humans. Brain Stimul. 2010;3:230–237. doi: 10.1016/j.brs.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 43.Fritsch B, Reis J, Martinowich K, Schambra HM, Ji Y, Cohen LG, et al. Direct current stimulation promotes BDNF-dependent synaptic plasticity: potential implications for motor learning. Neuron. 2010;66:198–204. doi: 10.1016/j.neuron.2010.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kalmady SV, Venkatasubramanian G, Shivakumar V, Jose D, Ravi V, Gangadhar BN. Relationship between brain-derived neurotrophic factor and schneiderian first rank symptoms in antipsychotic-naïve schizophrenia. Front Psychiatry. 2013;4:64. doi: 10.3389/fpsyt.2013.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chib VS, Yun K, Takahashi H, Shimojo S. Noninvasive remote activation of the ventral midbrain by transcranial direct current stimulation of prefrontal cortex. Transl Psychiatry. 2013;3:e268. doi: 10.1038/tp.2013.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Krause B, Márquez-Ruiz J, Kadosh RC. The effect of transcranial direct current stimulation: a role for cortical excitation/inhibition balance? Front Hum Neurosci. 2013;7:602. doi: 10.3389/fnhum.2013.00602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Behrendt RP, Young C. Hallucinations in schizophrenia, sensory impairment, and brain disease: a unifying model. Behav Brain Sci. 2004;27:771–787. doi: 10.1017/s0140525x04000184. [DOI] [PubMed] [Google Scholar]
- 48.Demirtas-Tatlidede A, Vahabzadeh-Hagh AM, Pascual-Leone A. Can noninvasive brain stimulation enhance cognition in neuropsychiatric disorders? Neuropharmacology. 2013;64:566–578. doi: 10.1016/j.neuropharm.2012.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ditye T, Jacobson L, Walsh V, Lavidor M. Modulating behavioral inhibition by tDCS combined with cognitive training. Exp Brain Res. 2012;219:363–368. doi: 10.1007/s00221-012-3098-4. [DOI] [PubMed] [Google Scholar]
- 50.Palm U, Hasan A, Keeser D, Falkai P, Padberg F. Transcranial random noise stimulation for the treatment of negative symptoms in schizophrenia. Schizophr Res. 2013;146:372–373. doi: 10.1016/j.schres.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 51.Villamar MF, Volz MS, Bikson M, Datta A, Dasilva AF, Fregni F. Technique and considerations in the use of 4×1 ring high-definition transcranial direct current stimulation (HD-tDCS) J Vis Exp. 2013;(77):e50309. doi: 10.3791/50309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Park JH, Hong SB, Kim DW, Suh M, Im CH. A novel array-type transcranial direct current stimulation (tDCS) system for accurate focusing on targeted brain areas. IEEE Trans Magn. 2011;47:882–885. [Google Scholar]


