Abstract
Study design
Prospective clinical observational study of low back pain (LBP) in patients undergoing laminectomy or laminotomy surgery for lumbar spinal stenosis (LSS).
Objectives
To quantify any change in LBP following laminectomy or laminotomy spinal decompression surgery.
Patients and methods
119 patients with LSS completed Oswestry Disability Index questionnaire (ODI) and Visual Analogue Scale for back and leg pain, preoperatively, 6 weeks and 1 year postoperatively.
Results
There was significant (p < 0.0001) reduction in mean LBP from a baseline of 5.14/10 to 3.03/10 at 6 weeks. Similar results were seen at 1 year where mean LBP score was 3.07/10. There was a significant (p < 0.0001) reduction in the mean ODI at 6 weeks and 1 year postoperatively. Mean ODI fell from 44.82 to 25.13 at 6 weeks and 28.39 at 1 year.
Conclusion
The aim of surgery in patients with LSS is to improve the resulting symptoms that include radicular leg pain and claudication. This observational study reports statistically significant improvement of LBP after LSS surgery. This provides frequency distribution data, which can be used to inform prospective patients of the expected outcomes of such surgery.
Keywords: Spine, Back pain, Laminectomy, Spinal stenosis
Introduction
Low back pain (LBP) is a common cause of morbidity and disability, with a prevalence of 28.5 % in one recent study [1]. There are many causes of chronic LBP, one of which is said to be lumbar spinal stenosis (LSS) [2]. Incidence increases with age and hence a large proportion of sufferers are past retirement age with a peak at the age of 73 [3].
Symptomatic LSS causes spinal claudication, back and radicular leg pain. In severe cases, this can lead to cauda equina syndrome with loss of bladder and bowel control [4]. Spinal decompression surgery has long been considered the gold standard surgical treatment for symptomatic LSS. The aim of surgery is to improve radicular leg pain and walking distance. It is also noted that some have noticed improvement in associated LBP following decompression surgery [5].
This observational study sought to quantify the effect of spinal decompression surgery on LBP in patients with LSS and provide evidence for the expected outcome of spinal decompression surgery on the LBP.
Materials and methods
Patients
Consecutive patients with symptoms of LSS were entered into the study between January 2007 and December 2011. Spinal stenosis that included central and lateral recess stenosis was confirmed with MRI scan. A total of 140 patients underwent a primary procedure of laminectomy (75) or laminotomy (65). Patients with associated pathology or instability that required additional surgical intervention were excluded from the study population. This included six patients who had discectomies and 15 patients who had fusions in addition to the spinal decompression surgery.
This leaves a sample size of 119 patients for statistical analysis. The patient group had a mixture of central and lateral recess spinal stenosis, which was unilateral or bilateral. Seven patients had stable lumbosacral spondylolisthesis and one had scoliosis in addition to LSS. These were deemed stable and did not require additional stabilisation procedures.
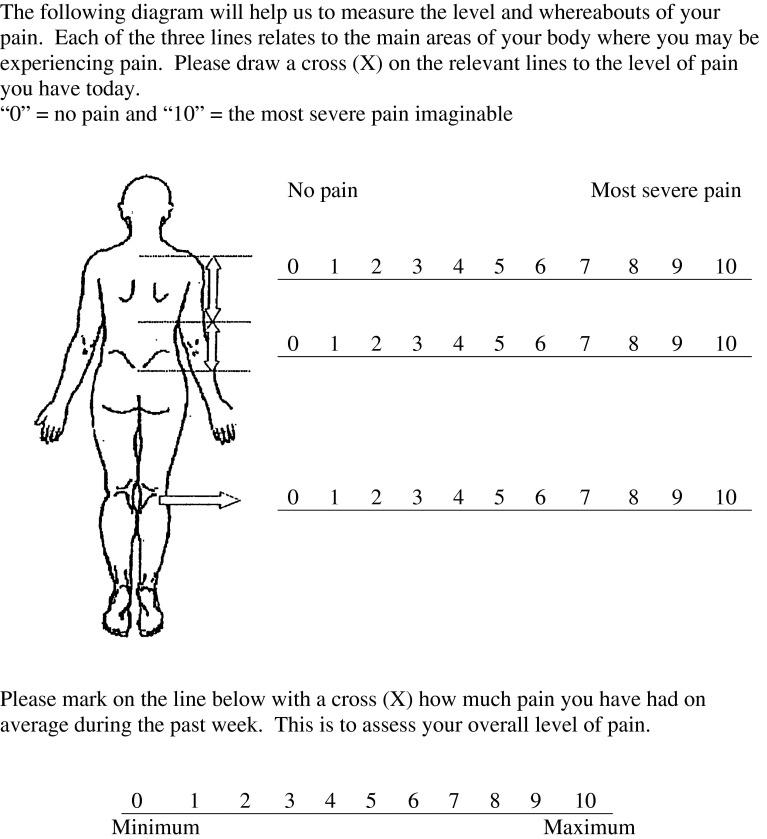
All patients provided informed consent and filled in Oswestry Disability Index (ODI) and Visual Analogue Scale (VAS) questionnaires (Fig. 1) preoperatively. These were repeated in clinic at 6 weeks and at 1 year postoperatively.
Fig. 1.
Visual Analogue Pain Score sheet
Operative procedure
Patients were positioned prone/kneeling. Image intensifier was used to confirm the level and a paramedian approach has been used utilising Cobb’s spinal elevators to gain subperiosteal access to the lamina. Coagulation diathermy was used to maintain haemostasis while cutting diathermy is used to demarcate surgical landmarks such as the facet joints. Laminectomy patients had the spinous processes removed. Closure was with vicryl in layers and skin clips were used in all patients.
Outcome measures
The severity of back and leg pain was assessed using the VAS [6] and the ODI [7]. The patients were asked to fill out the questionnaire just before their clinic consultation. For the VAS (Fig. 1), patients were asked to score their pain from 0 (no pain) to 10 (severe pain) for lower back and leg pain.
Although this is entirely subjective, the pain scale has been validated in back pain patients and has been shown to have moderate to good reliability [6].
The ODI questionnaire was used to determine the effect of LSS on everyday life. The questionnaire generates a percentage score indicating the level of disability from minimal (0–20 %) to bed-bound (80–100 %). The Oswestry scoring system has been shown to be a reliable and valid method for assessing changes in back pain symptoms [7, 8].
Statistical analyses
Patients who did not respond via post were excluded from the statistical analysis. Statistical analysis was carried out using GraphPad software. Pre- and postoperative scores were compared using the paired Student’s T test, generating a two-tailed p value. A p value of <0.05 was considered to be significant. Bonferroni correction factor was used for subgroups, giving a significant p value of <0.0083 for the male/female, laminotomy/laminectomy and central stenosis/lateral recess stenosis subgroups. VAS data were displayed in the form of frequency distributions with percentage change calculated for 6 weeks and 1 year. The mean preoperative and postoperative VAS scores were then used to calculate p values using the paired Student’s T-test.
Results
119 patients with central or lateral recess LSS were included in this study. 49 men and 70 women completed 6 weeks and 1-year follow-up assessments, generating data for statistical analysis. The average age of the study population was 68.2 with a range of 31–89. Fifteen patients had right sided, 10 had left-sided and 94 had bilateral decompressions. 24 patients had lateral recess stenosis and 95 had central spinal stenosis. The most common single level (n = 44) for primary operation was at L4/5 level, with the second commonest levels for primary surgery being L3/4 (n = 13), L2/3 (n = 6) and L5/S1 (n = 8). Of the 119 patients, 27 had single-level and 92 had multi-level surgery. The surgical procedure was complicated by small dural tears in 11 patients (9.25 %). These were repaired intraoperatively and had no long-term sequel. More bleeding than expected was experienced in four patients, and careful diathermy, use of bone wax and haemostatic sponges achieved adequate haemostasis. During the postoperative period one patient developed a chest infection and one patient had an epidural haematoma that was explored. There was an intraoperative spinous process fracture in one patient. The average inpatient stay was 2.66 days.
The results of the pre- and postoperative ODI scores are shown in Table 1. The average preoperative disability caused by back pain was 44.82 %. This figure falls into the category of severe disability as described by the designers of the scoring system [7]. Oswestry scores fell to an average of 25.13 at 6 weeks (p < 0.0001) and 28.39 at 1 year postoperatively (p < 0.0001). These scores both fall into the category of moderate disability. This decrease in ODI was not significantly affected by gender or indication for operating. Laminectomy patients had a better outcome than laminotomy patients (decrease of 24.38 vs. 14.43 % at 6 weeks and 20.16 vs. 12.25 % at 1 year), but these differences were not statistically significant, having considerable overlap of the confidence intervals. Decrease in ODI at 1 year for patients with lateral recess stenosis was not shown to be significant, with a p value of 0.0104.
Table 1.
Oswestry Disability Index percentage scores preoperatively and at 6 weeks and 1 year postoperatively
| n | Preop | 6 weeks postop | 1 year postop | 6 weeks mean reduction (CI) | P value | 1 year mean reduction (CI) | P value | |
|---|---|---|---|---|---|---|---|---|
| All | 119 | 44.82 | 25.13 | 28.39 | 19.69 (16.24–23.15) | <0.0001 | 16.43 (12.66–20.22) | <0.0001 |
| Gender | ||||||||
| Male | 49 | 43.27 | 26.16 | 29.39 | 17.11 (11.59–22.62) | <0.0001 | 13.88 (7.83–19.93) | <0.0001 |
| Female | 70 | 45.91 | 24.4 | 27.69 | 21.51 (16.2–26.83) | <0.0001 | 18.22 (12.68–23.78) | <0.0001 |
| Operation | ||||||||
| Laminectomy | 63 | 47.40 | 23.02 | 27.24 | 24.38 (18.37–30.39) | <0.0001 | 20.16 (13.67–26.64) | <0.0001 |
| Laminotomy | 56 | 41.93 | 27.5 | 29.68 | 14.43 (8.18–20.67) | <0.0001 | 12.25 (5.83–18.67) | <0.0003 |
| Indication | ||||||||
| Central stenosis | 95 | 45.62 | 24.88 | 28.78 | 20.74 (16.02–25.46) | <0.0001 | 16.84 (11.82–21.87) | <0.0001 |
| Lateral recess stenosis | 24 | 41.67 | 26.08 | 26.83 | 15.59 (4.53–26.64) | 0.0068 | 14.84 (3.66–26.01) | 0.0104 |
Results of VAP scoring pre- and postoperatively are shown in Table 2. As back pain can be variable in spinal stenosis, results have been displayed as frequency distributions rather than a mean score.
Table 2.
Back pain levels preoperatively and at 6 weeks and 1 year postoperatively, recorded using the Visual Analogue Score for pain
| N | VAP range | Preop | 6 weeks postop | 1 year postop | 6 weeks change (%) | 1 year change (%) | |
|---|---|---|---|---|---|---|---|
| All | 119 | 0–2 | 25 | 63 | 65 | +152 | +160 |
| 3–4 | 17 | 21 | 13 | +23.5 | −23.5 | ||
| 5–6 | 30 | 14 | 18 | −53.3 | −40 | ||
| 7–8 | 36 | 16 | 16 | −55.6 | −55.6 | ||
| 9–10 | 11 | 5 | 7 | −54.5 | −36.4 | ||
| Gender | |||||||
| Male | 49 | 0–2 | 14 | 26 | 27 | +85.7 | +92.9 |
| 3–4 | 9 | 8 | 5 | −11.1 | −44.4 | ||
| 5–6 | 10 | 4 | 4 | −60 | −60 | ||
| 7–8 | 12 | 7 | 8 | −41.7 | v33.3 | ||
| 9–10 | 4 | 4 | 5 | 0 | +25 | ||
| Female | 70 | 0–2 | 11 | 37 | 38 | +236.4 | +245.5 |
| 3–4 | 8 | 13 | 8 | +62.5 | 0 | ||
| 5–6 | 20 | 10 | 14 | −50 | −30 | ||
| 7–8 | 24 | 9 | 8 | −62.5 | −67 | ||
| 9–10 | 7 | 1 | 2 | −85.7 | −71.4 | ||
| Operation | |||||||
| Laminectomy | 63 | 0–2 | 16 | 38 | 36 | +137.5 | +125 |
| 3–4 | 9 | 12 | 7 | +33.3 | −22.2 | ||
| 5–6 | 18 | 3 | 8 | −83.3 | −55.6 | ||
| 7–8 | 15 | 7 | 8 | −53.3 | −46.7 | ||
| 9–10 | 5 | 3 | 4 | −40 | −20 | ||
| Laminotomy | 56 | 0–2 | 9 | 25 | 29 | +177.8 | +222.2 |
| 3–4 | 8 | 9 | 6 | +12.5 | −25 | ||
| 5–6 | 12 | 11 | 10 | −8.3 | −16.7 | ||
| 7–8 | 21 | 9 | 8 | −57.1 | −61.9 | ||
| 9–10 | 6 | 2 | 3 | −66.7 | −50 | ||
| Indication | |||||||
| Spinal stenosis | 95 | 0–2 | 21 | 51 | 51 | +142.9 | +142.9 |
| 3–4 | 13 | 18 | 12 | +38.5 | −7.7 | ||
| 5–6 | 26 | 12 | 15 | −53.9 | −42.3 | ||
| 7–8 | 26 | 10 | 14 | −61.5 | −46.2 | ||
| 9–10 | 9 | 5 | 5 | −44.4 | −44.4 | ||
| Lateral recess stenosis | 24 | 0–2 | 4 | 12 | 14 | +200 | +250 |
| 3–4 | 4 | 3 | 1 | −25 | −75 | ||
| 5–6 | 4 | 2 | 3 | −50 | −25 | ||
| 7–8 | 10 | 6 | 4 | −40 | −60 | ||
| 9–10 | 2 | 0 | 2 | −100 | 0 | ||
The number of patients reporting LBP of 9–10 reduced by 54.5 % at 6 weeks and 36.4 % at 1 year postoperatively. Similar results were seen for preoperative LBP scores of 5–6 (53.3 % reduction at 6 weeks, 40 % reduction at 1 year) and 7–8 (55.6 % reduction at 6 weeks and 1 year). Using a mean value for preoperative, early postoperative and late postoperative VAS we show a reduction of 2.11 at 6 weeks and 2.08 at 1 year postoperatively (p < 0.0001) (Table 3). There were 18 patients reporting a worsening in pain score at 6 weeks postoperatively. This number rose to 29 at 1 year postoperatively.
Table 3.
Mean back pain levels preoperatively and at 6 weeks and 1 year postoperatively, recorded using the Visual Analogue Score for pain
| n | Preop | 6 weeks postop | 1 year postop | 6 weeks mean reduction (CI) | P value | 1 year mean reduction (CI) | P value | |
|---|---|---|---|---|---|---|---|---|
| All | 119 | 5.14 | 3.03 | 3.07 | 2.11 (1.53–2.69) | <0.0001 | 2.08 (1.38–2.77) | <0.0001 |
Results of VAS scoring for leg pain preoperatively and postoperatively are displayed in Table 4. The frequency of patients reporting pain, scores of 0–2 increased by 914.3 % at 6 weeks and 685.7 % at 1 year postoperatively. There was a decrease in the frequency of scores of 5 or more, with a 90 % decrease in pain scores of 9–10 at 6 weeks and an 80 % decrease at 1 year postoperatively. The shift in frequency distribution towards lower scores postoperatively was more marked in female patients, where there was a 95.2 % decrease in reported scores of 9–10 and a 1,050 % increase in scores of 0–2 at 6 weeks postoperatively. Fifteen patients reported a worsening leg pain at 6 weeks postoperatively. This number increased to 24 at 1 year postoperatively.
Table 4.
Leg pain levels preoperatively and at 6 weeks and 1 year postoperatively, recorded using the Visual Analogue Score
| N | VAP range | Preop | 6 weeks postop | 1 year postop | 6 weeks change (%) | 1 year change (%) | |
|---|---|---|---|---|---|---|---|
| All | 119 | 0–2 | 7 | 71 | 55 | +914.3 | +685.7 |
| 3–4 | 14 | 18 | 20 | +28.6 | +42.9 | ||
| 5–6 | 25 | 14 | 16 | −44 | −36 | ||
| 7–8 | 43 | 14 | 22 | −67.4 | −48.8 | ||
| 9–10 | 30 | 3 | 6 | −90 | −80 | ||
| Gender | |||||||
| Male | 49 | 0–2 | 3 | 25 | 21 | +733.3 | +600 |
| 3–4 | 8 | 10 | 10 | +25 | +25 | ||
| 5–6 | 13 | 5 | 6 | −61.5 | −53.8 | ||
| 7–8 | 16 | 7 | 9 | −56.3 | −43.8 | ||
| 9–10 | 9 | 2 | 3 | −77.8 | −66.7 | ||
| Female | 70 | 0–2 | 4 | 46 | 34 | +1050 | +750 |
| 3–4 | 6 | 8 | 10 | +33.3 | +66.6 | ||
| 5–6 | 12 | 9 | 10 | −25 | −16.7 | ||
| 7–8 | 27 | 7 | 13 | −74.1 | −51.9 | ||
| 9–10 | 21 | 1 | 3 | −95.2 | −85.7 | ||
| Operation | |||||||
| Laminectomy | 63 | 0–2 | 4 | 37 | 31 | +825 | +675 |
| 3–4 | 7 | 11 | 9 | +57.1 | +28.6 | ||
| 5–6 | 16 | 8 | 8 | −50 | −50 | ||
| 7–8 | 21 | 7 | 13 | −66.7 | −38.1 | ||
| 9–10 | 15 | 0 | 2 | −100 | −86.7 | ||
| Laminotomy | 56 | 0–2 | 3 | 34 | 24 | +1033.3 | +700 |
| 3–4 | 7 | 7 | 11 | 0 | +57.1 | ||
| 5–6 | 9 | 6 | 8 | −33.3 | −11.1 | ||
| 7–8 | 22 | 7 | 9 | −68.2 | −59.1 | ||
| 9–10 | 15 | 3 | 4 | −80 | −73.3 | ||
| Indication | |||||||
| Spinal stenosis | 95 | 0–2 | 6 | 55 | 41 | +816.7 | +583.3 |
| 3–4 | 12 | 15 | 17 | +25 | +41.7 | ||
| 5-6 | 22 | 14 | 14 | −36.4 | −36.4 | ||
| 7–8 | 32 | 10 | 19 | −68.8 | −40.6 | ||
| 9–10 | 23 | 2 | 4 | −91.3 | −82.6 | ||
| Lateral recess stenosis | 24 | 0–2 | 1 | 16 | 14 | +1500 | +1300 |
| 3–4 | 2 | 3 | 3 | +33.3 | +33.3 | ||
| 5–6 | 3 | 0 | 2 | −100 | −33.3 | ||
| 7-8 | 11 | 4 | 3 | −63.6 | −72.7 | ||
| 9–10 | 7 | 1 | 2 | −85.7 | −71.4 | ||
Table 5 displays the mean values of recorded VAS preoperatively and at 6 weeks and 1 year postoperatively. These figures show a statistically significant decrease in leg pain at both 6 weeks and 1 year.
Table 5.
Mean leg pain levels preoperatively and at 6 weeks and 1 year postoperatively, recorded using the Visual Analogue Score for pain
| n | Preop | 6 weeks postop | 1 year postop | 6 weeks mean reduction (CI) | P value | 1 year mean reduction (CI) | P value | |
|---|---|---|---|---|---|---|---|---|
| All | 119 | 6.70 | 2.42 | 3.30 | 4.28 (3.62–4.94) | <0.0001 | 3.39 (2.67–4.12) | <0.0001 |
Discussion
The cause of LBP is often multifactorial and can be the result of more than one pathology, therefore the exclusion criteria in this study was restricted to those patients who required secondary stabilisation procedure in addition to the primary decompression surgery. Most patients included are elderly with an average age of 68.2 years and suffer degeneracy. LSS patients often have facet arthrosis, degenerative discs and maybe associated pathology that may explain their back pain. We have included patients with stable spondylolisthesis (seven patients) and one lumbar scoliosis that did not require stabilisation procedure.
There was a significant improvement in LBP in a high proportion of patients undergoing spinal decompression surgery. There are a number of possible explanations.
Patients with LBP often maintain postures of increased lumbar flexion; this improves the diameter of the spinal neural canal and hence the leg pain and walking distance; but this posture may act to provoke LBP [9]. Spinal decompression reduces leg pain, which in turn improves walking distance and gait [10]. This eventually improves posture, and back pain. Spinal decompression has been shown to reduce back pain in up to 96 % of those whose pain has a postural component [2].
During the surgical exposure for spinal decompression, the facet joints are demarcated using cutting diathermy and partial joint resection may produce resection of the branch of the posterior primary ramus that innervates the facet joints. This might well be a factor that eliminates pain derived from distress of these joints. Denervation of the facet joints has been shown to have better perceived effects on LBP when compared to placebo [11], yielding partial to total relief of pain in up to 82 % of cases [12].
Another potential explanation to the improvement of LBP following decompression surgery is the improvement in nutrient supply to ischaemic nerves and the recovery of blood flow [13], and hence improving the claudication pain originating from muscles supplied by the dorsal rami at the stenotic level [14].
Improvement of the radicular leg pain was the overwhelming outcome of lumbar spinal decompression. The improvement of back pain, however, did not correlate to the improvement in leg pain. This indicates that improvement in LBP is not solely due to improved leg pain, and makes it difficult to predict the postoperative prognosis for LBP on an individual basis; but by displaying the results of the VAS as frequency distributions, one can overcome some of this difficulty and be able to inform patients with preoperative LBP of 9–10 that the incidence of reporting such severe pain is less than half at 6 weeks postoperatively.
Conclusion
Patients undergoing spinal decompression have previously been informed that the aim of their surgery is to improve leg pain as opposed to their back pain. Evidence that back pain is often improved after surgery will greatly affect patient expectations. We have shown that LBP significantly improves following spinal decompression alone, and have provided frequency distribution data that should prove useful in managing patient expectations. We have not seen a significant difference in outcome between the sexes, type of operation performed or the indication for the operation, but future research could aim to identify those patients who will have resistant back pain following decompression surgery. We conclude that we can now inform patients that although the aim of spinal decompression surgery is to improve leg pain there is also a decrease in associated LBP.
Conflict of interest
None.
References
- 1.Macfarlane GJ, Beasley M, Jones EA, Prescott GJ, Docking R, Keeley P, McBeth J, Jones GT (2012) The prevalence and management of low back pain across adulthood: Results from a population-based cross-sectional study (the MUSICIAN study). Pain 153(1):27–32. Epub 2011 Oct 5 [DOI] [PubMed]
- 2.Ganz JC. Lumbar spinal stenosis: postoperative results in terms of preoperative posture-related pain. J Neurosurg. 1990;72(1):71–74. doi: 10.3171/jns.1990.72.1.0071. [DOI] [PubMed] [Google Scholar]
- 3.Spivak JM. Degenerative lumbar spinal stenosis. J Bone Jt Surg Am. 1998;80(7):1053–1066. doi: 10.2106/00004623-199807000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Berthelot JM, Bertrand VA, Rodet D, et al. Lumbar spinal stenosis: a review. Rev Rheum Engl Ed. 1997;64:315–325. [PubMed] [Google Scholar]
- 5.Thomé C, Zevgaridis D, Leheta O, Bäzner H, Pöckler-Schöniger C, Wöhrle J, Schmiedek P. Outcome after less-invasive decompression of lumbar spinal stenosis: a randomized comparison of unilateral laminotomy, bilateral laminotomy, and laminectomy. J Neurosurg Spine. 2005;3(2):129–141. doi: 10.3171/spi.2005.3.2.0129. [DOI] [PubMed] [Google Scholar]
- 6.Boonstra AM, Schiphorst Preuper HR, Reneman MF, et al. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res. 2008;31(2):165–169. doi: 10.1097/MRR.0b013e3282fc0f93. [DOI] [PubMed] [Google Scholar]
- 7.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66(8):271–273. [PubMed] [Google Scholar]
- 8.Fairbank JCT, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25(22):2940–2953. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 9.O’Sullivan PB, et al. The relationship beween posture and back muscle endurance in industrial workers with flexion-related low back pain. Man Ther. 2006;11(4):264–271. doi: 10.1016/j.math.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Gionis TA, Groteke E (2003) Spinal decompression. Orthop Technol Rev 5–6. Nov–Dec 2003
- 11.van Wijk, et al. Radiofrequency denervation of lumbar facet joints in the treatment of chronic low back pain: a randomized, double-blind, sham lesion-controlled trial. Clin J Pain. 2005;21(4):335–344. doi: 10.1097/01.ajp.0000120792.69705.c9. [DOI] [PubMed] [Google Scholar]
- 12.Shealy CN (1976) Facet denervation in the management of back and sciatic pain. Clin Orthop Relat Res (115):157–164 [PubMed]
- 13.Carlson GD, Warden KE, Barbeau JM, Bahniuk E, Kutina-Nelson KL, Biro CL, Bohlman HH, LaManna JC. Viscoelastic relaxation and regional blood flow response to spinal cord compression and decompression. Spine. 1997;22(12):1285–1291. doi: 10.1097/00007632-199706150-00002. [DOI] [PubMed] [Google Scholar]
- 14.Porter RW. Spinal stenosis and neurogenic claudication. Spine. 1996;21(17):2046–2052. doi: 10.1097/00007632-199609010-00024. [DOI] [PubMed] [Google Scholar]