Abstract
Study design
Retrospective analysis of 53 patients who underwent single stage simultaneous surgery for tandem spinal stenosis (TSS) at single centre.
Objective
To discuss the presentation of combined cervical and lumbar (tandem) stenosis and to evaluate the safety and efficacy of single-stage simultaneous surgery.
Summary of background data
Combined stenosis is an infrequent presentation with mixed presentation of upper motor neuron and lower motor neuron signs. Scarce literature on its presentation and management is available. There is a controversy in the surgical strategy of these patients. Staged surgeries are frequently recommended and only few single-stage surgeries reported.
Methods
All the patients were clinico-radiologically diagnosed TSS. Surgeries were performed in single stage by two teams. Results were evaluated with Nurick grade, modified Japanese Orthopedic Association score (mJOA), oswestry disability index (ODI), patient satisfaction index, mJOA recovery rate, blood loss and complication.
Results
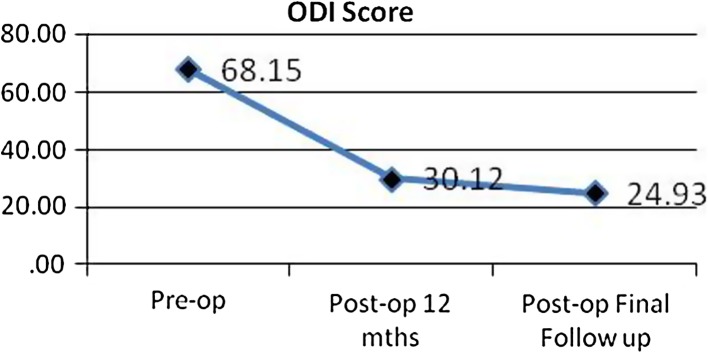
The mJOA cervical and ODI score improved from a mean 8.86 and 68.15 preoperatively to 13.00 and 30.11, respectively, at 12 months and to 14.52 and 24.03 at final follow-up. The average mJOA recovery rate was 48.23 ± 26.90 %. Patient satisfaction index was 2.13 ± 0.91 at final follow-up. Estimated blood loss of ≤400 ml and operating room time of <150 min showed improvement of scores and lessened the complications. In the age group below 60 years, the improvement was statistically significant in ODI (p = 0.02) and Nurick’s grade (p = 0.03) with average improvement in mJOA score.
Conclusion
Short-lasting surgery, single anaesthesia, reduced morbidity and hospital stay as well as costs, an early return to function, high patient satisfaction rate with encouraging results justify single-stage surgery in TSS. Age, blood loss and duration of surgery decide the complication rate and outcome of surgery. Staged surgery is recommended in patients above the age of 60 years.
Keywords: Tandem, Combined, Cervical, Lumbar, Single stage surgery
Introduction
With increased longevity, number of patients with spinal stenosis is increasing. It commonly affects the most mobile segments, i.e., cervical and lumbar [1–3]. Studies have shown that radiographic stenosis is common in the asymptomatic aging population [2, 3]. The clinical presentation varies according to central canal, neural foramina and/or the lateral recess stenosis [4]. Symptomatic degenerative cervical or lumbar spinal stenosis often needs surgical management [5]. Isolated single symptomatic cervical or lumbar stenosis has been frequently reported in the literature, but very few reports of co-existing cervical and lumbar stenosis are available [1, 6–15]. The severity of stenosis in one region may mask the symptoms of the other [6].
Concurrent cervical and lumbar stenosis was first reported by Teng et al. [8]. Dagi et al. [6] were the first to coin the term tandem spinal stenosis. The patients present with a complex clinical picture (combined UMN and LMN signs) of predominant symptoms of either cervical or lumbar stenosis initially. The diagnosis and subsequent treatment are the dilemma. Neurogenic claudication is the major clinical diagnostic feature of lumbar stenosis, whereas cervical stenosis presents with myelopathy and/or radiculopathy. The classic clinical TSS triad consists of (1) intermittent claudication, (2) mixed upper and lower extremities symptoms and signs, and (3) progressive gait disturbances [6, 11]. The gait disturbances vary and include pseudotabetic proprioceptive disturbances, mild-to-moderate proximal lower extremity weakness, and a flexed posture to relieve back/lower extremity pain with compensatory neck hyperextension to facilitate gaze above the horizon [6].
The incidence of TSS has been reported to range from 0.12 to 28 % [1, 6, 7]. Its possibility should always be considered in the primary management of patients with isolated cervical or lumbar spinal stenosis [7].
TSS being uncommon, there is still a controversy in the surgical strategy of these patients. Staged surgery (cervical followed by lumbar [1, 6, 12, 14] or vice versa [11]) or simultaneous surgery [10, 12, 13] has been advocated. Although not statistically determined, most would choose decompression of one region in accordance with each patient’s predominant clinical symptoms and regard one-staged decompression as too invasive in this elderly group [9, 11].
The purpose of this retrospective study is to contribute to literature the largest analysis of TSS patients clinical presentation and outcome of single staged surgery.
Materials and methods
Between January 2003 and March 2012, consecutive 72 patients were operated for TSS at our center. 53 patients had a follow-up of more than 1 year, which was kept as minimum follow-up period for inclusion in the study. Medical records of these 53 patients were reviewed for demographics including age, gender, duration of UE and LE symptoms (in months), first onset of symptoms (UE or LE), onset to presentation interval (≤1 year, 1–5 year or ≥5 years),co-morbidities and length of follow-up. Acute deterioration on chronic existing symptoms was also assessed as any increase in the symptoms before 1 month of surrendering for surgery. All the patients were followed until death or minimum 12 months after surgery.
The radiological severity of cervical and lumbar stenosis was analyzed with quantitative grading systems. Morphological grades of stenosis for cervical by Kang et al. [16] and lumbar by Schizas et al. [17] were used, respectively. Cervical T2 sagittal images were selected for grading. Description of the grading is as follows. Grade 0: the absence of central canal stenosis. Grade 1: nearly complete obliteration of subarachnoid space, including obliteration of the arbitrary subarachnoid space exceeding 50 %, without signs of cord deformity. Grade 2: central canal stenosis with cord deformity but without spinal cord signal change. Grade 3: presence of spinal cord signal change near the compressed level. In lumbar stenosis the grading is based on the CSF/rootlet ratio as seen in the axial T2 images in supine MRI acquisition. Description of the grading is as follows: Grade A: there is clearly CSF visible inside the dural sac, but its distribution is inhomogeneous: A1, the rootlets lie dorsally and occupy less than half of the dural sac area. A2, the rootlets lie dorsally, in contact with the dura but in a horseshoe configuration. A3, the rootlets lie dorsally and occupy more than half of the dural sac area. A4, the rootlets lie centrally and occupy the majority of the dural sac area. Grade B: the rootlets occupy the whole of the dural sac, but they can still be individualized. Some CSF is still present giving a grainy appearance to the sac. Grade C: no rootlets can be recognized, the dural sac demonstrating a homogeneous gray signal with no CSF signal visible. There is epidural fat present posteriorly. Grade D: in addition to no rootlets being recognizable, there is no epidural fat posteriorly. For decision making, consideration is Grade A as no or minor stenosis, B as moderate stenosis, C as severe stenosis, and D as extreme stenosis. The MRI scans were performed using various MRI scanners using different protocols and all studies were accepted irrespective of the quality of the obtained images.
All were operated under general anaesthesia in prone position with horse-shoe extension for head holding. Injection methylprednisolone 1 g dose was given intra-operatively. Single-stage simultaneous cervical and lumbar surgeries were performed by two teams. A separate set of instruments was used so that there is no interference with each other. Cervical laminectomy or laminoplasty at involved levels (all grade 2/3) was done (Fig. 1). Lumbar laminectomy was done in severe stenosis (grade C/D). Wide fenestration was done for patients with moderate stenosis (grade B). Pedicle screws with locally harvested bone grafts and interbody cage were used for lumbar fusion (Transforaminal interbody fusion) in patients with instability (Fig. 2). In cases of more than two levels of fixations, instead of interbody fusion posterolateral bone grafting was done. Drains were kept at both surgical sites and removed on the 3rd postoperative day. Routine analgesic and antibiotic protocols were followed. Patients were progressively mobilized from the 2nd postoperative day. Hemoglobin level above 10 g/dl was maintained with blood transfusion when required. Patients were discharged by 4th/5th postoperative day with supervised physiotherapy and gait training as tolerated. Follow-up was done every 6 weeks and as required.
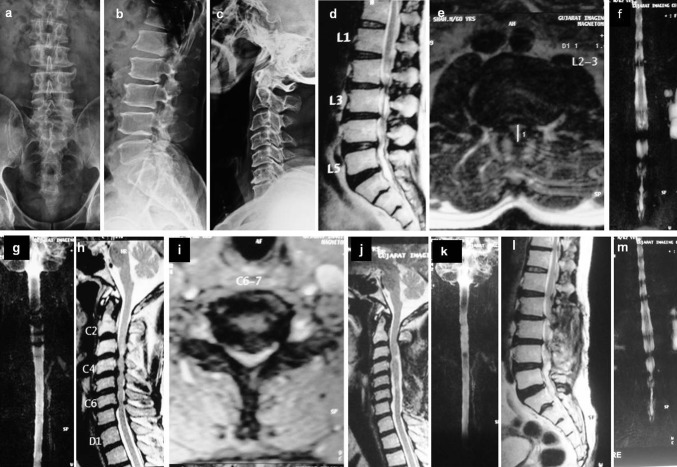
Fig. 1.
a, b X-ray lumbar AP and lateral; c X-ray cervical lateral; d, h MRI T2 sagittal shows multilevel lumbar stenosis and cervical multilevel grade ‘3’ stenosis; e, i MRI T2 axial shows grade ‘C’ L2–L3 stenosis and C 6–7 severe stenosis; f, g MR myelogram lumbar and cervical spine shows compression; j, l Postoperative T2 sagittal MRI and MR myelogram (k, l) shows decompression following laminectomy
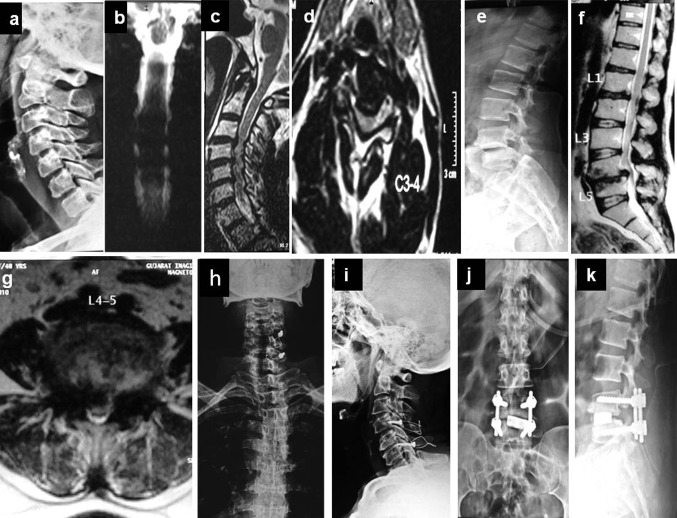
Fig. 2.
a X-ray of cervical spine lateral view; b, c MR myelogram and MRI T2 sagittal cervical spine showing multilevel stenosis with cord edema at C3–4 (grade 3 stenosis); d MRI T2 axial shows C3–4 stenosis; e X-ray lumbar spine lateral shows L4–L5 listhesis; f MRI T2 sagittal showing significant stenosis with listhesis of L4–5. g MRI T2 axial shows L4–L5 grade ‘C’ stenosis; h, i postoperative X-ray shows open door laminoplasty with wiring to lateral mass screws; j, k postoperative X-ray shows L4–L5 TLIF
The clinical results were evaluated according to Nurick’s score (1972) [18] and the modified Japanese Orthopaedic Association (mJOA) score [18] for cervical myelopathy, Patient satisfaction index [9, 19] and ODI score for low back [20]. mJOA recovery rate (expressed as %) was calculated as follows:
 |
The evaluation of outcome was done preoperatively, then postoperatively at 6 months, at 1 year and at final follow-up. As an indirect measure of assessment for invasiveness of a single staged surgery, amount of blood loss intraoperatively (≤200 ml or >200 ml) and total amount including loss in drain (≤400 ml or >400 ml), ORT (≤150 or >150 min) and the units of packed cell transfusion required were analyzed. ORT was the total time for both cervical and lumbar surgeries from beginning of the surgery to end. The number of cervical or lumbar surgery, type of surgery, the use of instrumentation and type of fusion were also analyzed. The complications were assessed. Complications were graded as major or minor. Major complications were those which had an effect on the final outcome. Minor complications were the one which did not have an effect on the final outcome and were managed conservatively.
Statistics
Patients’ demographics and characteristic categorical variables were analyzed. Mean ± 2SD (minimum and maximum) for applicable variables were calculated. Each category was compared using appropriate statistical tools like Pearson correlations, unpaired Student t test and paired t test. The software used is epi info version 3.5.1. 2005.(http://www.cdc.gov/epiinfo).
Results
The analysis is tabulated (Table 1). 53 patients (19 men and 34 women) had a follow-up period of an average 35.76 ± 22.17 (12–88) months. The average patient age was 63.28 ± 9.8 (43–88) years. Mean symptom duration was 28.96 ± 41.29 (1–240) months for lower limb and 17.02 ± 16.50 (1–72) months for upper limb. 33 (62.3 %) patients and 20 (37.7 %) patients had onset of symptoms in lower limbs and upper limbs, respectively. Onset to presentation interval was <1 year in 22 (41.5 %) patients, 1–5 years in 25 (47.2 %) patients and >5 years in 6 (11.3 %) patients.
Table 1.
Analysis of variables
| Variables | Preop mJOA | mJOA 12 months | Change in mJOA | Preop ODI | ODI 12 months | Change in ODI | Preop NG | NG 12 months | Change in NG | No of Complications |
|---|---|---|---|---|---|---|---|---|---|---|
| All patients | 8.86 | 13.57 | 2.67 | 68.15 | 30.11 | 20.31 | 3.83 | 2.23 | 1.16 | 0.79 |
| Age (years) | ||||||||||
| <60 | 9.66 | 15 | 4.89 | 75.89 | 26.31 | 49.58 | 3.66 | 1.66 | 2 | 0.5 |
| >60 | 8.44 | 13 | 4.37 | 63.92 | 32.19 | 35.74 | 3.91 | 2.54 | 1.51 | 0.91 |
| p value | 0.173 | 0.02 | 0.51 | 0.04 | 0.22 | 0.018 | 0.33 | 0.08 | 0.033 | 0.21 |
| EBL (ml) | ||||||||||
| <400 | 9.03 | 14.16 | 5.13 | 67.03 | 25.83 | 41.2 | 3.58 | 1.84 | 1.74 | 0.81 |
| >400 | 8.62 | 12.65 | 3.73 | 69.89 | 36.77 | 39.59 | 4.18 | 2.85 | 1.59 | 0.73 |
| p value | 0.64 | 0.02 | 0.59 | 0.67 | 0.02 | 0.775 | 0.01 | 0.02 | 0.559 | 0.81 |
| IBL (ml) | ||||||||||
| ≤200 | 9.25 | 14 | 5.16 | 66.94 | 26.72 | 40.22 | 3.53 | 1.84 | 1.69 | 0.75 |
| >200 | 8.25 | 12 | 3.62 | 70.17 | 35.82 | 41.03 | 4.28 | 2.89 | 1.67 | 0.81 |
| p value | 0.25 | 0 | 0.04 | 0.62 | 0.05 | 0.891 | 0 | 0 | 0.94 | 0.85 |
| ORT (min) | ||||||||||
| <150 | 9.96 | 14.43 | 4.48 | 65.54 | 26.23 | 39.31 | 3.57 | 2.09 | 1.48 | 0.52 |
| >150 | 8 | 12.86 | 4.6 | 70.3 | 33.31 | 41.5 | 4.03 | 2.36 | 1.83 | 0.97 |
| p value | 0.02 | 0.01 | 0.871 | 0.46 | 0.12 | 0.7 | 0.05 | 0.41 | 0.16 | 0.14 |
| First onset | ||||||||||
| UE | 8.15 | 14 | 5.55 | 68.64 | 27.98 | 40.66 | 3.85 | 1.89 | 2.05 | 0.9 |
| LE | 9.31 | 13 | 3.94 | 67.85 | 31.38 | 40.46 | 3.81 | 2.43 | 1.45 | 0.7 |
| p value | 0.18 | 0.43 | 0.032 | 0.9 | 0.47 | 0.973 | 0.89 | 0.1 | 0.02 | 0.56 |
| Acute precipitation | ||||||||||
| Acute on chronic | 7.78 | 13 | 4.54 | 63.42 | 31.75 | 37.6 | 4.04 | 2.36 | 1.88 | 0.96 |
| Chronic | 9.72 | 14 | 4.55 | 71.73 | 28.87 | 42.86 | 3.65 | 2.13 | 1.52 | 0.62 |
| p value | 0.02 | 0 | 0.989 | 0.19 | 0.53 | 0.359 | 0.1 | 0.49 | 0.497 | 0.286 |
| Fixation | ||||||||||
| Done | 8.77 | 14 | 4 | 74.8 | 33.89 | 40.02 | 3.55 | 1.88 | 1.92 | 0.85 |
| Not done | 10.15 | 15 | 4.73 | 70.35 | 26.61 | 40.7 | 3.7 | 2.25 | 1.6 | 0.75 |
| p value | 0.7 | 0.9 | 0.401 | 0.14 | 0.44 | 0.917 | 0.51 | 0.28 | 0.273 | 0.794 |
| Coexisting disease | ||||||||||
| Absent | 8.72 | 13.50 | 4.60 | 67.54 | 30.39 | 39.93 | 3.79 | 2.17 | 1.71 | 0.67 |
| Present | 10.20 | 14.20 | 4.00 | 73.77 | 27.61 | 46.17 | 4.20 | 2.80 | 1.40 | 1.80 |
| p value | 0.311 | 0.517 | 0.635 | 0.566 | 0.72 | 0.52 | 0.323 | 0.255 | 0.479 | 0.033 |
| Symptoms duration | ||||||||||
| ≤1 year | 7.71 | 12 | 4.32 | 70.68 | 33.87 | 39.3 | 4.18 | 2.6 | 1.82 | 0.64 |
| >1 year | 9.64 | 14 | 4.71 | 66.51 | 27.69 | 41.37 | 3.58 | 2 | 1.52 | 0.87 |
| p value | 0.02 | 0 | 0.6 | 0.52 | 0.18 | 0.722 | 0.01 | 0.07 | 0.357 | 0.47 |
| Cervical levels | ||||||||||
| ≤2 level | 7.95 | 13 | 5 | 67.66 | 31.91 | 43.38 | 3.81 | 2.22 | 1.59 | 0.91 |
| >2 level | 9.53 | 14 | 4.23 | 68.51 | 28.75 | 38.44 | 3.83 | 2.24 | 1.74 | 0.68 |
| p value | 0.06 | 0.09 | 0.3 | 0.89 | 0.49 | 0.39 | 0.93 | 0.96 | 0.56 | 0.47 |
| Lumbar levels | ||||||||||
| ≤1 level | 9.25 | 14 | 4.81 | 68.77 | 26.41 | 42.36 | 3.56 | 1.87 | 1.69 | 0.78 |
| >1 level | 8.25 | 13 | 4.14 | 67.1 | 36.35 | 37.61 | 4.23 | 2.84 | 1.67 | 0.76 |
| p value | 0.25 | 0.04 | 0.38 | 0.8 | 0.03 | 0.42 | 0 | 0 | 0.95 | 0.95 |
Each variable’s mean is written in the first two rows and p value in third row. p value <0.05 is considered significant
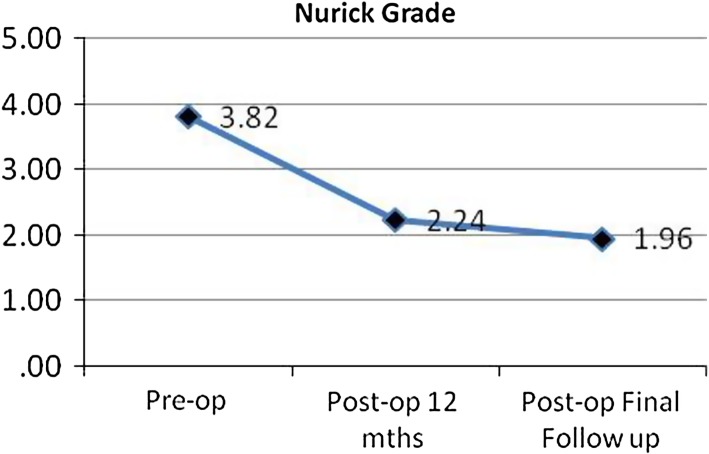
All the patients had grade 3 cervical stenosis. The grade of lumbar stenosis was grade B (n = 4), grade C (n = 14) and grade D (n = 35), respectively. 48 cervical laminectomy and 5 laminoplasty were done. 40 lumbar laminectomy, 4 wide fenestration and 13 fusions (10 TLIF and 3 pedicle screw fixation with posterolateral bone grafting) were done. Average ORT of surgery was 171.28 ± 48.13 (90–270) min. Average units of blood transfused were 0.81 ± 1.00 (1–4 units). Average IBL was 203.96 ± 63.74 ml (80–400) and EBL was 394.71 ± 131.14 (130–750) ml. Average preoperative mJOA was 8.86 ± 3.06 and mJOA at 12 months was 13.00 ± 2.26, giving average improvement of 4.1 points. The average preoperative ODI was 68.15 ± 22.77 and ODI at 12 months was 30.11 ± 16.27, giving an average improvement of 38 points. mJOA and ODI further improved to 14.53 ± 1.83 and 24.03 ± 18.39 at final follow-up. The average preoperative NG was 3.83 ± 0.87, which improved to 2.23 ± 1.16 at 12 months and further remained stabilized at 1.96 ± 1.17 at final follow-up. The average patient satisfaction index was 2.13 ± 0.91 at final follow-up. The average mJOA recovery rate was 48.23 ± 26.90 %.
There were two major complications. One patient had septicemia following urinary tract infection and the patient died at 3 weeks postoperatively. The other patient developed pulmonary embolism following TKR 3 months postoperative and died. It may or may not be related to spine surgery, but we have considered in our result analysis. Other two patients died due to cerebral malaria and myocardial infarction, respectively, after 1 year. 19 patients reported minor complications with some patient having multiple complications. Deep vein thrombosis occurred in two patients (who remained uneventful later), bilateral C5 palsy occurred in five patients (four recovered), UTI occurred in five patients, hyponatremia and reversible paralytic ileus in eight patients, transient renal function alteration in four patients, superficial infection in one, wound gaping requiring re-suturing in two and dual tear requiring primary repair in three cases occurred. All these complications did not have an effect on the final outcome except for one patient of C5 palsy who did not recover. But, they did increase the hospital stay. 48 patients had at least one coexisting disease. The diseases were diabetic neuropathy (n = 16), ischemic heart disease (n = 12), hypertension (n = 20), rheumatoid arthritis (n = 1), hypothyroid (n = 9) and obesity (n = 19), respectively.
The surgical improvement was measured by assessing difference between preoperative and postoperative score at 12 months of mJOA, ODI and Nurick’s grade. The improvement of all the three scores was significant (p = 0.01) (Figs. 3, 4, 5). The mJOA, ODI or NG outcome achieved at 1 year remained stabilized and further improved at final follow-up (p = 0.01) at an average of 35.76 ± 22.17 months.
Fig. 3.
Line diagram of mJOA impovement
Fig. 4.
Line diagram of ODI impovement
Fig. 5.
Line diagram of NG impovement
In the age group below 60 years, the improvement was statistically higher in terms of ODI (p = 0.02) and Nurick’s grade (p = 0.03). There was no statistical significant difference in the two age groups in terms of change in mJOA score, though the average of improvement of mJOA was higher in the age group below 60 years (4.89). There was a positive but small association between preoperative low mJOA and the number of complications (p = 0.05, r = 0.28). Statistically significant difference was observed for mJOA score (p = 0.02) and for Nurick grade (p = 0.00) 12 months after surgery, when compared on the basis of patients age (<60 years and ≥60 years). The mean number of complications noted in the age group above 60 years was higher (0.91); there is no statistically significant difference in the number of complications found in patients in the two age groups. Significant number of patients ≥60 years age reported minor complications (r = 0.28, p = 0.03), but not major complication.
There is a strong negative correlation between preoperative and postoperative 12 months mJOA score (p = 0.00, r = −0.684) and significant positive correlation between preoperative and postoperative ODI scores (p = 0.05, r = −0.510).
The improvement in mJOA score was significantly higher (p = 0.04) when the IBL was <200 ml. But, there was no significant effect of IBL on ODI and Nurick’s grade improvement. When the EBL is <400 ml, the average improvement in mJOA, ODI and Nurick’s grade was higher but it is statistically insignificant. The mean number of complications noted in the group with IBL <200 ml was lower (0.75), but no statistical significance was noted when the IBL was ≥200 ml and EBL ≥400 ml.
The increase in ORT ≥150 min had no statistically significant effect on the improvement in mJOA, ODI and NG. The mean number of complications increased (0.97) when the ORT ≥150 min, but it was statistically insignificant.
On assessment of onset of the first symptoms (UE or LE), statistical significance was noted for improvement in mJOA (p = 0.03) and NG (p = 0.02) but not for ODI. Acute deterioration of symptoms within 1 month before the surgery showed no significant improvement in mJOA, ODI or NG at 12 months.
No statistically significant improvement in mJOA, ODI or NG outcome was noted with fixation in either cervical or lumbar spine. The average number of complications increased with either fixation (0.85), but it was statistically insignificant.
There is a significant positive correlation between blood transfusion and improvement of ODI (r = 0.357, p = 0.009). There is no relationship between mJOA and NG improvement with blood transfusion.
The presence of coexisting diseases neither statistically deteriorate the mJOA, ODI or NG outcome, nor does it increase the complications.
No statistically significant improvement in mJOA, ODI or NG outcome was noted when the symptom duration was ≥1 year. The average number of complications increased when the symptom duration was ≥1 year (0.87), but it was statistically insignificant.
Cervical and lumbar grade of stenosis, levels of involvement (Table 2) and surgery had no statistically significant improvement in mJOA, ODI, NG outcome or complications.
Table 2.
Number of cervical and lumbar levels of stenosis operated
| Cross tabulation | No. of lumbar levels | Total | |||
|---|---|---|---|---|---|
| 1 | 2 | 3 | |||
| No. of cervical levels | 1 | 3 | 4 | 2 | 9 |
| 2 | 9 | 4 | 0 | 13 | |
| 3 | 11 | 3 | 1 | 15 | |
| 4 | 8 | 2 | 3 | 13 | |
| 5 | 1 | 2 | 0 | 3 | |
| Total | 32 | 15 | 6 | 53 | |
Discussion
An abnormal imaging finding has been reported in 24–37 % of asymptomatic cases and all of them are not surgical indications [12, 21]. The differential diagnosis of TSS includes other UMN diseases [6, 10, 22] and peripheral vascular disease [23]. Constitutional narrow spinal canal [4] and ankylosing spinal hyperostosis [24] could be predisposing factors for TSS. These cases were excluded in our study. As an indirect measurement of invasiveness of the surgery in our study, it was found that with IBL <200 the improvement in mJOA outcome was higher (p = 0.04) and average number of complication was lower. ORT ≤150 min reduces the average number of complications, but does not have any statistically significant effect on the outcomes. Only one paper comparing simultaneous and staged procedure concluded that irrespective of surgical algorithm, combined surgical ORT >150 min and blood loss of >400 ml had higher complication rate [13]. Blood loss in our series is much less as compared to index paper. This variation may be due to the surgical technique, two teams and the lesser ORT. There is a significant positive correlation between blood transfusion and improvement of ODI (r = 0.357, p = 0.009). It is suggested that the hemoglobin level in these group of patients should be maintained above 10 g %. Also cautious approach to prevent hyponatremia, paralytic ileus and alteration in RFT should be taken by maintaining adequate hydration and salt intake. Although the duration from the onset of the symptoms to the first consultation varied in our patients (1 month–7 years), there was an acute episode of aggravation of symptoms (n = 18) which led them to surgery in chronic symptomatic patients. Thus, in spite of early first symptoms, there was a delay in the surgical treatment. Similar acute precipitation and delay in surgical treatment were noted by others also [6].
Postoperative improvement correlated inversely with symptom duration in some studies [6, 25]. But, the duration of symptoms of >1 year did not deteriorate the outcomes in our series. The onset of first symptom (UE/LE) did prognosticate outcome in our study. The onset of symptoms in UE increased the chances of improvement of outcome. Prognosis for patients with TSS and myelopathy is no worse than for patients with isolated cervical spondylitic myelopathy, while for those in whom symptoms of lumbar radiculopathy and neurogenic claudication predominate, the prognosis parallels that of isolated lumbar stenosis [12]. The predictors of surgical outcome prognosis can be considered in isolated lumbar or cervical stenosis with preoperative neurologic severity, the transverse area of the compressed spinal cord and newly recommended cerebrospinal fluid nitric oxide metabolites [25]. In our series also significantly low mJOA and high ODI scores led to poor outcomes.
Although, non-operative therapy should initially be recommended in all cases of lumbar spinal stenosis [26], cervical myelopathy requires early surgical consideration [11, 25, 27]. Likewise, TSS also requires early surgical intervention [1, 6–8, 11]. In cases with symptomatic TSS, staged procedures have the dilemma regarding the choice of the region to be addressed first. Proponents of cervical first believe that the lumbar tracts passing through cervical region get decompressed while addressing the cervical region and thereby improving lumbar symptoms [12, 28]. Cervical cord decompression often results in improvement in lumbar symptoms with resolution of pain, spasticity, and sensory deficits of myelopathic origin. However, latent symptoms of intermittent claudication of lumbar stenosis are not affected by cervical decompression. [1] The proponents of lumbar first surgery believe that improved lumbar stoop following surgery leads to flexion attitude of neck creating more space in cervical canal [6].
Failure to detect cervical stenosis in a patient presenting predominantly with lumbar stenosis may carry significant risk of injury to the cervical cord during positioning for lumbar decompression surgery [14]. Whole spine screening (T2 sagittal) at least for elderly patients is recommended for detecting double existing pathologies [29].
The phenomenon of late deterioration after initial postoperative improvement is well recognized in cervical myelopathy [25, 27]. In TSS, late deterioration because of other systemic comorbidities is also noted [10]. The mJOA, ODI or NG outcome achieved at 1 year remained stable and further improved at final follow-up (p = 0.01) of an average 35.76 months in our study. Though, further long-term outcome still needs to be seen. The presence of coexisting diseases neither statistically deteriorate the mJOA, ODI or NG outcome, nor does it increase the complications in our study. One of our patients needed TKR at 3 months for osteoarthritis knee and he died with pulmonary embolism in postoperative period and one patient had myocardial infarction. So late outcomes may be influenced by coexisting diseases.
In our series, patients with greater than 60 years had more complications. Thus, these patients may be considered for staged surgery. According to Eskander et al. [13], also age increases the risks of major and minor complications regardless of the surgical algorithm chosen to manage TSS. In our series, no association was reported between outcome and involved levels of surgery (cervical and lumbar) and whether fixation was done or not. Though, there was an obvious increase in ORT and blood loss which, in turn, increased the average number of complications (0.85).
In carpel tunnel syndrome with additional cervical compressive radiculopathy (double crush syndrome), optimal results are obtained with decompression at both levels [30]. In the field of artificial joint surgery, concept of bilateral total knee arthroplasty and bilateral total hip arthroplasty under single anesthesia has come into being in this decade [31]. Also in spine circumferential fusions, single stage surgery is recommended as morbidity in two staged single admission surgery is as high as 24 % [32]. One-staged surgery for TSS also have many benefits. Simultaneous procedure reduces the surgical duration, blood loss, hospital stay and costs resulting in an early return to function in these morbid elderly patients single team [10, 12, 13].
The surgical improvement was measured by the difference between preoperative and postoperative score at 12-month mJOA, ODI and NG. It showed significant improvement (p = 0.01) suggesting the better outcome of surgery. NG, ODI and mJOA scores in our patients improved more as compared to other studies (Table 3). Though they are standard outcome measures, this may be due to the subjective method or the more severe score grades on presentation in our patients.
Table 3.
Comparative outcome measures in various studies
| References | No. of pts | Single(I) or staged surgery (II) | Nurick’s Score | ODI Score | mJOA Score | mJOA recovery rate % | Patient satisfaction index | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Preop | Postop# | Preop | Postop# | Preop | Postop# | |||||
| Present series | 53 | I | 3.83 | 1.96 | 68.15 | 24.93 | 8.8 | 14.48 + 1.89 | 48.23 ± 26.90 | 2.41 ± 1.48 |
| Aydogant.al. [11]. | 8 | II | NA | NA | 58.1 | 19.3 | 8.1 | 12.7 | NA | NA |
| Kikuike et al. [10] | 17 | I | NA | NA | NA | NA | 14.4 ± 6.1* | 14.8 ± 9.5* | 13.3 ± 88.8* | 2.1 ± 0.8 |
| Eskander et al. [13] | 21 | I | NA | NA | 60.64 | 23.18 | 10.14 | 12.45 | NA | NA |
| 22 | II | NA | NA | 62.38 | 22.67 | 9.90 | 12.10 | NA | NA | |
NA not applicable. Scoring not done by the respective authors
#Score at final follow-up
* The authors have modified the mJOA score
Our study is a retrospective analysis and it has many limitations also. The major limitation of the present study is that the long-term results beyond 7 years are not available. The quantitative measurement tools of stenosis like dural sac cross-sectional area are more accurate tools, but not available everywhere. However, the grading system used are enough to be applied consistently and to be understood and learned, especially when MRI acquisitions have not followed the same protocols and were from different referrals. The advanced modality of treatment like minimal invasive cervical laminoplasty, lumbar laminoplasty, spinous process splitting decompression, or cross over decompression is not done at our centre. Though, they may be the standard of care at advanced spine care setups. Another limitation of the study is the subjective criteria used for the evaluation. But, they are all standard outcome measures. Postoperative MRI was not done in all patients due to economic constraints in our patients. No comparative study with staged surgery group was done. It is also unknown whether the alteration in treatment has resulted in better outcome. The data are heterogeneous with regard to the age, presentation, preoperative outcome scores, number of levels, the grade of stenosis, instrumentation, type of fusion, etc. Thus, the final analysis dilutes the weight of data. Also, the study was conducted at a single centre, which perhaps limits its generalization. Although, the relatively limited number of subjects evaluated in the present series does not allow us to make any definite conclusions regarding the optimal strategies for managing TSS, there are a number of findings that are clearly of great interest to practitioners. However, to the best of our knowledge, it remains a relatively large series in the available literature and the overall results support the safety of single-stage two-team surgery.
Conclusion
Though TSS occurs relatively infrequently, the unrecognized occurrence in the general population may be higher. Detailed examination for even subtle signs followed by whole spine MRI (T2 sagittal) screening should be done. A single stage simultaneous surgery by two teams gives favorable results. The patients older than 60 years should be considered for staged surgery to reduce complications. Lower EBL/IBL and ORT are important to improve the outcome. Thus, only experienced teams should undertake these challenging cases in single stage.
Acknowledgments
We thank Dr. Rajesh Chudasama, Associate Professor, Community Medicine Department, Medical College, Rajkot, Gujarat and Miss Anitha Sunil, Assistant Professor, LJIMS, Ahmedabad for their support for statistical analysis.
Conflict of interest
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Abbreviations
- AP
Anteroposterior
- EBL
Estimated blood loss
- IBL
Intraoperative blood loss
- LMN
Lower motor neuron
- mJOA
Modified Japanese orthopaedic association
- MRI
Magnetic resonance imaging
- NG
Nurick’s grade
- ODI
Oswestry disability index
- ORT
Operation room time
- TLIF
Transforaminal lumbar interbody fusion
- TSS
Tandem spinal stenosis
- UMN
Upper motor neuron
References
- 1.Epstein NE, Epstein JA, Carras R, et al. Coexisting cervical and lumbar spinal stenosis: diagnosis and management. Neurosurgery. 1984;15(4):489–496. doi: 10.1227/00006123-198410000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Okada E, Matsumoto M, Fujiwara H, Toyama Y. Disc degeneration of cervical spine on MRI in patients with lumbar disc herniation: comparison study with asymptomatic volunteers. Eur Spine J. 2011;20(4):585–591. doi: 10.1007/s00586-010-1644-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matsumoto M, Okada E, Toyama Y, Fujiwara M, Momoshima S, Takahata T. Tandem age-related lumbar and cervical intervertebral disc changes in asymptomatic subjects. Eur Spine J. 2012;22(4):708–713. doi: 10.1007/s00586-012-2500-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Edwards WC, Larocca SH. The developmental segmental sagittal diameter in combined cervical and lumbar spondylosis. Spine. 1985;10(1):42–49. doi: 10.1097/00007632-198501000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Dendra H, Kimura S, Yamazaki A, Hosana N, Imura K, et al. Clinical significance of cerebrospinal fluid nitric oxide concentrations in degenerative cervical and lumbar diseases. Eur Spine J. 2011;20(4):604–611. doi: 10.1007/s00586-010-1663-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dagi TF, Tarkington MA, Leech JJ. Tandem lumbar and cervical spinal stenosis: natural history, prognostic indices, and results after surgical decompression. J Neurosurg. 1987;66(6):842–849. doi: 10.3171/jns.1987.66.6.0842. [DOI] [PubMed] [Google Scholar]
- 7.Laban MM, Green ML. Concurrent (tandem) cervical and lumbar spinal stenosis: a 10-yr review of 54 hospitalized patients. Am J Phys Med Rehabil. 2004;83(3):187–190. doi: 10.1097/01.PHM.0000113405.48879.45. [DOI] [PubMed] [Google Scholar]
- 8.Teng P, Papatheodorou C. Combined cervical and lumbar spondylosis. Arch Neurol. 1964;10:298–307. doi: 10.1001/archneur.1964.00460150068007. [DOI] [PubMed] [Google Scholar]
- 9.Hsieh CH, Huang TJ, Hsu RW. Tandem spinal stenosis: clinical diagnosis and surgical treatment. Changgeng Yi Xue Za Zhi. 1998;21(4):429–435. [PubMed] [Google Scholar]
- 10.Kikuike K, Miyamoto K, Hosoe H, Shimizu K. One-staged combined cervical and lumbar decompression for patients with tandem spinal stenosis on cervical and lumbar spine: analyses of clinical outcomes with minimum 3 years follow-up. J Spinal Disord Tech. 2009;22(8):593–601. doi: 10.1097/BSD.0b013e3181929cbd. [DOI] [PubMed] [Google Scholar]
- 11.Aydogan M, Ozturk C, Mirzanli C, et al. Treatment approach in tandem (concurrent) cervical and lumbar spinal stenosis. Acta Orthop Belg. 2007;73(2):234–237. [PubMed] [Google Scholar]
- 12.Naderi S, Mertol T. Simultaneous cervical and lumbar surgery for combined symptomatic cervical and lumbar spinal stenoses. J Spinal Disord Tech. 2002;15(3):229–231. doi: 10.1097/00024720-200206000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Eskander MS, Aubin ME, Balsis SM, Eck J, Drew JM, et al. Is there a difference between simultaneous or staged decompression for combined cervical and lumbar stenosis. J Spinal Disord Tech. 2011;24(6):409–413. doi: 10.1097/BSD.0b013e318201bf94. [DOI] [PubMed] [Google Scholar]
- 14.Zulkefli A, Ramanathan R. Tandem spinal stenosis. Malays Orthop J. 2010;4(1):46–49. doi: 10.5704/MOJ.1003.010. [DOI] [Google Scholar]
- 15.Caron TH, Bell GR. Combined (tandem) lumbar and cervical stenosis. Semin Spine Surg. 2007;19(1):44–46. doi: 10.1053/j.semss.2007.01.009. [DOI] [Google Scholar]
- 16.Kang Y, Lee JW, Koh YH, Hur S, Kim SJ, Chai JW, Kang HS. New MRI grading system for the cervical canal stenosis. AJR. 2011;197(1):134–140. doi: 10.2214/AJR.10.5560. [DOI] [PubMed] [Google Scholar]
- 17.Schizas C, Theuman N, Burn A, Tansey R, Wardlaw D, et al. Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine. 2010;35(21):1919–1924. doi: 10.1097/BRS.0b013e3181d359bd. [DOI] [PubMed] [Google Scholar]
- 18.William KE, Paul R, Dewan Y. Functional outcome of corpectomy in cervical spondylitic myelopathy. Indian J Orthop. 2009;43(2):205–209. doi: 10.4103/0019-5413.50855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Toyone T, Tanaka T, Kato D, et al. Patients’ expectations and satisfaction in lumbar spine surgery. Spine. 2005;30(23):2689–2694. doi: 10.1097/01.brs.0000187876.14304.15. [DOI] [PubMed] [Google Scholar]
- 20.Fairbank JCT, Pynsent PB. The oswestry disability index. Spine. 2000;25(22):2940–2952. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 21.Teresi LM, Lufkin RB, Reicher MA, et al. Asymptomatic degenerative disk disease and spondylosis of the cervical spine: MR imaging. Radiology. 1987;164(1):83–88. doi: 10.1148/radiology.164.1.3588931. [DOI] [PubMed] [Google Scholar]
- 22.Opstelten FW, Boon AJ. Suspected amyotrophic lateral sclerosis? Don’t forget diagnostic imaging of the spine. Ned Tijdschr Geneeskd. 2001;145(11):505–509. [PubMed] [Google Scholar]
- 23.Dodge LD, Bohlman HH, Rhodes RS. Concurrent lumbar spinal stenosis and peripheral vascular disease. A report of nine patients. Clin Orthop Relat Res. 1998;230:141–148. [PubMed] [Google Scholar]
- 24.Laroche M, Moulinier L, Arlet J, et al. Lumbar and cervical stenosis. Frequency of the association, role of the ankylosing hyperostosis. Clin Rheumatol. 1992;11(4):533–535. doi: 10.1007/BF02283114. [DOI] [PubMed] [Google Scholar]
- 25.Fager CA. Results of adequate posterior decompression in the relief of spondylitic cervical myelopathy. J Neurosurg. 1973;38(6):684–692. doi: 10.3171/jns.1973.38.6.0684. [DOI] [PubMed] [Google Scholar]
- 26.Amundsen T, Weber H, Nordal HJ, et al. Lumbar spinal stenosis: conservative or surgical management? A prospective 10-year study. Spine. 2000;25(11):1424–1435. doi: 10.1097/00007632-200006010-00016. [DOI] [PubMed] [Google Scholar]
- 27.Mann KS, Khosla VK, Gulati DR. Cervical spondylitic myelopathy treated by single-stage multilevel anterior decompression. A prospective study. J Neurosurg. 1984;60(1):81–87. doi: 10.3171/jns.1984.60.1.0081. [DOI] [PubMed] [Google Scholar]
- 28.Richter M, Kluger P, Puhl W. Diagnosis and therapy of spinal stenosis in the elderly. Z Orthop Ihre Grenzgeb. 1999;137(6):474–481. doi: 10.1055/s-2008-1039374. [DOI] [PubMed] [Google Scholar]
- 29.Han IH, Suh SH, Kuh SU, Chin DK, Kim KS. Types and prevalence of coexisting spine lesions on whole spine sagittal MR images in surgical degenerative spinal diseases. Yonsei Med J. 2010;51(3):414–420. doi: 10.3349/ymj.2010.51.3.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Osterman AL. The double crush syndrome. Orthop Clin North Am. 1998;19(1):147–155. [PubMed] [Google Scholar]
- 31.Taneja T, Kumar R, Amin A, et al. Bilateral simultaneous total knee replacements: the Harlow experience. J Bone Joint Surg Br. 2009;92:328. [Google Scholar]
- 32.Passias PG, Ma Y, Chiu YL, Mazumdar M, Girardi FP, Memtsoudis SG. Comparative safety of simultaneous and staged anterior and posterior spinal surgery. Spine. 2012;37(3):247–255. doi: 10.1097/BRS.0b013e31821350d0. [DOI] [PMC free article] [PubMed] [Google Scholar]