Abstract
Purpose
The purpose of this cohort study was to classify sagittal standing alignment of pre-peak height velocity (pre-PHV) girls, and to evaluate whether identified subgroups were associated with measures of spinal pain. This study further aimed at drawing attention to similarities and differences between the current postural classification and a previous system determined among pre-PHV boys.
Methods
557 pre-PHV girls [mean age, 10.6 years (SD, 0.47 years)] participated in the study. Three gross body segment orientation parameters and five specific lumbopelvic characteristics were quantified during habitual standing. Postural subgroups were determined by cluster analysis. Logistic regression was applied to assess the relationship between postural subgroups and spinal pain measures (pain and seeking care, assessed by self-administered questionnaire). Chi-square statistics, independent samples T test, and distribution-based methods were used for comparison with postural categorization in pre-PHV boys.
Results and conclusion
Among pre-PHV girls, clinically meaningful posture clusters emerged both on the gross body segment and specific lumbopelvic level. The postural subtypes identified among pre-PHV girls closely corresponded to those previously described in pre-PHV boys, thereby allowing the use of the same, working nomenclature. In contrast to previous findings among pre-PHV boys, no associations between posture clusters and spinal pain measures were significant in girls at pre-PHV age. When comparing discrete ‘global’ alignment scores across corresponding posture types, some intriguing differences were found between genders which might involve different biomechanical loading patterns. Whether habitual posture forms a risk factor for developing spinal pain up to adulthood needs evaluation in prospective multifactorial follow-up research.
Keywords: Posture, Sagittal balance, Classification, Adolescent, Spinal pain
Introduction
Postural classification appears to be part of routine clinical practice. For sagittal standing alignment among a general population of pre-peak height velocity (pre-PHV) boys, Dolphens et al. [1] have recently published an innovative classification system thereby providing a refinement of several other classification systems. The concepts that underlie this grading system were derived from clinical and scientific publications [2–8] as well as from clinical experience. Essentially, posture characteristics that might have clinical relevance were quantified using a screening protocol with clinical applicability and were incorporated into a consistent clustering framework in which the clinical relevance of the identified posture types was appreciated in terms of their association with spinal pain measures [1]. As such, a two-level subject typology emerged with each case classified first as one of three major categories that was based on the interrelation between three gross body segment orientations with respect to the gravity vector (legs, trunk, and body segments). Next, each case was further allocated into a lumbopelvic subcategory according to recurring characteristic postural patterns defined from five lumbopelvic shape and orientation parameters. Specifically, the resulting ‘global’ cluster proportions among healthy pre-PHV boys were 41.6 % neutral, 31.1 % sway-back, and 27.2 % leaning-forward. Neutral global alignment was characterized by a small pelvic displacement angle (i.e., little forward translation of the pelvis over the base of support as measured at the ankle), small trunk lean angle (i.e., limited tilt of the trunk with respect to the vertical), and an intermediate body lean angle that is close to 0 (i.e., the vertical projection of the C7 spinous process is close to the lateral malleolus). Sway-back was characterized by an intermediate pelvic displacement angle (i.e., slight forward carriage of the pelvis relative to the base of support), large trunk lean angle (i.e., a backward trunk lean relative to the hips), and a large (positive) body lean angle (i.e., the C7 spinous process line passes well behind the lateral malleolus). Leaning-forward was characterized by a large pelvic displacement angle, an intermediate trunk lean angle, and a small (negative) body lean angle (i.e., the vertical projection of the C7 spinous process is anterior to the lateral malleolus). Among pre-PHV boys, a meaningful and working nomenclature also existed on the lumbopelvic level with posture types closely corresponding to clinical insights. However, in terms of clinical importance (i.e., the cross-sectional association between sagittal plane posture and spinal pain measures), the proposed classification could be simplified to a ‘global’ alignment categorization as far as its possible role in the development of spinal pain symptoms was concerned among pre-PHV boys: higher odds for measures of low back pain (LBP) and neck pain (NP) were found in those boys classified as having sway-back compared with those classified as having neutral overall alignment, whereas spinal pain measures did not differ between the groups of the lumbopelvic subclassification [1]. To date, such data are lacking for girls who are within the same crucial phase of musculoskeletal development, i.e., before the age of attainment of PHV.
The primary aim of the current study was to construct a classification scheme of sagittal standing alignment within a general population of pre-PHV girls, and to evaluate whether identified subgroups were associated with spinal pain measures thereby establishing the clinical significance of the proposed classification system. The secondary aim was to draw attention to major similarities and differences between the current classification scheme among pre-PHV girls and the previous among pre-PHV boys.
Materials and methods
Study design
This school-based study was designed as an initial cross-sectional baseline study where participating subjects underwent a screening protocol consisting of sagittal standing alignment assessment and an evaluation of a wide range of potential posture-associated factors. The current study focuses on postural classification and its association with spinal pain among a representative sample of pre-PHV girls.
Sample
The present study analyzed data from an established cohort of healthy pre-PHV girls [3, 5]. The methodology and sample have been described in detail previously [1, 3, 5]. Briefly, 557 fifth-grade girls (mean age 10.6 ± 0.47 years) took part in this study. Exclusion criteria included a history of neurologic conditions, rheumatic disorders, metabolic or endocrine diseases, major congenital anomalies, skeletal disorders (major leg length discrepancy, spondylolysis, spondylolisthesis, major scoliosis), connective tissue disorders, previous spinal fracture or previous spinal surgery.
All youngsters and guardians gave written informed consent prior to participation and ethical approval was granted by the Ethics Committee of the Ghent University Hospital.
Measures
The testing procedure involved sagittal plane posture assessment during habitual standing and completion of self-reported spinal pain measures.
Measurement of habitual standing posture
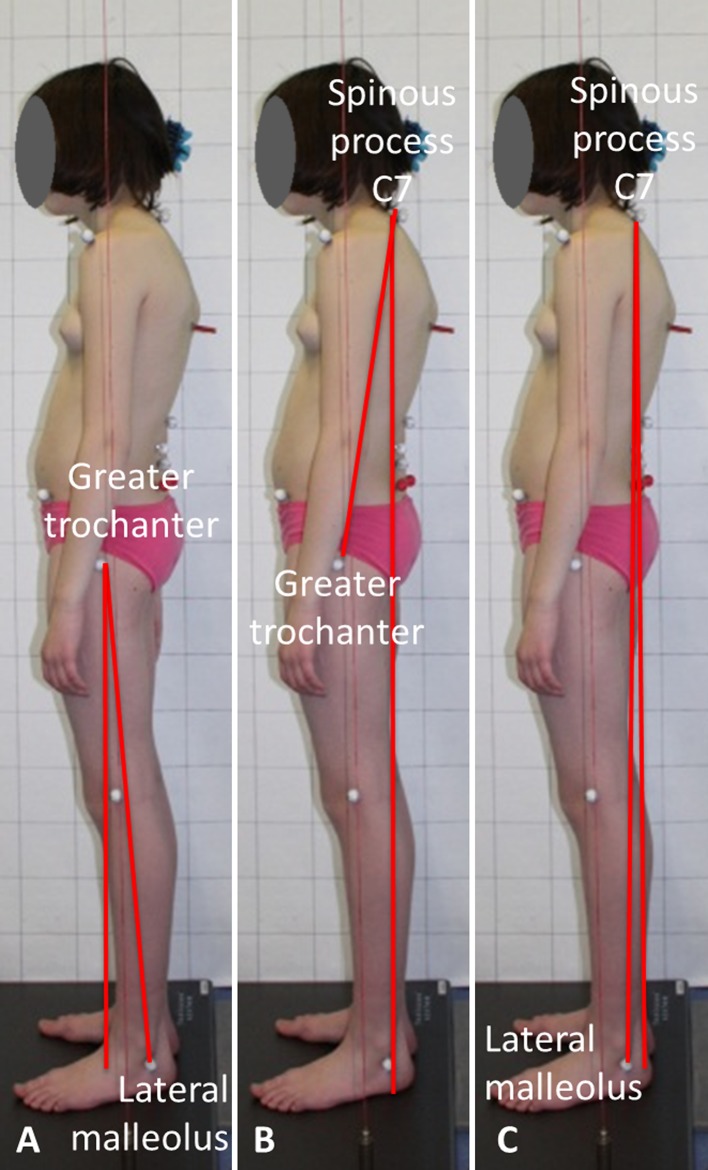
Gross body segment orientations and lumbopelvic shape/orientation indices were quantified using post hoc analysis of digitized photographs of participants and direct body measurements (i.e., digital inclinometry, wheeled accelerometry (spinal mouse), and visual inspection and palpation), respectively. More specifically, three angular measures of gross body segment orientation with respect to the gravity line (pelvic displacement, trunk lean, and body lean angle; Fig. 1) and five lumbopelvic parameters (pelvic tilt, sacral inclination, lumbar lordosis, vertebral level of the lumbar apex, and number of vertebrae constituting the ‘lumbar’ curve) were quantified and were used to develop the classification scheme (see “Statistical analysis”).
Fig. 1.
Definitions of postural angles describing global sagittal alignment. a Pelvic displacement angle, b trunk lean angle, c body lean angle
Visual inspection, palpation and marker placement were performed once per participant. This was done by one trained examiner (MD, a physiotherapist specialized in orthopedic rehabilitation and manual therapy) before photography, wheeled accelerometry and digital inclinometry took place. Photographs and measurements of the pelvic tilt, sacral inclination and lumbar lordosis were taken three times (viz., once at the end from each of three standing trials). Procedures for collection and processing of the indicators of ‘global’ and ‘local’ posture have been detailed elsewhere [1, 3, 5]. The intertrial reliability of the ‘gross’ posture parameters has been shown to be good in pre-PHV girls, with the intraclass correlation coefficients ICC(2,1) for absolute agreement ranging from 0.65 to 0.76 and with standard error of measurements (SEM) ranging from 0.62° to 1.25° (unpublished data); for lumbopelvic parameters, the ICC(2,1) and corresponding SEM ranged from 0.72 to 0.89 and from 1.44° to 3.71°, respectively, indicating good to excellent intertrial reliability within this population [3].
Questionnaire on spinal complaints
Self-administered questionnaires assessed spinal pain measures [1, 3, 9]. The questions relevant to this study included an inquiry about lifetime prevalence, 1-month prevalence, and doctor visit for LBP, NP, or thoracic spine pain (TSP) (“yes” or “no”).
Statistical analysis
Data were analyzed using PASW Statistics version 18.0 (Chicago: SPSS Inc., 2009) and Matlab version 7.10.0. (Natick, Massachusetts: TheMathWorks Inc., 2010) with statistical significance set at α = 0.05.
Postural subgroups were determined using cluster analysis. Both hierarchical (Ward’s) and non-hierarchical (K-means) clustering procedures were conducted, with the quality and stability of the clustering solutions being investigated using dendrograms, scree- and silhouette plots, ANOVA’s and post hoc tests (Bonferroni correction), validation samples (two random samples of approximately 50 % of all cases), and clinical meaningfulness assessment. In a first step, the clustering procedure was conducted on the three gross body segment orientation parameters to obtain subgroups of overall sagittal alignment. Next, the clustering procedure was repeated on the five lumbopelvic parameters to determine the lumbopelvic subclasses within each group of the global alignment categorization. The different clusters were given labels that characterize the postural pattern. Further detail on the cluster analysis procedure can be found in Dolphens et al. [1]. To examine the association of posture clusters with spinal pain measures, binary logistic regression (enter method) was used. Adequate model fit was assessed using the model Chi-squared likelihood ratio test and Hosmer–Lemeshow goodness of fit test.
Additionally, gender differences in proportions of the key posture categories were tested with Chi-square statistics. To this end, the posture data set of pre-PHV boys described previously [1] was used besides the current data set of pre-PHV girls. Within corresponding posture types, differences between genders in mean scores on discrete posture parameters were evaluated with the independent samples T test (statistical significance assessment) and distribution-based methods using the effect size (ES) and minimal important difference (MID) (clinical relevance estimation). A description of these latter concepts and methods can be found elsewhere [5, 10].
Results
Postural grouping according to the sagittal standing profile
On the gross body segment level, the three-cluster solution was found to be adequate and meaningful regarding the different postural patterns found. The frequencies and mean values of each global alignment cluster, as well as the results of univariate analysis on the variables between subgroups are displayed in Table 1. The postural patterns of the three clusters were similar to those described previously among pre-PHV boys [1] and were termed as follows: cluster 1, neutral; cluster 2, sway-back; cluster 3, leaning-forward. The neutral cluster (1) was characterized by low scores on pelvic displacement and trunk lean, and moderate values (close to 0) for body lean angle. The sway-back group (cluster 2) had moderate pelvic displacement angle scores and high values for trunk and body lean. Characteristic of the leaning-forward cluster (cluster 3) were the high scores on pelvic displacement together with the moderate and low (negative) values on trunk lean and body lean, respectively. In Fig. 2, the three-dimensional scatter plot of the global alignment categorization among pre-PHV girls is shown.
Table 1.
Frequencies and mean values of each global cluster from entire sample (N = 557) using K-means clustering procedure
| Univariate analysis for global angular measures | ||||
|---|---|---|---|---|
| Cluster | 1 Neutral 40.0 % (N = 223) |
2 Sway-back 31.8 % (N = 177) |
3 Leaning-forward 28.2 % (N = 157) |
|
| Pelvic displacement angle | 2.8 ± 1.03 (0 to 4.8) | 5.2 ± 1.33 (2.2 to 9.2) | 6.2 ± 1.38 (3.9 to 10.8) | ANOVA: P < 0.001†
Post hoc Bonferroni: P < 0.001†; Neu < SB < LF |
| Trunk lean angle | 5.7 ± 1.75 (0 to 8.8) | 10.2 ± 1.51 (7.6 to 15.2) | 6.9 ± 1.77 (2.1 to 11.4) | ANOVA: P < 0.001†
Post hoc Bonferroni: P < 0.001†; Neu < LF < SB |
| Body lean angle | 8 ± 0.79 (−1.4 to 3.1) | 1.4 ± 0.83 (−1 to 3.8) | −6 ± 0.71 (−3.4 to 6) | ANOVA: P < 0.001†
Post hoc Bonferroni: P < 0.001†; LF < Neu < SB |
Data are reported as [mean ± SD (range)]; all postural parameters in degrees (°)
For pelvic displacement angle, a greater value indicates more forward carriage of the pelvis relative to the feet; for trunk lean angle, a greater value indicates more backward inclination of the trunk with respect to the vertical; for body lean angle, a positive value indicates the vertical projection of the C7 spinous process to be posterior to the lateral malleolus, whereas a negative value indicates the vertical projection of the C7 spinous process to be anterior to the lateral malleolus
Neu neutral, SB sway-back, LF leaning-forward
† P < 0.05
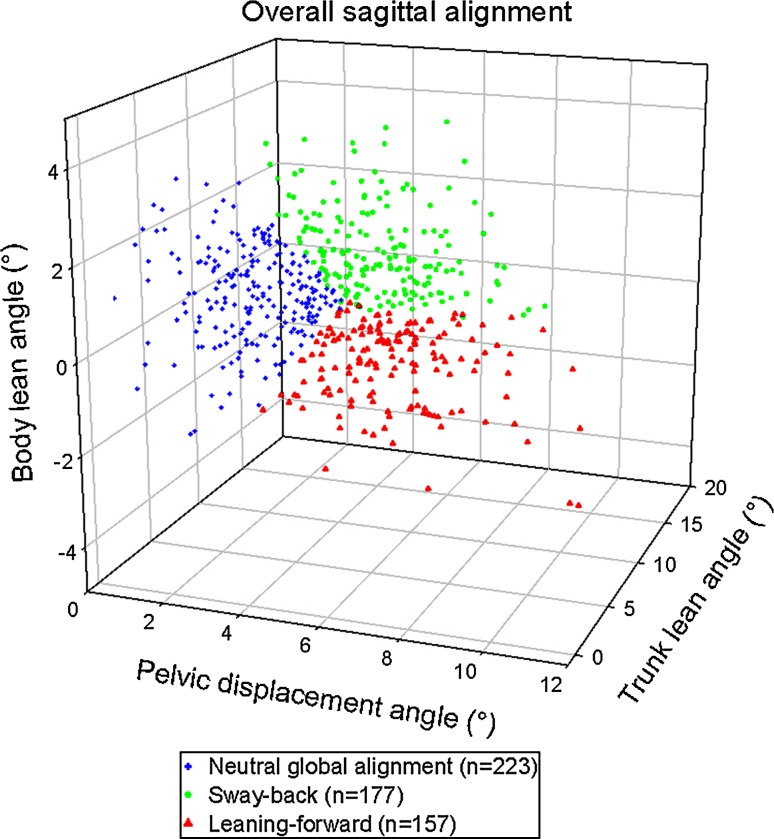
Fig. 2.
Scatter plot showing the pelvic displacement, trunk lean, and body lean angle scores (expressed in degrees). The points correspond to 557 pre-PHV girls who were classified as neutral, sway-back or leaning-forward using cluster analysis on the overall sagittal posture level
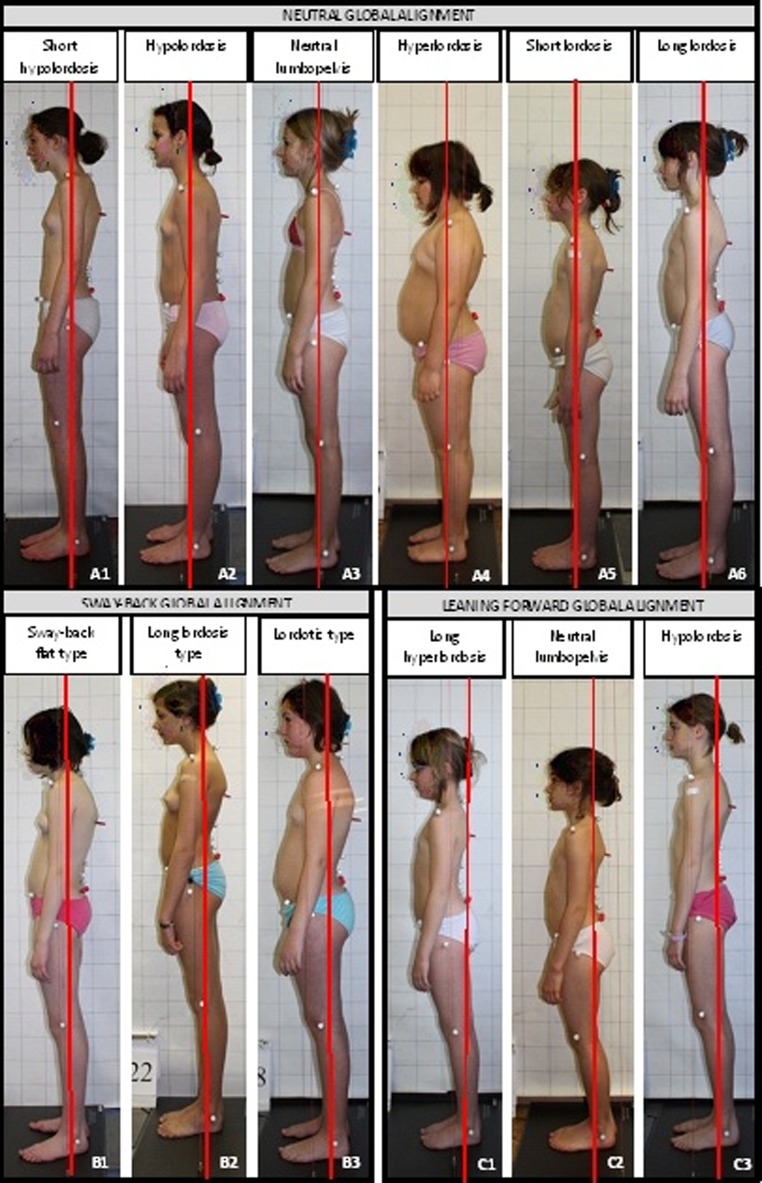
When lumbopelvic clustering was performed within each subgroup of the three-part global alignment classification system, cluster analyses resulted in similar postural subtypes as described previously among pre-PHV boys [1]. In short, 12 lumbopelvic subcategories emerged. Within the neutral global alignment category, 6 postural clusters were obtained. More specifically, clusters 2 (hypolordosis), 3 (neutral lumbopelvis), and 4 (hyperlordosis) were characterized by an average amount of vertebrae included in the lumbar lordosis and by an average position of the lumbar apex. Clusters 1 (short hypolordosis) and 5 (short lordosis), in contrast, had a low inflection point—thereby creating a short lordosis—as well as a low position of the lumbar apex. Characteristic for type 6 (long lordosis) was the high number of vertebrae constituting the lumbar lordosis and the lumbar apex which is located high. The postural subtypes further distinguished among them in terms of the degree of lumbar lordosis, pelvic tilt, and sacral inclination. Analogously, a three-cluster solution was obtained both in the sway-back and leaning-forward clusters. Results and descriptive statistics are detailed in Table 2. A typical member from each posture cluster is depicted in Fig. 3.
Table 2.
Frequencies and mean values of each lumbopelvic cluster within subgroups of the three-part global alignment classification system using K-means clustering procedure
| Univariate analysis for lumbopelvic parameters | |||||||
|---|---|---|---|---|---|---|---|
| Neutral global alignment (N = 221) | |||||||
| 1 Short hypolordosis 14.5 % (N = 32) |
2 Hypolordosis 21.3 % (N = 47) |
3 Neutral lumbopelvis 23.5 % (N = 52) |
4 Hyperlordosis 12.2 % (N = 27) |
5 Short lordosis 13.1 % (N = 29) |
6 Long lordosis 15.4 % (N = 34) |
||
| Lordosis | −22.9 ± 4.58 (−31.0 to −13.3) | −27.0 ± 4.16 (−36.3 to −18.0) | −30.8 ± 3.76 (−36.7 to −20.3) | −42.4 ± 5.19 (−55.7 to −33.7) | −32.5 ± 4.21 (−42.3 to −21.3) | −35.3 ± 5.41 (−44.3 to −24.7) | ANOVA: P < 0.001†
Post hoc Bonferroni: 4 < 6 < 5 = 3 < 2 < 1 |
| No. of lordotic vertebrae | 3.9 ± 0.42 (3.0 to 4.5) | 5.0 ± 0.54 (4.0 to 6.5) | 4.7 ± 0.52 (3.5 to 6.0) | 5.4 ± 0.65 (4.0 to 7.0) | 4.2 ± 0.79 (2.0 to 5.5) | 6.2 ± 0.75 (5.0 to 8.5) | ANOVA: P < 0.001†
Post hoc Bonferroni: 1 = 5 < 3 = 2 = 4 < 6 |
| Lumbar apex | 15.3 ± 0.52 (14.0 to 16.5) | 14.3 ± 0.56 (13.0 to 16.0) | 14.6 ± 0.42 (14.0 to 15.5) | 14.7 ± 0.54 (13.5 to 16.0) | 15.8 ± 0.52 (15.0 to 17.0) | 13.6 ± 0.62 (12.0 to 15.0) | ANOVA: P < 0.001†
Post hoc Bonferroni: 6 < 2 = 3 = 4 < 1 < 5 |
| Pelvic tilt | 9.3 ± 3.45 (−1.5 to 16.0) | 9.9 ± 2.60 (2.2 to 14.2) | 16.2 ± 2.49 (10.9 to 21.6) | 18.3 ± 3.06 (12.2 to 25.5) | 14.2 ± 2.26 (9.6 to 19.2) | 13.3 ± 4.05 (7.0 to 23.2) | ANOVA: P < 0.001†
Post hoc Bonferroni: 1 = 2 < 6 = 5 = 3 < 4 |
| Sacral inclination | 14.4 ± 3.63 (6.3 to 22.3) | 15.9 ± 3.22 (9.3 to 22.7) | 21.3 ± 3.62 (12.0 to 27.0) | 29.5 ± 3.67 (25.0 to 40.3) | 21.8 ± 3.10 (16.7 to 27.7) | 23.0 ± 2.85 (16.7 to 28.0) | ANOVA: P < 0.001†
Post hoc Bonferroni: 1 = 2 < 3 = 5 = 6 < 4 |
| Univariate analysis for lumbopelvic parameters | ||||
|---|---|---|---|---|
| Sway-back (N = 176) | ||||
| 1 Flat type 32.4 % (N = 57) |
2 Long lordosis type 25.6 % (N = 45) |
3 Lordotic type 42.0 % (N = 74) |
||
| Lordosis | −24.8 ± 5.54 (−35.7 to −11.0) | −32.5 ± 5.24 (−42.3 to −21.3) | −35.7 ± 5.58 (−49.7 to −23.7) | ANOVA: P < 0.001†
Post hoc Bonferroni: 3 < 2 < 1 |
| No. of lordotic vertebrae | 4.1 ± 0.60 (3.0 to 5.5) | 5.8 ± 0.68 (4.5 to 7.5) | 4.8 ± 0.64 (3.5 to 6.5) | ANOVA: P < 0.001†
Post hoc Bonferroni: 1 < 3 < 2 |
| Lumbar apex | 15.1 ± 0.60 (14.0 to 17.0) | 13.8 ± 0.55 (12.0 to 14.5) | 15.0 ± 0.62 (14.0 to 17.0) | ANOVA: P < 0.001†
Post hoc Bonferroni: 2 < 3 = 1 |
| Pelvic tilt | 9.2 ± 2.86 (2.4 to 16.6) | 12.4 ± 3.41 (6.3 to 19.4) | 15.6 ± 3.47 (9.1 to 24.5) | ANOVA: P < 0.001†
Post Hoc Bonferroni: 1 < 2 < 3 |
| Sacral inclination | 14.6 ± 5.13 (−2.3 to 25.0) | 18.6 ± 3.97 (7.7 to 25.7) | 22.6 ± 4.59 (11.3 to 32.0) | ANOVA: P < 0.001†
Post hoc Bonferroni: 1 < 2 < 3 |
| Univariate analysis for lumbopelvic parameters | ||||
|---|---|---|---|---|
| Leaning-forward (N = 152) | ||||
| 1 Long hyperlordosis 38.8 % (N = 59) |
2 Neutral lumbopelvis 21.1 % (N = 32) |
3 Hypolordosis 40.1 % (N = 61) |
||
| Lordosis | −33.8 ± 5.77 (−48.0 to −23.0) | −31.8 ± 6.12 (−44.7 to −20.7) | −24.8 ± 5.08 (−33.7 to −10.0) | ANOVA: P < 0.001†
Post hoc Bonferroni: 1 < 2 < 3 |
| No. of lordotic vertebrae | 5.3 ± 0.68 (4.0 to 8.0) | 4.5 ± 0.75 (2.5 to 5.5) | 4.2 ± 0.77 (1.5 to 5.5) | ANOVA: P < 0.001†
Post hoc Bonferroni: 3 = 2 < 1 |
| Lumbar apex | 14.2 ± 0.44 (13.0 to 15.0) | 15.2 ± 0.64 (14.0 to 17.0) | 15.2 ± 0.62 (13.5 to 17.0) | ANOVA: P < 0.001†
Post hoc Bonferroni: 1 < 3 = 2 |
| Pelvic tilt | 18.1 ± 3.60 (10.0 to 26.0) | 13.1 ± 3.22 (5.9 to 22.9) | 11.4 ± 2.76 (5.8 to 18.1) | ANOVA: P < 0.001†
Post hoc Bonferroni: 3 < 2 < 1 |
| Sacral inclination | 22.0 ± 4.22 (10.7 to 32.3) | 23.6 ± 3.79 (14.7 to 31.0) | 15.0 ± 4.11 (3.7 to 23.7) | ANOVA: P < 0.001†
Post hoc Bonferroni: 3 < 1 = 2 |
Data are reported as [mean ± SD (range)]
Lumbar lordosis, pelvic tilt, and sacral inclination in degrees (°); the number of vertebrae constituting the lumbar lordosis was determined via palpation of the inflection point. The vertebral level of the clinical identifiable points of interest (inflection point and lumbar apex) was coded as follows: 9 for T9 level, 10 for T10 level,…13 for L1 level,…17 for L5 level. When a point of interest was, e.g., at the L2–L3 interspace, level was coded as 14.5
For lumbar lordosis, a more negative value indicates a more pronounced curvature; pelvic tilt is positive when the anterior superior iliac spine is inferior to the posterior superior iliac spine; sacral inclination is positive when tilted forward with respect to the vertical
† P < 0.05
Fig. 3.
Standing sagittal lumbopelvic alignment within a the neutral global alignment cluster, b the sway-back global cluster, and c the leaning-forward global cluster
Associations between postural subgroups and spinal pain measures
At pre-PHV age, sagittal plane posture type was not associated with the presence/absence of spinal pain or care seeking in girls.
Comparison of posture types between genders at pre-PHV age
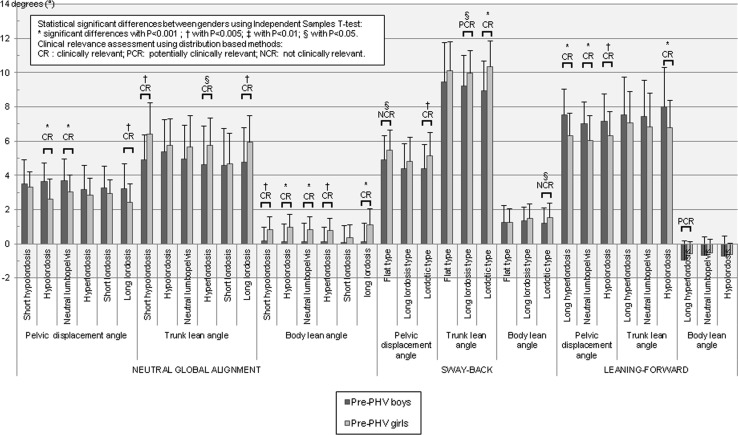
Cluster analysis yielded the same number of posture clusters in pre-PHV girls and boys: a three-part classification system emerged on the ‘global’ alignment level together with 12 lumbopelvic subcategories. The postural patterns were similar in both genders thereby enabling the use of the same cluster terminology. Results of Chi-square testing demonstrated similar proportions of genders within each of the gross body segment postural categories [neutral girls: 40.0 %, 223/557; boys: 41.6 %, 266/639 (χ2(1, 489) = 3.78, P > 0.05)]; sway-back [girls: 31.8 %, 177/557; boys: 31.1 %, 199/639 (χ2(1, 376) = 1.28, P > 0.05)]; leaning-forward [girls: 28.2 %, 157/557; boys: 27.2 %, 174/639 (χ2(1, 331) = 0.87, P > 0.05)]. The mean overall body segment orientation scores for each posture cluster, as well as values for statistical significance and clinical relevance in the comparison between genders are detailed in Fig. 4. A summary of the results on the ‘global’ categorization level (data not shown in Fig. 4) is as follows. Compared to their male counterparts, pre-PHV girls categorized as ‘neutral’ stood with slightly less forward translation of the pelvis over the base of support as measured at the ankle [P < 0.001, potentially clinically relevant (PCR) results] together with slightly more posterior tilt of the trunk with respect to the vertical (P < 0.001, PCR), resulting in a vertical projection of the C7 spinous process that is located more posterior to the lateral malleolus [P < 0.001, clinically relevant (CR) results]. In the case of the ‘non-neutral’ posture types (i.e., sway-back and leaning-forward), analyses revealed the difference in body lean angle between pre-PHV boys and girls to be neither statistically significant nor clinically relevant. However, within the sway-back category pre-PHV girls demonstrated more backward trunk lean (P < 0.001, CR) and slightly more forward translation of the pelvis (P < 0.001, PCR) compared to pre-PHV boys belonging the same postural subgroup. Furthermore, a smaller pelvic displacement angle was observed in leaning-forward girls compared to leaning-forward boys (P < 0.001, CR) together with a slightly less pronounced backward trunk lean with respect to the vertical (P < 0.001, PCR).
Fig. 4.
Mean, standard deviation, and comparison of gross body segment orientation parameters between pre-PHV boys (n = 639) and pre-PHV girls (n = 557) for corresponding postural subgroups including both statistical significance and clinical relevance assessment
Discussion
The sum of these data indicate that pre-PHV girls essentially have the same posture clusters as do pre-PHV boys, both on the gross body segment and lumbopelvic level. No associations between posture clusters and spinal pain measures were significant among pre-PHV girls which appears not to agree with research performed previously among pre-PHV boys [1]. At pre-PHV age, intriguing differences were found between genders when comparing discrete ‘global’ alignment scores across corresponding posture types thereby lending further support to identify and use postural subgroups in clinical research taking into account gender, biological and/or chronological age.
The first objective was to develop a classification system among pre-PHV girls according to their sagittal standing alignment and to compare the identified groups regarding spinal pain measures. Present proposed classification system includes both gross body segment and specific lumbopelvic posture characteristics in a systematic manner and fits with previous research among pre-PHV boys [1] reporting that a clinically meaningful categorization of sagittal standing profile can be achieved if three ‘global’ alignment clusters are distinguished (neutral, sway-back, and leaning-forward), together with 12 lumbopelvic subgroups (Fig. 3). Although these classifications among pre-PHV subjects recognize the heterogeneity of sagittal plane posture, they do not reflect separate and compact entities of sagittal plane posture (Fig. 2) which may, however, not be expected given the continuous nature of the various postural parameters in stance. The association between posture types and spinal pain addresses another issue. At pre-PHV age, gross body segment categorization has been reported to be associated with spinal pain measures at the more mobile regions of the spine in boys [1]. Such associations between posture clusters and pain, however, were not observed within the current cohort of pre-PHV girls. Absence of such associations might be due to the possibility for gender- and/or age-dependent differences in the presence and dominance of posture as a contributing factor within the widely accepted multifactorial nature of spinal pain. Factors that come into play might include biological, mechanical, psychological, cognitive and social factors [11–21]. Alternatively, the association between postural types and spinal pain in pre-PHV boys yet not in girls might suggest that habitual stance in these populations involves different biomechanical loading patterns (see below). As recently put forward by O’Sullivan et al. [22] and Guimond et al. [23], one might also suggest that true spinal pain–posture relationships may be masked by a complexity of interactions between biopsychosocial factors which may be associated with both habitual posture and spinal pain, or, that posture could act as a surrogate measure for other biopsychosocial factors that are the real mechanisms underlying spinal pain. In any case, based on the present study findings, it does not seem justified to label ‘non-neutral’ posture types as postural ‘faults’ in pre-PHV girls since such a designation could result in an inappropriate stratification for risk-determined prevention/therapy of spinal pain in girls before pubertal peak growth. Nonetheless, the current authors recognize the importance of long-term multifactorial follow-up of pre-PHV subjects for a better comprehension of habitual posture as a potential risk factor for developing spinal pain up to adulthood. Although not within the scope of the current contribution, the postural categorization presented here and in Dolphens et al. [1] in healthy subjects before pubertal peak growth might also prove useful in future research on the potential contribution of habitual standing posture to the aggregate risk profile of spinopelvic disorders other than pain, such as (progressive) deformity or early degenerative diseases. It is furthermore interesting to note that a possible change in the list of postural entities is anticipated in the present clustering methodology, thereby allowing an evaluation of how postural patterns set in pre-adolescence change with increasing age.
The second objective was to examine major similarities and differences between the current posture classification system among pre-PHV girls and that proposed previously for pre-PHV boys [1]. These categorizing systems turn out to be similar in that they both rely on gross body segment orientation parameters and specific lumbopelvic features to establish a clinically meaningful two-level subject typology. An equal number of posture clusters was obtained with similar postural patterns, thereby allowing the use of the same terminology across genders. The notion of in-depth comparisons between genders to be made on a ‘global’ alignment level in the current study, was supported by previous study findings establishing that gross body segment orientations appear to be paramount over ‘specific’ lumbopelvic characteristics with respect to their association with spinal pain measures at pre-PHV age [1, 3]. As such, equal percentages of pre-PHV boys and girls were classified in the corresponding ‘overall’ categories. Moreover, for the majority of ‘global’ alignment parameters a highly interesting pattern was found when gender comparisons were made across corresponding posture types: (potentially) clinically relevant differences were shown between genders in addition to statistically significant differences. Combined with previous research reporting that statistical differences in geometric parameters between boys and girls were—at most—questionable clinically relevant when a general pre-PHV population was considered (i.e., when subjects were not classified) [5], these findings may imply the potential for a “wash-out effect” for postural differences between genders caused by the heterogeneity of the values on postural characteristics, thereby lending further support for the need to apply postural subgrouping in clinical research.
Acknowledgments
We express our gratitude to Tom Barbe and Gizem İrem Güvendik for their assistance in data collection, and to all of the school teams, local pupil guidance centers and participants for their cooperation in this study.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Dolphens M, Cagnie B, Coorevits P, Vleeming A, Danneels L. Classification system of the normal variation in sagittal standing plane alignment: a study among young adolescent boys. Spine. 2013;38:E1003–E1012. doi: 10.1097/BRS.0b013e318280cc4e. [DOI] [PubMed] [Google Scholar]
- 2.Guo J, Liu Z, Lv F, et al. Pelvic tilt and trunk inclination: new predictive factors in curve progression during the Milwaukee bracing for adolescent idiopathic scoliosis. Eur Spine J. 2012;21:2050–2058. doi: 10.1007/s00586-012-2409-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dolphens M, Cagnie B, Coorevits P, et al. Sagittal standing posture and its association with spinal pain: a school-based epidemiological study of 1196 Flemish adolescents before age at peak height velocity. Spine. 2012;37:1657–1666. doi: 10.1097/BRS.0b013e3182408053. [DOI] [PubMed] [Google Scholar]
- 4.Chanplakorn P, Wongsak S, Woratanarat P, Wajanavisit W, Laohacharoensombat W. Lumbopelvic alignment on standing lateral radiograph of adult volunteers and the classification in the sagittal alignment of lumbar spine. Eur Spine J. 2011;20:706–712. doi: 10.1007/s00586-010-1626-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dolphens M, Cagnie B, Vleeming A, Vanderstraeten G, Coorevits P, Danneels L. A clinical postural model of sagittal alignment in young adolescents before age at peak height velocity. Eur Spine J. 2012;21:2188–2197. doi: 10.1007/s00586-012-2416-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005;30:346–353. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 7.Bergoin M, Gennari J-M, Tallet J-M. Taking the shoulders and pelvis into account in the preoperative classification of idiopathic scoliosis in adolescents and young adults (a constructive critique of King’s and Lenke’s systems of classification) Eur Spine J. 2011;20:1780–1787. doi: 10.1007/s00586-011-1899-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith A, O’Sullivan P, Straker L. Classification of sagittal thoraco-lumbo-pelvic alignment of the adolescent spine in standing and its relationship to low back pain. Spine. 2008;33:2101–2107. doi: 10.1097/BRS.0b013e31817ec3b0. [DOI] [PubMed] [Google Scholar]
- 9.Staes F, Stappaerts K, Vertommen H, Everaert D, Coppieters M. Reproducibility of a survey questionnaire for the investigation of low back problems in adolescents. Acta Paediatr. 1999;88:1269–1273. doi: 10.1111/j.1651-2227.1999.tb01030.x. [DOI] [PubMed] [Google Scholar]
- 10.Armijo-Olivo S, Warren S, Fuentes J, Magee DJ. Clinical relevance vs. statistical significance: using neck outcomes in patients with temporomandibular disorders as an example. Man Ther. 2011;16:563–572. doi: 10.1016/j.math.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Kovacs FM, Gestoso M, Gil del Real MT, López J, Mufraggi N, Méndez JI. Risk factors for non-specific low back pain in children and their parents: a population based study. Pain. 2003;103:259–268. doi: 10.1016/S0304-3959(02)00454-2. [DOI] [PubMed] [Google Scholar]
- 12.Szpalski M, Gunzburg R, Balagué F, Nordin M, Mélot C. A 2-year prospective longitudinal study on low back pain in primary school children. Eur Spine J. 2002;11:459–464. doi: 10.1007/s00586-002-0385-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Watson KD, Papageorgiou AC, Jones GT, et al. Low back pain in schoolchildren: the role of mechanical and psychosocial factors. Arch Dis Child. 2003;88:12–17. doi: 10.1136/adc.88.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Siivola SM, Levoska S, Latvala K, Hoskio E, Vanharanta H, Keinänen-Kiukaanniemi S. Predictive factors for neck and shoulder pain: a longitudinal study in young adults. Spine. 2004;29:1662–1669. doi: 10.1097/01.BRS.0000133644.29390.43. [DOI] [PubMed] [Google Scholar]
- 15.Briggs AM, Smith AJ, Straker LM, Bragge P. Thoracic spine pain in the general population: prevalence, incidence and associated factors in children, adolescents and adults. A systematic review. BMC Musculoskelet Disord. 2009;10:77. doi: 10.1186/1471-2474-10-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gatchel RJ, Turk DC. Criticisms of the biopsychosocial model in spine care—creating and then attacking a straw person. Spine. 2008;33:2831–2836. doi: 10.1097/BRS.0b013e31817d24ad. [DOI] [PubMed] [Google Scholar]
- 17.Balagué F, Dudler J, Nordin M. Low-back pain in children. Lancet. 2003;361:1403–1404. doi: 10.1016/S0140-6736(03)13148-0. [DOI] [PubMed] [Google Scholar]
- 18.Ståhl M, Mikkelsson M, Kautiainen H, Häkkinen A, Ylinen J, Salminen JJ. Neck pain in adolescence. A 4-year follow-up of pain-free preadolescents. Pain. 2004;110:427–431. doi: 10.1016/j.pain.2004.04.025. [DOI] [PubMed] [Google Scholar]
- 19.Vikat A, Rimpelä M, Salminen JJ, Rimpelä A, Savolainen A, Virtanen SM. Neck or shoulder pain and low back pain in Finnish adolescents. Scand J Public Health. 2000;28:164–173. [PubMed] [Google Scholar]
- 20.Racine M, Tousignant-Laflamme Y, Kloda LA, Dion D, Dupuis G, Choinière M. A systematic literature review of 10 years of research on sex-gender and pain perception—part 2: do biopsychosocial factors alter pain sensitivity differently in women an men? Pain. 2012;153:619–635. doi: 10.1016/j.pain.2011.11.026. [DOI] [PubMed] [Google Scholar]
- 21.Keogh E, Eccleston C. Sex differences in adolescent chronic pain and pain-related coping. Pain. 2006;123:275–284. doi: 10.1016/j.pain.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 22.O’Sullivan PB, Smith AJ, Beales DJ, Straker LM. Association of biopsychosocial factors with degree of slump sitting posture and self-report of back pain in adolescents: a cross-sectional study. Phys Ther. 2011;91:470–483. doi: 10.2522/ptj.20100160. [DOI] [PubMed] [Google Scholar]
- 23.Guimond S, Massrieh W. Intricate correlation between body posture, personality trait and incidence of body pain: a cross-referential study report. PLoS ONE. 2012;7:e37450. doi: 10.1371/journal.pone.0037450. [DOI] [PMC free article] [PubMed] [Google Scholar]