Abstract
Background
The threshold for patients with breast cancer to receive radiation therapy continues to be lowered. I reviewed the literature to determine the clinical impact that the increasing use of radiation therapy has had on the management of patients with breast cancer who desire autologous tissue-based breast reconstruction.
Methods
The MEDLINE database was searched for articles on breast reconstruction and radiation therapy published between January 2008 and June 2011. Abstracts of those articles were reviewed to identify articles that addressed the most pressing radiation-related issues facing reconstructive breast surgeons performing autologous tissue-based reconstruction. This subgroup of articles was reviewed in detail.
Results
Two-hundred eighty-five articles were identified. Seventeen papers were reviewed in detail. Nine papers provided level III evidence, mostly from retrospective comparative studies. Five papers provided level I (n = 2) or II (n = 3) evidence from high-quality multicenter or single-center randomized controlled trials or prospective cohort studies. Three papers provided level IV evidence from case series and were included in the review because they offered a novel approach or perspective. Since my last review of the literature in 2009 there have been changes in the practice patterns in the approach to autologous breast reconstruction in patients who undergo radiation therapy.
Conclusions
With the increasing use of radiation therapy in patients with breast cancer, future studies should seek to provide more meaningful data (level I and II evidence) to help guide clinical decision-making.
INTRODUCTION
The use of postmastectomy radiation therapy (PMRT) has been increasing since the mid-1990s because PMRT has been shown to impart a survival advantage, even in patients with early-stage breast cancer.1 In women who desire breast reconstruction after mastectomy, the sequencing and timing of reconstruction and PMRT and the technique used for breast reconstruction can influence complication rates, radiation delivery, and aesthetic outcomes.
In an article published in Plastic and Reconstructive Surgery in 2009,2 I reviewed the literature on breast reconstruction in patients receiving PMRT and summarized the evidence in an effort to help guide decision making by surgeons and patients. The main conclusions from that review were the following: 1) In patients receiving PMRT, outcomes of implant-based reconstruction are inferior to outcomes of autologous tissue-based reconstruction, regardless of whether the implant is placed before or after PMRT. 2) The presence of a reconstructed breast, whether the breast was reconstructed with autologous tissue, an implant, or a combination, can compromise the design of the radiation fields to treat the internal mammary lymph node basin. 3) Delivery of PMRT to a reconstructed breast can have negative aesthetic consequences, regardless of the method of reconstruction. 4) In patients who will receive PMRT, the optimal approach is delayed autologous tissue-based reconstruction after PMRT. 5) If the need for PMRT is not known at the time of mastectomy but it seems likely that PMRT will be required, initial placement of a tissue expander may be considered.2
I recently reviewed articles on breast reconstruction in patients undergoing PMRT published since the time of our 2009 review. The main issues that I was most interested in exploring were: 1) Does preoperative radiation therapy adversely effect delayed autologous tissue-based reconstruction? 2) Do the direct effects of modern radiation delivery adversely impact the outcome of autologous tissue-based reconstruction? 3) Can immediate, skin-preserving breast reconstruction be performed in patients with advanced stages of breast cancer without compromising oncologic safety? 4) What is the optimal time to perform delayed reconstruction after PMRT and can it be perform safely within less than 1 year of PMRT? 5) Which new strategies are being used to deliver radiation in patients who already had immediate autologous breast reconstruction? Here, I summarize the findings related to autologous tissue-based reconstruction. For the most part, the new studies on autologous tissue-based reconstruction reinforce many of the conclusions from our preceding review however there is new data that sheds a contrasting perspective on the best approach to reconstruction in patients who will require PMRT.
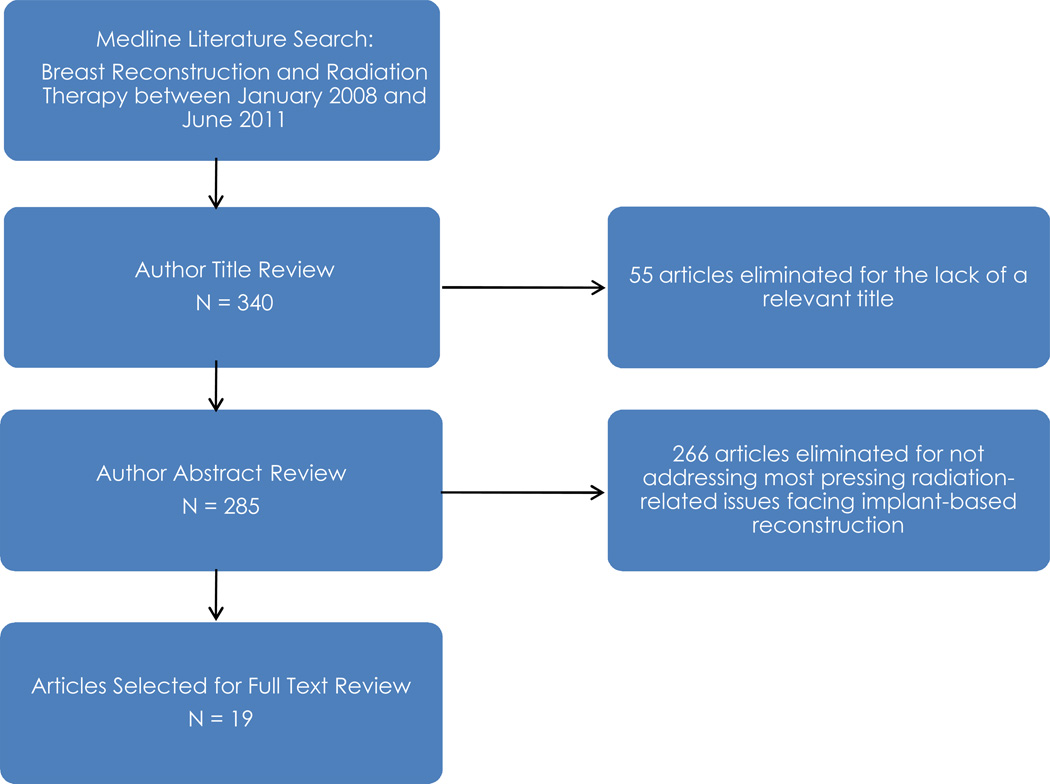
To find articles for review, the author searched the MEDLINE database for studies of radiation therapy and breast reconstruction published between January 2008 and June 2011 (Figure 1). The search terms used were breast reconstruction and radiation therapy. Relevant studies were assigned a level of evidence using the American Society of Plastic Surgeons Evidence Rating Scale for Therapy (Table 1). Two-hundred eighty-five articles were identified, and the abstracts of those articles were reviewed to identify articles that addressed the most pressing radiation-related issues facing reconstructive breast surgeons. This subgroup of articles was reviewed in detail.
Fig. 1.
Citation Attribution Diagram
Table 1.
American Society of Plastic Surgeons Evidence Rating Scale for Therapy
| Level of Evidence |
Qualifying Studies |
|---|---|
| I | High-quality, multicenter or single-center randomized controlled trial with adequate power; or systematic review of these studies. |
| II | Lesser quality, randomized controlled trial; prospective cohort study; or systematic review of these studies. |
| III | Retrospective comparative study; case-control study; or systematic review of these studies |
| IV | Case series |
| V | Expert opinion; case report or clinical example; or evidence based on physiology, bench research, or “first principles” |
Reproduced with permission from Haase SC, Chung KC. An Evidence-Based Approach to Treating Thumb Carpometacarpal Joint Arthritis. Plast Reconstr Surg 127(2):918-25 2011.
OVERVIEW OF ARTICLES INCLUDED IN THE REVIEW
Seventeen articles that addressed the most pressing radiation-related issues facing reconstructive breast surgeons were selected for detailed assessment and included in this review (Table 2). Nine papers provided level III evidence, mostly from retrospective comparative studies. Five papers provided level I (n = 2) or II (n = 3) evidence from high-quality multicenter or single-center randomized controlled trials or prospective cohort studies. Three papers provided level IV evidence from case series and were included in the review because they offered a novel approach or perspective.
Table 2.
Evidence of Impact of Radiation on Breast Reconstructive Technique
| Reference | Level of Evidence |
Reconstructions | Timing of Reconstruction |
Reconstructive Techniques |
Results | Conclusion |
|---|---|---|---|---|---|---|
| Berry T, et al2 | III | 1037 patients | Immediate | 2-stage implant, Autologous (latissimus dorsi; pedicled and five TRAM; DIEP flaps) | Radiation increased the major complication rate of 2-stage implant reconstruction from 21.2 to 45.4%. There was no significant difference between the radiated and non-radiated autologous tissue reconstructions. | Increased major complication with radiated TE, but still successful majority of cases and radiation has no influence on autologous tissue reconstruction. |
| McCarthy CM, e al3 | I | 482 patients | Delayed | Implant | Silicone implants preferred (P=.016) however receipt of PMRT had a significant negative effect on patient satisfaction (P < .000) | Information can be used to optimize patient decision-making. |
| Hvilsom GB, et al4 | II | 717 reconstructions | Delayed | 1– and 2-stage implant | History of PMRT associated with increased risk of severe capsular contracture for 1- and 2-stage procedures. | Breast Reconstruction approaches other than implants should be seriously considered among women who have received radiation therapy. |
| Whitfield GA, et al5 | III | 178 patients | Immediate | 1-and 2-stage implant (TE/I); autologous tissue (latissimus dorsi, pedicled and free TRAM, and DIEP flaps | 110 patients had implant-based reconstruction with a median follow up of 51 months. In the RT group (41 patients), there were 8 patients with severe capsular contracture, a crude rate of 19.5%, and in the unirradiated group, there were no cases of severe capsular contracture (p < 0.001). | This series showed a higher rate of capsular contracture with radiation therapy hypofractionation (40 Gy in 15 fractions over 3 weeks) |
| Khansa I, et al6 | III | 802 reconstructions | Immediate postmastectomy reconstruction after prior BCT (lumpectomy plus radiation therapy) | 2-stage implant (TE/I); autologous tissue (latissimus dorsi, pedicled and free TRAM, and DIEP flaps) | Prior BCT did not correlate with higher complication rates (p = 0.690) or lower satisfaction (p = 0.559); however, there was a higher rate of mastectomy skin flap necrosis with prior BCT compared to no prior BCT (12.4% versus 6.8%, p = 0.024). | Prior BCT does not increase overall complication rates or reduce satisfaction with breast reconstruction after completion mastectomy. |
| Roostaeian J, et al7 | IV | 35 patients | Immediate | Direct to Implant (1 stage implant) | Patients who receive PMRT had a significant (P=0.047) need for revision and lower mean in aesthetic scores than patients who did not receive PMRT (2.46 versus 3.19, respectively). | Immediate implant breast reconstruction safe and viable option. Recommend caution and patient counseling with history of PMRT. |
| Gross E, et al8 | II | 141 patients | Immediate | 2-stage implant | Baker 1 and 2 capsular contracture in 67.5%, Baker 3 and 4 in 32.5%. 32 reconstruction failures. | Highest risk with immediate 2-stage implant in patients with large tumors T3/T4, smokers, and positive axillary nodes. |
| Jhaveri JD, et al9 | II | 92 patients | Immediate | 2-stage implant (TE/I); autologous tissue (latissimus dorsi, pedicled and free TRAM, and DIEP flaps) | The rate of grade 3 or 4 complications (necessitating surgical intervention or removal or replacement of reconstructed breast) was 33.3% for TE/I versus 0% for autologous tissue (p = 0.001). Acceptable cosmesis was reported in 51% of TE/I versus 82.6% of autologous tissue reconstruction (p = 0.007). | In patients undergoing PMRT after immediate reconstruction, autologous tissue-based reconstruction is associated with fewer long-term complications and better cosmetic results than reconstruction with a tissue expander plus an implant. |
| Lee BT, et al10 | III | 919 reconstructed breasts | Immediate; Delayed | 2-stage; Autologous with implant; Autologous only | Overall complication rates of patients who received PMRT before or after were higher than control group (no PMRT) (39.66% versus 23.16%; P<0.001). | Proper counseling of patients who may need PMRT, including her timing of reconstruction and PMRT may affect type of reconstruction. |
| McKeown DJ, et al11 | III | 24 patients | Immediate; Delayed | Autologous Latissimus Dorsi | Trend toward better outcomes in patients undergoing delayed reconstruction after PMRT than immediate reconstruction before PMRT, with volume and contour (upper pole) being most affected. | Similar patient satisfaction between 2 groups but most patients would have preferred immediate reconstruction before PMRT, so continue to offer immediate autologous latissimus reconstruction, yields satisfactory outcome. |
| Barry M, Kell MR12 | III | 1105 (meta-analysis) | Immediate; delayed | 2-stage implant (TE/I); autologous tissue (latissimus dorsi, pedicled and free TRAM, and DIEP flaps) | Patients undergoing PMRT were more likely to suffer morbidity compared to patients not undergoing PMRT. When PMRT was delivered after breast reconstruction, autologous reconstruction was associated with less morbidity than implant-based reconstruction. | PMRT has a detrimental effect on breast reconstruction outcome. When PMRT is delivered after immediate reconstruction, use of an autologous tissue flap results in less morbidity than implant-based reconstruction. |
| Parsa AA, et al1,13 | II | 170 patients | Delayed | 2-stage bilateral implant (PMRT to only 1side of chest wall) | Patients who develop induration or severe post-radiation skin changes, have a greater rate of Baker class IV capsular contracture and poor results that range from 75% to 100% of reconstructed breasts. | A history of chest wall radiation should not exclude a patient from receiving tissue expander/implant reconstruction, especially patients who do not have severe skin changes or induration. |
| Chang D, et al14 | III | 1000 patients | Delayed | 2-stage implant; latissimus plus implant; TRAM plus implant | Fewer reconstruction failures when TRAM or latissimus combined with implant than with implant alone. | The addition of flap to implant in a previously irradiated breast has lower rates of implant loss. |
| Kronowitz SJ, et al15 | II | 47 patients | Delayed-delayed | Tissue expander placement at mastectomy to preserve breast skin followed by a delayed autologous tissue-based reconstruction after PMRT using preserved breast skin | The protocol group had a lower rate of complications of definitive breast reconstruction than the standard delayed-reconstruction group (24% versus 38%). There was no difference in 3-year recurrence-free survival rates between the groups. | Patients with advanced breast cancer may be able to undergo skinpreserving breast reconstruction after PMRT. |
| Koutcher L, et al16 | III | 41 patients | Immediate | 2-stage implant (TE/I) | In 73% of patients, all chest wall borders were adequately covered, and in 22%, all borders but 1 were adequately covered; 30-month actuarial local control was 97%. | Women undergoing immediate expander-implant reconstruction, PMRT can achieve excellent local control with acceptable heart and lung doses |
| Classen J, et al17 | IV | 109 patients | Immediate | 2-stage implant (TE/I); autologous tissue (latissimus dorsi, pedicled and free TRAM, and DIEP flaps) | After a mean follow-up of 34 months, the 3-year incidence of ≥grade III fibrosis was 20% as assessed using the Baker score (implant-based reconstructions) and 43% as assessed using the CTCAE. | Severe fibrosis is a frequent complication after breast reconstruction and PMRT. |
| Wong JS, et al18 | III | 62 patients | Immediate | Pedicled TRAM flap; latissimus dorsi flap; latissimus dorsi flap plus implant; implant alone | Of the patients followed ≥6 months after PMRT, none of the 38 nonimplant patients underwent major corrective surgery within 6 months, compared to 3 of the 13 (23%) implant patients (p = 0.01). | Patients who undergo immediate implant-based reconstruction followed by PMRT have a high rate of major corrective surgery. |
| Panettiere P, et al19 | II | 61 patients | Immediate | Implants | Improvement in LENT-SOMA scores after fat grafting; the scores after fat grafting were lower than those before fat grafting and lower than irradiated reconstruction that were not fat grafted. | Fat grafting improves outcomes of irradiated reconstructed breasts with implants. |
| Serra-Renom JM, et al20 | II | 65 patients | Delayed | 2-stage implant (TE/I) | Delayed 2-stage implant reconstruction after PMRT with fat grafting at time of expander placement and implant exchange was associated with no complications, good patient satisfaction, and no cases of capsular contracture (>than Baker classification1). | With delayed reconstruction after PMRT, fat grafting in addition to traditional tissue expander and implant breast reconstruction achieves better outcomes with creation of new subcutaneous tissue. |
PMRT: postmastectomy radiation therapy; TE: tissue expander; DIEP: deep inferior epigastric perforator; TRAM: transverse rectus abdominis myocutaneous; TFL: tensor fascilata, SIEA: superficial inferior epigastric artery; SGAP: superior gluteal artery perforator
INITIAL PLACEMENT OF A TISSUE EXPANDER AT MASTECTOMY FOR PATIENTS UNDERGOING BREAST RECONSTRUCTION WHO MAY OR WILL REQUIRE PMRT
A recent study by Kronowitz and colleagues3 detailed important technical and timing considerations in implementing delayed-immediate reconstruction, the 2-stage approach to breast reconstruction for patients who may require PMRT (patients with stage II and some with stage I breast cancer). Some of the important considerations included: 1) Preoperative consultation with a radiation oncologist before initiating delayed-immediate. 2) Inflate expander at mastectomy to scaffold breast skin envelope and minimize expansion. 3) Not to use full height expanders because they may interfere with radiation treatment of the clavicular nodal basins. 4) Review permanent pathology to determine need for PMRT prior to definitive breast reconstruction. 5) If expander is deflated for PMRT, only partially deflate, and reinflate within 2 weeks after PMRT. 6) In patients that receive PMRT, perform a skin-preserving delayed reconstruction using the preserved radiated breast skin, no longer than 3 months after the completion of PMRT (level II evidence).3
The most recent publication by Kronowitz and colleagues compared the outcomes in 47 patients with advanced breast cancer (stages IIB and III) who underwent a multidisciplinary protocol for planned skin-preserving delayed reconstruction and 47 disease-matched control patients who underwent standard delayed reconstruction after PMRT (no skin preservation or tissue expander).4 Although approximately one-third of the tissue expanders were lost in the protocol group, the protocol group had a lower rate of complications of definitive breast reconstruction than the standard delayed-reconstruction group (24 percent versus 38 percent). There was no difference in 3-year recurrence-free survival rates between the groups, which established the possibility of a new reconstructive paradigm enabling patients with advanced breast cancer to undergo skin-preserving breast reconstruction (level II evidence).
IMPACT OF PREVIOUS IRRADIATION ON OUTCOMES OF RECONSTRUCTION
Fosnot and colleagues5 sought to determine whether prereconstruction radiation therapy affects the rate of vascular complications in patients undergoing breast reconstruction with free flaps. In this retrospective study, 226 flaps that were placed into an irradiated chest were compared to 799 flaps that were transferred into a radiation-naive defect. Vascular complications overall were more prevalent in the irradiated group (17.3 percent versus 9.6 percent, p = 0.001), and regression modeling showed radiation therapy to be an independent risk factor.5 A subgroup analysis showed that a previously irradiated chest wall was associated with a significantly higher rate of intraoperative vascular complications (14.2 percent versus 7.6 percent, p = 0.003) but had no effect on delayed vascular complications (level III evidence).
Berry and colleagues6 performed a retrospective review of 1037 patients who underwent breast reconstruction to determine whether radiation therapy delivered before or after reconstruction increases the risk of major complications necessitating reoperation. Among patients who had reconstruction with autologous tissues, there was a lack of impact of preoperative irradiation on major complications. Multivariate analysis revealed no statistically significant difference in rates of major complications between the patients who received preoperative radiation therapy and those who did not (p = 0.84) (level III evidence).
Khansa and colleagues7 evaluated whether prior breast conservation therapy (lumpectomy and radiation therapy) led to higher rates of complications and dissatisfaction with subsequent mastectomy and breast reconstruction. They evaluated 532 patients, of whom 113 (137 reconstructions) had had prior breast conservation therapy and 419 (665 reconstructions) had not. Prior breast conservation therapy did not correlate with higher complication rates (p = 0.690) or lower satisfaction (p = 0.559) with aesthetic outcomes; however, it did correlate with an increased rate of mastectomy skin flap necrosis (12.4 percent versus 6.8 percent, p = 0.024) (level III evidence).
IMPACT OF RADIATION ON THE RECONSTRUCTED BREAST
In the review by Berry and colleagues mentioned in the preceding section, among patients who underwent reconstruction with autologous tissue, there was a lack of impact of postoperative irradiation on major complications. Multivariate analysis revealed no significant difference in rates of major complications between patients who received postoperative radiation therapy and those who did not (p = 0.61) (level III evidence).
Crisera and colleagues8 performed a retrospective study of 183 immediate free flap reconstructions in 170 patients with advanced breast cancer (≥stage IIB), of whom 103 underwent postoperative irradiation. Importantly, the overall cosmetic outcome in patients who underwent postoperative irradiation was comparable to that of those who did not. Administration of postoperative radiation therapy was not an independent predictor of fat necrosis within the autologous tissue flap (p = 0.42). Some degree of flap shrinkage was observed in 30 percent of patients treated postoperatively with radiation, but only 10 percent of patients treated with radiation experienced severe breast distortion and were subsequently advised to undergo placement of an additional flap or custom-made implant to correct a deformity (level IV evidence).
Albino and colleagues9 studied the impact of PMRT in 76 patients who underwent immediate autologous microsurgical breast reconstruction. Complications occurred in 53 patients (70 percent) 7.2 ± 6 months after irradiation. Thirty-six patients (47 percent) required reoperation because of postirradiation effects. Parenchymal complications (fat necrosis or parenchymal fibrosis) occurred in 19.7 percent of the patients, and skin complications (tissue envelope retraction or hypertrophic scarring) occurred in 30.3 percent; in 27.6 percent of the cases, either the surgeon or the patient expressed general dissatisfaction with the outcome of the reconstruction. Parenchymal complications were significantly associated with smoking, type II diabetes mellitus, and older patient age. Neoadjuvant chemotherapy significantly increased the risk of complications, particularly skin changes (level III evidence).
A study from the United Kingdom measured whether adjuvant radiation therapy following immediate deep inferior epigastric perforator (DIEP) free flap reconstruction affected flap volume.10 Sixty-eight patients underwent immediate DIEP flap breast reconstruction following mastectomy for breast cancer. Of the 68 patients in the study, 22 received postoperative radiation therapy (45 Gy in 20 fractions over 4 weeks), and 46 did not. Flap volumes were recorded intraoperatively and then reassessed at least 1 year after surgery. After a median follow-up of 5.5 years, there was no significant difference in volume change between patients who had and those who did not have postreconstruction radiation therapy (level III evidence).
Jhaveri and colleagues11 determined long-term complication rates and cosmetic results for patients undergoing PMRT after immediate reconstruction. These authors evaluated 92 patients who underwent modified radical mastectomy, immediate reconstruction, and PMRT. Sixty-nine patients underwent reconstruction with a tissue expander plus an implant, and 23 underwent reconstruction with autologous tissue. After a median follow-up of 38 months, the overall rate of severe complications (grade 3, surgical intervention or intravenous antibiotics required, or grade 4, removal or replacement of the reconstructed breast) was 25 percent. The overall rate of poor functional results (grade 2–4, functional score ≥2, impact on ability to perform activities of daily living) was 43.4 percent. When results were analyzed as a function of type of reconstruction, the rate of grade 3 or 4 complications was 33.3 percent for reconstruction with a tissue expander plus an implant versus 0 percent for reconstruction with autologous tissue (p = 0.001). The rate of grade 2–4 complications was 55 percent for reconstruction with a tissue expander plus an implant versus 8.7 percent for reconstruction with autologous tissue (p<0.001). Acceptable cosmesis was reported in 51 percent of patients in the implant group versus 82.6 percent in the autologous tissue group (p = 0.007). The authors concluded that in patients undergoing PMRT after immediate reconstruction, autologous tissue-based reconstruction is associated with fewer long-term complications and better cosmetic results than reconstruction with a tissue expander plus an implant (level II evidence).
An interesting study assessed fibrosis of the reconstructed breast after radiation therapy in 109 patients who underwent breast reconstruction followed by PMRT.12 Radiation therapy was applied with a median dose of 50.4 Gy, and 44 patients (40.4 percent) also received a boost treatment with a median dose of 10 Gy. Fibrosis was assessed in 20 autologous tissue-based reconstructions, 82 implant-based reconstructions, and 7 combined reconstructions using the Baker score for implant reconstruction and the Common Terminology Criteria for Adverse Events (CTCAE) for all patients. After a mean follow-up of 34 months, the 3-year incidence of ≥grade III fibrosis was 20 percent as assessed using the Baker score (implant-based reconstructions) and 43 percent as assessed using the CTCAE. The 3-year rate of surgical correction of the contralateral breast was 30 percent, and unplanned surgery on the reconstructed breast was performed in 39 patients (35.8 percent). Boost treatment and type of reconstruction (implant versus autologous) were not significantly associated with the incidence of fibrosis. The authors found severe fibrosis to be a frequent complication after PMRT and breast reconstruction (level IV evidence).
Wong and colleagues13 evaluated the incidence of major corrective surgery after immediate breast reconstruction and PMRT. The study group consisted of 62 patients who underwent modified radical mastectomy and immediate reconstruction followed by PMRT to the reconstructed breast. Reconstruction was performed with a pedicled transverse rectus abdominis myocutaneous flap in 42 patients, an LD flap in 5 patients, an LD flap plus an implant in 6 patients, and an implant alone in 9 patients. The median follow-up time was 13 months for nonimplant patients and 10 months for implant patients. The primary end point was the incidence of major corrective surgery. Ten patients (16 percent) underwent major corrective surgery between 1 and 28 months after irradiation; 4 of the 47 nonimplant patients (9 percent) underwent major corrective surgery, compared to 6 of the 15 implant patients (40 percent). Among patients followed for at least 6 months after PMRT, 0 of 38 nonimplant patients underwent major corrective surgery within 6 months, compared to 3 of the 13 implant patients (23 percent) (p = 0.01). For patients followed for at least 12 months after PMRT, the rates of major corrective surgery within 12 months were 4 percent (1 of 24) in the nonimplant group and 29 percent (2 of 7) in the implant group. The authors concluded that patients who undergo implant-based reconstruction followed by PMRT have a high rate of subsequent major corrective surgery. The difference in the rate of major corrective surgery between the implant and nonimplant groups was significant in early follow-up (level III evidence).
SHOULD RECONSTRUCTION BE PERFORMED BEFORE OR AFTER PMRT?
A meta-analysis was performed to determine the optimal sequencing of breast reconstruction in patients receiving PMRT.14 A total of 1105 patients were identified from 11 selected studies. In general, the study found that patients undergoing PMRT are 4.2 times as likely to suffer adverse events as patients not undergoing PMRT. When PMRT was delivered after immediate breast reconstruction, patients who had autologous tissue-based reconstruction had one-fifth the risk of adverse events of patients who had implant-based reconstruction. Delaying breast reconstruction until after PMRT had no significant effect on outcome (level III evidence).
OPTIMAL INTERVAL BETWEEN PMRT AND DELAYED BREAST RECONSTRUCTION
In the past, reconstruction was delayed for several years after PMRT because of concerns that the reconstructed breast would interfere with surveillance for recurrence in the higher-risk breast cancer patients who tend to receive PMRT. However, subsequent studies found that a reconstructed breast does not delay the detection of recurrence and that overall survival after a locoregional recurrence of breast cancer is not adversely impacted by the presence of a reconstructed breast. Recently, there has been a trend toward performing reconstruction sooner after PMRT to reduce the time patients must wait to have a reconstructed breast.
Baumann and colleagues15 evaluated the optimal interval between PMRT and delayed abdominal free flap breast reconstruction. Patients were classified as having undergone reconstruction less than 12 months after PMRT (group I) or 12 months or more after PMRT (group II). One hundred eighty-nine patients were identified, 82 (43.4 percent) in group I and 107 (56.6 percent) in group II. The total flap loss rate was 2.6 percent, and all flap losses occurred in group I (p = 0.014). The reoperation rate was higher in group I (14.6 percent versus 4.7 percent; p = 0.022) (level III evidence).
Momoh and colleagues16 retrospectively evaluated the outcomes in 100 patients who underwent delayed autologous tissue-based breast reconstruction after PMRT—17 who underwent reconstruction within 6 months after PMRT and 83 who underwent reconstruction more than 6 months after PMRT. No significant differences in complication rates were observed between the 2 groups. An alternate analysis examined 51 patients who underwent reconstruction within 12 months after PMRT and 49 patients who underwent reconstruction more than 12 months after PMRT; again, no significant differences in complication rates were observed. The authors concluded that as overall complication rates were similar in patients who had reconstruction early or late after PMRT, it may be reasonable to perform autologous breast reconstruction less than 1 year after PMRT instead of the currently accepted practice of many reconstructive surgeons, which is to wait at least 1 year after PMRT (level III evidence).
IMPACT OF AUTOLOGOUS FAT GRAFTING ON COSMETIC OUTCOMES OF IRRADIATED RECONSTRUCTED BREASTS
Losken and colleagues17 evaluated the use of autologous fat grafting after transverse rectus abdominis myocutaneous flap breast reconstruction to improve contour, improve shape, or increase volume. Patients with a history of radiation therapy had a significantly increased incidence of repeat injections (36 percent versus 18 percent, p = 0.002) (level IV evidence).
EVOLVING PATTERNS OF RADIATION DELIVERY
A study presented at this year’s American Society of Clinical Oncology meeting found that in patients with early-stage, node-positive breast cancer (T1 or T2 tumors with 1–3 involved axillary lymph nodes) who underwent breast conservation therapy with axillary lymph node dissection, the addition of irradiation of the internal mammary, supraclavicular, and apical axillary lymph nodes resulted in a significantly higher 5-year disease-free survival rate (89.7% versus 84.0%, HR, 0.68) (level I evidence).18 These findings will most likely be extrapolated to patients who undergo mastectomy and will most likely reinforce the increasing use of PMRT in patients with early-stage breast cancer. Routine delivery of PMRT to the regional nodal basins in patients with early-stage disease may make it more difficult to deliver radiation after immediate breast reconstruction, even with intensity-modulated radiation therapy (IMRT).
Some centers are attempting to improve outcomes of PMRT after reconstruction in patients with early-stage breast cancer by using hypofractionation.20 This strategy involves delivering a lower overall dose in fewer, larger fractions than standard regimens (41.6 Gy in 13 fractions of 3.2 Gy over 5 weeks or 39 Gy in 13 fractions of 3.0 Gy over 5 weeks versus the standard of 50 Gy in 25 fractions of 2.0 Gy over 5 weeks). This strategy has been shown to decrease the volume loss associated with standard dosages of PMRT after immediate autologous breast reconstruction (level I evidence).19
Another alternative approach to breast reconstruction that has been suggested for patients who will require PMRT is to deliver radiation before mastectomy and immediate reconstruction in all patients (level I evidence).20 Although this concept is appealing, a premastectomy sentinel lymph node biopsy would be required in patients with early-stage breast cancer to assess the need for PMRT. In addition, it is well known that premastectomy irradiation is associated with higher rates of mastectomy skin flap necrosis.
SUMMARY AND CLINICAL IMPACT OF THE EVIDENCE
In patients with advanced stages of cancer, immediate breast reconstruction, either with a tissue expander or a flap has not been shown to adversely affect recurrence free survival.4,8 In conjunction with the breast cancer team, reconstructive surgeons can now consider in select patients preserving the breast skin and perform immediate breast reconstruction in patients with advanced stages of breast cancer. This opportunity creates a new reconstructive perspective and allows these patients to now awake from mastectomy with a breast and receive the same aesthetic and psychological benefits as patients with early-stages of breast cancer.
This review revealed contrasting outcomes in regards to whether prior PMRT increases the complication rates of delayed microvascular breast reconstruction. One study found that prior PMRT increases the rate of intraoperative vascular complications,5 while another study found no adverse impact.6 Different outcomes were also found as to the best timing to perform delayed autologous tissue-based reconstruction after PMRT. A study by Momoh and colleagues16 found similar complication rates in patients who had early delayed reconstruction after PMRT (less than 12 months) and those patients who had late delayed reconstruction after PMRT (longer than 12 months). However, another study15 found higher total rates of flap loss and an increased need for reoperation when delayed microvascular breast reconstruction was performed within 12 months of PMRT.
Although some surgeons support waiting 1 year or longer after PMRT to perform breast reconstruction, there is a trend toward successful outcomes of breast reconstruction performed soon after PMRT, in some cases within 6 months after PMRT. This trend toward earlier reconstruction after PMRT along with the increasing use of skin-preserving mastectomy in patients with advanced breast cancer means that patients with advanced disease may no longer have to endure a long wait between PMRT and reconstruction and may expect improved aesthetic outcomes of delayed reconstruction.
Many surgeons are performing immediate autologous tissue-based reconstruction before PMRT with reasonable rates of complications and good cosmetic outcomes.6,8,10 However, another recent study9 continued to show the high complication rates and extensive need for major revision surgery or an additional flap that were seen in the classic studies on this subject.20–22 The decision as to whether to perform immediate autologous tissue-based reconstruction before PMRT or wait until after PMRT should be made in concert with a radiation oncologist. In an effort to decrease tissue injury to the reconstructed breast, creative strategies, like radiation hypofractionation are being implemented to alter the dosing and timing of radiation delivery in breast cancer patients.19
Uncertainty about the need for PMRT in many patients with early-stages of breast cancer who now present for immediate breast reconstruction has also led some reconstructive surgeons to opt for an intermediate approach: a tissue expander is placed at mastectomy as an initial step in breast reconstruction. This preserves breast skin that can then be used for reconstruction after mastectomy if PMRT is not required or for delayed reconstruction after PMRT if PMRT is required.3,4
Although at MD Anderson, we continue to partially deflate patients’ tissue expanders during PMRT in order to treat the internal mammary lymph node basins, the need to treat the internal mammary nodes in all patients remains controversial. Many centers do not treat these nodes and therefore do not deflate patients’ tissue expanders during PMRT. However, if the recently presented findings of the MA-20 trial18 get translated into clinical practice and all patients receive PMRT to the internal mammary nodes, immediate autologous tissue-based reconstruction may make it more difficult for those centers that currently do not deflate patients’ tissue expanders to adequately deliver PMRT.
Acknowledgments
MD Anderson is supported in part by the National Institutes of Health through MD Anderson’s Cancer Center Support Grant, CA016672.
Footnotes
Disclosure
The author serves on a Scientific Advisory Committee for Allergan Medical, Irving, CA.
REFERENCES
- 1.Shirvani SM, Pan IW, Buchholz TA, et al. Impact of evidence-based clinical guidelines on the adoption of postmastectomy radiation in older women. Cancer. 2011 Jun 27; doi: 10.1002/cncr.26081. [DOI] [PubMed] [Google Scholar]
- 2.Kronowitz SJ, Hunt KK, Kuerer HM, et al. Delayed-immediate breast reconstruction. Plast Reconstr Surg. 2004 May;113(6):1617–1628. doi: 10.1097/01.prs.0000117192.54945.88. (need to change citation. [DOI] [PubMed] [Google Scholar]
- 3.Kronowitz SJ. Delayed-immediate breast reconstruction: technical and timing considerations. Plast Reconstr Surg. 2010 Feb;125(2):463–474. doi: 10.1097/PRS.0b013e3181c82d58. [DOI] [PubMed] [Google Scholar]
- 4.Kronowitz SJ, Lam C, Terefe W, Hunt KK, et al. A multidisciplinary protocol for planned skin-preserving delayed breast reconstruction for patients with locally advanced breast cancer requiring postmastectomy radiation therapy: 3-year follow-up. Plast Reconstr Surg. 2011 Jun;127(6):2154–2166. doi: 10.1097/PRS.0b013e3182131b8e. [DOI] [PubMed] [Google Scholar]
- 5.Fosnot J, Fischer JP, Smartt JM, Jr, et al. Does previous chest wall irradiation increase vascular complications in free autologous breast reconstruction? Plast Reconstr Surg. 2011 Feb;127(2):496–504. doi: 10.1097/PRS.0b013e3181fed560. [DOI] [PubMed] [Google Scholar]
- 6.Berry T, Brooks S, Sydow N, et al. Complication rates of radiation on tissue expander and autologous tissue breast reconstruction. Ann Surg Oncol. 2010 Oct;17(Suppl 3):202–210. doi: 10.1245/s10434-010-1261-3. Epub 2010 Sep 19. [DOI] [PubMed] [Google Scholar]
- 7.Khansa I, Colakoglu S, Curtis MS, et al. Postmastectomy breast reconstruction after previous lumpectomy and radiation therapy: analysis of complications and satisfaction. Ann Plast Surg. 2011 May;66(5):444–451. doi: 10.1097/SAP.0b013e3182166b81. [DOI] [PubMed] [Google Scholar]
- 8.Crisera CA, Chang EI, Da Lio AL, et al. Immediate free flap reconstruction for advanced-stage breast cancer: is it safe? Plast Reconstr Surg. 2011 Jul;128(1):32–41. doi: 10.1097/PRS.0b013e3182174119. [DOI] [PubMed] [Google Scholar]
- 9.Albino FP, Koltz PF, Ling MN, Langstein HN. Irradiated autologous breast reconstructions: effects of patient factors and treatment variables. Plast Reconstr Surg. 2010 Jul;126(1):12–16. doi: 10.1097/PRS.0b013e3181da878f. [DOI] [PubMed] [Google Scholar]
- 10.Chatterjee JS, Lee A, Anderson W, Baker L, et al. Effect of postoperative radiotherapy on autologous deep inferior epigastric perforator flap volume after immediate breast reconstruction. Br J Surg. 2009 Oct;96(10):1135–1140. doi: 10.1002/bjs.6693. [DOI] [PubMed] [Google Scholar]
- 11.Jhaveri JD, Rush SC, Kostroff K, Derisi D, Farber LA, Maurer VE, Bosworth JL. Clinical outcomes of postmastectomy radiation therapy after immediate breast reconstruction. Int J Radiat Oncol Biol Phys. 2008 Nov 1;72(3):859–865. doi: 10.1016/j.ijrobp.2008.01.055. [DOI] [PubMed] [Google Scholar]
- 12.Classen J, Nitzsche S, Wallwiener D, et al. Fibrotic changes after postmastectomy radiotherapy and reconstructive surgery in breast cancer. A retrospective analysis in 109 patients. Strahlenther Onkol. 2010 Nov;186(11):630–636. doi: 10.1007/s00066-010-2158-6. [DOI] [PubMed] [Google Scholar]
- 13.Wong JS, Ho AY, Kaelin CM, Bishop KL, et al. Incidence of major corrective surgery after post-mastectomy breast reconstruction and radiation therapy. Breast J. 2008 Jan-Feb;14(1):49–54. doi: 10.1111/j.1524-4741.2007.00522.x. [DOI] [PubMed] [Google Scholar]
- 14.Barry M, Kell MR. Radiotherapy and breast reconstruction: a meta-analysis. Breast Cancer Res Treat. 2011 May;127(1):15–22. doi: 10.1007/s10549-011-1401-x. [DOI] [PubMed] [Google Scholar]
- 15.Baumann DP, Crosby MA, Selber JC, et al. Optimal timing of delayed free lower abdominal flap breast reconstruction after postmastectomy radiation therapy. Plast Reconstr Surg. 2011 Mar;127(3):1100–1106. doi: 10.1097/PRS.0b013e3182043652. [DOI] [PubMed] [Google Scholar]
- 16.Momoh AO, Colakoglu S, de Blacam C, et al. Delayed Autologous Breast Reconstruction After Postmastectomy Radiation Therapy: Is There an Optimal Time? Ann Plast Surg. 2011 May 27; doi: 10.1097/SAP.0b013e31821ee4b6. [DOI] [PubMed] [Google Scholar]
- 17.Losken A, Pinell XA, Sikoro K, et al. Autologous fat grafting in secondary breast reconstruction. Ann Plast Surg. 2011 May;66(5):518–522. doi: 10.1097/SAP.0b013e3181fe9334. [DOI] [PubMed] [Google Scholar]
- 18.Whelan TJ, Olivotto I, Ackerman I, et al. Abstract: NCIC-CTG MA.20: An intergroup trial of regional nodal irradiation in early breast cancer. American Society of Clinical Oncology 2011 Annual Meeting; 6/2011; Chicago, IL. [Google Scholar]
- 19.START Trialists' Group. Bentzen SM, Agrawal RK, Aird EG, Barrett JM, Barrett-Lee PJ, Bliss JM, Brown J, Dewar JA, Dobbs HJ, Haviland JS, Hoskin PJ, Hopwood P, Lawton PA, Magee BJ, Mills J, Morgan DA, Owen JR, Simmons S, Sumo G, Sydenham MA, Venables K, Yarnold JR. The UK Standardisation of Breast Radiotherapy (START) Trial A of radiotherapy hypofractionation for treatment of early breast cancer: a randomised trial. Lancet Oncol. 2008 Apr;9(4):331–341. doi: 10.1016/S1470-2045(08)70077-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Giacalone PL, Rathat G, Daures JP, et al. New concept for immediate breast reconstruction for invasive cancers: feasibility, oncological safety and esthetic outcome of post-neoadjuvant therapy immediate breast reconstruction versus delayed breast reconstruction: a prospective pilot study. Breast Cancer Res Treat. 2010 Jul;122(2):439–451. doi: 10.1007/s10549-010-0951-7. Epub 2010 May 26. [DOI] [PubMed] [Google Scholar]
- 21.Williams JK, Carlson GW, Bostwick J, 3rd, Bried JT, Mackay G. The effects of radiation treatment after TRAM flap breast reconstruction. Plast Reconstr Surg. 1997 Oct;100(5):1153–1160. doi: 10.1097/00006534-199710000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Tran NV, Chang DW, Gupta A, Kroll SS, Robb GL. Comparison of immediate and delayed free TRAM flap breast reconstruction in patients receiving postmastectomy radiation therapy. Plast Reconstr Surg. 2001 Jul;108(1):78–82. doi: 10.1097/00006534-200107000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Rogers NE, Allen RJ. Radiation effects on breast reconstruction with the deep inferior epigastric perforator flap. Plast Reconstr Surg. 2002 May;109(6):1919–1924. doi: 10.1097/00006534-200205000-00022. discussion 1925-6. [DOI] [PubMed] [Google Scholar]