Abstract
Background:
The fourth survey of the surveillance system named “childhood and adolescence surveillance and prevention of adult non-communicable disease” (CASPIAN-IV study), was conducted among a national representative sample of Iranian students. This paper describes the methods and early findings of this survey.
Methods:
This nationwide school-based study was conducted in 2011-2012 in 30 provinces of Iran among 13,486 students, 6-18 years (6640 girls, 75.6% from urban areas) and one of their parents.
Results:
Mean age of students was 12.5 years. Based on the World Health Organization growth curves, 12.2% were underweight, 9.7% overweight and 11.9% were obese. Abdominal obesity was observed in 19.1% of students. The dominant type of cooking oil in urban families was liquid oil and hydrogenated fat (39% and 32%), most rural families used hydrogenated fat (53%), respectively. A total of 18% of students had at least 30 min of daily physical activity; 41% of students used computer in weekdays and 44% used it in weekends. Almost 34.5% of students reported to have at least one cigarette smoker and 21.5% reported to have a waterpipe smoker in their relatives. Moreover, 20.3% of students reported that they had suffered an injury needing the help of school health providers during the year prior to the study.
Conclusions:
Current evidence on the health risky behaviors among Iranian children and adolescents confirms the importance of conducting comprehensive surveillance surveys to identify health risk behaviors. Data of this survey and the trend of variables provide necessary information for health policy makers to implement action-oriented interventions.
Keywords: Chronic diseases, prevention, risk behaviors, risk factors, school health, surveillance
INTRODUCTION
The majority of behavioral risk factors of non-communicable chronic diseases (NCDs) originate in childhood and adolescence.[1,2,3,4,5] Sedentary life-style has been linked to an undesirable cardiovascular disease risk profile including obesity,[6] insulin resistance,[7] and high blood pressure.[8] On the other hand, tobacco use at a young age has been associated with emotional and psychological problems, risky behaviors such as violence and sexual activity and an increased risk of cancers later in life.[9,10] In addition, childhood obesity has been linked to increased risk of dyslipidemia, hyperinsulinemia, hypertension and a number of psychosocial problems.[11,12]
The global school-based health survey (GSHS) in students has been developed by World Health Organization (WHO) and Centers for Disease Control and Prevention in cooperation with United Nations’ UNICEF, UNESCO, UNAIDS. The GSHS was designed to help countries measure and assess the behavioral risk factors and protective factors among children and adolescents aged 13-17 years.[13] This surveillance system is entitled “childhood and adolescence surveillance and prevention of adult non-communicable disease” (CASPIAN) study. It is a national school-based surveillance of the risk behaviors and risk factors of chronic diseases using GSHS among children and adolescents in Iran. So far, four surveys of CASPIAN studies have been conducted, beginning from 2003 to 2004. The surveys are repeated every 2 years, with blood sampling for biochemical measurements every 4 years.[14,15,16]
This paper presents the methodological aspects and early findings of the 4th survey of CASPIAN study.
METHODS
The CASPIAN-IV study was performed in 2011-2012 in urban and rural areas of the central counties of 31 provinces in Iran. Data was checked at the district level by academic supervisors (expert of school health) and controlled by national supervisors and operators.
Study population and sampling framework
The study population consisted of students from elementary, intermediate and high schools of urban and rural areas. They were selected by multistage, cluster sampling method from 31 provinces of the country (48 clusters of 10 students in each province). Stratification was performed in each province according to the residence area (urban/rural) and school grade (elementary/intermediate/high school). The sampling was proportional to size with equal sex ratio; i.e., equal number of boys and girls were selected from each province and the ratios in urban and rural areas were proportionate to the population of urban and rural students. In this way, the number of samples in rural/urban areas and in each school grade was divided proportionally to the population of students in each grade.
Cluster sampling with equal clusters was used in each province to reach the necessary sample size. Clusters were determined at the level of schools, including 10 sample units (students and their parents) in each cluster.
The sample size was determined according to the cluster sampling method and to achieve a good estimate of the main risk factors of interest such as dietary behaviors, overweight and obesity and physical inactivity. The maximum sample size that could give a good estimate of all risk factors of interest was selected. Thus, the sample size was calculated as 480 subjects in each province. A total of 48 clusters of 10 subjects in each of the provinces and a total of 14,880 students and an equal number of their parents were selected from 31 provinces.
Procedure and measurements
Questionnaires
Two sets of questionnaires were completed for students and their parents. The questionnaires were obtained from GSHS and translated to Persian. The validity and reliability of questionnaires has been assessed previously.[17] The face validity was approved by the expert panel and in the phase of content validity assessment, questions got a score of more than 0.75 which affirm the content validity. Cronbach's alpha coefficient of the whole questionnaires was 0.97 and the Pearson correlation coefficient of the test-retest phase was 0.94, which confirmed the reliability of questionnaires.
The student questionnaire included questions about the relationship with peers, body image, and psychosocial environment of school, dietary habits, life-style habits, physical activity pattern, unintentional injuries, violence behavior, active and passive smoking, as well as psychosocial relations with family. Trained personnel completed the questionnaires in a calm atmosphere inside the schools; the whole process was supervised and controlled by a team of health care professionals.
Concerns such as family composition, socio-demographic factors and genetic determinants (family history of hypertension, diabetes, obesity, sever osteoporosis, cancer), past history of student (birth weight, breastfeeding, type of complementary food), family dietary habits and unintentional injuries to the student were included in the parent's questionnaire. These questionnaires were also completed by trained interviewers and at least one of the parents was required to be present for answering the questions.
Physical measurements
All measurements were conducted under standard protocols and by using calibrated instruments. The project team measured height, weight, waist, hip and wrist circumferences. Weight was measured to the nearest 0.1 kg on a scale placed on a flat ground and subjects wearing light clothing and standing motionless and height were measured without shoes to the nearest 0.1 cm.[18] Waist circumference was measured using a non-elastic tape at a point midway between the lower border of the rib cage and the iliac crest at the end of normal expiration to the nearest 0.1 cm. Hip circumference was measured at the widest part of the hip at the level of the greater trochanter to the nearest 0.1 cm.[19] Body mass index (BMI) was calculated by dividing weight (kg) to height squared (m2). We used the WHO growth charts to categorize BMI.[20] Abdominal obesity was defined as waist-to-height ratio of more than 0.5.[21]
Wrist circumference was measured to the nearest 0.1 cm on the dominant arm using a tape meter. Subjects were asked to hold their arm on a flat surface as a table. The superior border of the tape measure was placed just distal to the prominences of radial and ulnar bones. The wrist circumference was measured without the tape was too tight or too loose and with lying flat on the skin. Wrist circumference was measured before measuring blood pressure.
Blood pressure was measured in the sitting position on the right arm using a mercury sphygmomanometer with an appropriate cuff size. It was measured 2 times at 5-min intervals and the average was registered.[22]
Ethical concerns
Study protocols were reviewed and approved by ethical committees and other relevant national regulatory organizations. After complete explanation of the study objectives and protocols, written informed consent and verbal consent was obtained from the parents and students, respectively.
Statistical analysis
Mean of continuous variables was reported with 95% of the confidence interval (CI), categorical variables are expressed as a percentage. Comparison of mean of continuous variables across genders was investigated by Student t-test. Chi-square test was used to analyze categorical data. Statistical measures were estimated using survey data analysis methods in th StataCorp. 2011. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP. package. P < 0.05 was considered as statistically significant.
RESULTS
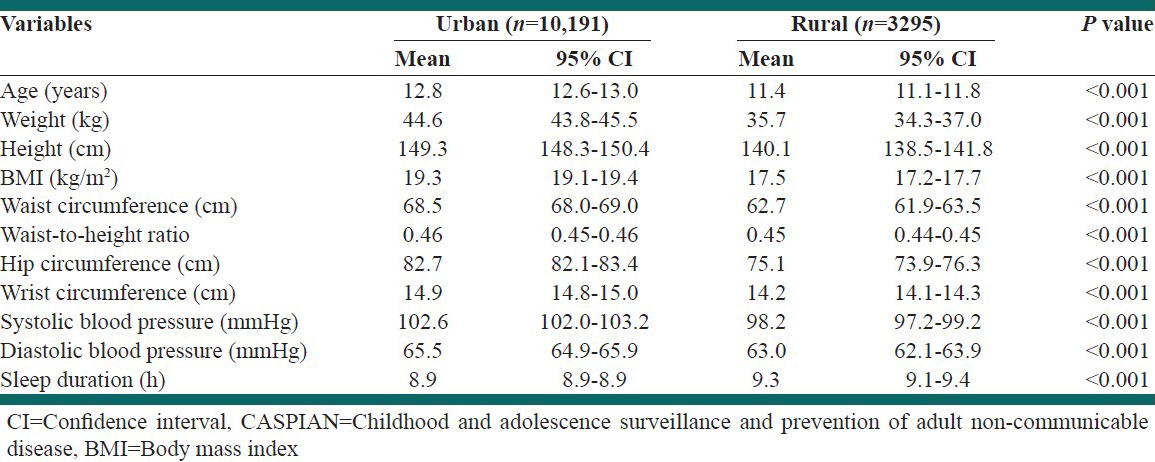
The population of this survey consisted of 13,486 children and adolescents out of 14,880 invited subjects (participation rate of 90.6%) and one of their parents. The whole data of one of the provinces was not available; therefore analysis was performed on data of 30 provinces. The students were 6640 girls and 6846 boys with a mean age of 12.5 years (12.3-12.6, 95% CI). A total of 75.6% of students were from urban and nearly 24.4% were from rural areas. Tables 1 and 2 present the characteristics of students by sex and living area, respectively.
Table 1.
Characteristics of participants according to gender: The CASPIAN-IV study
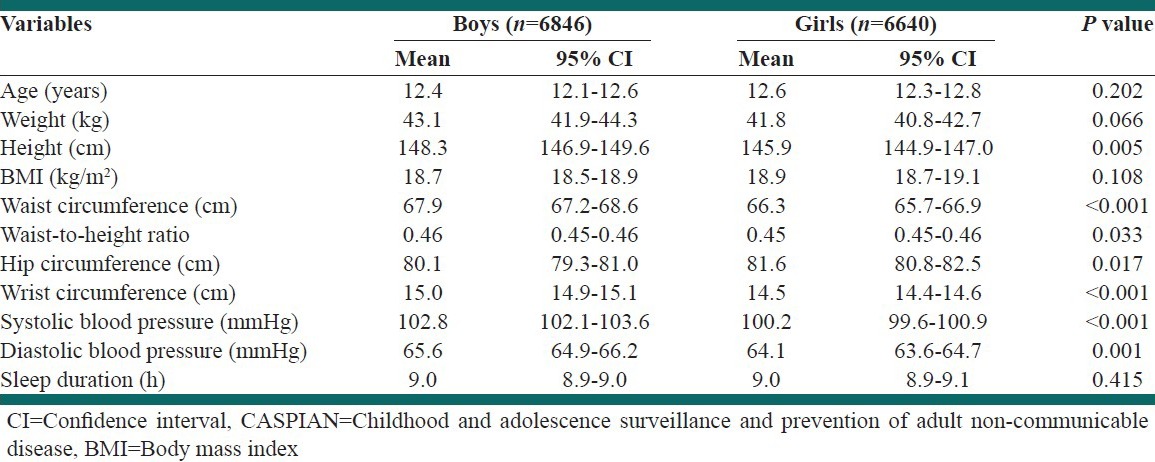
Table 2.
Characteristics of participants according to living area: The CASPIAN-IV study
Overall, 12.2% (11.3% of girls and 13.0% of boys) were underweight, 9.7% (10.1% of girls and 9.3% of boys) were overweight and 11.9% (10.1% of girls and 13.6% of boys) were obese. Abdominal obesity was documented in 19.1% of students (17.8% of girls and 20.4% of boys; 21.2% in urban and 12.8% in rural residents).
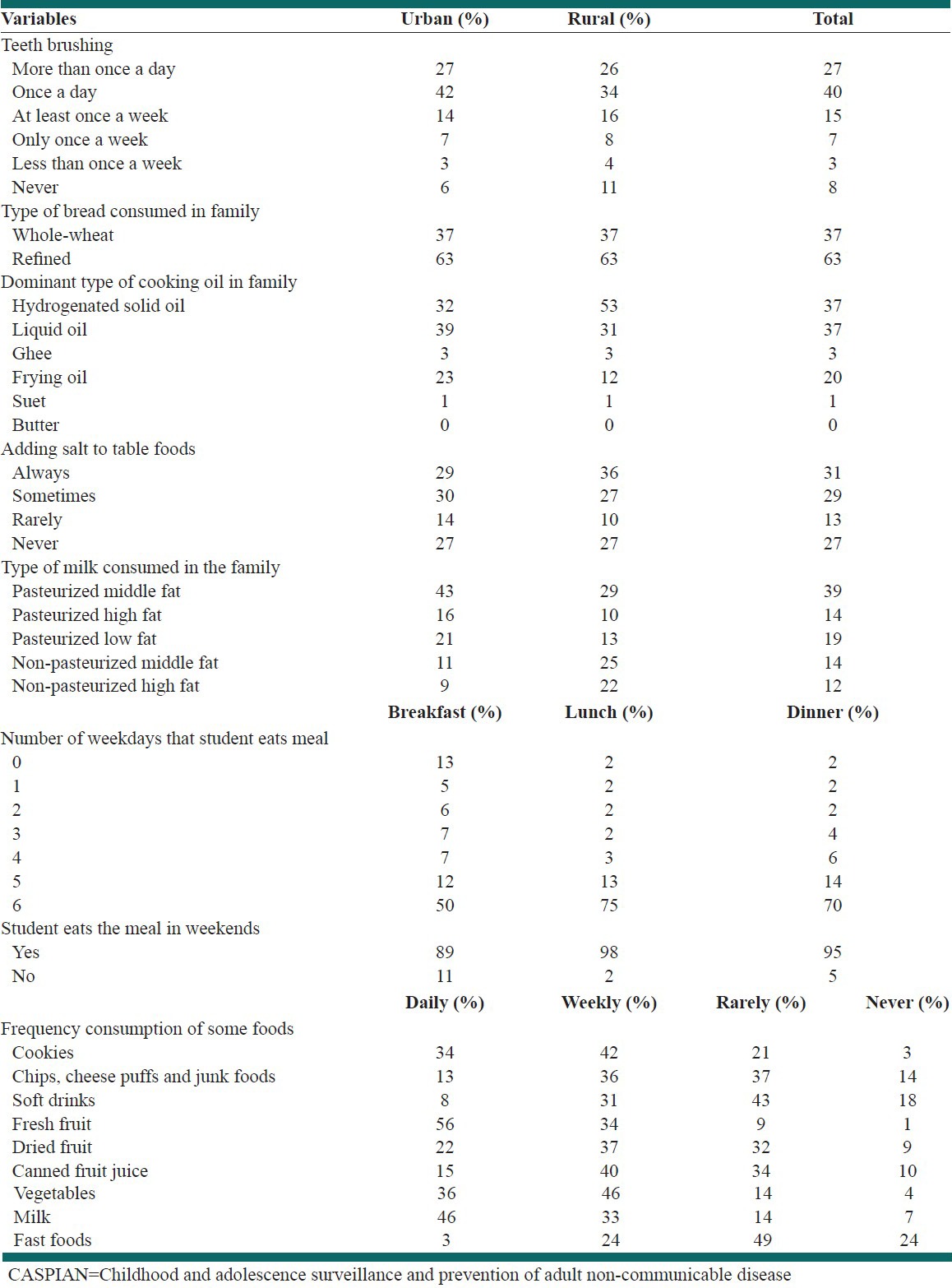
Table 3 presents some health and dietary behaviors of students or their families. According to reports by students, 42% of urban participants and 34% of rural participants brush their teeth once a day, 34% of girls and 20% of boys reported to brush their teeth more than once a day. Overall, 37% of families in both urban and rural areas consumed whole-wheat breads. Most of the rural families used hydrogenated solid fat (53%) and the most prevalent types of cooking oil in urban families were liquid oil and hydrogenated solid fat (39% and 32%, respectively). More rural students reported to always add salt to table food than urban participants (36% vs. 29%, respectively, P < 0.05). A total of 13% of students skipped breakfast during weekdays. Overall, 36% of students ate junk foods every week, 31% consumed soft drinks every week and 24% ate fast foods every week. More urban students reported to use fresh fruit daily than rural students (59% vs. 45%, respectively, P < 0.05).
Table 3.
Some health and dietary behaviors in Iranian children and adolescents: The CASPIAN-IV study
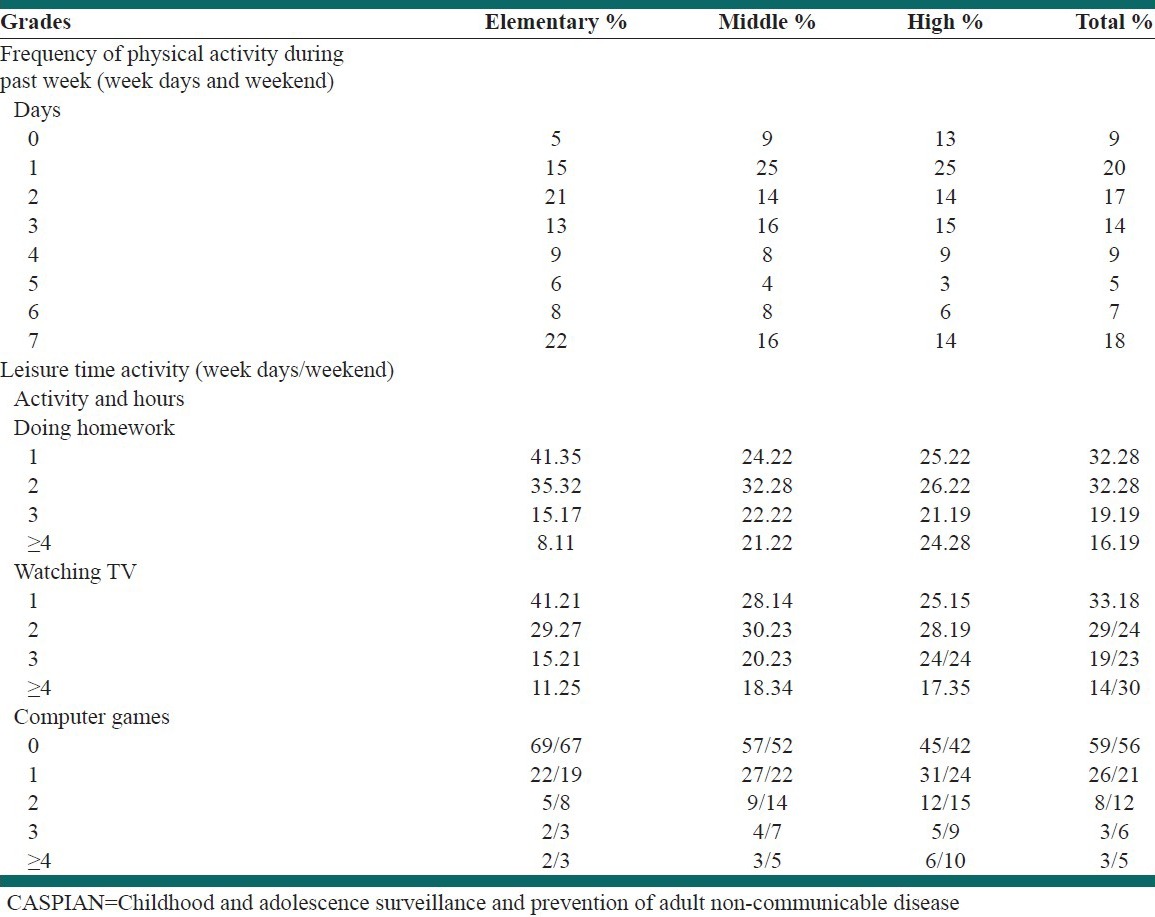
According to reports by students, 18% had at least 30-min a day leisure-time physical activity all days during the week prior to the study; however, 9% reported not to have any leisure time physical activity. Regular physical activity was reported as 24% among boys and 13% among girls. Of students participated, 41% used computer in weekdays and 44% in weekends; these frequencies were higher in urban areas and among boys [Table 4].
Table 4.
Physical activity and leisure time activity in Iranian children and adolescents: The CASPIAN-IV study
Regarding passive smoking, 34.5% of students reported to have at least one cigarette smoker and 21.5% reported to have waterpipe smoker in their relatives, totally 43.9% of students were passive smoker. Overall, 5.9% of students (7.5% in boys and 4.2% in girls) were ever smoker; this prevalence was higher in adolescents than in younger age group. The mean age of the first attempt to smoke was 11.9 years.
A total of 27.4% and 17.5% of students asserted that in the 3 months before the study they bullied others or experienced getting bullied which was significantly more frequent among boys than girls.
Regarding injuries, 20.3% of students (19.4% elementary, 23.1% middle, 18.9% in high school; 25.7% in boys and 14.6% in girls) reported that in the 12 months prior to the study, they had suffered an injury needing the help of school health providers. The prevalence of these injuries was not statistically different according to living area (20.1% in urban and 20.7% in rural areas). In most of the cases, the injury occurred in home (39.9%) when they were playing and/or exercising. We also asked parents about some factors of early life of their children. Most students had a history of using breast milk and homemade complementary foods. The average duration of breastfeeding of students during the two 1st years of life was 15.39 months.
DISCUSSION
In the fourth phase of CASPIAN survey, different aspects of the general health status were assessed among a large number of Iranian children and adolescents. According to our findings, there is a need for reinforcement of the current health regulations and for setting practical policies, education and intervention strategies for both health promotion and primordial/primary prevention of chronic diseases.
In the current survey, both features of weight disorders, namely overweight and underweight were documented in the study participants and this confirms the nutrition and epidemiologic transition in Iran.[23,24] Compared with the CASPIAN-III study,[25] the increment in the prevalence of abdominal obesity was observed in the current survey (16.3% vs. 19%). The frequency of underweight had decreased from 13.9% in the CASPIAN-III study to 12% and it may be a confirmatory evidence for improvement in health care system. The aforementioned changes are consistent with the results reported from other studies conducted in the population of most developing countries in the East-Mediterranean region, which are experiencing double burden of nutritional disorders due to the rapid socio-economic alterations.[26,27,28]
Shifting away from healthy eating habits to fast foods, high-calorie low-nutrient diets combined with sedentary activities made children and adolescents more prone for development of overweight and its associated comorbidities as type two diabetes, cardiovascular and fatty liver diseases.[29,30,31,32]
Assessment of physical activity showed that most of the students were physically active for only 1 day/week; this finding is in line with the previous surveys of the CASPIAN study. Overall, the frequency and intensity of leisure time physical activity is low in Iranian children and adolescents. The exception was for elementary school students and rural districts devoting all weekdays for exercise. Having more free time, less homework and type of activities of elementary students, reinforcement of the ministerial regulations for physical activity in elementary schools, as well as more active life-styles in rural areas may explain such differences. The screen time was approximately two-fold higher than the recommended time.
Feeding pattern in the 1st year of life was breast milk, which can be a protective factor against many risk factors of chronic diseases, as obesity and hypertension. However, conflicting results exist and longitudinal studies are necessary to document such long-term effects.[33,34]
Regarding dietary habits; refined grains (63%) and liquid oil (39%) were mostly consumed among Iranian families. However, more than half of rural inhabitants (57%) reported consumption of solid hydrogenated fats. Added salt after the food preparation was mentioned by most of the students, except for elementary children. Type of dairy consumed was pasteurized-regular fat, eaten daily except for high-school students (weekly). Although the consumption frequency of unhealthy foods such as processed foods and low-nutrient snacks was low, parents declared that they made no significant changes in the child's diet in the year prior to the study.
Given the high prevalence of overweight and metabolic disorders in the country, it seems necessary to make practical policies to modify children's diet. As an example, dairy products, containing high amounts of calcium, with preventive effects against osteoporosis, overweight and insulin resistance, were not consumed daily among high-school students.[35,36]
Self-reported smoking was not prevalent among Iranian students compared to their peers in other countries,[37,38] however the first attempt to smoke was around 11 years, which was about 2 years earlier than the first CASPIAN study in 2003-2004.[39] This emphasizes on the importance of education and preventive approaches among families.
Assessment of the students’ health status showed that most of the participants were in suitable health condition, rarely felt sadness, dizziness and so on. Violence, bullying and other aggressive behaviors, were not frequent, similar to reports from other countries.[40,41]
Study limitations and strengths
The main limitation of this study was its cross-sectional design by which causality cannot be determined. Despite this limitation, the major strengths of this survey are the large sample size and the nationwide design of the study, which ensures the representativeness of the findings and providing the possibility of making comparisons with previous phases of the CASPIAN study. Besides, data of wrist circumference was collected for the 1st time during all CASPIANs; a measure which has been recently proposed as an important predictor of diabetes and pre-diabetes in adults and correlates with cardio metabolic risk factors. Finally, a high quality control of data collection was the other strength of this study.
CONCLUSIONS
The findings of this survey and the changes of variables studied in this surveillance system provide useful information for health policy makers and stakeholders to implement action-oriented interventions. The priorities of the health system for health promotion of children and adolescents are assumed to be development of effective intersectoral intervention programs promoting physical activity, healthy eating and improved life-style behaviors involving cooperative and immediate efforts of individuals, families, schools, community and government for primordial and primary prevention of NCDs.
ACKNOWLEDGMENTS
We forward our sincere thanks to the large team working in 45 universities of the provinces, in which the study was conducted. We would like to thank all organizations contributed to this survey, students and their parents who participated in this study.
Footnotes
Source of Support: This study was conducted in collaboration of the Ministry of Education and Training, Child Growth and Development Research Center, Isfahan University of Medical Sciences, Endocrinology and Metabolism Research Institute, and Chronic Diseases Research Center, Tehran University of Medical Sciences
Conflict of Interest: None declared
REFERENCES
- 1.Milton B, Woods SE, Dugdill L, Porcellato L, Springett RJ. Starting young? Children's experiences of trying smoking during pre-adolescence. Health Educ Res. 2008;23:298–309. doi: 10.1093/her/cym027. [DOI] [PubMed] [Google Scholar]
- 2.Dube SR, Miller JW, Brown DW, Giles WH, Felitti VJ, Dong M, et al. Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. J Adolesc Health. 2006;38:444.e1–10. doi: 10.1016/j.jadohealth.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 3.Basterfield L, Adamson AJ, Frary JK, Parkinson KN, Pearce MS, Reilly JJ, et al. Longitudinal study of physical activity and sedentary behavior in children. Pediatrics. 2011;127:e24–30. doi: 10.1542/peds.2010-1935. [DOI] [PubMed] [Google Scholar]
- 4.Sisson SB, Church TS, Martin CK, Tudor-Locke C, Smith SR, Bouchard C, et al. Profiles of sedentary behavior in children and adolescents: The US National Health and Nutrition Examination Survey, 2001-2006. Int J Pediatr Obes. 2009;4:353–9. doi: 10.3109/17477160902934777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Herman KM, Craig CL, Gauvin L, Katzmarzyk PT. Tracking of obesity and physical activity from childhood to adulthood: The Physical Activity Longitudinal Study. Int J Pediatr Obes. 2009;4:281–8. doi: 10.3109/17477160802596171. [DOI] [PubMed] [Google Scholar]
- 6.Tremblay MS, Willms JD. Is the Canadian childhood obesity epidemic related to physical inactivity? Int J Obes Relat Metab Disord. 2003;27:1100–5. doi: 10.1038/sj.ijo.0802376. [DOI] [PubMed] [Google Scholar]
- 7.Kasa-Vubu JZ, Lee CC, Rosenthal A, Singer K, Halter JB. Cardiovascular fitness and exercise as determinants of insulin resistance in postpubertal adolescent females. J Clin Endocrinol Metab. 2005;90:849–54. doi: 10.1210/jc.2004-0455. [DOI] [PubMed] [Google Scholar]
- 8.Leary SD, Ness AR, Smith GD, Mattocks C, Deere K, Blair SN, et al. Physical activity and blood pressure in childhood: Findings from a population-based study. Hypertension. 2008;51:92–8. doi: 10.1161/HYPERTENSIONAHA.107.099051. [DOI] [PubMed] [Google Scholar]
- 9.Mathers M, Toumbourou JW, Catalano RF, Williams J, Patton GC. Consequences of youth tobacco use: A review of prospective behavioural studies. Addiction. 2006;101:948–58. doi: 10.1111/j.1360-0443.2006.01438.x. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization: Health effects of smoking among young people. [Last accessed on 2013 Jul 12]. Available from: http://www.who.int/tobacco/research/youth/health_effects/en .
- 11.Reilly JJ, Methven E, McDowell ZC, Hacking B, Alexander D, Stewart L, et al. Health consequences of obesity. Arch Dis Child. 2003;88:748–52. doi: 10.1136/adc.88.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ho TF. Cardiovascular risks associated with obesity in children and adolescents. Ann Acad Med Singapore. 2009;38:48–9. [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention (CDC); 2009. [Last accessed on 2013 Aug 21]. Global School-based Student Health Survey. Available from: http://www.cdc.gov/GSHS . [Google Scholar]
- 14.Kelishadi R, Ardalan G, Gheiratmand R, Gouya MM, Razaghi EM, Delavari A, et al. CASPIAN Study Group. Association of physical activity and dietary behaviours in relation to the body mass index in a national sample of Iranian children and adolescents: CASPIAN Study. Bull World Health Organ. 2007;85(1):19–26. doi: 10.2471/BLT.06.030783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kelishadi R, Ardalan G, Adeli K, Motaghian M, Majdzadeh R, Mahmood-Arabi MS, et al. CASPIAN Study Group. Factor analysis of cardiovascular risk clustering in pediatric metabolic syndrome: CASPIAN study. Ann Nutr Metab. 2007;51:208–15. doi: 10.1159/000104139. [DOI] [PubMed] [Google Scholar]
- 16.Kelishadi R, Heshmat R, Motlagh ME, Majdzadeh R, Keramatian K, Qorbani M, et al. Methodology and Early Findings of the Third Survey of CASPIAN Study: A National School-based Surveillance of Students’ High Risk Behaviors. Int J Prev Med. 2012;3:394–401. [PMC free article] [PubMed] [Google Scholar]
- 17.Kelishadi R, Majdzadeh R, Motlagh ME, Heshmat R, Aminaee T, Ardalan G, et al. Development and evaluation of a questionnaire for assessment of determinants of weight disorders among children and adolescents: The Caspian-IV Study. Int J Prev Med. 2012;3:699–705. [PMC free article] [PubMed] [Google Scholar]
- 18.Geneva, Switzerland: World Health Organization; 1995. World Health Organization. Expert Committee on Physical Status. Physical Status: The Use and Interpretation of Anthropometry; p. 420. WHO Technical Report 854. [PubMed] [Google Scholar]
- 19.Knowles KM, Paiva LL, Sanchez SE, Revilla L, Lopez T, Yasuda MB, et al. Waist Circumference, Body Mass Index, and Other Measures of Adiposity in Predicting Cardiovascular Disease Risk Factors among Peruvian Adults. Int J Hypertens. 2011;2011:931402. doi: 10.4061/2011/931402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl. 2006;450:76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x. [DOI] [PubMed] [Google Scholar]
- 21.Li C, Ford ES, Mokdad AH, Cook S. Recent trends in waist circumference and waist-height ratio among US children and adolescents. Pediatrics. 2006;118:e1390–8. doi: 10.1542/peds.2006-1062. [DOI] [PubMed] [Google Scholar]
- 22.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–76. [PubMed] [Google Scholar]
- 23.Ghassemi H, Harrison G, Mohammad K. An accelerated nutrition transition in Iran. Public Health Nutr. 2002;5:149–55. doi: 10.1079/PHN2001287. [DOI] [PubMed] [Google Scholar]
- 24.Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M, et al. Prevention of non-communicable disease in a population in nutrition transition: Tehran lipid and glucose study phase II. Trials. 2009;10:5. doi: 10.1186/1745-6215-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Al-Hazzaa HM, Abahussain NA, Al-Sobayel HI, Qahwaji DM, Musaiger AO. Physical activity, sedentary behaviors and dietary habits among Saudi adolescents relative to age, gender and region. Int J Behav Nutr Phys Act. 2011;8:140. doi: 10.1186/1479-5868-8-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wrotniak BH, Malete L, Maruapula SD, Jackson J, Shaibu S, Ratcliffe S, et al. Association between socioeconomic status indicators and obesity in adolescent students in Botswana, an African country in rapid nutrition transition. Pediatr Obes. 2012;7:e9–13. doi: 10.1111/j.2047-6310.2011.00023.x. [DOI] [PubMed] [Google Scholar]
- 27.Zaghloul S, Al-Hooti SN, Al-Hamad N, Al-Zenki S, Alomirah H, Alayan I, et al. Evidence for nutrition transition in Kuwait: Over-consumption of macronutrients and obesity. Public Health Nutr. 2013;16:596–607. doi: 10.1017/S1368980012003941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Langevin DD, Kwiatkowski C, McKay MG, Maillet JO, Touger-Decker R, Smith JK, et al. Evaluation of diet quality and weight status of children from a low socioeconomic urban environment supports “at risk” classification. J Am Diet Assoc. 2007;107:1973–7. doi: 10.1016/j.jada.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 29.Després JP, Lemieux I, Bergeron J, Pibarot P, Mathieu P, Larose E, et al. Abdominal obesity and the metabolic syndrome: Contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol. 2008;28:1039–49. doi: 10.1161/ATVBAHA.107.159228. [DOI] [PubMed] [Google Scholar]
- 30.Hsiao PY, Mitchell DC, Coffman DL, Craig Wood G, Hartman TJ, Still C, et al. Dietary patterns and relationship to obesity-related health outcomes and mortality in adults 75 years of age or greater. J Nutr Health Aging. 2013;17:566–72. doi: 10.1007/s12603-013-0014-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu J, Hickson DA, Musani SK, Talegawkar SA, Carithers TC, Tucker KL, et al. Dietary patterns, abdominal visceral adipose tissue, and cardiometabolic risk factors in African Americans: The Jackson heart study. Obesity (Silver Spring) 2013;21:644–51. doi: 10.1038/oby.2012.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ferolla SM, Ferrari TC, Lima ML, Reis TO, Tavares WC, Jr, Couto OF, et al. Dietary patterns in Brazilian patients with nonalcoholic fatty liver disease: A cross-sectional study. Clinics (Sao Paulo) 2013;68:11–7. doi: 10.6061/clinics/2013(01)OA03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang J, Himes JH, Guo Y, Jiang J, Yang L, Lu Q, et al. Birth weight, growth and feeding pattern in early infancy predict overweight/obesity status at two years of age: A birth cohort study of Chinese infants. PLoS One. 2013;8:e64542. doi: 10.1371/journal.pone.0064542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sahni S, Tucker KL, Kiel DP, Quach L, Casey VA, Hannan MT. Milk and yogurt consumption are linked with higher bone mineral density but not with hip fracture: The Framingham Offspring Study. Arch Osteoporos. 2013;8:119. doi: 10.1007/s11657-013-0119-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Izadi V, Kelishadi R, Qorbani M, Esmaeilmotlagh M, Taslimi M, Heshmat R, et al. Duration of breast-feeding and cardiovascular risk factors among Iranian children and adolescents: The CASPIAN III study. Nutrition. 2013;29:744–51. doi: 10.1016/j.nut.2012.10.016. [DOI] [PubMed] [Google Scholar]
- 36.Akter S, Kurotani K, Nanri A, Pham NM, Sato M, Hayabuchi H, et al. Dairy consumption is associated with decreased insulin resistance among the Japanese. Nutr Res. 2013;33:286–92. doi: 10.1016/j.nutres.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 37.Slama K, David-Tchouda S, Plassart JM. Tobacco consumption among young adults in the two French departments of Savoie in 2008. Rev Epidemiol Sante Publique. 2009;57:299–304. doi: 10.1016/j.respe.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 38.Befinoana M, Razanamihaja N. Prevalence of tobacco use and associated factors among teenage students in Madagascar. Sante Publique. 2011;23:465–74. [PubMed] [Google Scholar]
- 39.Kelishadi R, Ardalan G, Gheiratmand R, Majdzadeh R, Delavari A, Heshmat R, et al. CASPIAN Study Group. Smoking behavior and its influencing factors in a national-representative sample of Iranian adolescents: CASPIAN study. Prev Med. 2006;42:423–6. doi: 10.1016/j.ypmed.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 40.Lemstra M, Rogers M, Redgate L, Garner M, Moraros J. Prevalence, risk indicators and outcomes of bullying among on-reserve First Nations youth. Can J Public Health. 2011;102:462–6. doi: 10.1007/BF03404201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lemstra ME, Nielsen G, Rogers MR, Thompson AT, Moraros JS. Risk indicators and outcomes associated with bullying in youth aged 9-15 years. Can J Public Health. 2012;103:9–13. doi: 10.1007/BF03404061. [DOI] [PMC free article] [PubMed] [Google Scholar]


