Abstract
Homeless men are frequently unsheltered and isolated, disconnected from supportive organizations and individuals. However, little research has investigated these men’s social networks. We investigate the structure and composition of homeless men’s social networks, vis-a-vis short- and long-term homelessness with a sample of men drawn randomly from meal lines on Skid Row in Los Angeles. Men continuously homeless for the past six months display networks composed of riskier members when compared to men intermittently homeless during that time. Men who report chronic, long-term homelessness display greater social network fragmentation when compared to non-chronically homeless men. While intermittent homelessness affects network composition in ways that may be addressable with existing interventions, chronic homelessness fragments networks, which may be more difficult to address with those interventions. These findings have implications for access to social support from network members which, in turn, impacts the resources homeless men require from other sources such as the government or NGOs.
Keywords: Homeless men, social networks, chronic homelessness, intermittent homelessness, social support
Men comprise the largest group of homeless in the United States (Burt et al., 1999). Unfortunately, however, homeless men receive less attention in the literature despite evidence that they face the lion’s share of negative outcomes of homelessness and are in greatest need of assistance (Breakey et al., 1989; Calsyn & Morse, 1990; Roll et al., 1999; Stein & Gelberg, 1995; Susser et al., 1989), possibly due to poorer physical health, limited access to health care and prevention services, and greater likelihood of hard drug use and mental health problems when compared with stably housed men, or homeless women and youth (Centers for Disease Control and Prevention, 1997; Magura et al., 2000; Metraux et al., 2004; Rosenberg et al., 2001; St. Lawrence & Brasfield, 1995; Zlotnick & Zerger, 2009).
Homeless men are also the most frequently unsheltered when compared to other homeless, with fewer opportunities to receive support from existing programs. They are also most often isolated, unconnected to others who might provide them with tangible or emotional support (Calsyn & Morse, 1990; Roll et al., 1999), which have been shown to buffer the impact of adverse life events such as physical, mental and emotional trauma, the development of drug and alcohol dependencies and addictions, the decision to participate in risky, possibly transactional sex, and so on (Cohen, 2004; Wong & Piliavin, 2001). Cohen argues that support may directly impact health, or may buffer the impact of stressful events (2004). Thus, even perceived access to tangible and emotional support through an individual’s social network may mitigate the impact of stressful events and lead to better health or health choices, and improved ability to cope with stressful events.
A homeless man is most likely to receive support from his social network: those individuals with whom he interacts on a regular basis. The number and type of individuals that surround a homeless man, known as his network composition, has been shown to be both protective (supportive) and risky (C. Latkin et al., 1995; C. A. Latkin et al., 2003; C. A. Latkin et al., 1996; Montgomery et al., 2002; Neaigus et al., 1994; Neaigus et al., 1996). The set of connections among those individuals, referred to as network structure, has also been shown to be both protective (supportive) and risky (C. Latkin et al., 1995; C. A. Latkin et al., 2003; C. A. Latkin et al., 1996; Montgomery et al., 2002; Neaigus et al., 1994; Neaigus et al., 1996). This suggests that for homeless men, the composition and structure of social networks may have a strong impact on life experiences, affecting access (or perceived access) to support from network members, from shelters, and from other support providers. Understanding the associations between homelessness and men’s social networks allows us to develop interventions appropriate to where in the homelessness trajectory a man may be, and thus best target resources for the best possible outcomes.
Dimensions of homelessness
Generally, the magnitude of homelessness is gauged by a single indicator related to chronic homelessness (often considered long-term or lifetime homelessness). Chronic homelessness is defined by HUD as having spent more than twelve months on the street in one’s lifetime (“McKinney-Vento Homeless Assistance Act,” 1987). While this indicator does reflect lifetime experience of homelessness, it does not completely describe the contours of the homeless experience. It is also important to consider more near-term or recent experiences of homelessness, such as whether an individual has been continuously or intermittently homeless during the past six months (Kuhn & Culhane, 1998). Considering both dimensions of homelessness, long-term and near-term, allows us to better understand how men experience homelessness. It also allows us to compare how these distinct dimensions of homelessness are related to the composition and structure of homeless men’s social networks, and thus impact their ability to buffer stressful outcomes associated with homelessness, as suggested by Cohen and discussed previously. It has been over 25 years since the first study of the personal networks of the homeless was completed by Mitchell (1987). Though this study focused on homeless women, it explored similar ideas of risk and support that this study explores. It has been more than twenty years since researchers argued that it was important to understand the role that social ties play in homelessness (Shlay & Rossi, 1992), though little research directly addressing social networks using systematic network methodologies has been reported in the literature since.
In this study we investigate how two dimensions of homelessness—long-term and near-term homelessness—are related to social network composition and structure to understand how men’s social ties are linked to time spent homeless. Based on existing research, we believe that, in terms of near-term homelessness, being continuously homeless may be associated with increased exposure to high-risk individuals and decreased exposure to protective or supportive individuals. Specifically we posit that continuous, near-term homelessness will be associated with greater proportions of risky network members like drug users and sexual risk takers, and lesser proportions of supportive network members like family. Further, we propose that because the people a homeless man interacts with changes rapidly while they are on the street, chronic homelessness is more strongly associated with network structure than it is with network composition (Calsyn & Morse, 1991). That is, we posit that men who are chronically homeless will have more fragmented networks than those not chronically homeless, as evidenced by more isolated network members (isolates) and groups of two (dyads) and fewer groups of three or more in the networks of chronically homeless men, both overall and among risky subgroups of their networks.
As a contribution to the body of descriptive information regarding homeless populations, and because our study is uniquely capable of comparing chronically and intermittently homeless men with their counterparts, we also present key demographic comparisons (including time homeless) across these dimensions. Because homeless men report higher rates of crack use than their female and youth counterparts (Magura et al., 2000; Metraux et al., 2004; St. Lawrence & Brasfield, 1995; Zlotnick & Zerger, 2009) we also present comparisons of hard drug use (crack, cocaine, methamphetamines, and heroin) across these dimensions. In an effort to identify as many possible defining characteristics associated with these two dimensions of homelessness, we present bivariate statistics rather than multivariate statistics which, while able to control for multiple factors, might possibly obscure important unknown associations.
Methods
Study Participants
Participants were 305 homeless men randomly sampled and interviewed in 13 meal programs in the Skid Row area of Los Angeles. This area is home to the highest concentration of homeless persons in Los Angeles County. Men were eligible if they were age 18 or older, could complete an interview in English, and experienced homelessness in the past 12 months (defined as spending at least one night on the street, or in a shelter, mission, vehicle, public or abandoned building, or voucher hotel because they could not stay in a home of their own or of a family member or friend). As this sample was collected as part of a study of heterosexual risk behavior, all participants reported having vaginal or anal sex with a female partner in the past 6 months. Participants were 45.6 years old on average, 72% were African American, and 86% reported not currently having a regular place to stay. Computer-assisted structured interviews were conducted by trained male interviewers between July and October 2010. Men were paid $30 for participation in the interview, which lasted on average 83 minutes. The research protocol was approved by the institutional review boards of the University of Southern California and the RAND Corporation.
Study Design
To obtain a representative sample of heterosexually active homeless men from the Skid Row area of Los Angeles, we implemented a probability sample of homeless men recruited from meal lines in the study area. The list of meal lines in Skid Row was developed using existing directories of services for homeless individuals and interviews with service providers. Our final list contained 13 meal lines (5 breakfasts, 4 lunches, and 4 dinners) offered by 5 different organizations. Each meal line was investigated to obtain an estimate of the average number of men served daily, which was then used to assign an overall quota to each site approximately proportional to its size. The second stage of the sampling design consisted of drawing a probability sample of homeless men from the 13 distinct meal lines. Men were selected for eligibility screening by their position in line using random number tables. Of the 338 men who screened eligible for the study, 320 men were interviewed (18 refusals). Of these 320: 4 named too few network members, 7 were partial completes/break-offs (when interviews could not be completed because the respondent had to leave suddenly, refused to finish the interview, or otherwise did not fully complete the interview process), and 4 were later found to be repeaters. The final sample size was 305, for a completion rate of 91% (305/334).
Network Data Collection
Men in this study completed a personal network survey nearly identical to one conducted by Clyde Mitchell among homeless women and described in Social Networks in 1987 (Mitchell, 1987). This type of survey has four modules. First, a man provides information about himself such as age and gender. In this module we also collected information on sexual behaviors, drug use, and drinking behaviors and attitudes (among other variables), providing us with the non-structural variables used in our study. Second, a man provides us with a list of twenty network members (also called alters), following standard personal network data collection methods, which have shown that twenty alters is adequate to assess the variability in network structure and composition (Campbell & Lee, 1991; McCarty, 2002; McCarty et al., 1997; McCarty et al., 2007). To address ethical concerns associated with the ability to identify those who appear as secondary participants via the profiles men provided in the social network section of our survey, we requested that men provide only first names for 20 adult network members. In the third survey section, a man provides us with information about his network members, including but not limited to demographics, provision of social support, and the respondent’s perceptions of the network members’ engagement in substance use and risky sex behaviors. In the final module, a man reports his perception of the level of interaction among his network members. The third and fourth modules provide us with the data we use to calculate social network composition and fragmentation, respectively.
Study Variables
We investigate differences across two key homelessness dimensions in our study. Those dimensions are, as mentioned previously, an indicator of continuous homelessness in the near-term (past six months), and an indicator of chronic, long-term homelessness. Along those dimensions we are interested in presenting key differences with respect to respondent demographics, length of time homeless, hard drug use, social network fragmentation, and social network composition (risky and protective). These measures are described in more detail in the following paragraphs.
1. Homelessness Transitions
We define the two measures of homelessness based on two questions associated with the trajectory of men’s time on the street. First, chronic homelessness is defined, based on the commonly accepted HUD definition (“McKinney-Vento Homeless Assistance Act,” 1987), as having spent at least 12 months on the street in one’s lifetime. Of our 305 respondents, 85% (257) qualify as chronically homeless. As a measure of recent homelessness, we define continuous near-term homelessness as having spent all of the past six months on the street. Of our sample, 60% (190) qualify as continuously near-term homeless. Of the 257 chronically homeless, 68% (175) have been living on the street for all six of the past six months, making them continuously homeless in the near-term as well. Table 2 presents a cross-tabulation of chronic homelessness and continuous near-term homelessness in our sample.
Table 2.
Descriptive statistics (mean and standard deviation or percentage) for study variables
| Mean (Percentage) | Standard Deviation | |
|---|---|---|
| Age | 45.56 | 10.33 |
| African American | (72) | |
| Hispanic | (10) | |
| High-School Degree or GED | (73) | |
| Spent at least one night in jail past 6 months | (46) | |
| Employed in the past 6 months | (18) | |
| Monthly Income | $467.57 | $432.28 |
| Total Number of Months Homeless | 64.61 | 72.43 |
| Used Cocaine in the Past 6 Months | (12) | |
| Used Crack in the Past 6 Months | (40) | |
| Used Methamphetamine in the Past 6 Months | (11) | |
| Used Heroin in the Past 6 Months | (7) | |
| Network Isolates | 9.94 | 6.40 |
| Network Dyads | .64 | .91 |
| Network Components | 1.23 | .92 |
| Alcohol Using Isolates | 3.75 | 4.44 |
| Alcohol Using Dyads | .36 | .71 |
| Alcohol Using Components | .33 | .56 |
| Drug Using Isolates | 3.44 | 4.25 |
| Drug Using Dyads | .27 | .62 |
| Drug Using Components | .33 | .57 |
| Sexual Risk Taking Isolates | 2.54 | 3.83 |
| Sexual Risk Taking Dyads | .17 | .43 |
| Sexual Risk Taking Components | .19 | .47 |
| Number of Family Members | 4.48 | 4.51 |
| Number of Sex Partners | 3.03 | 3.42 |
| Number of Other Homeless | 3.85 | 4.77 |
| Number of Alters who Drink to Intoxication | 6.43 | 5.75 |
| Number of Alters who Use Drugs | 5.95 | 5.90 |
| Number of Alters who Have Risky Sex | 4.09 | 5.32 |
| Number of ‘Responsible’ Alters | .84 | 1.84 |
| Number of Alters who Care | 6.48 | 5.65 |
| Number of Alters who Provide Support | 7.78 | 6.02 |
2. Demographics, Homelessness, and Hard Drug Use Indicators
Age was measured in years. Race indicated whether the respondent was African American or not or Hispanic or not. Education was a dichotomous measure indicating whether the respondent had graduated high school or had a GED or more. We compared whether respondents had spent any night in the past six months incarcerated. Employment was a dichotomous measure of whether the respondent had been employed at all in the past six months. Income was the amount of money a respondent received in the past 30 days from panhandling, work or other sources such as disability. We compared the total number of months homeless our respondents reported. We investigated hard drug use with dichotomous measures of whether respondents had used cocaine, crack, methamphetamines or heroin in the past six months (to harmonize with our near-term homelessness measure) (Wenzel et al., 2009).
3. Social Network Fragmentation
We chose measures of network structure that, when considered together, indicate network fragmentation. Specifically we are interested in the number of network members who were unconnected to respondents’ other alters (isolates), the number of small groups of two (dyads) and the number of groups of three or more network members (components ≥ 3), because high numbers of isolates and dyads, and low numbers of groups of any size larger than 2 indicate network fragmentation. We looked into these network fragmentation measures across all network members and within subgroups of network members thought to drink alcohol to intoxication, use drugs, or have risky sex (without a condom, multiple partners, etc.).
4. Social Network Composition
Because all respondents reported 20 network members, and because we are interested in the overall impact of the number of network members who are protective and risky, we compared the count of network members who were reported to have specific characteristics or were reported to have been met in particular social environments: To gauge the support available in these men’s networks, we counted the number of family members, sex partners, and other homeless individuals in the network. To gauge risky peers, we counted the number of alters who were thought to drink to intoxication, use drugs, or have risky sex. To gauge protective peers, we counted the number of alters thought to be ‘responsible’, who ‘cared for the respondent’, and who would ‘provide assistance’ to the respondent no matter what. Descriptive statistics for these variables appear in Table 2.
Analytic Approach
Because little is known about homeless men’s social networks, we adopt an exploratory approach, assessing relationships among our two dimensions of homelessness without controlling for other factors, the likely approach for confirmatory analyses. The goal is to present relationships worthy of exploration and confirmation in future research. Because our dimensions are each dichotomous, we present the result of ANOVAs (accounting for sampling weights) associated with our demographic and social network measures.
Results
Demographics, Homelessness, and Hard Drug Use
For near-term homelessness, analyses revealed that men who were continuously homeless for the past six months were more likely to be Hispanic, unemployed, have a lower income, and to have spent more total months homeless in their lifetimes than their intermittently homeless counterparts. For long-term homelessness, men who were chronically homeless were more likely to be older, African-American, less educated, to have spent at least one night in jail, to be unemployed, to have spent more total months homeless in their lifetimes, and to have used crack in the past six months than their non-chronically homeless counterparts.
Social Network Fragmentation
For near-term homelessness, men who were continuously homeless for the past six months reported more isolates thought to engage in drug use and risky sex compared to their intermittently homeless peers. The associations suggest that men who have been continuously homeless for the past six months may have more fragmented network subgroups than their intermittently homeless counterparts. For long-term homelessness, men who were chronically homeless had more overall isolates, fewer overall components, fewer alcohol using dyads, more drug using isolates, fewer drug using dyads and fewer dyads and components made up of those thought to participate in risky sex than their non-chronically homeless counterparts. Taken together these findings suggest that chronic homelessness is associated with fragmented social networks among homeless men.
Social Network Composition
Men who reported continuous near-term homelessness had networks composed of more homeless individuals, fewer family members, more drug users, more people thought to engage in risky sex, fewer responsible adults, fewer personal opinion leaders, and fewer people who had jobs or were in school than their intermittently homeless counterparts. These findings suggest that continuous near-term homelessness is associated with more risky and less supportive social networks among homeless men. Men who reported chronic homelessness had networks composed of more people they were emotionally close to, and more people who would provide them with support than their non-chronically homeless counterparts. These findings suggest that chronically homeless men may be creating support structures for themselves within their networks, possibly formed from others on the street.
Overall Synthesis
Comparing our two homelessness dimensions—near-term and long term—and their relationships with network fragmentation and composition, an important pattern arises. There are only two significant associations between near-term homelessness and network fragmentation as defined by the measures in our study; but there are seven significant associations between chronic homelessness and network fragmentation. This suggests that long-term homelessness, when compared to near-term homelessness, has a stronger relationship to network structure. On the other hand, there are seven significant associations between near-term homelessness and network composition and only three significant associations between long-term homelessness and network composition as defined by these network measures. This suggests that long-term homelessness doesn’t have as strong a relationship with network composition as defined by these measures as does near-term homelessness. In short, near-term homelessness appears more related to network composition while long-term homelessness appears more related to network fragmentation.
Comment
This study responds to Shlay and Rossi’s still largely unaddressed call for social research into the relationship between social relationships and homelessness (Shlay & Rossi, 1992)and to the more recent call for continued investigations of individual risk factors (such as support networks and interpersonal relationships) for homelessness from Lee and colleagues (Lee et al., 2010). These analyses have shown that continuous near-term homelessness (similar to what Kuhn and Culhane (1998) would term episodic homelessness and chronic homelessness are associated with risky individual characteristics, risky network composition and fragmented network structure. We posited that near-term homelessness would be associated with those individuals a homeless man knows (rather than to the pattern of connections among the people a man knows), increasing the proportion of risky network members and decreasing the proportion of protective network members, which our analyses support. However, near-term homelessness is also associated with network sub-structures in a few ways. Further, we posited that chronic homelessness has less association with network composition than it does with network structure, evidenced by increasing network fragmentation. Our analyses also support this conjecture. Having spent the past six months on the street may be linked to limited opportunity to interact with protective network members, with changes seen in the composition of homeless men’s social networks.
Among the chronically homeless we see few (albeit important) associations with the composition of men’s social networks, but we do see many important associations with the structure of men’s social networks. From these analyses, it seems that in the short term (by definition, less than six months), the composition of homeless men’s social networks changes and the structure of their risky subgroups tends to fragment. In the longer term, chronic homelessness (by definition, a minimum of 12 months) seems associated with further changes in network composition as men attempt to recreate supportive networks from their risky network members; but, most importantly, chronic homelessness seems associated with fragmentation of the overall network, suggesting larger-scale fragmentation that likely signals the ultimate dissolution of these men’s social networks.
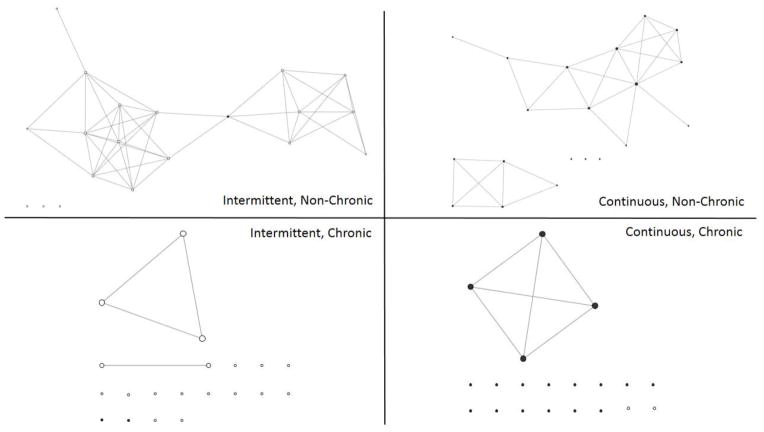
In short, intermittent homelessness affects network composition in ways that are fairly easy to counteract. Chronic homelessness fragments networks in ways that are more difficult to address. The fact that homeless men, no matter who long they have been homeless, are less likely to receive support from service providers and are more likely to spend their days and nights alone suggests limited options for those networks to be reconstituted. However, if they are reconstituted, they are more likely to be comprised of risky individuals who are perceived to provide support, which echoes some findings of Wong and Piliavin regarding the availability of social resources among the homeless (Wong & Piliavin, 2001). These findings are summarized in Figure 1, which presents exemplar social networks for respondents in each of the four possible classes in our taxonomy: chronically but intermittently homeless in the near term, chronically and continuously homeless in the near term, non-chronic and intermittently homeless, and non-chronic but continuously homeless. In this figure, lines represent connections among a homeless man’s network members, and dark nodes represent risky network members. These diagrams very clearly suggest two areas for future research. The first is to incorporate GIS technologies so that these maps can display the spatial distribution of network alters, and thus may suggest how urban geography is associated with network structure and composition. The second is to enroll network alters and explore the structure and composition of the second-order networks that surround our respondents, to assess indirect protective and risky network features.
Figure 1.
Exemplar networks of homeless men distinguished by intermittent homeless and chronic homelessness
This study should be considered in light of some limitations. These limitations include a focus on heterosexual men who have recently had sex (which may impact the age of our respondents) and the reliance on respondents’ reports of the attributes and behaviors of their network members that may introduce bias. Another limitation is the cross-sectional design, which precludes the examination of actual changes in networks over time and whether they are antecedents or consequences of time homeless. For example, an erosion of network structure may lead to homelessness, which in turn is followed by an increase in risky network composition, as Shinn’s work with homeless families suggests (Shinn et al., 1991). A third is the previously explained reliance here on univariate analyses, which do not control for demographic or other factors and thus may misrepresent associations. Finally, the findings may not generalize to populations of homeless men outside of Los Angeles County. Nonetheless, we believe that these findings may indicate the kinds of changes in social context that homeless men may experience over the timeline of their homelessness, regardless of where they are in the United States.
Practically, our results are well situated within the policy debates surrounding chronic homelessness highlighted by Burt (2003) in 2002 and in line with Housing First approaches. They suggest, however, that the greatest changes in men’s social networks may occur early in the history of their homelessness before men enter what Wolch and colleagues have called the ‘culture of chronicity’ (Wolch et al., 1988). They also point out that determining the impact an intervention will have relative to position in the homelessness career is key, with no single best outcome evident. We believe that if service providers can work to provide recently homeless men with housing and then, as quickly as possible, other services that focus on building appropriate support networks, their interventions may have the greatest impact on a man’s social network and may be more likely to minimize the expected costs and other individual sequelae of homelessness (Culhane, 2008). By moving non-chronically homeless men into housed situations and in contact with protective individuals, these men’s networks may begin to reconstitute themselves with protective network members and network inter-connections may re-form among these new, protective network members. The longer men are on the street, however, the more difficult it may be to impact their social networks, though existing interventions provided for by Continuum of Care (Couzens, 1997) or Housing First approaches (Stefancic & Tsemberis, 2007) may, in the long run, also begin to change their social networks. The primary outcomes for these men, however, may be satisfying basic needs including food security and housing, with changes in social networks as secondary to addressing more dire individual needs that are the result of long-term homelessness (e.g., malnutrition, chronic illness, mental health problems)
Table 1.
Cross-tabulation of chronic and continuous near-term homelessness.
| Chronic Homelessness | Non-chronic Homelessness | Total | |
|---|---|---|---|
| Continuous Near-Term Homelessness | 175 | 15 | 190 |
| Intermittent Near-Term Homelessness | 82 | 33 | 115 |
| Total | 257 | 48 | 305 |
Table 3.
Comparison of demographic, homelessness, and hard drug use variables for long-term homelessness and near-term homelessness.
| Long-term Homelessness: Mean (Std. Dev.) | Near-term Homelessness: Mean (Std. Dev.) | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Chronic | Non-Chronic | F | Sig. | Continuous | Intermittent | F | Sig. | |
|
| ||||||||
| Age | 47.06 (9.80) | 38.51 (9.92) | 33.40 | <0.001 | 45.78 (10.59) | 45.33 (10.09) | 0.15 | 0.7 |
| African-American | 0.76 (0.43) | 0.50 (0.50) | 15.00 | <0.001 | 0.70 (0.46) | 0.74 (0.44) | 0.72 | 0.4 |
| Hispanic | 0.11 (0.31) | 0.10 (0.30) | 0.06 | 0.81 | 0.15 (0.35) | 0.06 (0.24) | 6.04 | 0.01 |
| High-School Degree or GED | 0.71 (0.46) | 0.86 (0.35) | 5.56 | 0.02 | 0.70 (0.46) | 0.77 (0.42) | 2.05 | 0.15 |
| Spent at least one night in jail past six months | 0.50 (0.50) | 0.27 (0.45) | 9.63 | <0.001 | 0.47 (0.5) | 0.46 (0.50) | 0.03 | 0.87 |
| Employed in the past six months | 0.15 (0.36) | 0.3 (0.46) | 6.87 | 0.01 | 0.12 (0.33) | 0.24 (0.43) | 6.97 | 0.01 |
| Monthly Income | 474.81 (412.62) | 433.54 (517.94) | 0.40 | 0.53 | 410.64 (370.06) | 528.87 (484.40) | 5.79 | 0.02 |
| Total number of Months Homeless | 77.35 (73.73) | 4.73 (3.07) | 51.75 | <0.001 | 76.27 (78.32) | 52.06 (63.41) | 8.72 | <0.001 |
| Used crack in the past six months | 0.46 (0.50) | 0.09 (0.29) | 27.66 | <0.001 | 0.39 (0.49) | 0.40 (0.49) | 0.04 | 0.84 |
| Used cocaine in the past six months | 0.13 (0.33) | 0.09 (0.28) | 0.73 | 0.39 | 0.09 (0.29) | 0.15 (0.36) | 2.85 | 0.09 |
| Used methamphetamine in the past six months | 0.11 (0.31) | 0.11 (0.32) | 0.02 | 0.88 | 0.11 (0.31) | 0.11 (0.31) | 0.01 | 0.91 |
| Used heroin in the past six months | 0.09 (0.28) | 0.03 (0.16) | 2.21 | 0.14 | 0.09 (0.28) | 0.06 (0.24) | 0.59 | 0.44 |
Table 4.
Comparison of social network fragmentation measures for long-term homelessness and near-term homelessness.
| Long-term Homelessness: Mean (Std Dev.) | Near-term Homelessness: Mean (Std. Dev.) | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Chronic | Non-Chronic | F | Sig. | Continuous | Intermittent | F | Sig. | |
|
| ||||||||
| Network Isolates | 10.30 (6.39) | 8.25 (6.27) | 4.58 | 0.03 | 10.22 (6.35) | 9.63 (6.46) | 0.65 | 0.42 |
| Network Dyads | 0.62 (0.90) | 0.69 (0.98) | 0.25 | 0.61 | 0.62 (0.91) | 0.65 (0.92) | 0.11 | 0.74 |
| Network Components | 1.18 (0.90) | 1.49 (0.96) | 5.06 | 0.03 | 1.19 (0.90) | 1.28 (0.93) | 0.68 | 0.41 |
| Alcohol Using Isolates | 3.78 (4.42) | 3.59 (4.61) | 0.08 | 0.78 | 4.07 (4.27) | 3.40 (4.61) | 1.70 | 0.19 |
| Alcohol Using Dyads | 0.31 (0.60) | 0.58 (1.09) | 6.57 | 0.01 | 0.31 (0.65) | 0.40 (0.77) | 1.12 | 0.29 |
| Alcohol Using Components | 0.31 (0.51) | 0.41 (0.72) | 1.56 | 0.21 | 0.35 (0.55) | 0.30 (0.56) | 0.65 | 0.42 |
| Drug Using Isolates | 3.68 (4.45) | 2.32 (2.87) | 4.52 | 0.03 | 3.94 (4.47) | 2.90 (3.93) | 4.57 | 0.03 |
| Drug Using Dyads | 0.22 (0.49) | 0.48 (1.03) | 8.09 | <0.001 | 0.24 (0.49) | 0.29 (0.74) | 0.48 | 0.49 |
| Drug Using Components | 0.31 (0.53) | 0.40 (0.69) | 1.04 | 0.31 | 0.36 (0.59) | 0.29 (0.54) | 1.40 | 0.24 |
| Sexual Risk Taking Isolates | 2.50 (3.69) | 2.72 (4.49) | 0.14 | 0.7 | 3.05 (4.14) | 2.00 (3.42) | 5.79 | 0.02 |
| Sexual Risk Taking Dyads | 0.13 (0.38) | 0.33 (0.59) | 9.79 | <0.001 | 0.17 (0.42) | 0.16 (0.45) | 0.06 | 0.80 |
| Sexual Risk Taking Components | 0.17 (0.43) | 0.32 (0.60) | 4.79 | 0.03 | 0.21 (0.49) | 0.18 (0.44) | 0.32 | 0.57 |
Table 5.
Comparison of social network composition measures for long-term homelessness and near-term homelessness.
| Number of | Long-term Homelessness: Mean (Std. Dev.) | Near-Term Homelessness: Mean (Std. Dev.) | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Chronic | Non-Chronic | F | Sig. | Continuous | Intermittent | F | Sig. | |
| Family Members | 4.47 (4.51) | 4.53 (4.55) | 0.01 | 0.93 | 3.98 (4.13) | 5.02 (4.84) | 4.10 | 0.04 |
| Sex Partners | 3.07 (3.59) | 2.83 (2.47) | 0.21 | 0.65 | 3.15 (3.75) | 2.90 (3.04) | 0.41 | 0.52 |
| Other Homeless | 3.98 (4.96) | 3.25 (3.73) | 1.05 | 0.31 | 4.83 (5.29) | 2.80 (3.88) | 14.50 | <0.001 |
| Alters who Drink to Intoxication | 6.19 (5.55) | 7.55 (6.54) | 2.49 | 0.12 | 6.96 (5.73) | 5.86 (5.73) | 2.78 | 0.10 |
| Alters who Use Drugs | 6.04 (5.91) | 5.53 (5.89) | 0.33 | 0.56 | 6.66 (6.11) | 5.19 (5.58) | 4.79 | 0.03 |
| Alters who Have Risky Sex | 3.91 (5.16) | 4.94 (6.02) | 1.66 | 0.20 | 4.85 (5.69) | 3.27 (4.78) | 6.85 | 0.01 |
| ‘Responsible’ Alters | 0.78 (1.87) | 1.11 (1.66) | 1.41 | 0.24 | 0.52 (1.17) | 1.18 (2.31) | 10.21 | <0.001 |
| Alters who Care About Respondent | 6.80 (5.83) | 5.01 (4.47) | 4.48 | 0.04 | 6.26 (5.74) | 6.72 (5.57) | 0.50 | 0.48 |
| Alters who Provide Support to Respondent | 8.09 (6.23) | 6.31 (4.63) | 3.94 | 0.05 | 7.37 (6.05) | 8.22 (5.97) | 1.53 | 0.22 |
Acknowledgments
This study was supported with funds from NIDA grant R01HD059307: Heterosexual HIV Risk Behaviors in Homeless Men. We would like to acknowledge the RAND Survey Research Group for their contribution to this study. We also acknowledge the contributions of our Technical Assistance Group, Skid Row Service Providers, and the homeless men who consented to participate in this study.
Contributor Information
Harold D. Green, Jr., Email: hgreen@rand.org.
Joan S. Tucker, Email: jtucker@rand.org.
Daniela Golinelli, Email: daniela@rand.org.
Suzanne L. Wenzel, Email: swenzel@usc.edu.
References
- Breakey WR, Fischer PJ, Kramer M, Nestadt G, Romanoski AJ, Ross A, et al. Health and mental health problems of homeless men and women in Baltimore. JAMA. 1989;262(10):1352–1357. [PubMed] [Google Scholar]
- Burt MR. Chronic homelessness: Emergence of a public policy. Fordham Urban Law Journal. 2003;30(3):1267. [Google Scholar]
- Burt MR, Aron LY, Douglas T, Valente J, Lee E, Iwen B. Findings of the national survey of homeless assistance providers and clients. Washington, DC: Urban Institute; 1999. Homelessness: Programs and the people they serve. [Google Scholar]
- Calsyn RJ, Morse G. Homeless men and women: Commonalities and a service gender gap. American Journal of Community Psychology. 1990;18(4):597–608. doi: 10.1007/BF00938062. [DOI] [PubMed] [Google Scholar]
- Calsyn RJ, Morse GA. Predicting chronic homelessness. Urban Affairs Review. 1991;27(1):155–164. [Google Scholar]
- Campbell KE, Lee BA. Name generators in surveys of personal networks. Social Networks. 1991;13(3):203–221. [Google Scholar]
- Centers for Disease Control and Prevention. Community-based HIV prevention in presumably underserved populations: July–September 1995. JAMA. 1997;277(11):876–877. [PubMed] [Google Scholar]
- Cohen S. Social relationships and health. American Psychologist. 2004;59(8):676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Couzens SE. Priority: Home! A true priority? An analysis of the federal plan to break the cycle of homelessness. Journal of Social Distress and the Homeless. 1997;6(4):275–282. [Google Scholar]
- Culhane DP. The cost of homelessness: A perspective from the United States. European Journal of Homelessness. 2008;2(1):97–114. [Google Scholar]
- Kuhn R, Culhane DP. Applying cluster analysis to test a typology of homelessness by pattern of shelter utilization: Results from the analysis of administrative data. American Journal of Community Psychology. 1998;26(2):207–232. doi: 10.1023/a:1022176402357. [DOI] [PubMed] [Google Scholar]
- Latkin C, Mandell W, Vlahov D, Knowlton A, Oziemkowska M, Celentano D. Personal network characteristics as antecedents to needle sharing and shooting gallery attendance. Social Networks. 1995;17(3–4):219–228. [Google Scholar]
- Latkin CA, Forman V, Knowlton A, Sherman S. Norms, social networks, and HIV-related risk behaviors among urban disadvantaged drug users. Social Science & Medicine. 2003;56:465–476. doi: 10.1016/s0277-9536(02)00047-3. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Mandell W, Vlahov D. The relationship between risk networks, patterns of crack cocaine and alcohol consumption and HIV-related sexual behaviors among adult injection drug users: A prospective study. Drug and Alcohol Dependence. 1996;42:175–181. doi: 10.1016/s0376-8716(96)01279-3. [DOI] [PubMed] [Google Scholar]
- Lee BA, Tyler KA, Wright JD. The new homelessness revisited. Annual Review of Sociology. 2010;36:501–521. doi: 10.1146/annurev-soc-070308-115940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magura S, Nwakeze PC, Rosenblum A, Joseph H. Substance misuse and related infectious diseases in a soup kitchen population. Substance Use & Misuse. 2000;35(4):551–583. doi: 10.3109/10826080009147472. [DOI] [PubMed] [Google Scholar]
- McCarty C. Structure in personal networks. Journal of Social Structure. 2002;3:1. [Google Scholar]
- McCarty C, Bernard H, Killworth P, Shelley GA, Johnsen EC. Eliciting representative samples of personal networks. Social Networks. 1997;19:303–323. [Google Scholar]
- McCarty C, Killworth PD, Rennell J. Impact of methods for reducing respondent burden on personal network structural measures. Social Networks. 2007;29(2):300–315. [Google Scholar]
- McKinney-Vento Homeless Assistance Act 1987 PL100-77: U.S. Government
- Metraux S, Metzger DS, Culhane DP. Homelessness and HIV risk behaviors among injection drug users. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2004;81(4):618–629. doi: 10.1093/jurban/jth145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JC. The components of strong ties among homeless women. Social Networks. 1987;9(1):37–47. [Google Scholar]
- Montgomery SB, Hyde J, De Rosa CJ, Rohrbach LA, Ennett S, Harvey SM, et al. Gender differences in HIV risk behaviors among young injectors and their social network members. American Journal of Drug and Alcohol Abuse. 2002;28(3):453–475. doi: 10.1081/ada-120006736. [DOI] [PubMed] [Google Scholar]
- Neaigus A, Friedman SR, Curtis R, Des Jarlais DC, Furst RT, Jose B, et al. The relevance of drug injectors’ social and risk networks for understanding and preventing HIV infection. Social Science and Medicine. 1994;38:67–78. doi: 10.1016/0277-9536(94)90301-8. [DOI] [PubMed] [Google Scholar]
- Neaigus A, Friedman SR, Jose B, Goldstein MF, Curtis R, Il defonso G, et al. High-risk personal networks and syringe sharing as risk factors for HIV infection among new drug injectors. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 1996;11:499–509. doi: 10.1097/00042560-199604150-00011. [DOI] [PubMed] [Google Scholar]
- Roll CN, Toro PA, Ortola GL. Characteristics and experiences of homeless adults: A comparison of single men, single women, and women with children. Journal of Community Psychology. 1999;27(2):189–198. [Google Scholar]
- Rosenberg SD, Goodman LA, Osher FC, Swartz MS, Essock SM, Butterfield MI, et al. Prevalence of HIV, hepatitis B, and hepatitis C in people with severe mental illness. American Journal of Public Health. 2001;91(1):31–37. doi: 10.2105/ajph.91.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinn M, Knickman JR, Weitzman BC. Social relationships and vulnerability to becoming homeless among poor families. American Psychologist. 1991;46(11):1180–1187. [PubMed] [Google Scholar]
- Shlay AB, Rossi PH. Social-science research and contemporary-studies of homelessness. Annual Review of Sociology. 1992;18:129–160. [Google Scholar]
- St Lawrence JS, Brasfield TL. HIV risk behavior among homeless adults. AIDS Education and Prevention. 1995;7(1):22–31. [PubMed] [Google Scholar]
- Stefancic A, Tsemberis S. Housing first for long-term shelter dwellers with psychiatric disabilities in a suburban county: A four-year study of housing access and retention. Journal of Primary Prevention. 2007;28(3–4):265–279. doi: 10.1007/s10935-007-0093-9. [DOI] [PubMed] [Google Scholar]
- Stein JA, Gelberg L. Homeless men and women: Differential associations among substance abuse, psychosocial factors, and severity of homelessness. Experimental and Clinical Psychopharmacology. 1995;3(1):75–86. [Google Scholar]
- Susser E, Struening EL, Conover S. Psychiatric-problems in homeless men. Lifetime psychosis, substance use, and current distress in new arrivals at New York City shelters. Archives of General Psychiatry. 1989;46(9):845–850. doi: 10.1001/archpsyc.1989.01810090087012. [DOI] [PubMed] [Google Scholar]
- Wenzel SL, Green HD, Jr, Tucker JS, Golinelli D, Kennedy DP, Ryan G, et al. The social context of homeless women’s alcohol and drug use. Drug and Alcohol Dependence. 2009;105(1–2):16–23. doi: 10.1016/j.drugalcdep.2009.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolch JR, Dear M, Akita A. Explaining homelessness. Journal of the American Planning Association. 1988;54(4):443–453. [Google Scholar]
- Wong YLI, Piliavin I. Stressors, resources, and distress among homeless persons: A longitudinal analysis. Social Science and Medicine. 2001;52(7):1029–1042. doi: 10.1016/s0277-9536(00)00209-4. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Zerger S. Survey findings on characteristics and health status of clients treated by the federally funded (US) Health Care for the Homeless Programs. Health Soc Care Community. 2009;17(1):18–26. doi: 10.1111/j.1365-2524.2008.00793.x. [DOI] [PubMed] [Google Scholar]