Abstract
Background/Objective
Dysmenorrhea is highly prevalent among adolescent women and a major cause of activity restriction. Standard pharmaceuticals used to treat dysmenorrhea are not effective for all women and have side effects that limit their use. Our study objective was to examine feasibility, acceptability, and preliminary effects of acupuncture point injection of vitamin K1 as an alternative treatment for primary dysmenorrhea among US women.
Methods/Design
We conducted a pilot study using a crossover trial design. Women with primary dysmenorrhea were randomized to receive vitamin K1 injection in the Spleen-6 acupuncture point at the start of menstruation followed by saline in a non-acupuncture point after two months, or the reverse order of treatments.
Setting/Participants
The study was conducted in the San Francisco Bay Area among women 18 and 25 years of age diagnosed with primary dysmenorrhea; fourteen women completed all study visits.
Primary Outcome Measure
Dysmenorrhea pain intensity was measured using a 0–10 numeric rating scale before and after injections.
Results
Women had an average 2.5 point decrease in pain after vitamin K1 injection in Spleen-6 (p < 0.001) compared with a 1.8 point decrease after saline (p < 0.001). Change scores of vitamin K1 compared with saline injection approached statistical significance (p < 0.10). Intensity and duration of menstrual symptoms measured by the Cox Retrospective Symptom Score also decreased following injections. After participating, 94% would still agree to go through with the injection therapy and 77% reported they would come every month were the treatment available.
Conclusions
Findings suggest high acceptability of acupuncture point injection of vitamin K1 as treatment for primary dysmenorrhea among young women in San Francisco. Pain decreased with both treatments, with a trend toward greater pain reduction for vitamin K1/Spleen-6 injection. This is consistent with outcomes from the Obstetrics & Gynecology Hospital in Shanghai, China, where the protocol was developed.
Keywords: acupuncture point injection, primary dysmenorrhea, vitamin K1, phylloquinone
Introduction
Dysmenorrhea, the occurrence of painful menstrual cramping of the uterus, is a major cause of activity restriction and absences from school and work among young women.1–3 It is a common complaint, affecting as many as 85% of women; up to 20% of whom experience severe pain and may be incapacitated for 1–3 days each menstrual cycle.4,5 Primary dysmenorrhea, defined as menstrual pain not caused by any specific disease pathology, typically begins 6 to 12 months following menarche when ovulatory cycles are established.1 Dysmenorrhea is caused by an excess release of prostaglandins that causes uterine cramping; these contractions lead to uterine hypoxia.6 Other symptoms, such as backache, nausea, vomiting, and diarrhea that accompany dysmenorrhea are also thought to result from the release of prostaglandins.6 Standard treatments for dysmenorrhea in the United States and Europe include nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, and hormonal contraceptive methods such as oral contraceptives pills (OCs).6 NSAIDs act as anti-prostaglandins and have well-established efficacy for treating dysmenorrhea.7,8 NSAIDs, however, have a failure rate as high as 20–25% and are associated with side effects such as gastrointestinal complaints and mild neurological symptoms.7,8 OCs are frequently prescribed for the treatment of dysmenorrhea despite limited evidence that they decrease pain.9 Many women prefer not to use hormonal contraception and others discontinue use due to side effects such as breakthrough bleeding. About 54% of women discontinue the use of OCs in the first year of use, primarily due to side effects.10 Other options are needed for women with unmitigated dysmenorrhea since NSAID’s and OC’s are not efficacious among all women and have side effects that limit their use.
Acupuncture point injection is the hypodermic injection of a small amount of drug, vitamin, saline, or plant extract at an acupuncture point. This innovative technique has evolved from traditionally-based Asian medicine, and has been in routine use in China and Korea for the past 40 years.11 Compared to standard acupuncture, which usually involves needles inserted at multiple points and left in place for 20–60 minutes, acupuncture point injection is: 1) easily administered; 2) less time intensive; and 3) easily standardized and replicated.12 Clinical benefits of acupuncture point injection may include enhanced pain relief, rapid treatment response, and prolonged treatment effects across a variety of pain conditions, such as arthritis, musculoskeletal pain, and chronic headaches.13–15 Acupuncture point injection has also been used for the treatment of dysmenorrhea since at least 1985.16–20 Studies conducted at the Menstrual Disorder Center at the Obstetrics & Gynecology Hospital in Shanghai, China indicate that acupuncture point injection with vitamin K3 at Spleen-6 (SP6) relieves pain from dysmenorrhea within 30 minutes, increases participation in daily activities, reduces number of hours in bed, and reduces the amount of pain medication ingested.16–19 Whether this treatment is acceptable to women in the US is unknown.
Utilization of acupuncture has risen in the United States,21 but acupuncture point injection is relatively uncommon. This study was designed to: (1) assess the feasibility and acceptability of acupuncture point injection treatment for dysmenorrhea among a sample of women in the United States; and (2) collect and compare preliminary data on the efficacy and safety of acupuncture point injection of vitamin K1 at SP6 versus an active control (saline injection at a non-acupuncture point) for the treatment of primary dysmenorrhea. The study focuses on vitamin K1 because it is the form of vitamin K widely available in clinical settings in the United States. Vitamins K3 and K1 have similar prophylactic effects for hemorrhage among newborns but have different safety profiles. High doses of vitamin K1 are not associated with toxicity,22 whereas vitamin K3 has been associated with liver toxicity, jaundice, and hemolytic anemia in infants.23 The extent to which vitamins K1 and K3 have comparable therapeutic benefits for dysmenorrhea is unknown, but a pilot study using vitamin K1 conducted in Italy reported similar effects to studies using vitamin K3 conducted in China.24
Methods
The University of California, San Francisco (UCSF) Committee on Human Research and the UCSF Clinical Research Center reviewed and approved all study procedures.
Trial design
The study employed a crossover design in which all participants received two treatments over the course of the study. Participants were randomized to two groups. The first group received acupuncture point injection with vitamin K1 in SP6 at Time 1; following a washout period of at least two months, they received a saline injection in a non-acupuncture point. Participants randomized to the second group received the injections in the reverse order, saline at Time 1 and vitamin K1 at Time 2. All injections were administered within 2 days after the onset of painful menstruation.
Participants
Young women between the ages of 18 and 25 years with primary dysmenorrhea were eligible for this study. The study defined primary dysmenorrhea as recurrent painful periods for six months or more, that was not relieved, or only partially relieved, by any other treatment. Participants were nulliparas, English speaking, with regular menstrual cycles for the past six months, who had a working telephone. Exclusion criteria included: current pregnancy or history of term pregnancy; history of abdominal surgery; diagnosed or suspected acute, chronic conditions; concomitant therapy for acute or chronic pain; use of hormonal contraception; current treatment with anti-coagulant drugs for any reason; intolerance to NSAIDs or aspirin; known allergy to vitamin K; history of pelvic inflammatory disease or chlamydia in the past year; bleeding or non-cyclic pelvic pain; any plans to be out of area during the five months of treatment cycles; and dysmenorrhea due to any other suspected or recognized causes.
Study participants were recruited from outpatient clinics at local community health centers in San Francisco, referred by physicians and nurses at the obstetrics and gynecology department of local hospitals, or responded to flyers and advertisements. Prospective participants who contacted study staff were pre-screened by telephone based on study inclusion and exclusion criteria. Prior to enrollment, the study coordinator reviewed the study details, verified participant’s understanding, and consented each participant. Diagnosis of primary dysmenorrhea was confirmed by the nurse practitioner based on history and physical examination. All in-person consent and screening procedures were conducted at the UCSF Clinical Research Center. Study visits were conducted at one of three UCSF clinic sites based on convenience for the study participant. Participants were offered an incentive of $40 cash for each injection visit and a $10 gift card for follow-up surveys completed.
Intervention
Since injection is outside the scope of practice for licensed acupuncturists in the state of California, study procedures were performed by nurse practitioners. Prior to study implementation, two nurse practitioners were trained by a senior acupuncturist with extensive traditional Chinese medicine (TCM) training and clinical practice in the US and in China. The nurse practitioners were trained to: (1) identify acupuncture point SP6; (2) identify the designated non-acupuncture control point; and (3) conduct acupuncture point injection therapy. Training also included a discussion of TCM needling philosophy regarding de qi, defined as a patient’s sensation of dull ache or heaviness near needle insertion and a practitioner’s perception of needle grasp that is thought to enhance acupuncture treatment benefits.25 De qi may have occurred during injections, but it was not an expected or measured outcome.
The two trained nurse practitioners performed all injections involved with the study. Injection treatment was administered to study participants presenting in pain, during the first 2 days of their menstrual cycle. Acupuncture point injections were administered bilaterally in both legs in SP6. SP6 is located on the lower leg, three cun or three transverse lengths of the patient’s middle phalanx of the index finger, proximal to the peak of the medial malleolus. This area is just along the posterior aspect of the tibial bone. The injected muscle was the soleus. SP6 can sometimes be palpated as a depression on the posterior border of the tibial bone. After ascertaining the correct placement of the needle, the skin around SP6 was cleaned with alcohol solution. Using a # 23 gauge 1 inch long needle, the nurse pracitioner inserted the needle 2.5 to 3 cm deep into the point and 5 mg/0.5ml of vitamin K1 was injected intra-muscularly. The needle was removed, and the point patted with gauze pads if bleeding was present.
Saline injection was used as a control for this study. Volume and syringe needles were identical to those used for acupuncture point injection of vitamin K1. Both the right and left leg of the participant were injected intramuscularly in a standardized non-acupuncture point located 1 cun (width of thumb) medial to the Liver channel and 5 cun above the medial malleolus. The location of this non-acupuncture point has been used as a control for the acupuncture point SP6 in previous research among women with pelvic pain.26 Usual injection procedures, as described above, were followed. As an additional quality assessment, nurse practitioners completed forms rating their level of certainty of point identification following each injection visit.
Consistent sourcing, quality, and storage of vitamin K1 were ensured by UCSF Pharmacy Services. Study participants were blinded, and syringes were covered with tape to mask color variation between vitamin K1 and saline. Anatomic points of injection differed, although both SP6 and the non-acupuncture control point are located on the medial side of the leg and injections were into the soleus. To minimize reporting bias, a research assistant who was not present during the injections obtained participants’ level of dysmenorrhea pain intensity before and after the intervention.
Outcome Measures
The primary measure of efficacy in this study was intensity of menstrual pain using a 0–10 unit numeric rating scale (NRS) from baseline to 60 minutes after injection. For both treatment visits, the NRS was obtained immediately before injection of vitamin K1 or saline. Participants stayed in the clinic and NRS was recorded at 5,15, 30 and 60 minutes after the injection treatment.
Data were also collected to assess presence and severity of recurrences of menstrual pain based on two measures. The Cox Retrospective Symptom Scale includes 17 symptoms commonly associated with menstrual distress. For each symptom, both intensity and duration is measured with a range of zero (not perceivable) to four (extremely upsetting). The Moos Menstrual Distress Questionnaire (MMDQ) assesses the presence of six symptoms (muscle stiffness, headache, cramps, backache, fatigue, and general aches and pains), each measured with ranges from zero (not present) to four (severe). During each cycle, study participants were also asked to report activity restrictions (absences from school, work, or other normal daily activities and hours in bed), use of analgesic and rescue medications (type, quantity, frequency, side effects), and any information on adverse events. These data were collected as part of follow-up surveys conducted one week following injection and one menstrual cycle after injection (within seven days of menstrual onset). Surveys were completed on the web using SurveyMonkey. Each follow-up survey took approximately ten minutes to complete. Surveys also included questions about participants’ use of analgesic medications, activity restrictions, and menstrual symptoms.
Descriptive measures
Data on medical history, including age at menarche, days of menstrual cycle, days with pain, when pain usually occurs during cycle, bleeding disorders, abnormal vaginal bleeding, use of herbs, supplements and medications, self-care measures for dysmenorrhea, past experience with acupuncture, pregnancy history, past and present sexual activity, use of birth control methods, standard medical and family history, were collected at the baseline visit, prior to treatment.
To assess treatment expectation, participants were asked how confident they were that the treatment would reduce pain at baseline. At follow-up, participants were asked which order they thought they received the injections (vitamin K first or saline first). To examine acceptability of treatment, we asked participants about their overall experience with the treatment/study; whether they would recommend the treatment to a friend with dysmenorrhea; and if there was anything they would change about the study.
Sample size and statistical analysis
Based on other studies of women in this age group,27 we anticipated an attrition rate of 20% among recruited participants. We aimed to recruit 20 women for the study for a final sample size of 16. Data were entered after each interview and imported into Stata.28 Means were calculated for continuous variables such as hours in bed, number of medications, and number of days absent from school/work. Difference in means, standard deviation, and 95% confidence intervals over the five study cycles were calculated. T-tests were used to analyze significance of change in means. For the categorical outcome measurements, proportion of each category was calculated and assessed by exact statistical methods for small samples. The primary outcome of interest, change in self-reported pain on the NRS from baseline to 60 minutes after injection, was analyzed using analysis of variance (ANOVA). Assessments were conducted to test for differences between groups at baseline, and differences within person at treatment time points for possible carryover effects.
Results
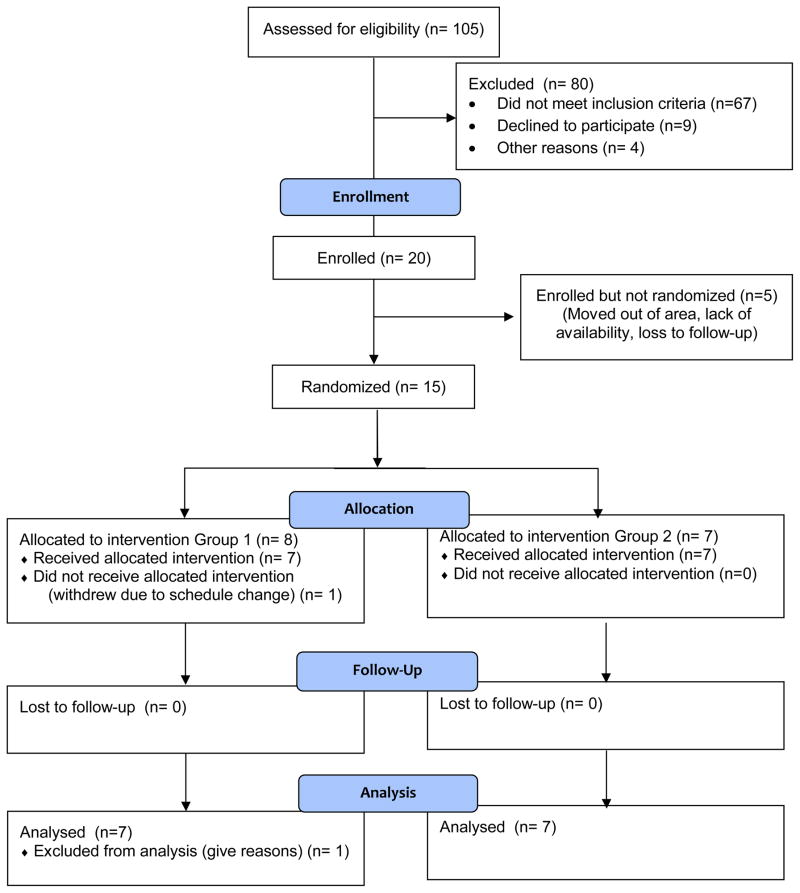
A total of 20 women were enrolled in the study (Fig. 1); 15 were randomized and 14 completed all study visits. Of the six women who were enrolled but did not complete study visits, three moved out of the San Francisco Bay Area, one started a graduate program that limited her availability, and two did not return emails or telephone calls after repeated attempts. Primary reasons reported for agreeing to participate in the study were curiosity (100%) and a desire to contribute to scientific research (71%).
Figure 1.
Consort Flowchart of Participants
Study participants were, on average, 22 years of age (range: 19 to 25); 50% white, 14% Asian, 27% Latina, and 29% other race (Table 1). Four participants (29%) had received acupuncture in the past for health reasons other than dysmenorrhea, such as stress relief, migraines, and general health. Among study participants, average age at menarche was 12.5 years (range: 11 to 15) and average cycle length was 28.0 days (Table 2). On a scale of zero to ten, average level of worst pain from menstrual cramps was 7.5 at baseline.
Table 1.
Demographics of study participants
| Sociodemographic Factors | % (n) |
|---|---|
|
| |
| Race | |
| White | 50 (7) |
| Asian | 14 (2) |
| Other | 29 (4) |
| More than one race | 7 (1) |
|
| |
| Ethnicity | |
| Latina | 27 (3) |
| Non-Latina | 72 (8) |
|
| |
| Highest Level of Education | |
| College | 92 (12) |
| Graduate School | 8 (1) |
|
| |
| Employment Status | |
| Employed | 15 (2) |
| Unemployed | 8 (1) |
| Full time student | 46 (6) |
| Working student | 31 (4) |
|
| |
| Primary language spoken at home | |
| Spanish | 7 (1) |
| English | 64 (9) |
| Other | 7 (1) |
| More than one | 21 (3) |
Table 2.
Baseline Characteristics of Participants’ Menstrual Cycles & Symptoms
| Mean (se) | |
|---|---|
| Current age (years) | 21.9 (0.50) |
| Age at menarche (years) | 12.5 (0.39) |
| Cycle length (days) | 28.0 (0.79) |
| Months until regular cycle established | 11.0 (2.95) |
| Hours of worst cramps (with no medicine) | 12.2 (2.23) |
| Hours of worst cramps (with medicine) | 6.5 (1.79) |
| Missed school or work in past month (days) | 1.4 (0.23) |
| Worst pain from menstrual cramps (0–10) | 7.6 (0.31) |
Effects of vitamin K1 vs. saline injection
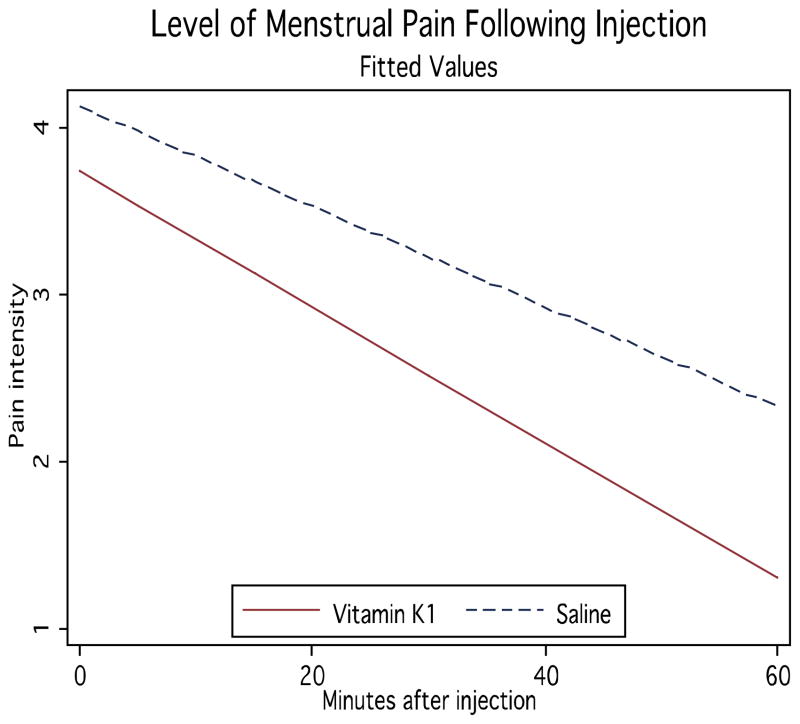
No differences in pain severity were found between the two randomized groups at baseline. The primary outcome measure was change in pain intensity on the NRS before injections to 60 minutes after injections. For acupuncture point injection of vitamin K1 in SP6, women had an average 2.5 point decrease in pain (from 4.1 to 1.6, p < 0.001, Fig. 2). When receiving saline in the non-acupoint, average pain decreased by 1.8 points (from 4.5 to 2.6, p < 0.001). Changes in NRS with vitamin K1 compared with saline approached statistical significance (p < 0.10).
Figure 2.
Change in Pain Intensity Following Injection
Effects on intensity and duration of menstrual symptoms
Participants experienced significant decreases in intensity and duration of menstrual symptoms after both acupuncture point injection of vitamin K1 and after saline injection as measured by the Cox Retrospective Symptom Scale (Table 3). Differences in change scores between vitamin K1 and saline were not significant on these measures. A significant decrease on the Moos Menstrual Distress Questionnaire was observed at one-month follow-up after acupuncture point injection of vitamin K1, but not after saline injection. No notable differences were observed in activity limitations or use of drugs or herbs throughout the five cycles of the study (data not shown).
Table 3.
Menstrual symptoms at five timepoints
| Vitamin K1 | Saline | ||||
|---|---|---|---|---|---|
| Baseline | During cycle with Injection | One month after injection | During cycle with Injection | One month after injection | |
| Pain NRS | 7.54 | 7.23 | 6.69* | 7.85 | 6.85 |
| Moos Menstrual Distress | 1.90 | 1.67 | 1.54* | 1.86 | 1.76 |
| Intensity of menstrual symptoms (Cox Scale) | 1.25 | 0.97* | 0.85* | 0.93* | 0.84* |
| Duration of menstrual symptoms (Cox Scale) | 1.59 | 1.34* | 1.28* | 1.25* | 1.17* |
Statistically significant difference compared to baseline, p < 0.05
Safety, feasibility, and acceptance
Four women experienced minor side effects that resolved prior to the end of the study visits (mild itching, pain during injection, or minor bleeding). Follow-up surveys included questions to assess feasibility and acceptability of study procedures. After participating in the study, 94% of those treated would seek injection therapy again; and 77% would come every month if the treatment were available. Randomization procedures were satisfactory to all participants in the study. The largest challenge of study implementation was scheduling injection visits to coincide with the start of participants’ menstrual cycles and availability of the nurse practitioner. All participants found study procedures satisfactory.
Assessment of Participant Blinding
As part of the exit interview, participants were asked which order they thought they received the injections in. Combined, 43% (n=6) were correct about the order of injections, with no differences between the two groups. These data suggest that blinding procedures were effective.
Discussion
This study contributes to the sparse literature on vitamin K and dysmenorrhea. Previous research examined use of vitamin K3 or K4 for dysmenorrhea;16,18,29,30 this pilot is the first experimental study conducted in the US of acupuncture point injection using vitamin K1 for dysmenorrhea. Study findings suggest high acceptability of this treatment for primary dysmenorrhea among US women aged 18–25 years old. Study implementation demonstrated feasibility in the US where acupuncture innovation is not commonplace.
Acupuncture point injection of vitamin K1 may provide an effective alternative treament for women whose pain is not alleviated by standard treaments. Pain research has suggested that a two-point reduction on the 11-point NRS is a clinically important difference.31 Thus, our study finding that women had an average decrease of 2.5 points in pain suggests clinically meaningful changes in pain intensity after acupuncture point injection of vitamin K1. We observed greater decreases in pain intensity after acupuncture point injection of vitamin K compared with saline injections. This within-group data suggest the potential therapeutic benefits of vitamin K1/SP6, though change score differences between the two treatments only approached statistical significance. These study findings are consistent with the literature indicating that the therapeutic effects of acupuncture for chronic pain conditions tend to be modestly larger than the effects of sham controls.32 Larger sample sizes than were included in this pilot study are necessary to determine whether the effects of acupuncture point injection of vitamin K1 are statistically significant and clinically meaningful compared with the effects of saline injection for alleviating the symptoms of dysmenorrhea.
Acupuncture point injection of vitamin K1 may be a welcome alternative treatment for women who have had unsatisfactory treatment outcomes with NSAIDS or OCs and for those women who prefer not to take medications or undergo a radical surgical intervention. Women who participated in the study were overall satisfied with the injection treatment and reported that they were interested in coming back for the injection if their painful menstrual cramps returned. Although further safety and efficacy studies are needed, the risks of this procedure in the clinical setting appear minimal. Vitamin K1 is readily available in US hospitals as it is routinely administered to newborn infants. Key challenges to implementing this type of treatment include scheduling logistics and provider training. Given the unpredictability of many women’s menstrual cycles, scheduling of appointments can be challenging. Women would need to be able to access services in the first two days of menses. Since the visit for the injection would be brief and can be done by ancillary staff, the acupuncture point injection could be offered on a drop-in basis. In the training we conducted for the nurse practitioners involved with the study, both the procedure and the location of the SP6 acupuncture point were taught in less than 30 minutes. Licensed healthcare providers whose scope of practice includes administering injections can easily be trained in the procedure. Some providers may, however, have difficulty accessing those trained in acupuncture point injection since it is only part of the scope of practice for TCM providers in seven states in the US.
The potential biological mechanism of acupuncture point injection of vitamin K1 on dysmenorrhea is unknown. NSAIDs alleviate the pain of menstrual cramps through their effect on prostaglandin levels. While acupuncture at SP6 does not change prostaglandin levels,33 to our knowledge, the association between vitamin K1 and prostaglandin levels has not been examined. Vitamin K is typically studied in the context of blood clotting and bone health, though recent research suggests that vitamin K may play a role in reproductive health.34 Though beyond the scope of the current study, the pharmacokinetics of vitamin K and possible effects of prostaglandin inhibition warrant additional research.
Study Limitations
Aspects of the study design and implementation limit the generalizability of study findings. Due to resource constraints, we opted for a study design that allowed for an assessment of acupuncture point injection of vitamin K as a whole treatment. With a two-arm trial, the therapeutic effects resulting from vitamin K1 vs. stimulation of the acupuncture point SP6 cannot be isolated. In addition, the current study used a washout period of two months between treatments. If acupuncture point injection of vitamin K1 has affects that endure beyond a two-month period, as has been suggested by previous research,16 differences between vitamin K1 and saline injection may have been underestimated in this study.
Recruitment and scheduling challenges resulted in a sample of 14 randomized participants who completed the study visits. This small sample size affects estimates of treatment effects and the generalizability of study findings. Studies in China suggest that acupuncture point injection of vitamin K is most effective among women suffering from severe symptoms of dysmenorrhea.16 Due to scheduling challenges, study participants were not always able to come in for injection visits at the height of their pain. While study findings suggest beneficial effect of acupuncture point injection on moderate menstrual pain, effect sizes may have been larger if women were able to receive the treatment when they were most in pain. In addition, being acupuncture naïve was not an inclusion criterion for our study and 29% of our study participants had previously experienced acupuncture. Expectancy about the effectiveness of acupuncture can affect treatment outcomes.35 Although prior acupuncture experience may have led to an overestimation of treatment effects in our study, effective blinding procedures addressed this bias to a certain degree. Lastly, licensed acupuncturists are trained to obtain a de qi sensation as part of needling and de qi may be an important aspect of the therapeutic effects of acupuncture for dysmenorrhea.36 In this study, procedures were performed by skilled nurse practitioners trained in acupuncture point injection but not in necessarily obtaining de qi while needling.
Conclusions
This study, demonstrating the feasibility and acceptability of administering the treatment in the US, along with single-arm studies conducted in China and Italy which suggest that the treatment provides rapid pain relief, is part of a research portfolio of a network of international collaborators working on an evidence-based approach to Chinese medicine and women’s health.16,24,37 The planned next step is a randomized pragmatic trial conducted in China, the US, and Italy, which would compare acupuncture point injection of vitamin K with NSAIDs, a standard-of-care treatment well-tested against placebo. Such a trial would require a coordinated international effort and a large sample size to evaluate comparative effectiveness.
Acknowledgments
Support for the study was provided by the Mount Zion Health Fund. Additional study resources were provided by the UCSF Clinical Research Center (UL1 RR024131) and the Vitamin K Laboratory at the Jean Mayer USDA Human Nutrition Research Center on Aging at Tufts University. We thank Stephanie Goodman, MPH for assistance with study administration. The first author received support from the National Center for Complementary and Alternative Medicine (NCCAM) at the National Institutes of Health (NIH) (T32AT003997 and K01AT006545). Manuscript contents are solely the responsibility of the authors and do not necessarily represent the official views of NIH or NCCAM.
Footnotes
Institution(s) in which the work was performed: University of California, San Francisco
Contributor Information
Maria T. Chao, Email: chaom@ocim.ucsf.edu, University of California, San Francisco, Osher Center for Integrative Medicine, Division of General Internal Medicine – San Francisco General Hospital, UCSF Box # 1726, San Francisco, CA 94143-1726.
Christine M. Wade, Email: wade@columbia.edu, Institute for East West Medicine, 102 E 30th Street, New York, NY 10016.
Priscilla D. Abercrombie, Email: Priscilla.Abercrombie@ucsfmedctr.org, University of California, San Francisco, Department of Obstetrics, Gynecology & Reproductive Sciences; Community Health Systems, School of Nursing; UCSF Pelvic Pain Clinic; Osher Center for Integrative Medicine; SFGH Women’s Health Center.
Denise Gomolak, Email: Denise.Gomolak@ucsfmedctr.org, Lakeshore Family Medicine, Box 1950, 1569 Sloat Blvd 333, University of California, San Francisco, San Francisco, CA. 94143 - 1950.
References
- 1.Harlow SD, Park M. A longitudinal study of risk factors for the occurrence, duration and severity of menstrual cramps in a cohort of college women. Br J Obstet Gynaecol. 1996;103(11):1134–1142. doi: 10.1111/j.1471-0528.1996.tb09597.x. [DOI] [PubMed] [Google Scholar]
- 2.Klein JR, Litt IF. Epidemiology of adolescent dysmenorrhea. Pediatrics. 1981;68(5):661–664. [PubMed] [Google Scholar]
- 3.Johnson J. Level of knowledge among adolescent girls regarding effective treatment for dysmenorrhea. J Adolesc Health Care. 1988;9(5):398–402. doi: 10.1016/0197-0070(88)90036-8. [DOI] [PubMed] [Google Scholar]
- 4.Dawood MY. Dysmenorrhea. Clin Obstet Gynecol. 1990;33(1):168–178. doi: 10.1097/00003081-199003000-00023. [DOI] [PubMed] [Google Scholar]
- 5.Latthe PM, Champaneria R, Khan KS. Dysmenorrhoea. Clin Evid. 2011 [PMC free article] [PubMed] [Google Scholar]
- 6.Dawood MY. Primary dysmenorrhea: advances in pathogenesis and management. Obstet Gynecol. 2006;108(2):428–441. doi: 10.1097/01.AOG.0000230214.26638.0c. [DOI] [PubMed] [Google Scholar]
- 7.Dawood MY. Ibuprofen and dysmenorrhea. Am J Med. 1984;77(1A):87–94. doi: 10.1016/s0002-9343(84)80025-x. [DOI] [PubMed] [Google Scholar]
- 8.Marjoribanks J, Proctor M, Farquhar C, Derks RS. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane DB Syst Rev. 2010;(1):CD001751. doi: 10.1002/14651858.CD001751.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Wong CL, Farquhar C, Roberts H, Proctor M. Oral contraceptive pill as treatment for primary dysmenorrhoea. Cochrane DB Syst Rev. 2009;(2):CD002120. doi: 10.1002/14651858.CD002120.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Lete I, Perez-Campos E, Correa M, et al. Continuation rate of combined hormonal contraception: a prospective multicenter study. J Womens Health. 2012;21(5):490–495. doi: 10.1089/jwh.2011.2967. [DOI] [PubMed] [Google Scholar]
- 11.Chen CH. Acupuncture: A Comprehensive Text, Shanghai College of Traditional Medicine. Shanghai: Eastland Press; 1981. [Google Scholar]
- 12.Strudwick MW, Hinks RC, Choy ST. Point injection as an alternative acupuncture technique--an exploratory study of responses in healthy subjects. Acupunct Med. 2007;25(4):166–174. doi: 10.1136/aim.25.4.166. [DOI] [PubMed] [Google Scholar]
- 13.Kwon YB, Kang MS, Kim HW, et al. Antinociceptive effects of bee venom acupuncture (apipuncture) in rodent animal models: a comparative study of acupoint versus non-acupoint stimulation. Acupunct Electrother Res. 2001;26(1–2):59–68. doi: 10.3727/036012901816356054. [DOI] [PubMed] [Google Scholar]
- 14.Lee MS, Pittler MH, Shin BC, Kong JC, Ernst E. Bee venom acupuncture for musculoskeletal pain: a review. J Pain. 2008;9(4):289–297. doi: 10.1016/j.jpain.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 15.Park JM, Park SU, Jung WS, Moon SK. Carthami-Semen acupuncture point injection for chronic daily headache: a pilot, randomised, double-blind, controlled trial. Complement Ther Med. 2011;19 (Suppl 1):S19–25. doi: 10.1016/j.ctim.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 16.Wang L, Cardini F, Zhao W, et al. Vitamin K acupuncture point injection for severe primary dysmenorrhea: an international pilot study. Med Gen Med. 2004;6(4):45. [PMC free article] [PubMed] [Google Scholar]
- 17.Yu J. Efficacy of vitamin K3 in the treatment of functional dysmenorrhoea: Clinical and laboratory observations. New Med Clin Trial. 1985:4. [Google Scholar]
- 18.Yu J. A clinical trial of acupoint injection of vitamin K3 in the treatment of pelvic pain. Chinese Acupuncture. 2000;7:393–394. [Google Scholar]
- 19.Zhao WJ, Weng JE, Yu J. Clinical study of Vitamin K3 acupoint injection in treating pelvic pain. Chinese Acupuncture & Moxibustion. 2000;20:393–394. [Google Scholar]
- 20.Zhao L, Li P. A survey of acupuncture treatment for primary dysmenorrhea. J Tradit Chin Med. 2009;29(1):71–76. doi: 10.1016/s0254-6272(09)60035-2. [DOI] [PubMed] [Google Scholar]
- 21.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;(12):1–23. [PubMed] [Google Scholar]
- 22.Food and Nutrition Board IoM. Vitamin K. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington, D.C: National Academy Press; 2001. [PubMed] [Google Scholar]
- 23.American Academy of Pediatrics Vitamin K Ad Hoc Task Force. Controversies concerning vitamin K and the newborn. Pediatrics. 1993;91(5):1001–1003. [PubMed] [Google Scholar]
- 24.Lesi G, Gramenzi A, Gammi L, Cardini F. Vitamin K injection in San Yin Jiao acupoint (SP6) to treat severe primary dysmenorrhoea: results of a pilot study. Eur J Integr Med. 2012;4:S51. [Google Scholar]
- 25.Cheng XN. Chinese Acupuncture and Moxibustion. 3. Beijing: Foreign Languages Press; 1987. [Google Scholar]
- 26.Schnyer RN, Iuliano D, Kay J, Shields M, Wayne P. Development of protocols for randomized sham-controlled trials of complex treatment interventions: Japanese acupuncture for endometriosis-related pelvic pain. J Altern Complement Med. 2008;14(5):515–522. doi: 10.1089/acm.2007.0826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elder JP, Shuler L, Moe SG, et al. Recruiting a diverse group of middle school girls into the trial of activity for adolescent girls. J Sch Health. 2008;78(10):523–531. doi: 10.1111/j.1746-1561.2008.00339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stata statistical software: Release 10.0. College Station, TX: StataCorp; 2007. [computer program] [Google Scholar]
- 29.Yu J. Clinical and experimental study of functional dysmenorrhea treated with Vit K3. New Drugs & Clinical Medicine. 1985;(5):14–15. [Google Scholar]
- 30.Zhao WJ, Wang L, Weng JE, Yu J. Clinical study of Vitamin K3 acupoint injection in treating pelvic pain. Chin J Integr Med. 2003;9(2):136–138. [Google Scholar]
- 31.Farrar JT, Young JP, Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 32.Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for Chronic Pain: Individual Patient Data Meta-analysis. Arch Intern Med. 2012:1–10. doi: 10.1001/archinternmed.2012.3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shi GX, Liu CZ, Zhu J, Guan LP, Wang DJ, Wu MM. Effects of acupuncture at Sanyinjiao (SP6) on prostaglandin levels in primary dysmenorrhea patients. Clin J Pain. 2011;27(3):258–261. doi: 10.1097/AJP.0b013e3181fb27ae. [DOI] [PubMed] [Google Scholar]
- 34.Truong JT, Booth SL. Emerging issues in vitamin K research. J Evid Based Complement Altern Med. 2011;16(1):73–79. [Google Scholar]
- 35.Colagiuri B, Smith CA. A systematic review of the effect of expectancy on treatment responses to acupuncture. Evid Based Complement Alternat Med. 2012;2012:857804. doi: 10.1155/2012/857804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xiong J, Liu F, Zhang M-M, Wang W, Huang G-Y. De-qi, not psychological factors, determines the therapeutic efficacy of acupuncture treatment for primary dysmenorrhea. Chin J Integr Med. 2012;18(1):7–15. doi: 10.1007/s11655-011-0857-1. [DOI] [PubMed] [Google Scholar]
- 37.Wade C, Cardini F, Wang L, Kronenberg F. Acu-injection of vitamin K for primary dysmenorrhoea: a randomised trial of active treatments. Eur J Integr Med. 2012;4:S53. [Google Scholar]