Abstract
Nausea and vomiting are two of the most troubling side effects patients experience during chemotherapy. While newly available treatments have improved our ability to manage nausea and vomiting, anticipatory and delayed nausea and vomiting are still a major problem for patients receiving chemotherapy. Many cancer patients will delay or refuse future chemotherapy treatments and contemplate stopping chemotherapy altogether because of their fear of experiencing further nausea and vomiting. The purpose of this article is to provide an overview of the patho-psychophysiology of chemotherapy-induced nausea and vomiting and the recommended guidelines for treatment.
Keywords: Cancer, chemotherapy, nausea, vomiting
Cancer treatments are quite challenging for cancer patients to endure. The cancer treatments and subsequent side effects patients experience often make them feel worse than the disease itself.1–3 Chemotherapy-induced nausea and vomiting (CINV) are two of the most common and troublesome side effects experienced by cancer patients. 1–3 Cancer patients will delay chemotherapy treatments and contemplate refusing future treatments because of fear of further CINV.1–4 While significant advances have been made in the treatment of acute chemotherapy-induced vomiting (CIV), chemotherapy-induced nausea (CIN), anticipatory nausea and vomiting (ANV) and delayed nausea and vomiting (DNV) remain substantial problems for cancer patients.1, 2 Anticipatory nausea is reported by 30% of patients who experienced nausea during earlier chemotherapy treatment cycles.1 Anticipatory vomiting is reported in 20% who experienced vomiting during earlier chemotherapy treatment cycles.5, 6 Anticipatory, acute and delayed CINV lead to poorer chemotherapy adherence, impaired function, increased anxiety and depression, and diminished quality of life (QOL) among patients. 4, 7–9 In turn, physicians and patients increase utilization of healthcare resources to manage these side effects, substantially increasing the public health burden of cancer and its effective treatment.4, 7–9,2–6The purpose of this chapter is to provide an overview of the patho-psychophysiology of CINV and the recommended guidelines for treatment of CINV.
Pathophysiology of Chemotherapy-Induced Nausea and Vomiting: The Role of Neurotransmitters
CINV are distinct symptoms; however, they often go hand-in-hand and are one of the most unpleasant side effects of most chemotherapy regimens for cancer patients. It is important to note that nausea can occur without vomiting. CINV can be acute (during the first 24 hours post-treatment) and delayed (after the first 24 hours post-treatment and up to 5–8 days post-treatment). 10 CINV, once experienced during early chemotherapy cycles, can create a conditioned response that leads to anticipatory nausea in future cycles of treatment.11 Many of the clinical symptoms commonly reported by patients in association with nausea are manifestations of autonomic nervous system activity in response to chemotherapy delivery. For example, physical manifestations such as pallor, sweating, and feeling hot or cold all over commonly precede or accompany nausea.7, 12 Vomiting is a reflex triggered by toxic substances, such as chemotherapeutic agents, causing cell damage within the stomach and small intestines. Broadly, these agents are sensed in the gastric or small bowl mucosa and cause stimulation of vagal afferents that interact with the hindbrain of the central nervous system (CNS), resulting in efferent vagal action that ultimately leads to an emetic response.
Numerous classic neurotransmitters affect the emetic response including serotonin, substance P, dopamine, acetylcholine, and γ-aminobutyric acid (GABA). Other chemical messengers, acting as neurotransmitters, that affect emetic response include histamine, endorphins, and cannabinoids.13 We know that inhibiting some of these pathways is effective in alleviating chemotherapy-related vomiting, although these same methods have not done a good job of alleviating chemotherapy-related nausea. This suggests that different pathways may play a role in the manifestation of nausea.
The most widely studied compound related to the development of CINV is serotonin, also known as 5-HT. 5-HT is produced by enterochromaffin cells, a unique cell-type dispersed throughout the enteric epithelium. These cells constitutively express 5-HT and 5-HT is expressed more abundantly upon exposure to a chemotherapeutic agent. At elevated levels, 5-HT is released from the basal surface into the lamina propria. There, secreted 5-HT binds to cognate 5-HT3 receptors located on vagus nerve terminals, thus acting as a neurotransmitter transducing a signal to the hindbrain. In turn, the translated signal triggers a motor response of NV, carried by efferenting vagal nerves.14
For approximately 30 years, 5-HT3 antagonists have been extremely useful for curbing NV in patients receiving chemotherapy.1, 15 These drugs exert their anti-emetic potential by competing with 5-HT for binding of 5-HT3 receptors, thereby blocking a pro-emetic signal to the CNS. The newest 5HT3 antagonist, palonosetron, has a higher receptor binding affinity than other commonly used 5HT3 antagonists,7 which makes it more effective at preventing NV. Palonosetron also exhibits allosteric positive cooperativity with the 5-HT3 receptor compared to other 5-HT3 antagonists (such as ondansetron and granisetron),8 and can trigger 5-HT3 internalization to prolong inhibitory effects of 5HT3 receptor function.9 Moreover, this drug has a half-life of 40 hours, which may allow more effective prevention of delayed NV than achieved with the other 5-HT3 antagonoists.16 Additionally, palonosetron may act to also influence the neurokinin-1 receptor (NK-1) pathway as there is downstream crosstalk between 5-HT3 and NK-1 receptor pathways.10
Since 5-HT synthesis is increased significantly after chemotherapy, another method of potential therapeutic benefit would decrease 5-HT synthesis in the gut. Since HT synthesis is dependent on tryptophan hydroxylase (TPH), this enzyme may represent a viable and more broadly acting target. Pre-clinical studies have been conducted using an TPH inhibitor to selectively inhibit 5-HT in the gut using a ferret model of chemotherapy-induced emesis.17
Substance P is another strong regulator of the emetic response; it binds to the NK-1 receptor. Both Substance P compound and NK-1 receptor are found within the CNS and also within the gut. Unlike 5-HT/5-HT3 receptor interaction, less is known about how and where substance P and neurokinin-1 act in promoting emetic potential, although peripheral and central components may be involved. Pre-clinical studies suggest that antagonizing neurokinin-1 receptor action in the CNS is key to preventing NV, as agents not capable of crossing the blood-brain barrier do not protect against emesis. 18 Clinically, administration of aprepitant, the first drug devised to antagonize the NK-1 receptor, has proven effective in preventing NV when combined with 5-HT3 receptor antagonists.19–21
Other pathways controlling the emetic reflex exist but far less is known about their regulation of the emetic response, especially in CINV. For example, dopamine release and cognate dopamine receptor-2 signaling may also play a role, as dopamine antagonists have been shown to be effective in treating NV. Additionally, while participation of the CNS is clearly a major contributor to the emetic process, it is also possible the enteric nervous system (ENS) itself may be able to control NV effects without CNS interplay. Understanding of the role of mediators in the pathological development of CINV will advance the development of a broader range of more effective anti-emetic treatments for CINV. Further research on the physiological mechanisms involved in the development of nausea and vomiting are needed in order to develop therapies to fully eradicate anticipatory, acute and delayed CINV.
Pathopsychology of Nausea and Emesis: The Role of Conditioning and Cognition
ANV occurs before chemotherapy infusion. ANV is believed to be a conditioned response, such that ANV will only occur after a patient has experienced nausea and/or vomiting in response to chemotherapy treatment.22 However, there are reports of ANV developing without an individual previously experiencing post-treatment nausea (e.g., in children 23). The general understanding of ANV as a conditioned response is that contextual factors, such as sights, sounds, and smells of the clinic, become conditioned stimuli paired to the unconditioned stimulus (the chemotherapy agent) that produces the unconditioned response (nausea and vomiting). Therefore, the conditioned stimuli come to elicit the conditioned response – nausea and vomiting prior to chemotherapy (ANV). There is support for ANV as a conditioned response through correlational studies 24–26, as well as through laboratory models in humans 25 and rats 27. ANV has been estimated to occur in roughly 25–30% of patients,6, 28, 29 though there is significant variability between studies.6, 24, 29 ANV negatively affects patients’ quality of life and may interfere with treatment. 6, 24
The 2010 National Comprehensive Cancer Network Guidelines recommend that ANV be prevented through optimal antiemetic therapy during every cycle of chemotherapy.22 Despite decreases in the frequency of post-treatment emesis over time, decreases in ANV were not observed in a large community study.28 Therefore, ANV continues to be a problem for patients despite advances and aggressive treatment with anti emetics. 28 Unfortunately, pharmacological interventions typically do not reduce ANV; however, cognitive-behavioral interventions, such as systematic desensitization, can be effective.30, 31 Additionally, conditioning techniques, such as overshadowing (i.e., pairing a strong flavored beverage with the beginning of infusion for a couple of cycles and then removing the stimulus at the next cycle) can help alleviate ANV.25, 32, 36
The conditioning paradigm does not fully account for the development of ANV, and cognitive factors have been identified as contributors to ANV, including anxiety and response expectations.5, 6, 26, 31, 33–37 Anxiety is believed to contribute to ANV, at least in part, through negative expectations.34, 38–40 The relationships between anxiety and negative expectations are reciprocally interactive. For example, increased anxiety produces negative expectations and negative expectations increase anxiety. Evidence suggests that patients’ expectations of experiencing nausea strongly predict the actual occurrence of ANV.35, 41 It is most likely that a combination of classical conditioning and expectancy theories more fully explain the psychopathology of ANV because conditioning effects are mediated by patient expectations and conditioning effects moderate patient expectations.42–44
Patients’ expectations of nausea are also a strong predictor of post-treatment nausea even when controlling for other known contributors.45–51 Individual variation in patient expectations may also explain why the frequency and severity of CINV are different for different patients on the same chemotherapy regimens. These between patient differences cannot be fully accounted for by the properties of the chemotherapy agents or patient demographic characteristics.30, 51, 52 Patient and treatment factors associated with CINV include: female gender, younger age, lower alcohol intake history, history of motion sickness, history of emesis during pregnancy, history of CINV, and pre-treatment expectations of nausea.53 Family conflict has been found to be related to post-treatment nausea and ANV for younger adult and female patients.54 Additional cognitive and behavioral interventions that focus on changing expectations are needed as adjuncts to standard pharmaceutical anti-emetic therapies to help fully control anticipatory, acute and delayed CINV. Roscoe and colleagues found that using a cognitive manipulation technique to increase beliefs that acupressure bands could prevent CINV resulted in significantly reduced CINV among patients with high initial expectations of experiencing CINV.50 These findings enhance our understanding of factors that contribute to CINV and the combined use of techniques like systematic desensitization, overshadowing, and expectation manipulation with pharmaceutical interventions may lead to more effective management of CINV. More research is needed investigating the psychopathology of CINV in order to effectively manage the full spectrum of anticipatory, acute and delayed CINV.
Integrative Medicine Interventions
Integrative medicine approaches, consisting of both complementary and alternative medicine interventions, are commonly used by cancer patients to reduce the toxic side effects of chemotherapy treatment. Patients typically use these types of interventions along side of their traditional allopathic (e.g., pharmaceutical) interventions. Integrative modalities are used by the majority of patients with cancer and are most commonly used by patients with advanced stage disease.55, 56 These types of treatments usually do not require a prescription from a physician, can be accessed in the community, and are gaining increasing scientific evidence to support their use.
Herbal Supplements
Ginger is the most abundantly used supplement for the prevention and/or reduction of CINV. Since the 16th century, the dried aromatic rhizome (underground stem) of ginger (Zingiber Officinale) has been used by practitioners of both Indian (Ayurvedic) and traditional Chinese medicine to treat gastrointestinal upsets such as nausea and excessive flatulence.57 Ginger has been thoroughly studied and found useful for nausea and vomiting associated with motion sickness, surgery and pregnancy.58–66 Although ginger has been approved for use to prevent motion sickness in Europe and its use is recommended,57 ginger is not a US FDA-approved medicinal treatment in the United States. However, ginger is readily available over-the-counter and in grocery stores as it is not an FDA regulated substance. The FDA currently classifies ginger as a generally regarded as safe (GRAS) substance if consumption is limited to 4 grams daily. As previously mentioned, current 5-HT antiemetic medications, such as 5-HT, are receptor antagonists for specific neurotransmitters in the gastrointestinal tract.67 Likewise, ginger can bind 5-HT3 receptors to enhance antiemetic effects and can increase detoxification enzymes to counteract oxidative damage to tissues.68 For the best results in reducing CINV, ginger should be implemented before the onset of symptoms or before the first chemotherapy treatment cycle. Our research group previously demonstrated, in a 744 patient phase III randomized, placebo-controlled clinical trial, that three different daily doses of ginger (0.5 gram, 1.0 gram, 1.5 grams) plus standard 5-HT3 receptor antagonists and dexemethasone significantly reduced acute CINV compared to placebo plus standard standard 5-HT3 receptor antagonists and dexamethasone.69, 70 Our findings suggest that cancer patients can achieve greater alleviation of acute CINV by using ginger supplementation of 0.5 to 1.0 gram daily (equivalent to ¼ to ½ teaspoon of ground ginger) along with standard 5-HT3 receptor antagonists and dexamethasone.69, 70 It is important to note that the ginger used in this study consisted of capsules containing a purified liquid extract equivalent to 250 milligrams of ginger. The purified liquid extract concentrated the biologically active components of the ginger root, such as gingerols, zingerones, and shogaols.58 Unclear forms of ginger, such as crystallized, raw, tea, or aromatherapy, are thought to have similar effectiveness.
Many other herbal supplements, in the form of tea or aromatherapy, have been recommended for the relief of CINV. Cinnamon bark, peppermint, chamomile, fennel, and rosewood are among the most common.71 Similar to ginger, these herbs have anti-spasmodic activity and promote digestive health. Studies have shown that citrus bioflavonoids can actually cause nausea and vomiting.71 Chinese medicinal herbs have demonstrated effectiveness against CINV.55 Chinese medicinal herbs are highly variable compounds and include any liquid extract of a mixture of herbal compounds used to treat symptoms or diseases. Chinese medicinal herbs are prepared by Chinese medicine practioners to reduce therapeutic toxicity and/or strengthen the body’s resistance and immunity.55 Usually, Chinese herbalists determine the combination of herbs on an individual basis depending on patient symptoms and conditions. Therefore a Chinese herbalist, as well as oncologist should be consulted before use of Chinese medicinal herbs. Three published studies favored use of Chinese medicinal herbs for the relief of CINV. Shenqi fuzheng injections (consisting of two herbs),72 Aidi injections (consisting of four herbs),73 and Aifukang (consisting of 11 herbs)74 reduced CINV in a sample of breast cancer patients.55
Acupuncture & Acupressure
Acupuncture is another form of traditional Chinese medicine that has been used for centuries to treat nausea and vomiting. Over the past 20 years, clinical evidence supports acupuncture for CINV.75 Acupuncture is a 4000-year-old therapeutic technique that involves inserting and manipulating needles with and without electrical stimulation and providing pressure or electrical stimulation at specific points in the body.75 Research suggests that acupuncture works primarily on the nervous system through stimulating brain activation or deactivation as documented by neuroimaging techniques.76 Needle insertion points are chosen based on specific anatomical sites associated with specific bodily functions.76 The acupuncture points most commonly used for control of nausea and vomiting are the P6 and ST36.75 The P6 is located between tendons in the wrist approximately two inches proximal to the crease of the wrist. The ST36 is on the anterior lateral side of the leg. Traditional acupuncture involves manual manipulation of needles, whereas electro-accupuncture involves applying a small electric current to the needles. Acupressure incorporates accu-point stimulation through the use of wrist-worn devices consisting of an elastic band and embedded stud, such as Seabands®.77 Electro-stimulation involves accu-point stimulation by an intermittent electrical current similar to units used for pain relief through the use of wrist-worn devices, such as Relief-bands®.77 Electro-stimulation units that confer a constant electro-stimulation are not recommended for control of CINV.77 Although the overall effect of accupuncture strongly suggests effectiveness against acute and delayed CINV, the data is not conclusive. For example, in 2005, Ezzo published a meta-analysis concluding that acupuncture combined with standard antiemetics significantly reduced acute CINV.78 However, in 2007, both Gardani79 and Dibble80 showed no effect of acupressure on acute CINV. Overall, acupuncture is considered to be a cost-effective, minimal risk, integrative therapy that can be used in conjunction with standard anti-emetic pharmaceuticals for the management of CINV.
Biopsychobehavioral
Biopsychobehavioral interventions such as progressive muscle relaxation, guided imagery, hypnosis, and exercise are also efficacious therapies for the treatment of anticipantory, acute and delayed CINV. Biopsychobehavioral interventions are especially appropriate and most beneficial if implemented in a preventive manner and started before the first chemotherapy treatment cycle and, most importantly, before the first onset of symptoms of CINV.81, 82
Progressive muscle relaxation (PMR) involves the tension and relaxation of muscle groups in sequence to relax physically and mentally.82 PMR alone reduces the severity of nausea associated with chemotherapy.83 PMR combined with a 20-minute massage during chemotherapy infusions reduces the severity of nausea.84 Guided imagery, a technique used to focus patients’ attention on a particular image and associated sensory experiences, reduces the incidence of vomiting in the 24 hours after chemotherapy.85 Patients who use guided imagery combined with an antiemetic regimen versus an antiemetic alone have a more positive chemotherapy experience.86 PMR is often combined with guided imagery to treat CINV with consistent, positive outcomes. PMR combined with guided imagery reduces the incidence of nausea87, 88 and vomiting 85, 87, 88 in the first four days after chemotherapy and the severity of nausea 84, 88–92 and vomiting88, 90 up to 5 days following chemotherapy. Cognitive distraction and systematic desensitization have been used to successfully reduce the severity of ANV93, 94 and CINV.89, 94 Overshadowing is also a technique that has been used to help alleviate ANV.25, 32, 36 Teaching self-hypnosis, which typically involves using the imagination to suggest feeling good and feeling safe, reduces the incidence of ANV93, 95 and the severity of CINV96 in children undergoing chemotherapy. Hypnosis has also been used successfully with adults to reduce ANV.97 Several researchers have used exercise interventions to aid in reducing CINV. Aerobic exercise has been shown to help reduce the severity of CINV98 and yoga has been shown to be beneficial in reducing for reducing CINV.99
Anti-emetics
Advances in 5HT3 antagonists and NK-1 antagonists have dramatically improved control of CINV. Palonosetron (Aloxi) and aprepitant (Emend) are the newest antiemetics.
Palonsetron is a second generation antagonist of 5-hydroxytyptamine receptors (5HT3). Its main advantages compared to the other 5HT3 receptors include: its significantly longer half-life (approximately 40h, 10× longer than first generation 5HT3 antagonists), its higher binding affinity, its high selectivity to the 5HT3 receptors (with little effect on other receptors), and its excellent safety profile (at even up to three times its FDA approved dose).100 A single dose (0.25 mg IV) of palonosetron can effectively prevent acute CINV resulting from moderately to highly emetogenic chemotherapy.4, 8, 9 Recent studies comparing palonosetron to ondansetron and granisetron suggest the superiority of palonsetron on all days, but particularly between 24–120 hours after chemotherapy. Complete response rates ranged from 48% and 57% using 0.75 mg of palonosetron and only 39% to 45% when not using it.101–103 Additionally, Saito and colleagues conducted a prospective randomized head-to-head trial between Palosetron and Granisetron for both acute and chronic CINV in 1019 patients. This study showed non-inferiority of Palonosetron compared to a first generation 5HT3 antagonist in the acute phase of CINV (0–24 hours) and superiority of Palonosetron in delayed CINV (24hrs to 120h).102 As such, current research supports the use of the second generation 5HT3 receptor antagonist in control of acute and delayed CINV, over the first generation 5HT3 receptor antagonists (e.g., ondansetron, granisetron, dolasetron) for moderately emetogenic chemotherapy agents.102
Aprepitant and fosapretitant are potent, selective NK-1 receptor competitive antagonists of Substance P, believed to be an essential component in triggering the emetic reflex.104 They can penetrate the CNS where there is a concentration of NK-1 receptors. Aprepitant is a 3 day regimen, with a recommended dosing of 125 mg orally 1 hour prior to chemotherapy treatment (Day 1) and 80 mg orally once daily in the morning on Days 2 and 3. Fosaprepitent is a pro-drug of aprepitant for injection (115 mg over 15 min) and can be substituted for aprepitant 30 minutes prior to chemotherapy on Day 1 only. In 2003, Hesketh et al.104 published a randomized, double blind, parallel-group, placebo-controlled trial of 530 patients receiving Cisplatin (a highly emetogenic agent). The Aprepitant group response was superior to standard therapy group in acute and delayed phases,as well as overall.104 Subsequently, a prospective, randomized, double blind, parallel study of 866 patients receiving moderately emetogenic chemotherapy over multiple cycles demonstrated the efficacy of Aprepitant in prevention of nausea and emesis over all 4 cycles of treatment.105 This randomized, placebo-controlled trial also evaluated daily Aprepitant with Dexamethasone for 3 days versus a single daily dose of Palonosetron with Dexamethasone for acute and delayed CINV. The study demonstrated no statistical significance between groups, suggesting that one dose of aprepitant with standard anti-emetic regimen has similar effectiveness to a 3 day aprepitant regimen for CINV105. The use of Aprepitant may also provide an advantage in that patients only have to take one dose of dexamethasone on day 1 with moderately emetic chemotherapy regimens.106 Fosaprepitant may offer an option for patients who cannot tolerate oral administration of antiemetics, particularly during an episode of severe nausea or vomiting.107
Guidelines
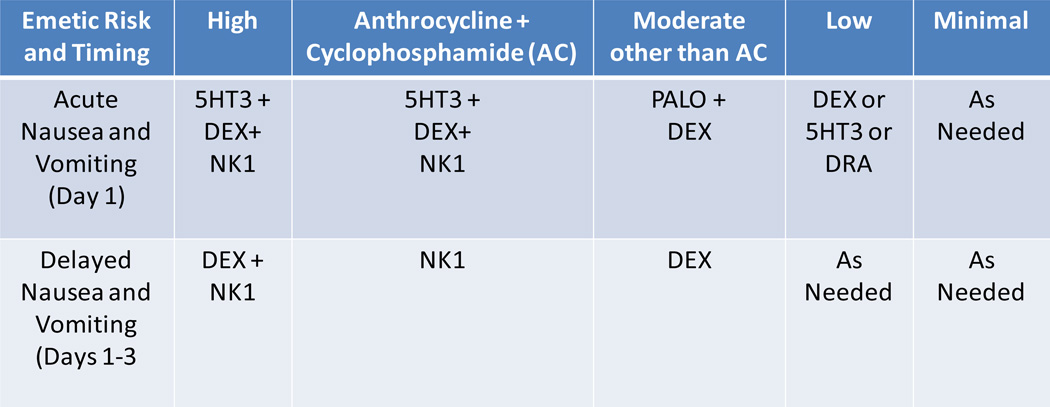
Clinical practice guidelines for CINV have been developed using evidence-based research by expert panels including the American Society of Clinical Oncology (ASCO), the National Comprehensive Cancer Network (NCCN), and the Multinational Association of Supportive Care in Cancer (MASCC).108–114 Research shows that adherence to these guidelines can improve complete control of CINV by almost 20%.115 Guidelines for antiemetic usage are based on the potential of experiencing CINV for specific chemotherapy regimens and classify regimens into four categories: highly-emetic (>90%), moderately-emetic (both with and without anthracycline and cyclophosphamide [AC]; 30–90%), low-emetic (10–30%), and minimally-emetic (<10%). The guidelines for antiemetic use are broken down further into categories based on the patient’s expectations (anticipatory), time of onset (acute and delayed), and resistance to antiemetic treatment (breakthrough and refractory; see Figure 1). As mentioned previously in this article, anticipatory CINV is an expected or conditioned response that usually occurs just prior to the actual administration of chemotherapy treatment.12, 116, 117 Acute CINV usually occurs within the first few hours of chemotherapy administration, peaking between 5–6 hours, and resolving within 24 hours.118 Delayed CINV occurs more than 24 hours after chemotherapy administration and can last up to 7 days. Delayed CINV is common in chemotherapy regimens that involve cisplatin, carboplatin, cyclophosphamide, and/or doxorubicin.119 Patients receiving multi-day chemotherapy regimens are at risk for both acute and delayed CINV depending on the chemotherapeutic agents and the sequence of administration. Breakthrough CINV occurs when prophylactic antiemetic treatment fails and “rescue” antiemetics are required, while refractory CINV occurs when previous antiemetic regimens have failed in prior chemotherapy treatment cycles. These comprehensive clinical practice guidelines are a valuable tool for oncologists in the prevention and treatment of CINV a summary of the recommended treatments are provided in Figure 1.
Figure 1.
Pharmacological Treatment Guidelines for Acute and Delayed Chemotherapy-Induced Nausea and Vomiting
5HT3: serotonin receptor antagonist; DEX: dexamethosone; NK1: neurokinin-1 receptor antagonist; PALO: palononsetron; DRA: dopamine receptor antagonist
Summary
Despite advances in pharmaceutical and behavioral therapies, and the provision of standard clinical guidelines for effectively managing CINV, patients continue to experience CINV. Although introduction of 5-HT3 and NK-1 antagonists has considerably reduced the incidence of CINV it remains a prevalent side effect among cancer patients. If oncologists follow the ASCO, NCCN or MASCC guidelines for the treatment of CINV, research suggests that control of CINV can be improved by approximately 20%.115 Evidence also suggests that the addition of integrative therapies including herbal supplements, accupuncture, progressive muscle relaxation, guided imagery, hypnosis, and exercise can improve control of anticipatory, acute and delayed CINV above and beyond what is achieved by the use of pharmaceuticals alone. These integrative behavioral interventions need to be included in standard clinical practice guidelines. CINV as a fearsome side effect is more manageable now than years past with the advent of powerful, long-acting agents. Unfortunately, adequate control of nausea remains a challenge and requires increased research focus.
Acknowledgments
Support: The publication of the article was funded by Eisai Inc. The views and opinions expressed are those of the authors and not necessarily those of Eisai Inc.
Footnotes
Disclosure: The authors have no conflicts of interest to declare.
References
- 1.Hickok JT, Roscoe JA, Morrow GR, et al. 5-Hydroxytryptamine-receptor antagonists versus prochlorperazine for control of delayed nausea caused by doxorubicin: a URCC CCOP randomised controlled trial. Lancet Oncol. 2005;6:765–772. doi: 10.1016/S1470-2045(05)70325-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hickok JT, Morrow GW, Roscoe JA, et al. Prevalence and severity of acute and delayed NV association with 3 highly emetogenic chemotherapies. [abstract] Supportive Care in Cancer. 2001;9:289. [Google Scholar]
- 3.Hofman M, Morrow GR, Roscoe JA, et al. Cancer patients' expectations of experiencing treatment-related side effects. Cancer. 2004;101:851–857. doi: 10.1002/cncr.20423. [DOI] [PubMed] [Google Scholar]
- 4.Figueroa-Moseley C, Morrow GR. Major Advances and Alternative Approaches to Antiemetic Therapy. Oncology. 2008;21 [Google Scholar]
- 5.Aapro MS, Molassiotis A, Olver I. Anticipatory nausea and vomiting. Support Care Cancer. 2005;13:117–121. doi: 10.1007/s00520-004-0745-8. [DOI] [PubMed] [Google Scholar]
- 6.Morrow GR, Roscoe JA, Kirshner JJ, et al. Anticipatory nausea and vomiting in the era of 5-HT3 antiemetics. Support Care Cancer. 1998;6:244–247. doi: 10.1007/s005200050161. [DOI] [PubMed] [Google Scholar]
- 7.Hesketh PJ. Chemotherapy-induced nausea and vomiting. N Engl J Med. 2008;358:2482–2494. doi: 10.1056/NEJMra0706547. [DOI] [PubMed] [Google Scholar]
- 8.Schwartzberg LS. Chemotherapy-induced nausea and vomiting: Which antiemetic for which therapy? ONCOLOGY. 2007;21:946–953. [PubMed] [Google Scholar]
- 9.Grote T, Hajdenberg J, Cartmell A, et al. Combination therapy for chemotherapy-induced nausea and vomiting in patients receiving moderately emetogenic chemotherapy: palonosetron, dexamethasone, and aprepitant. J Support Oncol. 2006;4:403–408. [PubMed] [Google Scholar]
- 10.Roscoe JA, Morrow GR, Hickok JT, et al. Biobehavioral factors in chemotherapy-induced nausea and vomiting. J Natl Compr Canc Netw. 2004;2:501–508. doi: 10.6004/jnccn.2004.0039. [DOI] [PubMed] [Google Scholar]
- 11.Roscoe JA, Morrow GR, Aapro MS, et al. Anticipatory nausea and vomiting. Support Care Cancer. doi: 10.1007/s00520-010-0980-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morrow GR. Clinical characteristics associated with the development of anticipatory nausea and vomiting in cancer patients undergoing chemotherapy treatment. J Clin Oncol. 1984;2:1170–1176. doi: 10.1200/JCO.1984.2.10.1170. [DOI] [PubMed] [Google Scholar]
- 13.Navari RM. Pharmacological management of chemotherapy-induced nausea and vomiting: focus on recent developments. Drugs. 2009;69:515–533. doi: 10.2165/00003495-200969050-00002. [DOI] [PubMed] [Google Scholar]
- 14.Gershon MD. Review article: serotonin receptors and transporters -- roles in normal and abnormal gastrointestinal motility. Aliment Pharmacol Ther. 2004;20(Suppl 7):3–14. doi: 10.1111/j.1365-2036.2004.02180.x. [DOI] [PubMed] [Google Scholar]
- 15.Hickok JT, Roscoe JA, Morrow GR, et al. Use of 5-HT3 receptor antagonists to prevent nausea and emesis caused by chemotherapy for patients with breast carcinoma in community practice settings. Cancer. 1999;86:64–71. doi: 10.1002/(sici)1097-0142(19990701)86:1<64::aid-cncr11>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 16.Tonini G, Vincenzi B, Santini D. New drugs for chemotherapy-induced nausea and vomiting: focus on palonosetron. Expert Opin Drug Metab Toxicol. 2005;1:143–149. doi: 10.1517/17425255.1.1.143. [DOI] [PubMed] [Google Scholar]
- 17.Liu Q, Yang Q, Sun W, et al. Discovery and characterization of novel tryptophan hydroxylase inhibitors that selectively inhibit serotonin synthesis in the gastrointestinal tract. J Pharmacol Exp Ther. 2008;325:47–55. doi: 10.1124/jpet.107.132670. [DOI] [PubMed] [Google Scholar]
- 18.Tattersall FD, Rycroft W, Francis B, et al. Tachykinin NK1 receptor antagonists act centrally to inhibit emesis induced by the chemotherapeutic agent cisplatin in ferrets. Neuropharmacology. 1996;35:1121–1129. doi: 10.1016/s0028-3908(96)00020-2. [DOI] [PubMed] [Google Scholar]
- 19.de Wit R, Herrstedt J, Rapoport B, et al. Addition of the oral NK1 antagonist aprepitant to standard antiemetics provides protection against nausea and vomiting during multiple cycles of cisplatin-based chemotherapy. J Clin Oncol. 2003;21:4105–4111. doi: 10.1200/JCO.2003.10.128. [DOI] [PubMed] [Google Scholar]
- 20.Warr DG, Grunberg SM, Gralla RJ, et al. The oral NK(1) antagonist aprepitant for the prevention of acute and delayed chemotherapy-induced nausea and vomiting: Pooled data from 2 randomised, double-blind, placebo controlled trials. Eur J Cancer. 2005;41:1278–1285. doi: 10.1016/j.ejca.2005.01.024. [DOI] [PubMed] [Google Scholar]
- 21.Warr DG, Hesketh PJ, Gralla RJ, et al. Efficacy and tolerability of aprepitant for the prevention of chemotherapy-induced nausea and vomiting in patients with breast cancer after moderately emetogenic chemotherapy. J Clin Oncol. 2005;23:2822–2830. doi: 10.1200/JCO.2005.09.050. [DOI] [PubMed] [Google Scholar]
- 22.Network NCC. NCCN Practice Guidelines in Oncology: Antiemesis - v.2.2010. 2010 http://www.nccn.org/professionals/physician_gls/f_guidelines.asp. Published Last Modified Date|. Accessed Dated Accessed|.
- 23.Tyc VL, Mulhern RK, Barclay DR, et al. Variables associated with anticipatory nausea and vomiting in pediatric cancer patients receiving ondansetron antiemetic therapy. J Pediatr Psychol. 1997;22:45–58. doi: 10.1093/jpepsy/22.1.45. [DOI] [PubMed] [Google Scholar]
- 24.Akechi T, Okuyama T, Endo C, et al. Anticipatory nausea among ambulatory cancer patients undergoing chemotherapy: Prevalence, associated factors, and impact on quality of life. Cancer Sci. 2010 doi: 10.1111/j.1349-7006.2010.01718.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stockhorst U, Enck P, Klosterhalfen S. Role of classical conditioning in learning gastrointestinal symptoms. World J Gastroenterol. 2007;13:3430–3437. doi: 10.3748/wjg.v13.i25.3430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bovbjerg DH. The continuing problem of post chemotherapy nausea and vomiting: contributions of classical conditioning. Auton Neurosci. 2006;129:92–98. doi: 10.1016/j.autneu.2006.07.016. [DOI] [PubMed] [Google Scholar]
- 27.Limebeer CL, Krohn JP, Cross-Mellor S, et al. Exposure to a context previously associated with nausea elicits conditioned gaping in rats: a model of anticipatory nausea. Behav Brain Res. 2008;187:33–40. doi: 10.1016/j.bbr.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 28.Roscoe JA, Morrow GR, Hickok JT, et al. Nausea and vomiting remain a significant clinical problem: trends over time in controlling chemotherapy-induced nausea and vomiting in 1413 patients treated in community clinical practices. J Pain Symptom Manage. 2000;20:113–121. doi: 10.1016/s0885-3924(00)00159-7. [DOI] [PubMed] [Google Scholar]
- 29.Morrow GR, Dobkin PL. Anticipatory nausea and vomiting in cancer patients undergoing chemotherapy treatment: Prevalence, etiology, and behavioral interventions. Clinical Psychology Review. 1988;8:517–556. [Google Scholar]
- 30.Morrow GR, Roscoe JA, Hynes HE, et al. Progress in reducing anticipatory nausea and vomiting: a study of community practice. Support Care Cancer. 1998;6:46–50. doi: 10.1007/s005200050131. [DOI] [PubMed] [Google Scholar]
- 31.Roscoe JA, Morrow GR, Aapro MS, et al. Anticipatory nausea and vomiting. Support Care Cancer. 2010 doi: 10.1007/s00520-010-0980-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stockhorst U, Wiener JA, Klosterhalfen S, et al. Effects of overshadowing on conditioned nausea in cancer patients: an experimental study. Physiol Behav. 1998;64:743–753. doi: 10.1016/s0031-9384(98)00135-8. [DOI] [PubMed] [Google Scholar]
- 33.Zachariae R, Paulsen K, Mehlsen M, et al. Anticipatory nausea: the role of individual differences related to sensory perception and autonomic reactivity. Ann Behav Med. 2007;33:69–79. doi: 10.1207/s15324796abm3301_8. [DOI] [PubMed] [Google Scholar]
- 34.Andrykowski MA. The role of anxiety in the development of anticipatory nausea in cancer chemotherapy: a review and synthesis. Psychosom Med. 1990;52:458–475. doi: 10.1097/00006842-199007000-00008. [DOI] [PubMed] [Google Scholar]
- 35.Montgomery GH, Tomoyasu N, Bovbjerg DH, et al. Patients' pretreatment expectations of chemotherapy-related nausea are an independent predictor of anticipatory nausea. Ann Behav Med. 1998;20:104–109. doi: 10.1007/BF02884456. [DOI] [PubMed] [Google Scholar]
- 36.Hickok JT, Roscoe JA, Morrow GR. The role of patients' expectations in the development of anticipatory nausea related to chemotherapy for cancer. J Pain Symptom Manage. 2001;22:843–850. doi: 10.1016/s0885-3924(01)00317-7. [DOI] [PubMed] [Google Scholar]
- 37.Kim Y, Morrow GR. The effects of family support, anxiety, and post-treatment nausea on the development of anticipatory nausea: a latent growth model. J Pain Symptom Manage. 2007;34:265–276. doi: 10.1016/j.jpainsymman.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 38.Jacobsen P, Die-Trill M, Holland J, et al. Nonpharmacologic factors in the development of posttreatment nausea with adjuvant chemotherapy for breast cancer. Cancer. 1988;61:379–385. doi: 10.1002/1097-0142(19880115)61:2<379::aid-cncr2820610230>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 39.Andrykowski MA, Redd WH, Hatfield AK. Development of anticipatory nausea: a prospective analysis. J Consult Clin Psychol. 1985;53:447–454. doi: 10.1037//0022-006x.53.4.447. [DOI] [PubMed] [Google Scholar]
- 40.Watson M, McCarron J, Law M. Anticipatory nausea and emesis, and psychological morbidity: assessment of prevalence among out-patients on mild to moderate chemotherapy regimens. Br J Cancer. 1992;66:862–866. doi: 10.1038/bjc.1992.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Montgomery GH, Bovbjerg DH. Specific response expectancies predict anticipatory nausea during chemotherapy for breast cancer. J Consult Clin Psychol. 2001;69:831–835. doi: 10.1037//0022-006x.69.5.831. [DOI] [PubMed] [Google Scholar]
- 42.Kirsch I. Specifying nonspecifics: Psychological mechanisms of placebo effects. The placebo effect: An interdisciplinary exploration. 1997:166–186. [Google Scholar]
- 43.Stewart-Williams S, Podd J. The placebo effect: dissolving the expectancy versus conditioning debate. Psychological Bulletin. 2004;130:324–340. doi: 10.1037/0033-2909.130.2.324. [DOI] [PubMed] [Google Scholar]
- 44.Kirsch I, Lynn S, Vigorito M, et al. The role of cognition in classical and operant conditioning. Journal of Clinical Psychology. 2004;60:369–392. doi: 10.1002/jclp.10251. [DOI] [PubMed] [Google Scholar]
- 45.Roscoe JA, Bushunow P, Morrow GR, et al. Patient expectation is a strong predictor of severe nausea after chemotherapy: a University of Rochester Community Clinical Oncology Program study of patients with breast carcinoma. Cancer. 2004;101:2701–2708. doi: 10.1002/cncr.20718. [DOI] [PubMed] [Google Scholar]
- 46.Roscoe JA, Hickok JT, Morrow GR. Patient expectations as predictor of chemotherapy-induced nausea. Ann Behav Med. 2000;22:121–126. doi: 10.1007/BF02895775. [DOI] [PubMed] [Google Scholar]
- 47.Colagiuri B, Roscoe JA, Morrow GR, et al. How do patient expectancies, quality of life, and postchemotherapy nausea interrelate? Cancer. 2008;113:654–661. doi: 10.1002/cncr.23594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Colagiuri B, Zachariae R. Patient expectancy and post-chemotherapy nausea: a meta-analysis. Ann Behav Med. 2010;40:3–14. doi: 10.1007/s12160-010-9186-4. [DOI] [PubMed] [Google Scholar]
- 49.Olver I, Taylor A, Whitford H. Relationships between patients' pre-treatment expectations of toxicities and post chemotherapy experiences. Psycho-Oncology. 2005;14:25–33. doi: 10.1002/pon.804. [DOI] [PubMed] [Google Scholar]
- 50.Roscoe J, O'Neill M, Jean-Pierre P, et al. An Exploratory Study on the Effects of an Expectancy Manipulation on Chemotherapy-Related Nausea. Journal of Pain and Symptom Management. 2010 doi: 10.1016/j.jpainsymman.2009.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Roscoe JA, Morrow GR, Colagiuri B, et al. Insight in the prediction of chemotherapy-induced nausea. Support Care Cancer. 2010;18:869–876. doi: 10.1007/s00520-009-0723-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hickok J, Roscoe J, Morrow G, et al. Nausea and emesis remain significant problems of chemotherapy despite prophylaxis with 5-hydroxytryptamine-3 antiemetics: a University of Rochester James P. Wilmot Cancer Center Community Clinical Oncology Program Study of 360 cancer patients treated in the community. Cancer. 2003;97:2880–2886. doi: 10.1002/cncr.11408. [DOI] [PubMed] [Google Scholar]
- 53.Nevidjon B, Chaudhary R. Controlling emesis: evolving challenges, novel strategies. The journal of supportive oncology. 8:1. [PubMed] [Google Scholar]
- 54.Kim Y, Morrow G. Changes in family relationships affect the development of chemotherapyrelated nausea symptoms. Supportive Care in Cancer. 2003;11:171–177. doi: 10.1007/s00520-002-0416-6. [DOI] [PubMed] [Google Scholar]
- 55.Zhang M, Liu X, Li J, et al. Chinese medicinal herbs to treat the side-effects of chemotherapy in breast cancer patients. Cochrane Database Syst Rev. 2007:CD004921. doi: 10.1002/14651858.CD004921.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yates JS, Mustian KM, Morrow GR, et al. Prevalence of complementary and alternative medicine use in cancer patients during treatment. Supportive Care in Cancer. 2005;13:806–811. doi: 10.1007/s00520-004-0770-7. [DOI] [PubMed] [Google Scholar]
- 57.Shukla Y, Singh M. Cancer preventive properties of ginger: a brief review. Food Chem Toxicol. 2007;45:683–690. doi: 10.1016/j.fct.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 58.Natural Health Bible: From the most trusted source in health information, here is your A–Z guide to over 200 herbs, vitamins, and supplements. Roseville, CA: Prima Publishing; 1999. [Google Scholar]
- 59.Arfeen Z, Owen H, Plummer JL, et al. A double-blind randomized controlled trial of ginger for the prevention of postoperative nausea and vomiting. Anaesth Intensive Care. 1995;23:449–452. doi: 10.1177/0310057X9502300406. [DOI] [PubMed] [Google Scholar]
- 60.Bone ME, Wilkinson DJ, Young JR, et al. Ginger root--a new antiemetic. The effect of ginger root on postoperative nausea and vomiting after major gynaecological surgery. Anaesthesia. 1990;45:669–671. doi: 10.1111/j.1365-2044.1990.tb14395.x. [DOI] [PubMed] [Google Scholar]
- 61.Fischer-Rasmussen W, Kjaer SK, Dahl C, et al. Ginger treatment of hyperemesis gravidarum. Eur J Obstet Gynecol Reprod Biol. 1991;38:19–24. doi: 10.1016/0028-2243(91)90202-v. [DOI] [PubMed] [Google Scholar]
- 62.Grontved A, Brask T, Kambskard J, et al. Ginger root against seasickness. A controlled trial on the open sea. Acta Otolaryngol. 1988;105:45–49. doi: 10.3109/00016488809119444. [DOI] [PubMed] [Google Scholar]
- 63.Morrow GR, Dobkin PL. Anticipatory nausea and vomiting in cancer patients undergoing chemotherapy treatment: Prevalence, etiology, and behavioral interventions. Clinical Psychology Reviews. 1988;8:517–556. [Google Scholar]
- 64.Mowrey DB, Clayson DE. Motion sickness, ginger, and psychophysics. Lancet. 1982;1:655–657. doi: 10.1016/s0140-6736(82)92205-x. [DOI] [PubMed] [Google Scholar]
- 65.Phillips S, Ruggier R, Hutchinson SE. Zingiber officinale (ginger)--an antiemetic for day case surgery. Anaesthesia. 1993;48:715–717. doi: 10.1111/j.1365-2044.1993.tb07188.x. [DOI] [PubMed] [Google Scholar]
- 66.Visalyaputra S, Petchpaisit N, Somcharoen K, et al. The efficacy of ginger root in the prevention of postoperative nausea and vomiting after outpatient gynaecological laparoscopy. Anaesthesia. 1998;53:506–510. doi: 10.1046/j.1365-2044.1998.00369.x. [DOI] [PubMed] [Google Scholar]
- 67.Herrstedt J, Dombernowsky P. Anti-emetic therapy in cancer chemotherapy: current status. Basic Clin Pharmacol Toxicol. 2007;101:143–150. doi: 10.1111/j.1742-7843.2007.00122.x. [DOI] [PubMed] [Google Scholar]
- 68.Geiger JL. The essential oil of ginger, Zingiber officinale, and anaesthesia. The International Journal of Aromatherapy. 2005;15:7–14. [Google Scholar]
- 69.Ryan JL, Heckler C, Dakhil SR, et al. Ginger for chemotherapy-related nausea in cancer patients: A URCC CCOP randomized, double-blind, placebo-controlled clinical trial of 644 cancer patients. Journal of Clinical Oncology. 2009;27 suppl abstr 9511. [Google Scholar]
- 70.Ryan JL, Heckler CE, Roscoe JA, et al. Ginger (Zingiber officinale) reduces acute chemotherapyinduced nausea: A URCC CCOP study of 744 patients. Journal of Clinical Oncology. 2010 doi: 10.1007/s00520-011-1236-3. In review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Publishing ES. Essential Oils Desk Reference. 4th ed. Orem, UT: Essential Science Publishing; 2007. [Google Scholar]
- 72.Li XL, Tian QY, Ma WJ. Clinical study on Shenqi Fuzheng injections combined with chemotherapy for advanced breast cancer patients. Chinese Practical Medicine Journal. 2002;2:2263–2264. [Google Scholar]
- 73.Yang L. Clinical study on Aidi injections combined with chemotherapy for advanced cancer patients. Chinese Journal of Integrated Traditional and Western Medicine. 2004;24:755–756. [Google Scholar]
- 74.Situ HL, Lin Y, Chen QJ, et al. Effects of Aifukang on quality of life of breast cancer patient treated with chemotherapy after operation. Journal of Guangzhou University of Tradiational Chinese Medicine. 2005;22:26–29. [Google Scholar]
- 75.Ma L. Acupuncture as a complementary therapy in chemotherapy-induced nausea and vomiting. Proc (Bayl Univ Med Cent) 2009;22:138–141. doi: 10.1080/08998280.2009.11928494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wu MT, Hsieh JC, Xiong J, et al. Central nervous pathway for acupuncture stimulation: localization of processing with functional MR imaging of the brain--preliminary experience. Radiology. 1999;212:133–141. doi: 10.1148/radiology.212.1.r99jl04133. [DOI] [PubMed] [Google Scholar]
- 77.Cassileth BR, Deng GE, Gomez JE, et al. Complementary therapies and integrative oncology in lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition) Chest. 2007;132:340S–354S. doi: 10.1378/chest.07-1389. [DOI] [PubMed] [Google Scholar]
- 78.Ezzo J, Vivkers A, Richardson MA, et al. Acupuncture-Point Stimulation for Chemotherapy- Induced Nausea and Vomiting. Journal of Clinical Oncology. 2005 Oct 1;23:7188–7198. doi: 10.1200/JCO.2005.06.028. [DOI] [PubMed] [Google Scholar]
- 79.Gardani G, Cerrone R, Biella C, et al. A progress study of 100 cancer patients treated by acupressure for chemotherapy-induced vomiting after failure with the pharmacological approach. Minerva Med. 2007;98:665–668. [PubMed] [Google Scholar]
- 80.Dibble SL, Luce J, Cooper BA, et al. Acupressure for chemotherapy-induced nausea and vomiting: a randomized clinical trial. Oncol Nurs Forum. 2007;34:813–820. doi: 10.1188/07.ONF.xxx-xxx. [DOI] [PubMed] [Google Scholar]
- 81.Redd WH. Behavioral intervention for cancer treatment side effects. Acta Oncol. 1994;33:113–117. doi: 10.3109/02841869409098393. [DOI] [PubMed] [Google Scholar]
- 82.Morrow GR, Hickok JT. Behavioral treatment of chemotherapy-induced nausea and vomiting. Oncology (Williston Park) 1993;7:83–89. discussion 93–84, 97. [PubMed] [Google Scholar]
- 83.Cotanch PH, Strom S. Progressive muscle relaxation as antiemetic therapy for cancer patients. Oncology nursing forum. 1987;14:33–37. [PubMed] [Google Scholar]
- 84.Billhult A, Bergbom I, Stener-Victorin E. Massage relieves nausea in women with breast cancer who are undergoing chemotherapy. J Altern Complement Med. 2007;13:53–57. doi: 10.1089/acm.2006.6049. [DOI] [PubMed] [Google Scholar]
- 85.Burish TG, Snyder SL, Jenkins RA. Preparing patients for cancer chemotherapy: effect of coping preparation and relaxation interventions. J Consult Clin Psychol. 1991;59:518–525. doi: 10.1037//0022-006x.59.4.518. [DOI] [PubMed] [Google Scholar]
- 86.Troesch LM, Rodehaver CB, Delaney EA, et al. The influence of guided imagery on chemotherapy-related nausea and vomiting. Oncol Nurs Forum. 1993;20:1179–1185. [PubMed] [Google Scholar]
- 87.Molassiotis A, Yung HP, Yam BM, et al. The effectiveness of progressive muscle relaxation training in managing chemotherapy-induced nausea and vomiting in Chinese breast cancer patients: a randomised controlled trial. Support Care Cancer. 2002;10:237–246. doi: 10.1007/s00520-001-0329-9. [DOI] [PubMed] [Google Scholar]
- 88.Molassiotis A. A pilot study of the use of progressive muscle relaxation training in the management of post-chemotherapy nausea and vomiting. Eur J Cancer Care (Engl) 2000;9:230–234. doi: 10.1046/j.1365-2354.2000.00220.x. [DOI] [PubMed] [Google Scholar]
- 89.Vasterling J, Jenkins RA, Tope DM, et al. Cognitive distraction and relaxation training for the control of side effects due to cancer chemotherapy. J Behav Med. 1993;16:65–80. doi: 10.1007/BF00844755. [DOI] [PubMed] [Google Scholar]
- 90.Lyles JN, Burish TG, Krozely MG, et al. Efficacy of relaxation training and guided imagery in reducing the aversiveness of cancer chemotherapy. J Consult Clin Psychol. 1982;50:509–524. doi: 10.1037//0022-006x.50.4.509. [DOI] [PubMed] [Google Scholar]
- 91.Burish TG, Carey MP, Krozely MG, et al. Conditioned side effects induced by cancer chemotherapy: prevention through behavioral treatment. J Consult Clin Psychol. 1987;55:42–48. doi: 10.1037//0022-006x.55.1.42. [DOI] [PubMed] [Google Scholar]
- 92.Burish TG, Jenkins RA. Effectiveness of biofeedback and relaxation training in reducing the side effects of cancer chemotherapy. Health Psychol. 1992;11:17–23. doi: 10.1037//0278-6133.11.1.17. [DOI] [PubMed] [Google Scholar]
- 93.Zeltzer LK, Dolgin MJ, LeBaron S, et al. A randomized, controlled study of behavioral intervention for chemotherapy distress in children with cancer. Pediatrics. 1991;88:34–42. [PubMed] [Google Scholar]
- 94.Morrow GR, Asbury R, Hammon S, et al. Comparing the effectiveness of behavioral treatment for chemotherapy-induced nausea and vomiting when administered by oncologists, oncology nurses, and clinical psychologists. Health Psychol. 1992;11:250–256. doi: 10.1037//0278-6133.11.4.250. [DOI] [PubMed] [Google Scholar]
- 95.Jacknow DS, Tschann JM, Link MP, et al. Hypnosis in the prevention of chemotherapy-related nausea and vomiting in children: a prospective study. J Dev Behav Pediatr. 1994;15:258–264. [PubMed] [Google Scholar]
- 96.Cotanch P, Hockenberry M, Herman Self-hypnosis as antiemetic therapy in children receiving chemotherapy. Oncol Nurs Forum. 1985;12:41–46. [PubMed] [Google Scholar]
- 97.Marchioro G, Azzarello G, Viviani F, et al. Hypnosis in the treatment of anticipatory nausea and vomiting in patients receiving cancer chemotherapy. Oncology. 2000;59:100–104. doi: 10.1159/000012144. [DOI] [PubMed] [Google Scholar]
- 98.Winningham ML, MacVicar MG. The effect of aerobic exercise on patient reports of nausea. Oncol Nurs Forum. 1988;15:447–450. [PubMed] [Google Scholar]
- 99.Raghavendra RM, Nagarathna R, Nagendra HR, et al. Effects of an integrated yoga programme on chemotherapy-induced nausea and emesis in breast cancer patients. European journal of cancer care. 2007;16:462–474. doi: 10.1111/j.1365-2354.2006.00739.x. [DOI] [PubMed] [Google Scholar]
- 100.Navari RM. Palonosetron for the prevention of chemotherapy-induced nausea and vomiting in patients with cancer. Future Oncology. 2010;6:1073–1084. doi: 10.2217/fon.10.74. [DOI] [PubMed] [Google Scholar]
- 101.Aapro M, Grunberg S, Manikhas G, et al. A phase III, double-blind, randomized trial of palonosetron compared with ondansetron in preventing chemotherapy-induced nausea and vomiting following highly emetogenic chemotherapy. Annals of oncology. 2006;17:1441. doi: 10.1093/annonc/mdl137. [DOI] [PubMed] [Google Scholar]
- 102.Saito M, Aogi K, Sekine I, et al. Palonosetron plus dexamethasone versus granisetron plus dexamethasone for prevention of nausea and vomiting during chemotherapy: a double-blind, double-dummy, randomised, comparative phase III trial. The Lancet Oncology. 2009;10:115–124. doi: 10.1016/S1470-2045(08)70313-9. [DOI] [PubMed] [Google Scholar]
- 103.Yu Z, Liu W, Wang L, et al. The efficacy and safety of palonosetron compared with granisetron in preventing highly emetogenic chemotherapy-induced vomiting in the Chinese cancer patients: a phase II, multicenter, randomized, double-blind, parallel, comparative clinical trial. Supportive Care in Cancer. 2009;17:99–102. doi: 10.1007/s00520-008-0503-4. [DOI] [PubMed] [Google Scholar]
- 104.Hesketh PJ, Grunberg SM, Gralla RJ, et al. The oral neurokinin-1 antagonist aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a multinational, randomized, double-blind, placebo-controlled trial in patients receiving high-dose cisplatin—the Aprepitant Protocol 052 Study Group. Journal of Clinical Oncology. 2003;21:4112. doi: 10.1200/JCO.2003.01.095. [DOI] [PubMed] [Google Scholar]
- 105.Herrstedt J, Muss HB, Warr DG, et al. Efficacy and tolerability of aprepitant for the prevention of chemotherapy induced nausea and emesis over multiple cycles of moderately emetogenic chemotherapy. Cancer. 2005;104:1548–1555. doi: 10.1002/cncr.21343. [DOI] [PubMed] [Google Scholar]
- 106.Merck. EMEND (fosaprepitant dimeglumine) for injection. 2011 Apr 12; http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/022023s002s003s005lbl.pdf.
- 107.Langford P, Chrisp P. Fosaprepitant and aprepitant: an update of the evidence for their place in the prevention of chemotherapy-induced nausea and vomiting. Core Evidence. 2010;5:77. doi: 10.2147/ce.s6012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. [Accessed 04/14, 2011];NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Anitemesis. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#supportive.
- 109.Basch E, et al. American Society of Clinical Oncology guideline for antiemetics in oncology: update 2011. J Clin Oncol. doi: 10.1200/JCO.2006.06.9591. in press. [DOI] [PubMed] [Google Scholar]
- 110. [Accessed 04/14, 2011];MASCC/ESMO Antiemetic Guidelines. 2011 http://www.mascc.org/mc/page.do?sitePageId=88041. [Google Scholar]
- 111.Ettinger DS, Armstrong DK, Barbour S, et al. Antiemesis. Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2009;7:572–595. doi: 10.6004/jnccn.2009.0039. [DOI] [PubMed] [Google Scholar]
- 112.Kris MG, Tonato M, Bria E, et al. Consensus recommendations for the prevention of vomiting and nausea following high-emetic-risk chemotherapy. Support Care Cancer. 2011;19(Suppl 1):S25–S32. doi: 10.1007/s00520-010-0976-9. [DOI] [PubMed] [Google Scholar]
- 113.Olver I, Clark-Snow RA, Ballatori E, et al. Guidelines for the control of nausea and vomiting with chemotherapy of low or minimal emetic potential. Support Care Cancer. 2011;19(Suppl 1):S33–S36. doi: 10.1007/s00520-010-0985-8. [DOI] [PubMed] [Google Scholar]
- 114.Roila F, Herrstedt J, Aapro M, et al. Guideline update for MASCC and ESMO in the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting: results of the Perugia consensus conference. Ann Oncol. 2010;21(Suppl 5):v232–v243. doi: 10.1093/annonc/mdq194. [DOI] [PubMed] [Google Scholar]
- 115.O'Kane A. Evaluate The Effects Of Implementing The Multinational Association Of Supportive Care In Cancer (MASCC) Antiemetic Guideline On The Incidence Of Chemotherapy-Induced Nausea And Vomiting (CINV) Following Platinum Chemotherapy. Supportive Care in Cancer. 2009;17:875. [Google Scholar]
- 116.Jacobsen PB, Redd WH. The development and management of chemotherapy-related anticipatory nausea and vomiting. Cancer Invest. 1988;6:329–336. doi: 10.3109/07357908809080656. [DOI] [PubMed] [Google Scholar]
- 117.Moher D, Arthur AZ, Pater JL. Anticipatory nausea and/or vomiting. Cancer Treat Rev. 1984;11:257–264. doi: 10.1016/0305-7372(84)90011-2. [DOI] [PubMed] [Google Scholar]
- 118.Herrstedt J, Rapoport B, Warr D, et al. Acute emesis: moderately emetogenic chemotherapy. Support Care Cancer. 2011;19(Suppl 1):S15–S23. doi: 10.1007/s00520-010-0951-5. [DOI] [PubMed] [Google Scholar]
- 119.Roila F, Warr D, Aapro M, et al. Delayed emesis: moderately emetogenic chemotherapy (singleday chemotherapy regimens only) Support Care Cancer. 2011;19(Suppl 1):S57–S62. doi: 10.1007/s00520-010-1039-y. [DOI] [PubMed] [Google Scholar]
Reference List
- 1.Morrow GR, Roscoe JA. Anticipatory nausea and vomiting: Models, mechanisms and management. In: Dicato M, editor. Medical management of cancer treatment induced emesis. London: Martin Dunitz; 1997. pp. 149–166. [Google Scholar]
- 2.Hesketh PJ. Chemotherapy-induced nausea and vomiting. N Engl J Med. 2008;358(23):2482–2494. doi: 10.1056/NEJMra0706547. [DOI] [PubMed] [Google Scholar]
- 3.Cancer Network. Chemotherapy-Induced Nausea and Vomiting. 2008 cancernetwork.com. Ref Type: Electronic Citation.
- 4.Figueroa-Moseley C, Morrow G. Major Advances and Alternative Approaches to Antiemetic Therapy. Cancer Network. 2008 Ref Type: Electronic Citation. [Google Scholar]
- 5.Schwartzberg L. Chemotherapy-Induced Nausea and Vomiting: Which Antiemetic for Which Therapy? Cancer Network. 2008 Ref Type: Electronic Citation. [PubMed] [Google Scholar]
- 6.Grote T, Hajdenberg J, Cartmell A, Ferguson S, Ginkel A, Charu V. Combination therapy for chemotherapy-induced nausea and vomiting in patients receiving moderately emetogenic chemotherapy: palonosetron, dexamethasone, and aprepitant. J Support Oncol. 2006;4(8):403–408. [PubMed] [Google Scholar]
- 7.Wong EH, Clark R, Leung E, et al. The interaction of RS 25259-197, a potent and selective antagonist, with 5-HT3 receptors, in vitro. British Journal of Pharmacology. 1995;114(4):851–859. doi: 10.1111/j.1476-5381.1995.tb13282.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rojas C, Stathis M, Thomas AG, et al. Palonosetron exhibits unique molecular interactions with the 5-HT3 receptor.[Erratum appears in Anesth Analg. 2008 Oct;107(4):1405 Note: Massuda, Edward B [corrected to Massuda, Ed B]; Rubenstein, Ed [corrected to Rubenstein, Edward].] Anesthesia & Analgesia. 2008;107(2):469–478. doi: 10.1213/ane.0b013e318172fa74. [DOI] [PubMed] [Google Scholar]
- 9.Rojas C, Thomas AG, Alt J, et al. Palonosetron triggers 5-HT(3) receptor internalization and causes prolonged inhibition of receptor function. European Journal of Pharmacology. 2010;626(2–3):193–199. doi: 10.1016/j.ejphar.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 10.Rojas C, Li Y, Zhang J, et al. The antiemetic 5-HT3 receptor antagonist Palonosetron inhibits substance P-mediated responses in vitro and in vivo. J Pharmacol Exp Ther. 2010;335(2):362–368. doi: 10.1124/jpet.110.166181. [DOI] [PMC free article] [PubMed] [Google Scholar]