Abstract
The goal of this study was to quantify the burden of cervical cancer in Texas and provide information about the health care needs of survivors. Data from multiple sources including the Texas Cancer Registry, Behavioral Risk Factor Surveillance System, and Texas Medicare claims were used in this effort. In 2009, there were over 100,000 cervical cancer survivors in Texas. Our descriptive analysis revealed that these women consumed less fruit and vegetables, were more often smokers, and had worse physical and mental health than women without a history of cancer. Survivors aged 65 and older cost Medicare over $15 million in inpatient, outpatient, and hospice care in 2009 alone, or $9,827 per cervical cancer survivor – nearly a third more than the average Medicare enrollee in Texas that year. Providers and public health practitioners can play an integral role in reducing the human and economic burden of cervical cancer in Texas through smoking cession and healthy lifestyle counseling for survivors, recommending the HPV vaccine to males and females aged 9-26, and continuing to offer cervical cancer screening for women up to age 65.
INTRODUCTION
The emergence and widespread adoption of technology for cervical cancer prevention, screening, and treatment has made cervical cancer one of the most preventable and curable female cancers. Since 1975, cervical cancer incidence and mortality have fallen by about 50%, largely due to widespread cervical cancer screening, better treatment services for pre-cancerous lesions and invasive cancer, and improved access to publically-funded programs and clinics. The age-adjusted number of incident cases per year has fallen from 14.8 per 100,000 women in 1975 to 6.9 cases per 100,000 women in 2009; while the number of deaths per year has fallen from 5.6 per 10,000 women in 1975 to 2.3 per 10,000 women in 20091. While rates have fallen for both white and black women, the greatest declines have been experienced among blacks- though disparities still persist. The American Cancer Society estimates that in 2012 there will be 12,170 new cases and 4,220 deaths from cervical cancer in the U.S. For all stages combined, we can expect a 5-year relative survival of about 68% (69% for Whites, 59% for Blacks). When the cancer is found at a localized stage, 5-year survival increases to 91%2. Research has also shown that women who are uninsured or from less-affluent communities are at a survival disadvantage3.
Despite the very positive effects of early detection and treatment on survival, cervical cancer survivors experience a wide array of reported physical and mental health issues following treatment including sexual dysfunction4,5, gastrointestinal toxicity6, and anxiety7. Furthermore, since the population at risk for cervical cancer tends to be disadvantaged, these problems may be particularly difficult to manage due to compounding burdens (e.g., low income, language barriers, inadequate access to care). These issues cause significant health and economic burden to cervical cancer survivors and to the healthcare delivery and financing systems. The focus of this study is to estimate those human and economic burdens by examining the epidemiology of cervical cancer in Texas, focusing on survivors’ health burdens, behaviors, and utilization of healthcare services. Our goal is to provide researchers, public health practitioners, and providers with information about the magnitude of the burden of cervical cancer in TX and the health care needs of survivors.
METHODS
Data Sources
Three data sources were used: The Texas Cancer Registry's (TCR) web query tool, the Behavioral Risk Factor Surveillance System (BRFSS), and the TCR-Medicare linked claims data sets. Each data source provided a different perspective of the overall picture of cervical cancer in Texas. The TCR web query tool provided data on cervical cancer incidence and mortality; the BRFSS dataset provided data on cervical cancer survivors’ health burdens and behaviors; and the TCR-Medicare linked claims data provided resource utilization data.
Cervical cancer incidence and mortality data were obtained from the TX Cancer Registry's (TCR) web query tool8. This tool allows individuals to extract cancer incidence and mortality rates across a variety of geographies in Texas (e.g., county, health service region, metropolitan statistical area). Rates can be aggregated over time, age-adjusted, and stratified by sex and race/ethnicity, if requested. The TCR uses the direct method of age-adjustment, which weights the age-specific rates by the age distribution in a standard population – in this case, we used the 2000 U.S. population as the standard9.
The 2009 Behavioral Risk Factor Surveillance System (BRFSS) provided information on the health burdens and behaviors of cervical cancer survivors. Among the questions asked on the telephone interview to participants aged 20 years and older, selected by random-digit dialing, we selected questions related to health behaviors (e.g., leisure time physical activity, daily consumption of fruits and vegetables, cigarette smoking status) and quality of life (e.g., self-ratings of physical health, mental health, and overall health) and compared the responses between cervical cancer survivors (n=87, weighted to Texas population=102,728) with female respondents who never had any cancer (n=6,399, Texas population=7,883,296). We excluded respondents who self-reported a diagnosis of cervical cancer but were less than one year post diagnosis to ensure that participants’ reported health behaviors were reflective of survivors, rather than women currently undergoing treatment. We also excluded respondents who reported more than one type of cancer.
Data from the linked TCR-Medicare dataset were used to examine the healthcare resource utilization patterns of cervical cancer survivors. This data was previously obtained and linked through the Comparative Effectiveness Research on Cancer in Texas (CERCIT) program (http://www.txcercit.org/). We extracted the 2009 claims records from the dataset for all patients first diagnosed with cervical cancer in 1995 through 2007 (N = 1,595). We choose 2009 claims, which provided two years minimum since the date of first cancer diagnosis, to ensure that we are examining the chronic healthcare needs of cancer survivors instead of the services and costs of cancer treatment. This study was granted IRB approval from the Institutional Review Board at The University of Texas MD Anderson Cancer Center.
Data Analysis
Using the TCR web query tool, we extracted age-adjusted cervical cancer incidence and mortality rates at the Health Service Region (HSR) level. Rates were aggregated over a 5-year period (2005-2009) to ensure stability and an adequate number of cases. Health service region (HSR) level rates were obtained from the web query tool and used to produce choropleth maps to highlight geographic variation in cancer rates using ArcGIS Version 10.010. Geographic variability in race-specific incidence and mortality rates were also examined.
The BRFSS data was analyzed using SAS11 survey procedures to account for the complex sampling design. We used weighted data in all statistical analyses. The BRFSS dataset was used to evaluate the health behaviors and burdens of cervical cancer survivors, compared to women who reported no history of cancer. This analysis was stratified into two age categories, aged <65 and 65 and older, to highlight differences in behavioral patterns in these populations and to permit appropriate comparison to the utilization data. Health behaviors examined included physical activity (sedentary, insufficient, or met recommendation), diet (met recommendation for 5 fruits and vegetables per day vs. did not meet recommendation), and smoking (yes/no). Health burdens included three health-related quality of life constructs (poor health, physical health, and mental health), BMI, and a comorbidity count (0, 1-2, >2).
Engaging in vigorous physical activity for 20+ minutes 3 days per week or moderate physical activity for 30+ minutes 5 days per week was classified as meeting physical activity recommendations12. Individuals who did less than the recommended amount of physical activity, but more than 10 minutes, were categorized as insufficient. Finally, respondents who reported no moderate or vigorous physical activity were categorized as sedentary. Current smoking status was assessed by two survey questions: “Have you smoked at least 100 cigarettes in your entire life?” and “Do you now smoke cigarettes every day, some days, or not at all?” Individuals who indicated they had smoked 100+ cigarettes in their life and smoked every day or some days were classified as smokers. Former smokers and those who indicated they never smoked 100+ cigarettes were classified as non-smokers. Poor health was based on individuals’ response to whether their physical or mental health kept them from doing their usual activities. Physical health was measured as the number of days the individual indicated her physical health was not good and mental health was measured as the number of days the individual indicated his/her mental health was not good.
Using the TCR-Medicare linked claims data, healthcare utilization patterns were assessed for Medicare beneficiaries, stratified by time since first cervical cancer diagnosis (2-5 years, 6-10 years, 11-15 years). The number of patients with cervical cancer, as first reported in 1995-2007, who were still alive in 2009 was 2,341. The number of survivors with at least one Medicare claim in 2009 was 1,585. Specifically, we examined: 1) the average number of days in inpatient or hospice care, 2) the total number of outpatient visits, and 3) the average Medicare payments associated with inpatient, outpatient, and hospice care of cervical cancer survivors in 2009. Medicare payments are reported in 2009 U.S. dollars. Cervical cancer survivors who did not have a Medicare claim in 2009 were excluded.
RESULTS
Epidemiology of cervical cancer in TX
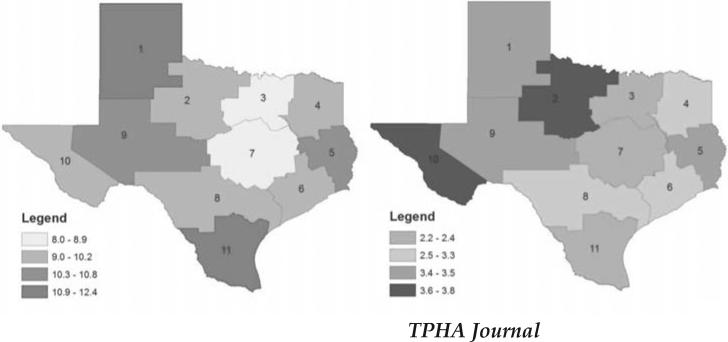
In Texas, cervical cancer incidence and mortality have declined over time, although they remain higher than the national average. From 1995 to 2009, the age-adjusted incidence rate decreased from 12.3 to 9.4 per 100,000 women and the age-adjusted mortality rate decreased from 4.0 to 2.7 per 100,000 women. Although rates have fallen for all racial/ethnic groups from 1995-2009, disparities persist for Hispanic and Black women (vs. whites). The incidence of cervical cancer varied across the state, from a low of 8.0 per 100,000 women in HSR 03 to a high of 12.4 per 100,000 women in HSR 01. Incidence was highest in HSR 04 for Hispanics and HSR 09 for Blacks. The lowest mortality was observed in HSR 07 (2.2 per 100,000) and the highest mortality in HSR 10 (3.8 per 100,000; Figure 1). Mortality was highest in HSR 02 for Hispanics and HSR 05 for Blacks.
Figure 1.
Geographic variation in age-adjusted cervical cancer incidence (left map) and mortality (right map) per 100,000 women in Texas, 2005-2009
Health behaviors and burdens of cervical cancer survivors in TX
Based on population-weighted data from the TX BRFSS, we estimate that there were 102,728 cervical cancer survivors 1+ year(s) post first cervical cancer diagnosis in 2009. About 86% of the BRFSS-reported cervical cancer survivors were <65 years of age and 74% were first diagnosed with cervical cancer >10 years ago. The majority of cervical cancer survivors were white (72% vs. 50% among women without a history of cancer) and reported having less than a high school education (77% vs.. 67% among women without a history of cancer). Because of its self-reported nature, BRFSS may include some women who mistakenly report a history of cervical cancer for a history of treatment of precancerous lesions.
Cervical cancer survivors under age 65 reported higher levels of physical activity than women without a history of any cancer (Table 1). The trend was reversed, however, for women aged 65 and older in whom cervical cancer survivors were less likely to meet the recommended level of physical activity than their counterparts (20.96% vs. 34.97%, respectively). Regardless of age, cervical cancer survivors reported less fruit and vegetable consumption than women without a history of cancer. Additionally, women with a history of cervical cancer were more than twice as likely to smoke than women without a history of cancer (44.31% vs. 14.35% for women <65; 21.75% vs. 9.63% for women ≥65).
Table 1.
Health behaviors of women with a reported history of cervical cancer vs. women without a history of cancer, stratified by age, 2009 Texas BRFSS
| Women with a history of cervical cancer | Women without a history of cancer | |||
|---|---|---|---|---|
| <65 | ≥65 | <65 | ≥65 | |
| N = 68 | N = 19 | N = 4,599 | N = 1,740 | |
| Est. N = 88,791* | Est. N = 13,937 | Est. N = 6,757,586 | Est. N = 1,125,710 | |
| Variable | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) |
| Physical activity | ||||
| Sedentary | 12.0 (0.9-23.0) | 17.7 (0-36.8) | 12.0 (10.47-13.46) | 23.6 (20.30-26.85) |
| Insufficient | 33.5 (15.7-51.4) | 61.3 (33.1-89.6) | 41.1 (38.71-43.47) | 41.5 (37.44-45.47) |
| Met recommendation | 54.5 (35.3-73.6) | 21.0 (0-43.7) | 47.0 (44.56-49.33) | 35.0 (31.39-38.55) |
| Five F&V/Day | ||||
| Did not meet recommendation | 79.9 (66.6-93.3) | 73.1 (45.5-100) | 72.3 (70.2-74.4) | 68.6 (65.2-71.9) |
| Met recommendation | 20.1 (6.7-33.4) | 26.9 (0-54.6) | 27.7 (25.7-29.8) | 31.5 (28.1-34.8) |
| Current Smoker | ||||
| Yes | 44.3 (26.6-62.0) | 21.8 (0-44.2) | 14.4 (12.8-15.9) | 9.6 (7.5-11.8) |
Est. N = estimated number of women based on weighted survey data
Women with a history of cervical cancer reported worse overall, physical, and mental health, than their counterparts, regardless of age (Table 2). This distinction is particularly notable among cervical cancer survivors under age 65, who reported about double the number of days their health kept them from doing their usual activities and double the number of days their physical/mental health was not good. The number of comorbidities among cervical cancer survivors under age 65 was also higher than their counterparts without a history of cancer. This pattern was not found in survivors aged 65 and older. Finally, we noted that although younger survivors reported higher levels of physical activity than their counterparts, more were classified as overweight or obese.
Table 2.
Health burdens of women with a reported history of cervical cancer vs. women without a history of cancer, stratified by age, 2009 Texas BRFSS
| Women with a history of cervical cancer | Women without a history of cancer | |||||||
|---|---|---|---|---|---|---|---|---|
| <65 | ≥65 | <65 | ≥65 | |||||
| N = 68 | N = 19 | N = 4,599 | N = 1,740 | |||||
| Est. N = 88,791 | Est. N = 13,937 | Est. N = 6,757,586 | Est. N = 1,125,710 | |||||
| Variable | Est. N | Mean (95%CI) | Est. N | Mean (95% CI) | Est. N | Mean (95%CI) | Est. N | Mean (95% CI) |
| Health-Related Quality of Life | ||||||||
| Poor Health | 64,132 | 9.929 (4.9-15.0) | 9,950 | 6.16 (1.73-10.58) | 4,072,570 | 4.20 (3.68-4.73) | 581,818 | 5.82 (4.89-6.75) |
| Physical Health | 78,750 | 6.3 (2.9-9.6) | 13,826 | 6.27 (2.30-10.25) | 6,625,102 | 3.42 (3.11-3.74) | 1,068,292 | 5.36 (4.70-6.03) |
| Mental Health | 83,550 | 10.1 (4.7-15.4) | 13,937 | 4.62 (0.51-8.74) | 6,682,738 | 4.45 (4.03-4.86) | 1,094,849 | 2.43 (1.93-2.93) |
| Est. N | % (95% CI) | Est. N | % (95% CI) | Est. N | % (95% CI) | Est. N | % (95% CI) | |
| Comorbidity Count | ||||||||
| 0 | 35,244 | 39.7 (22.1-57.3) | 1,658 | 11.9 (0-27.4) | 3,737,078 | 55.3 (53.1-57.5) | 101,934 | 9.1 (7.2-11.0) |
| 1 or 2 | 37,867 | 42.7 (24.6-60.7) | 7,535 | 54.1 (25.1-83.1) | 2,517,948 | 37.3 (35.1-39.4) | 602,526 | 53.5 (49.8-57.2) |
| >2 | 15,680 | 17.7 (5.3-30.0) | 4,743 | 34.04 (6.9-61.2) | 502,115 | 7.4 (6.5-8.3) | 421,250 | 37.4 (33.9-40.9) |
| Body Mass Index | ||||||||
| Normal | 25,739 | 29.9 (13.1-46.6) | 3,863 | 27.7 (4.5-51.0) | 2,301,051 | 37.7 (35.4-40.0) | 425,937 | 40.1 (36.3-43.8) |
| Overweight | 23,746 | 27.6 (12.3-42.8) | 5,297 | 38.0 (10.8-65.2) | 1,867,474 | 30.6 (28.4-32.9) | 367,014 | 34.5 (31.1-38.0) |
| Obese | 36,690 | 42.6 (22.8-62.4) | 4.777 | 34.3 (9.8-58.8) | 1,933,329 | 31.7 (29.5-33.9) | 269,529 | 25.4 (21.6-29.1) |
Utilization of healthcare services among cervical cancer survivors in TX
Cervical cancer survivors aged 65 and older in Texas spent on average 12.1 days in inpatient or hospice care and had 5.1 outpatient hospitalizations in 2009 (Table 3). One-third of cervical cancer survivors were hospitalized an average of 7.31 days at a cost of almost $11 million to Medicare in 2009. During the same time period, 79% of survivors had outpatient office visits at a cost of over $3 million to Medicare. Women who were diagnosed more recently (2-5 years) spent more days on average in inpatient care than their counterparts. These women also were more frequent hospice users. These patterns were reflected in payments made by Medicare. Specifically, women diagnosed more recently had larger Medicare payments for inpatient and hospice care. Although women diagnosed more recently also had slightly more outpatient visits on average, Medicare payments did not differ substantially.
Table 3.
Utilization of healthcare services among cervical cancer survivors aged 65+ in Texas, by years since first cervical cancer diagnosis, 2009 TCR- Medicare
| Years since diagnosis | ||||
|---|---|---|---|---|
| Variable | 2-5 years | 6-10 years | 11-15 years | All years |
| Number of patients at risk | 483 | 524 | 578 | 1585 |
| No. of patients admitted for inpatient care (avg. length of stay) | 181 (8.46) | 156 (6.66) | 192 (6.95) | 529 (7.31) |
| No. of patients in hospice (avg. length of stay) | 57 (7.51) | 28 (3.29) | ------------ | 109 (4.80) |
| No. of patients seen in outpatient care (avg. number of visits) | 385 (5.43) | 410 (4.79) | 464 (5.21) | 1259 (5.14) |
| Avg. Medicare payment for inpatient care | $8,208 | $5,687 | $6,844 | $6,877 |
| Avg. Medicare payment for outpatient care | $2,215 | $2,224 | $2,218 | $2,219 |
| Avg. Medicare payment for hospice care | $1,146 | $521 | $575 | $731 |
Footnotes:
Cells with less than 25 patients are suppressed.
Average length of stay and average Medicare payments are based on the no. of patients at risk who had at least one claim during 2009.
CONCLUSIONS & DISCUSSION
We found that the human and economic burdens of cervical cancer are substantial. Cervical cancer survivors under age 65 reported worse overall, physical, and mental health, more comorbidities, and higher BMIs than their counterparts. These findings are largely consistent with previous studies that found cancer survivors reported worse general health, higher BMIs13, more comorbidities14, and more functional limitations than their counterparts13, 14. Studies focused on gynecologic cancers suggest that mental health problems are more common among survivors than controls,7, 15 which may be related to compromised sexual function5, 16 and body-image.16 Although not assessed in this study due to small sample size, several studies have found that these health burdens and behaviors are even more prevalent in cervical cancer survivors from underserved groups,17-21 who may lack the resources to receive affordable and quality treatment and follow-up services.The excess burdens of cervical cancer survivorship lead to high costs. Medicare payments for inpatient, outpatient, and hospice care for cervical cancer survivors in Texas in 2009 ($15,576,986; $9,827 per enrollee with a history of cervical cancer) were nearly a third more than the average Medicare enrollee in Texas that year ($6,142 per enrollee adjusted for age, sex and race)22.
The excess human and economic burdens may be due in part to suboptimal health behaviors among survivors of cervical cancer. We found that women with a history of cervical cancer have different health behaviors than women without a history of cancer. Cervical cancer survivors under age 65 reported slightly higher levels of physical activity, but less fruit and vegetable consumption than their counterparts. For women aged 65 and older, cervical cancer survivors had lower levels of physical activity and less fruit and vegetable consumption. Other studies have shown that cervical cancer survivors meet the fruit and vegetable consumption recommendation of the ACS (i.e., 5-a-day) more than other types of cancer survivors (19.1% vs. 14.8-18.2%), but have the lowest adherence to physical activity recommendations (29.6% vs. 35.0-47.3%)23.
Smoking was also more prevalent among cervical cancer survivors than controls, which is consistent with several other studies of health behavior among cancer survivors.24-27 Studies have even shown the prevalence of smoking among cervical cancer survivors to exceed most other cancer types; specifically, 5 times as high as that among lymphoma and prostate cancer survivors, and 2.5-3 times as high as that among survivors of all cancer types combined.24, 28
Implications for Public Health Practice
Public health professionals and primary care providers have important roles to play in reducing the human and economic costs of cervical cancer. First, and most importantly, because cervical cancer is one of the most preventable and most easily detectable cancers, they can help to reduce the incidence of cervical dysplasia and cancer by recommending the HPV vaccine and applicable cervical cancer/HPV DNA testing as recommended by the U.S. Preventive Services Task Force29 and the American Cancer Society30. The higher prevalence of health burdens among cervical cancer survivors, particularly women from racial/ethnic minority groups, also necessitates that providers ensure regular follow-up care and comorbidity management. Expanding access to prevention and treatment services for un/underinsured populations is equally important, given the increased cost of care and physical sequelae for cervical cancers diagnosed at late stages. Second, the differing health behaviors of cervical cancer survivors and their association with health and economic burden cannot be ignored. Primary care providers of cervical cancer survivors should query the health behaviors of their patients, particularly in the first 5 years after diagnosis when a “teachable moment” exists to encourage survivors to engage in physical activity, eat a balanced diet, and quit smoking31, 32. Given that cervical cancer survivors have one of the highest rates of smoking compared to both cancer survivors26 and non-cancer controls, and we know that smoking increases the risk of second primary cancers33-36, a considerable need exists for provider-level interventions to increase awareness and communication about smoking cessation and healthy lifestyles with cervical cancer survivors.
Because smoking may be an important coping strategy, education about healthier alternative coping strategies is crucial.
Cervical cancer causes significant health and economic burdens among Texas women. Public health professionals have a unique opportunity to reduce these burdens through doing what they do best, prevention, early detection, and education.
Acknowledgments
Funding:
This work was supported by the Cancer Prevention & Research Institute of Texas (RP101207; the Cancer Prevention Training Program at MD Anderson (R25T CA57730); the National Cancer Institute (CA16672). The funding sources played no role in any aspect of this study, including no role in data collection, analysis, or interpretation; writing of the manuscript; or the decision to submit it for publication.
Footnotes
There are no conflicts of interest to disclose.
REFERENCES
- 1. [January 22, 2013];Surveillance Epidemiology and End Results Cancer Statistics: Fast Stats. [Google Scholar]
- 2. [January 31, 2013];Surveillance Epidemiology and End Results: SEER Stat Fact Sheets: Cervix Uteri. Available from: http://seer.cancer.gov/statfacts/html/cervix.html#survival.
- 3.Brookfield KF, Cheung MC, Lucci J, Fleming LE, Knoiaris LG. Disparities in survival among women with invasive cervical cancer. Cancer. 2009;115(1):166–178. doi: 10.1002/cncr.24007. [DOI] [PubMed] [Google Scholar]
- 4.Donovan KA, Taliaferro LA, Alvarez EM, Jacobsen PB, Roetzheim RG, Wenham RM. Sexual health in women treated for cervical cancer: character istics and correlates. Gynecol Oncol. 2007;104(2):428–434. doi: 10.1016/j.ygyno.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 5.Lindau ST, Gavrilova N, Anderson D. Sexual morbidity in very long term survivors of vaginal and cervical cancer: a comparison to national norms. Gynecol Oncol. 2007;106(2):413–418. doi: 10.1016/j.ygyno.2007.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fosså S,R, Vassilopoulou-Sellin R, Dahl A. Long term physical sequelae after adult-onset cancer. J Cancer Survivorship. 2008;2(1):3–11. doi: 10.1007/s11764-007-0039-5. [DOI] [PubMed] [Google Scholar]
- 7.Bradley S, Rose S, Lutgendorf S, Costanzo E, Anderson B. Quality of life and mental health in cervical and endometrial cancer survivors. Gynecol Oncol. 2006;100(3):479–486. doi: 10.1016/j.ygyno.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 8. [November 14, 2002];Texas Cancer Registry Inquiry System. Available from: http://www.cancer-rates.info/tx/index.php.
- 9.Risser D, Bowcock CL, Miller EA, Williams MA, Magid R, Garcia R. Cancer in Texas: Texas Cancer Registry. Texas Cancer Registry, Texas Department of State Health Services; Cancer Prevention Research Institute of Texas; Austin, TX: 2011. [Google Scholar]
- 10.ArcGIS Version 10.0. ESRI; Redlands, California: 2009. [Google Scholar]
- 11.SAS/STAT software . SAS Institute Inc.; Cary, NC: [Google Scholar]
- 12.Haskell WL, Lee I-Min, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sport Exer. 2007;39(8):1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 13.Keating ML, Norredam M, Landrum MB, Huskamp HA, Meara E. Physical and mental health status of older long-term cancer survivors. J Am Geriatr Soc. 2005;53(12):2145–2152. doi: 10.1111/j.1532-5415.2005.00507.x. [DOI] [PubMed] [Google Scholar]
- 14.Yabroff RK, Lawrence WF, Clauser S, Davis WW, Brown ML. Burden of illness in cancer survivors: findings from a population-based national sample. J Natl Cancer Inst. 2004;96(17):1322–1330. doi: 10.1093/jnci/djh255. [DOI] [PubMed] [Google Scholar]
- 15.Korfage IJ, Essink-Bot ML, Mols F, van de Poll-Franse L, Kruitwagen R, van Ballegooijen M. Health-related quality of life in cervical cancer survivors: a population-based survey. Int J Radiat Oncol. 2009;73(5):1501–1509. doi: 10.1016/j.ijrobp.2008.06.1905. [DOI] [PubMed] [Google Scholar]
- 16.Park SY, Bae DS, Nam JH, Park CT, Cho CH, Lee JM, et al. Quality of life and sexual problems in disease-free survivors of cervical cancer compared with the general population. Cancer. 2007;110(12):2716–2725. doi: 10.1002/cncr.23094. [DOI] [PubMed] [Google Scholar]
- 17.Schultz PN, Stava C, Beck ML, Vassilopoulou-Sellin R. Ethnic/racial influences on the physiologic health of cancer survivors. Cancer. 2004;100(1):156–164. doi: 10.1002/cncr.11897. [DOI] [PubMed] [Google Scholar]
- 18.Brooks SE, Baquet CR, Gardner JF, Moses G, Ghosh A. Cervical cancer-the impact of clinical presentation, health, and race on survival. J Assoc Acad Minor Phys. 2000;11(4):55–9. [PubMed] [Google Scholar]
- 19.Brooks SE, Chen TT, Ghosh A, Mullins DC, Gardner JF, Baquet CR. Cervical cancer outcomes analysis: impace of age, race, and comorbid illness on hospitalizations for invasive carcinoma of the cervix. Gynecol Oncol. 2000;79(1):107–115. doi: 10.1006/gyno.2000.5901. [DOI] [PubMed] [Google Scholar]
- 20.Ashing-Giwa KT, Kagawa-Singer M, Padilla GV, Tejero JS, Hsiao E, Chhabra R. The impact of cervical cancer and dysplasia: A qualitative, multi-ethnic study. Psycho-Oncol. 2004;13(10):709–728. doi: 10.1002/pon.785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ashing-Giwa KT, Tejero JS, Kim J, Padilla GV, Kagawa-Singer M, Tucker BM, et al. Cervical cancer survivorship in a population based sample. Gynecol Oncol. 2009;112(2):358–364. doi: 10.1016/j.ygyno.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 22. [January 31, 2013];The Dartmouth Atlas of Health Care: Price-Adjusted Medicare Payments per Enrollee, by Adjustment Type and Program Component. Available at: http://www.darthmouthatlas.org/data.
- 23.Blanchard CM, Courneya KS, Stein K. Cancer survivors’ adherence to lifestyle behavior recommendations and associations with health-related quality of life: results from the American Cancer Society's SCS-II. J Clin Oncol. 2008;26(13):2198–2204. doi: 10.1200/JCO.2007.14.6217. [DOI] [PubMed] [Google Scholar]
- 24.Mayer DK, Carlson J. Smoking patterns in cancer survivors. Nicotine Tob Res. 2011;13(1):34–40. doi: 10.1093/ntr/ntq199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mayer DK, Terrin NC, Menon U, Kreps GL, McCance K, Parsons SK, et al. Health behaviors in cancer survivors. Oncol Nurs Forum. 2007;34(2):643–651. doi: 10.1188/07.ONF.643-651. [DOI] [PubMed] [Google Scholar]
- 26.Coups EJ, Ostroff JS. A population-based estimate of the prevalence of behavioral risk factors among adult cancer survivors and noncancer controls. Prev Med. 2005;40(6):702–711. doi: 10.1016/j.ypmed.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 27.Bellizzi KM, Rowland JH, Jeffery DD, McNeel T. Health behaviors of cancer survivors: examining opportunities for cancer control intervention. J Clin Oncol. 2005;23(34):8884–8893. doi: 10.1200/JCO.2005.02.2343. [DOI] [PubMed] [Google Scholar]
- 28.Underwood JM, Townsend JS, Stewart SL, Buchannan N, Ekwueme DU, Hawkins NA, et al. Surveillance of demographic characteristics and health behaviors among adult cancer survivors -- Behavioral Risk Factor Surveil-lance System, United States, 2009. MMWR. 2012;61(SS01):1–23. [PubMed] [Google Scholar]
- 29.Screening for Cervical Cancer [April 2, 2013];2012 Available from: http://www.uspreventiveservicestaskforce.org/uspstf/uspscerv.htm.
- 30.American Cancer Society Guidelines for the Early Detection of Cancer [April 2, 2013];2013 Available from: http://www.cancer.org/healthy/findcancerearly/cancer-screeningguidelines/american-cancer-society-guidelines-for-the-early-detection-of-cancer.
- 31.McBride C, Ostroff JS. Teachable moments for promoting smoking cessation: the context of cancer care and survivorship. Cancer Control. 2003;10(4):325–333. doi: 10.1177/107327480301000407. [DOI] [PubMed] [Google Scholar]
- 32.Gritz ER, Fingeret MC, Vidrine DJ, Lazev AB, Mehta NV, Reece GP. Successes and failures of the teachable moment. Cancer. 2006;106(1):17–27. doi: 10.1002/cncr.21598. [DOI] [PubMed] [Google Scholar]
- 33.Boice JJ, Day NE, Andersen A, Brinton LA, Brown R, Choi NW, et al. Second cancers following radiation treatment for cervical cancer. An international collaboration among cancer registries. J Natl Cancer Inst. 1985;74(5):955–75. [PubMed] [Google Scholar]
- 34.Kleinerman RA, Boice JD, Storm HH, Sparen P, Andersen A, Pukkala E, et al. Second primary cancer after treatment for cervical cancer. An international cancer registries study. Cancer. 1995;76(3):442–452. doi: 10.1002/1097-0142(19950801)76:3<442::aid-cncr2820760315>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 35.Hemminki K, Dong C, Vaittinen P. Second primary cancer after in situ and invasive cervical cancer. Epidemiology. 2000;11(4):457–461. doi: 10.1097/00001648-200007000-00016. [DOI] [PubMed] [Google Scholar]
- 36.Rabkin CS, Biggar RJ, Melbye M, Curtis RE. Second primary cancers following anal and carcinoma: evidence of shared etiologic factors. Am J Epidemiol. 1992;136(1):54–58. doi: 10.1093/oxfordjournals.aje.a116420. [DOI] [PubMed] [Google Scholar]