Abstract
OBJECTIVE
To estimate the prevalence of diabetes in U.S. youth aged <20 years in 2009 and to estimate the total number of youth with diabetes in the U.S. by age, race/ethnicity, and diabetes type.
RESEARCH DESIGN AND METHODS
To address one of its primary aims, the SEARCH for Diabetes in Youth Study identified youth aged <20 years on 31 December 2009 with physician-diagnosed diabetes in selected areas of Colorado, Ohio, South Carolina, and Washington, among health plan members of Kaiser Permanente Southern California and among American Indians living on reservations in Arizona and New Mexico. Diabetes was classified as type 1, type 2, or other. Race/ethnicity was by self-report.
RESULTS
From a population of 3,458,974 youth aged <20 years, 7,695 youth with diabetes were identified (2.22/1,000): 6,668 with type 1 diabetes (1.93/1,000), 837 with type 2 diabetes (0.24/1,000), and 190 (0.05/1,000) with other diabetes types. Prevalence increased with age, was slightly higher in females than males, and was most prevalent in non-Hispanic White and least prevalent in Asian/Pacific Islanders, with Native American and black youth having the highest prevalence of type 2 diabetes. An estimated 191,986 U.S. youth aged <20 years have diabetes; 166,984 type 1 diabetes, 20,262 type 2 diabetes, and 4,740 other types.
CONCLUSIONS
Diabetes, one of the leading chronic diseases in childhood, affects >190,000 (1 of 433) youth aged <20 years in the U.S., with racial and ethnic disparities seen in diabetes prevalence, overall and by diabetes type.
Introduction
Diabetes is the third most common chronic disease of childhood (1), and its incidence has been increasing worldwide (2,3). Diabetes in children and adolescents is a set of complex disorders with heterogeneity in etiology, pathogenesis, clinical presentation, and outcomes. Type 1 diabetes is caused by immune-mediated β-cell destruction, leading to insulin deficiency and a lifelong insulin requirement, while type 2 diabetes is characterized by insulin resistance in skeletal muscle, liver, and adipose tissues with a failure of β-cell compensation and a relative insulin deficiency (4). The occurrence of type 2 diabetes in youth has been documented in several studies over the past decade (5–7) and is thought to be secondary to coincident increases in obesity in the general population. In addition, there are multiple less common types of diabetes in youth such as monogenic forms, including maturity-onset diabetes in the young, neonatal diabetes, and other known genetic disorders (8,9).
There are few recent studies of the prevalence of diabetes in youth in the U.S. by diabetes type. Most of the prior registries active in the U.S. were initially focused on type 1 diabetes (10,11) and have only recently begun to include type 2 diabetes (12,13). The SEARCH for Diabetes in Youth Study (SEARCH), with centers located in multiple states across the U.S. (14), was developed to assess the prevalence and incidence of diabetes in youth, overall and by type. Surveillance of youth with diabetes began in 2001 and is ongoing for incident case ascertainment, while prevalence surveillance was conducted for calendar years 2001, which was published previously (15), and 2009. The purposes of this article are to report the prevalence of diabetes in 2009, overall and by diabetes type, age, sex, and race/ethnicity, and to apply these estimates to U.S. census data for youth aged <20 years to estimate the total burden (absolute number) of youth with diabetes in the U.S. in 2009.
Research Design and Methods
A detailed description of SEARCH was published previously (14). Physician-diagnosed diabetes was identified in five SEARCH sites in California, Colorado, Ohio, South Carolina, and Washington. Four of these sites were geographically based; Colorado (14 counties), Ohio (8 counties), South Carolina (4 counties), and Washington (5 counties). The California site comprised health plan enrollees in Kaiser Permanente Southern California (KPSC; seven counties). Coordinated by the Colorado site, SEARCH also collected data from American Indians on selected reservations in Arizona and New Mexico. All centers had active surveillance by endocrinologists (pediatric and adult), other health care providers, hospitals, community health centers, health plan databases, and previously established diabetes databases. The Indian Health Service (IHS) beneficiary roll was used to identify the reservation-based American Indian youth. Two-source capture-recapture in the geographically based centers was used to estimate the completeness of case identification (16,17). Capture-recapture was not conducted for the membership-based center because the data sources used to ascertain case subjects within the membership-based center were not independent.
SEARCH study participants or their parent/guardian completed a survey that recorded age, date of diagnosis, sex, self-reported race/ethnicity, and place of residence. The study was reviewed and approved by the institutional review board(s) at each center and complied with the privacy rules established by the Health Insurance Portability and Accountability Act. Because this registry attempts to identify 100% of case subjects, case subject identification was conducted with an approved Health Insurance Portability and Accountability Act consent waiver in most study locations.
Sources of case reports included physician reports, medical record review, or self-report. Case subjects were considered valid if the medical record indicated a physician diagnosis, the diagnosis was verified directly by a physician, the participant was referred directly from a physician, or the case was included in a diabetes database that had required physician verification, while eligibility was based on age and area of residence. Clinical diabetes type was determined by the physician and categorized by the study as type 1 diabetes (type 1, type 1a, or type 1b), type 2 diabetes, or other diabetes (including other, hybrid, monogenic diabetes, secondary diabetes, unknown, and missing type). Cases of gestational diabetes mellitus were not included in the study. All case subjects were registered anonymously with the coordinating center at Wake Forest University and included in this report if they were registered by 31 October 2011.
The numerator for this analysis included all case subjects prevalent in 2009 who were aged <20 years on 31 December 2009, lived in one of the included geographic areas or were a member of the KPSC Health Plan or included on the IHS rolls, and not on active military duty or living in an institution. Race/ethnicity, which was by self-report or extracted from the medical record for 97.3% and estimated using geocoding for 2.7% (18,19), was classified as non-Hispanic White (NHW), non-Hispanic black (black), Hispanic, Asian/Pacific Islander (ASPI), or American Indian/Alaskan Native (AIAN).
The denominator included youth <20 years of age on 31 December 2009 who were noninstitutionalized civilian residents of the study areas covered by the geographic centers or who were members of KPSC residing in seven counties or who were enrolled IHS members in 2009. Derivation of the appropriate denominators was a multistep process taking into account racial/ethnicity categorization and the civilian nature of the study population (15).
For the four geographic centers, age-, sex-, and race/ethnicity-specific denominators were determined using the 2009 bridged-race intercensal population estimates released in October 2012 by the National Center for Health Statistics (18) and pooled across centers. The five racial/ethnic groups listed above were used. The race-bridging methods developed by the National Center for Health Statistics were applied to determine the probability that a multiracial youth belongs to each of the four remaining racial/ethnic groups after excluding the Hispanics (19). For the KPSC population, addresses of all members eligible for inclusion in the study based on age and geographic location were geocoded to the census block level. For each geocoded address, the number of residents of each group living in that block was estimated using Census file SF1 Table P8. The race- and ethnic-specific proportions were then applied to the sex-specific denominator estimates in 1-year age increments to estimate the racial and ethnic composition of youth by age and sex. As with the geographic-based centers, race-bridging methods were used. For AIAN, denominators were based on the IHS user population, defined as at least one IHS visit in the previous 3 years.
To derive civilian population denominators for the geographic centers, denominators for the youth aged 17–19 years were adjusted by subtracting the age-, sex-, racial/ethnic-, and county-specific number of active-duty military personnel derived from the information from the Military Family Resource Center (http://www.mfrc.org) and the Census Bureau. Racial/ethnic-specific denominator estimates were subsequently pooled across all SEARCH centers.
Statistical Methods
The prevalence of diabetes was expressed per 1,000 youth using data pooled across all SEARCH centers. The 95% CIs were calculated using the skew-corrected inverted score test assuming a binomial distribution (20,21). To obtain an estimate of the total number of youth <20 years of age with physician-diagnosed diabetes in the U.S. population, age-, sex-, and racial/ethnic-specific U.S. prevalence estimates derived from SEARCH were applied to the age-, sex-, and racial/ethnic-specific U.S. population on the basis of 2009 census population estimates. For the purposes of presentation, the standardized rates by race/ethnicity and four age groups are shown.
Results
A total of 7,695 youth aged <20 years with diabetes of all types was identified from a population of 3,458,974 youth (Table 1) for a crude prevalence of 2.22 case subjects/1,000 (95% CI 2.18–2.27). Total diabetes prevalence increased with age group from 0.30/1,000 (0.26–0.33) in those aged <5 years to 4.03/1,000 (3.90–4.16) among those aged 15–19 years. Prevalence was highest in NHW youth (2.70 case subjects/1,000 [95% CI 2.62–2.77]) and lowest in ASPI youth (0.80 case subjects/1,000 [0.70–0.92]). Females had a slightly higher prevalence (2.30 case subjects/1,000 [2.23–2.37]) than males (2.16 case subjects/1,000 [2.09–2.23]). Of the 7,695 youth with diabetes, 7,505 (97.5%) were identified as having either type 1 or type 2 diabetes. Of the remaining 190 case subjects (2.5%), 127 had secondary diabetes, and 63 had other or unknown type. These case subjects with a type other than type 1 or type 2 diabetes or with missing information on type represented a prevalence of 0.05 case subjects/1,000 (0.05–0.06) (data not shown) and are excluded from results that follow.
Table 1.
Prevalence of diabetes (all types) in SEARCH by age, race/ethnicity, and sex, 2009
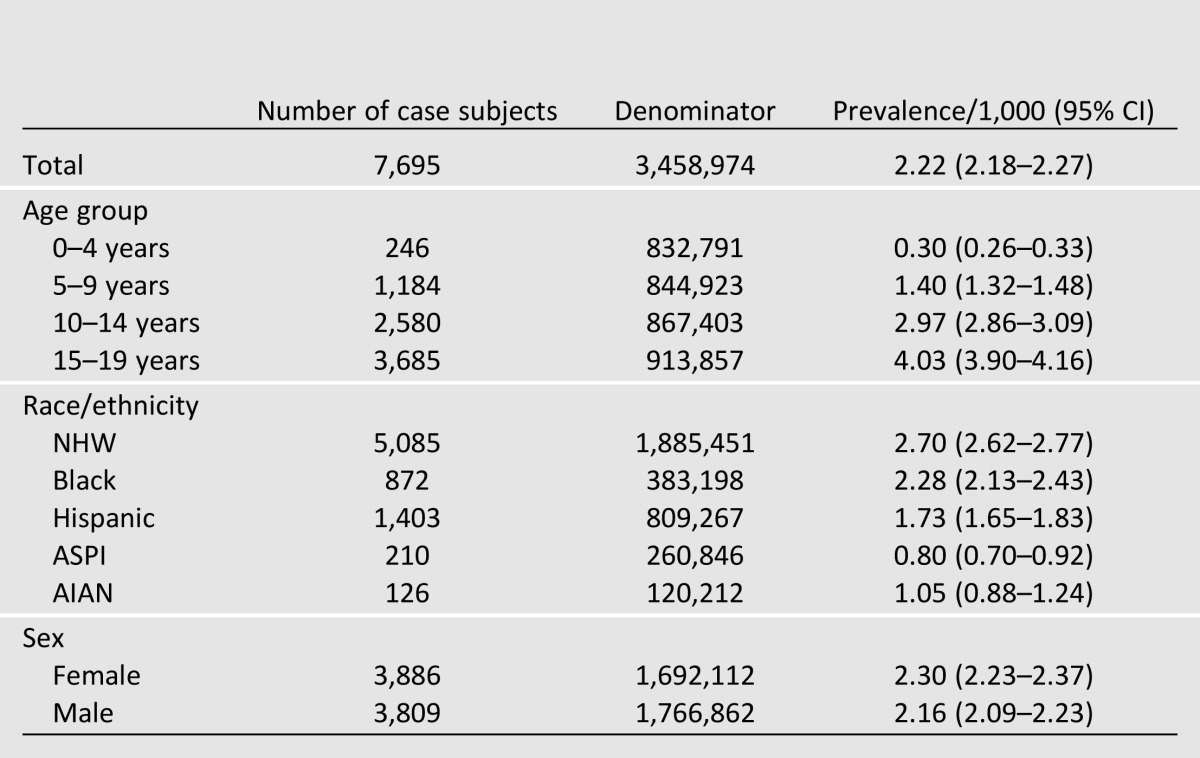
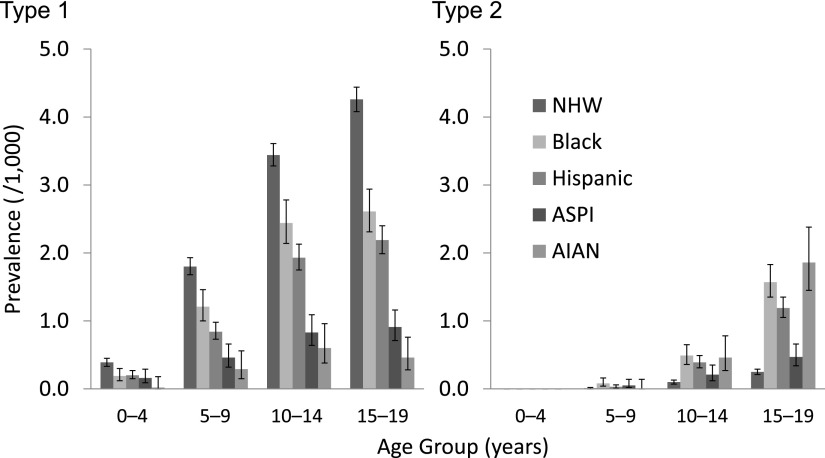
Table 2 shows the prevalence for type 1 and type 2 diabetes overall and by race/ethnicity. The prevalence of type 1 diabetes was 1.93 case subjects/1,000 (1.88–1.97) and of type 2 diabetes was 0.24 case subjects/1,000 (0.23–0.26). Type 1 diabetes prevalence was highest in NHW youth and lowest in AIAN. Conversely, type 2 diabetes prevalence was higher in youth from minority race/ethnic groups than in NHW youth. Among the 15–19-year-old AIAN, type 2 diabetes accounted for 80.0% of all case subjects (Fig. 1). Fig. 2 shows the age-specific prevalence by race/ethnicity and type. Prevalence rose with increasing age in all race/ethnic groups and was highest in the oldest age groups, except that in AIAN, the prevalence of type 1 diabetes was highest at age 10–14 years. The mean age of onset was 8.1 years for type 1 diabetes and 13.7 years for type 2 diabetes among youth diagnosed with diabetes before 20 years of age.
Table 2.
Estimates of prevalence in SEARCH/1,000 of diabetes according to diabetes type and race/ethnicity, 2009
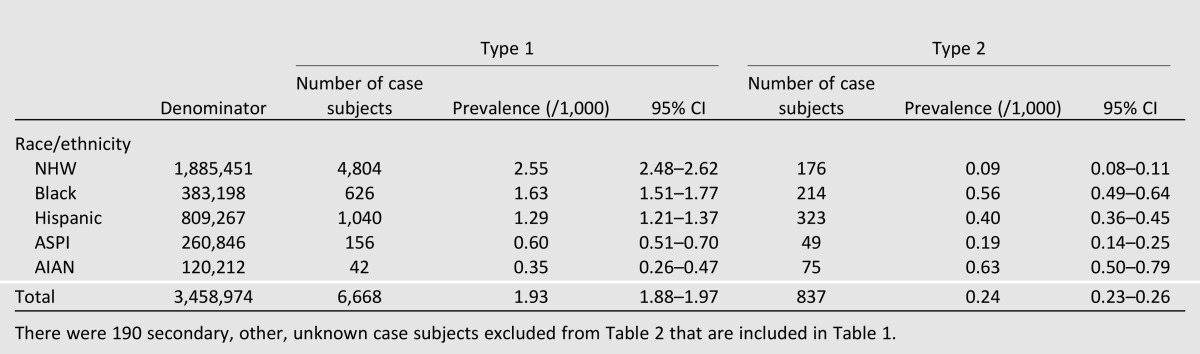
Figure 1.
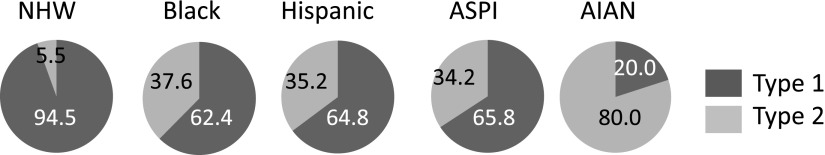
Proportion of type 1 and type 2 diabetes among 15–19 year olds in SEARCH by race/ethnicity. Diabetes type other/unknown not included in figure.
Figure 2.
Prevalence of diabetes in SEARCH/1,000 by type, age group, and race/ethnicity. Diabetes type other/secondary/unknown not included in figure. Error bars represent 95% CI.
The completeness of case ascertainment for type 1 diabetes in the four geographic centers was 99.3% (99.2–99.5%) and was similar by race/ethnicity and by age group. For type 2 diabetes, in which capture-recapture was restricted to ages 10–19 years due to small numbers under the age of 10 years, completeness was slightly lower at 96.1% (94.6–97.6%) and similar by race/ethnicity except for Hispanic youth, in whom it was 90.0% (88.0–92.0%).
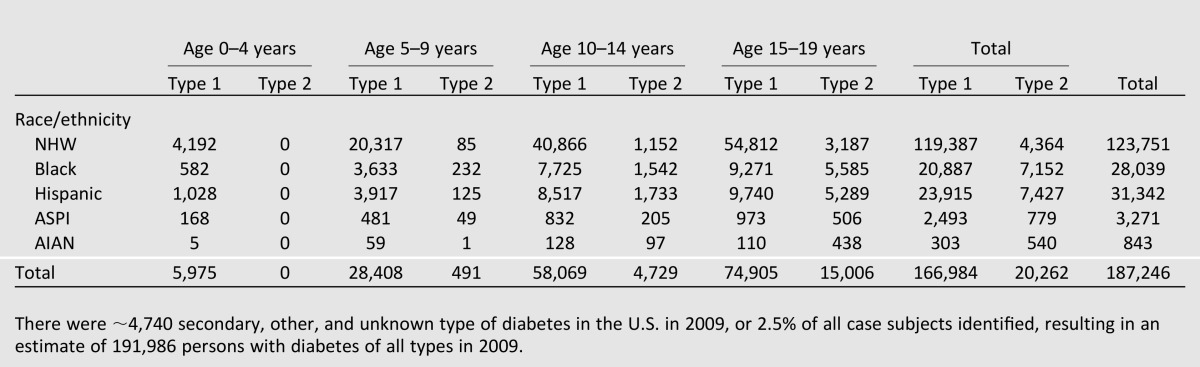
Based on SEARCH-derived prevalence, ∼191,986 youth with diabetes aged <20 years lived in the U.S. in 2009, including 166,984 with type 1 diabetes and 20,262 with type 2 diabetes (Table 3). There were ∼4,740 secondary, other, and unknown type of diabetes in the U.S. in 2009, or 2.5% of all case subjects identified.
Table 3.
Estimated number of youth with diabetes in the U.S. by age group, race/ethnicity, and diabetes type, 2009
Conclusions
Based on data from SEARCH, the largest, most comprehensive surveillance study of diabetes in U.S. youth to date, >190,000 youth in the U.S. were estimated to have physician-diagnosed diabetes in 2009. This represents ∼1 of every 433 of the ∼3.3 million youth aged <20 years. This represents an overall increase in the number of estimated cases of diabetes of 37,617 between our previously published estimates for 2001 (15) and 2009. The increase in the number of case subjects was primarily driven by an increase in type 1 diabetes, which increased among all race/ethnic groups.
Diabetes is one of the leading chronic diseases in youth—by our estimate, affecting 2.22/1,000 youth aged <20 years. Diabetes has a major impact on public health in this country, costing ∼$245 billion in 2012 and shortening life expectancy for those affected at young ages (22). The highest net value of future lost earnings due to premature death are for youth <18 years of age and for young adults between 18 and 34 years of age. The development of complications is related to the duration of diabetes, and youth with onset of diabetes early in life represent a population at high risk for developing these complications (23).
Comparisons of prevalence data may be subject to considerable bias, since prevalence is determined not only by disease incidence, but also by case survival, which may vary across populations. Prevalence data, however, are useful in determining the public health impact of diabetes. In 2011 and 2012, data from the National Survey of Children’s Health (24), based on parental self-report, estimated the prevalence of all types of diabetes among NHW youth aged <18 years to be 4.0 case subjects/1,000, 2.0/1,000 for Hispanics, 4.0/1,000 for blacks, and 1.0/1,000 for other race/ethnic groups. This is similar to our estimate for Hispanics (1.73/1,000), but is higher than our estimate for NHW (2.70/1,000) and black youth (2.28/1,000). However, those data are based on self-report and likely to be less reliable than the validated SEARCH data. A recent Canadian report on data from 2008 and 2009 suggests somewhat higher prevalence of diabetes in Canada at 2.0/1,000 for ages 1–9 years and 5.0/1,000 for ages 10–19 years (25).
Estimates of the prevalence of diabetes by type have also been reported from the U.S. state of South Carolina (26) and the Canadian province of Manitoba (27). In 1999, type 1 diabetes prevalence in South Carolina NHWs was 1.1/1,000 at ages 0–9 years and 2.5/1,000 among 10–19 year olds, somewhat lower than our results. In Manitoba from 1985–1993, prevalence of type 1 diabetes among NHW youth was 0.2/1,000 (age 0–4 years), 1.1/1,000 (age 5–9 years), and 2.4/1,000 (age 10–14 years), also lower than we report, likely due to rising rates of type 1 diabetes.
Type 2 diabetes occurred in youth from all race/ethnic groups in the SEARCH cohort. The proportion of type 2 diabetes was lowest in NHW but still represented 3.5% of all cases of diabetes in NHW youth. Studies of largely Caucasian youth in Germany, France, and the U.K. (28–30) indicate that type 2 diabetes remains rare. The overall burden of diabetes due to type 2 diabetes in SEARCH increased with age group in all race/ethnic groups, and, among 15–19 year olds, type 2 diabetes was more common than type 1 diabetes among AIAN youth. These prevalence figures, while estimating the current burden of diabetes by type, do not reflect any changes in proportion of diabetes types, which can only be estimated from incidence rates.
The prevalence of type 2 diabetes has been reported in other studies largely in minority populations. In Puerto Rican Hispanics, prevalence was 0.2/1,000 from age 10–19 years (31). The differentiation between type 1 and type 2 diabetes was based only on the use of insulin, likely underestimating the type 2 diabetes prevalence, as many youth with type 2 diabetes are also treated with insulin (32). The total prevalence of diabetes (any type) was 0.05/1,000 among >4,000 adolescents completing self-report information; 44% of these cases were classified as type 2 diabetes, implying a prevalence of 0.02/1,000, much lower than the 0.24/1,000 that we report. Possible factors contributing to differences in prevalence between studies include methods of ascertainment and ancestral region of the Hispanic population. In SEARCH, the majority of Hispanic participants’ families are of Mexican ancestry, rather than Caribbean (33), which would be likely in a sample from Puerto Rico.
There are several reports of type 2 diabetes prevalence in American Indian or First Nations, Canadian populations. Prevalence in American Indians residing in Montana, assessed using medical record review, was 3.5/1,000 (age 10–14 years) but only 0.8/1,000 in youth aged 15–19 years (34). In First Nations youth in Canada aged 5–14 years, prevalence was 7.7/1,000 (35), and was 13.0/1,000 among Oklahoma Cherokees aged 10–19 years who underwent screening (36). Among Pima Indians, who have undergone systematic oral glucose tolerance testing for many years, the prevalence in 1987–1996 was 38/1,000 among males aged 15–19 years and 53/1,000 among females (37), rates much higher than observed in the American Indian populations in SEARCH and the highest in the world. AIAN youth have the highest prevalence of type 2 diabetes of any race/ethnic group.
There are some limitations to this study. SEARCH relies on physician diagnosis of diabetes, identifying only clinically recognized case subjects reported to or directly identified by SEARCH sites, so undiagnosed case subjects are not included in these prevalence estimates. For type 1 diabetes, the number of undiagnosed case subjects is likely very small, but type 2 diabetes, at least in adults, can exist for an extended period of time prior to diagnosis. However, there is very little undiagnosed diabetes in youth (38). Some older youth diagnosed with type 2 diabetes might not be seeing a physician who is aware of the SEARCH study, therefore leading to an underestimation of prevalence in the older age group. However, this is likely to have only slight impact based on our capture-recapture estimates. Denominator estimates were based on U.S. Census estimates of the population in 2009 but corrected for 2010 census results; however, race/ethnicity was geocoded for 2.7% of case subjects using 2010 census data, likely resulting in some race/ethnicity misclassifications. Also, the number of AIAN youth was small, was primarily from IHS rolls in the Southwest, and may not be representative of AIAN youth from other parts of the country or those not using the IHS. In-person study visits were not conducted on 2009 prevalent case subjects, so presence of diabetes autoantibodies and details of medication use, obesity, and other risk factors are not available. However, previous SEARCH data demonstrated that provider assessment of diabetes type is a valid assessment of etiologic diabetes type (39). The number of participating sites in SEARCH has changed since 2001 when the first comprehensive prevalence survey was conducted (15). A detailed comparison of changes in prevalence, by diabetes type, between 2001 and 2009 taking into account the reduced number of sites will be published separately. Also, as case ascertainment was based on site/regional networks, some youth may not have been identified, particularly those who are older. Thus, the estimated prevalence presented in this article is more likely to be an underestimate in the upper age group, and this may explain the difference between these data and the higher prevalence observed in older Canadian youth.
This study also has important strengths. The population under surveillance by the SEARCH sites (∼3.5 million) has a similar distribution of important sociodemographic factors (e.g., race/ethnicity, parental education, and income) to the U.S. population as a whole, suggesting that SEARCH is a representative sample of U.S. youth at risk for diabetes (Supplementary Table 1). Thus, these prevalence estimates should be an accurate representation of the true number of diagnosed case subjects in the study areas. This is also the largest such study of diabetes in youth in the U.S., making the estimates for the numbers of case subjects reasonably precise. The paucity of data on the prevalence of type 1 diabetes in contemporary cohorts of youth make the contribution of the SEARCH study particularly valuable.
In conclusion, the burden of diabetes in U.S. youth <20 years of age in 2009 is estimated to be 191,986. Of these, 166,984 have type 1 diabetes, and 20,262 have type 2 diabetes. The burden of type 1 diabetes is highest among NHW youth and is highest for type 2 diabetes in minority youth, especially AIAN youth. Efforts are needed both to provide care for youth living with either type 1 or type 2 diabetes and to reduce the risk for development of diabetes and diabetes-related complications in high-risk populations.
Supplementary Material
Article Information
Acknowledgments. The SEARCH for Diabetes in Youth Study is indebted to the many youth, families, and health care providers whose participation made this study possible. The authors thank the General Clinical Research Centers at the South Carolina Clinical and Translational Research Institute at the Medical University of South Carolina (National Institutes of Health [NIH]/National Center for Research Resources grant UL1-RR-029882), Children’s Hospital and Regional Medical Center (grant M01-RR-00037), Colorado Pediatric General Clinical Research Center (grant M01-RR-00069) and the Barbara Davis Center at the University of Colorado at Denver (DERC NIH P30-DK-57516), and the Institutional Clinical and Translational Science Award, NIH/National Center for Research Resources at the University of Cincinnati (grant 1UL1-RR-026314-01), and the Children with Medical Handicaps program managed by the Ohio Department of Health for involvement in the study.
Funding. The SEARCH for Diabetes in Youth Study is funded by the Centers for Disease Control and Prevention (PA numbers 00097, DP-05-069, and DP-10-001) and is supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Site contract numbers: Kaiser Permanente Southern California (U48/CCU919219, U01DP000246, and U18DP002714), University of Colorado Denver (U48/CCU819241-3, U01DP000247, and U18DP000247-06A1), Children’s Hospital Medical Center (Cincinnati) (U48/CCU519239, U01DP000248, and 1U18DP002709), University of North Carolina at Chapel Hill (U48/CCU419249, U01DP000254, and U18DP002708-01), University of Washington School of Medicine (U58/CCU019235-4, U01DP000244, and U18DP002710-01), and Wake Forest University School of Medicine (U48/CCU919219, U01DP000250, and 200-2010-35171).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. D.J.P. and R.F.H. codeveloped and cowrote the manuscript. J.T. conducted the analyses. D.D. (study cochair), J.M.L., E.J.M.-D. (study cochair), and C.P. obtained funding, contributed to discussions, and edited the manuscript. J.D. supervised analyses and edited the manuscript. G.I., A.D.L., B.L., and S.H.S. contributed to discussions and edited the manuscript. D.A.S. contributed to discussion, edited the manuscript, and collected data. D.J.P. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. This study was presented in abstract form at the 72nd Scientific Sessions of the American Diabetes Association, Philadelphia, PA, 8–12 June 2012.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc13-1838/-/DC1.
A slide set summarizing this article is available online.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention and the National Institute of Diabetes and Digestive and Kidney Diseases.
References
- 1.Allen PJ, Vessey JA. Primary Care of the Child with a Chronic Condition. 4th ed St. Louis, Mosby-Yearbook, 2004 [Google Scholar]
- 2.Patterson CC, Gyürüs E, Rosenbauer J, et al. Trends in childhood type 1 diabetes incidence in Europe during 1989-2008: evidence of non-uniformity over time in rates of increase. Diabetologia 2012;55:2142–2147 [DOI] [PubMed] [Google Scholar]
- 3.Vehik K, Dabelea D. The changing epidemiology of type 1 diabetes: why is it going through the roof? Diabetes Metab Res Rev 2011;27:3–13 [DOI] [PubMed] [Google Scholar]
- 4.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care 2013;36(Suppl. 1):S67–S74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pinhas-Hamiel O, Zeitler P. The global spread of type 2 diabetes mellitus in children and adolescents. J Pediatr 2005;146:693–700 [DOI] [PubMed] [Google Scholar]
- 6.Dabelea D, Bell RA, D’Agostino RB, Jr, et al. Writing Group for the SEARCH for Diabetes in Youth Study Group Incidence of diabetes in youth in the United States. JAMA 2007;297:2716–2724 [DOI] [PubMed] [Google Scholar]
- 7.Dabelea D, Pettitt DJ, Jones KL, Arslanian S. Type 2 diabetes mellitus in minority children and adolescents. An emerging problem. Endocrinol Metab Clin North Am 1999;28:709–729 [DOI] [PubMed] [Google Scholar]
- 8.Gilliam LK, Pihoker C, Ellard S, et al. Unrecognized maturity onset diabetes of the young (MODY) due to HNF1-alpha mutations in the SEARCH for Diabetes in Youth Study. Diabetes 2007;56(Suppl. 1):A74–A75 [Google Scholar]
- 9.Kanakatti Shankar R, Pihoker C, Dolan LM, et al. SEARCH for Diabetes in Youth Study Group Permanent neonatal diabetes mellitus: prevalence and genetic diagnosis in the SEARCH for Diabetes in Youth Study. Pediatr Diabetes 2013;14:174–180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.LaPorte RE, Fishbein HA, Drash AL, et al. The Pittsburgh insulin-dependent diabetes mellitus (IDDM) registry. The incidence of insulin-dependent diabetes mellitus in Allegheny County, Pennsylvania (1965-1976). Diabetes 1981;30:279–284 [DOI] [PubMed] [Google Scholar]
- 11.Palta M, LeCaire T, Daniels K, Shen G, Allen C, D’Alessio D. Risk factors for hospitalization in a cohort with type 1 diabetes. Wisconsin Diabetes Registry. Am J Epidemiol 1997;146:627–636 [DOI] [PubMed] [Google Scholar]
- 12.Lipman TH, Levitt Katz LE, Ratcliffe SJ, et al. Increasing incidence of type 1 diabetes in youth: twenty years of the Philadelphia Pediatric Diabetes Registry. Diabetes Care 2013;36:1597–1603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lipton RB, Drum ML, Danielson KK, Greeley SAW, Bell GI, Hagopian WA. Onset features and subsequent clinical evolution of childhood diabetes over several years. Pediatr Diabetes 2011;12:326–334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.SEARCH Study Group SEARCH for Diabetes in Youth: a multi-center study of the prevalence, incidence and classification of diabetes mellitus in youth. Control Clin Trials 2004;25:458–471 [DOI] [PubMed] [Google Scholar]
- 15.Liese AD, D’Agostino RB, Jr, Hamman RF, et al. SEARCH for Diabetes in Youth Study Group The burden of diabetes mellitus among US youth: prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics 2006;118:1510–1518 [DOI] [PubMed] [Google Scholar]
- 16.Verlato G, Muggeo M. Capture-recapture method in the epidemiology of type 2 diabetes: a contribution from the Verona Diabetes Study. Diabetes Care 2000;23:759–764 [DOI] [PubMed] [Google Scholar]
- 17.Chao A, Tsay PK, Lin SH, Shau WY, Chao DY. The applications of capture-recapture models to epidemiological data. Stat Med 2001;20:3123–3157 [DOI] [PubMed] [Google Scholar]
- 18.Division of Vital Statistics. National Center for Health Statistics, July 1, 2000-July 2009 Revised Bridged-Race Intercensal Population Estimates [article online]. 2013. Available from http://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm#july2009 Accessed 17 September 2013
- 19.Chen W, Petitti DB, Enger S. Limitations and potential uses of census-based data on ethnicity in a diverse community. Ann Epidemiol 2004;14:339–345 [DOI] [PubMed] [Google Scholar]
- 20.Gart JJ, Nam J-M. Approximate interval estimation of the difference in binomial parameters: correction for skewness and extension to multiple tables. Biometrics 1990;46:637–643 [PubMed] [Google Scholar]
- 21.Hepworth G. Confidence intervals for proportions estimated by group testing with groups of unequal size. J Agric Biol Environ Stat 2005;10:478–497 [Google Scholar]
- 22.American Diabetes Association Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013;36:1033–1046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krakoff J, Lindsay RS, Looker HC, Nelson RG, Hanson RL, Knowler WC. Incidence of retinopathy and nephropathy in youth-onset compared with adult-onset type 2 diabetes. Diabetes Care 2003;26:76–81 [DOI] [PubMed] [Google Scholar]
- 24.Data Resource Center for Child and Adolescent Health. 2011/12 National Survey of Children's Health. Available from http://www.childhealthdata.org/browse/survey/results?q=2460&g=456&r=1 Accessed 4 June 2013
- 25.Pelletier C, Dai S, Roberts KC, Bienek A, Onysko J, Pelletier L. Report summary. Diabetes in Canada: facts and figures from a public health perspective. Chronic Dis Inj Can 2012;33:53–54 [PubMed] [Google Scholar]
- 26.Oeltmann JE, Liese AD, Heinze HJ, Addy CL, Mayer-Davis EJ. Prevalence of diagnosed diabetes among African-American and non-Hispanic white youth, 1999. Diabetes Care 2003;26:2531–2535 [DOI] [PubMed] [Google Scholar]
- 27.Blanchard JF, Dean H, Anderson K, Wajda A, Ludwig S, Depew N. Incidence and prevalence of diabetes in children aged 0-14 years in Manitoba, Canada, 1985-1993. Diabetes Care 1997;20:512–515 [DOI] [PubMed] [Google Scholar]
- 28.Schober E, Holl RW, Grabert M, et al. Diabetes mellitus type 2 in childhood and adolescence in Germany and parts of Austria. Eur J Pediatr 2005;164:705–707 [DOI] [PubMed] [Google Scholar]
- 29.Ortega-Rodriguez E, Levy-Marchal C, Tubiana N, Czernichow P, Polak M. Emergence of type 2 diabetes in an hospital based cohort of children with diabetes mellitus. Diabetes Metab 2001;27:574–578 [PubMed] [Google Scholar]
- 30.Feltbower RG, McKinney PA, Campbell FM, Stephenson CR, Bodansky HJ. Type 2 and other forms of diabetes in 0-30 year olds: a hospital based study in Leeds, UK. Arch Dis Child 2003;88:676–679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pérez-Perdomo R, Pérez-Cardona CM, Allende-Vigo M, Rivera-Rodríguez MI, Rodríguez-Lugo LA. Type 2 diabetes mellitus among youth in Puerto Rico, 2003. P R Health Sci J 2005;24:111–117 [PubMed] [Google Scholar]
- 32.Pihoker C, Badura A, Talton J, et al. SEARCH for Diabetes in Youth Correlates of Treatment Patterns Among Youth with Type 2 Diabetes. Pediatr Diab 2010;11(Suppl. S.14):108 [Google Scholar]
- 33.Lawrence JM, Mayer-Davis EJ, Reynolds K, et al. SEARCH for Diabetes in Youth Study Group Diabetes in Hispanic American youth: prevalence, incidence, demographics, and clinical characteristics: the SEARCH for Diabetes in Youth Study. Diabetes Care 2009;32(Suppl. 2):S123–S132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moore KR, Harwell TS, McDowall JM, Helgerson SD, Gohdes D. Three-year prevalence and incidence of diabetes among American Indian youth in Montana and Wyoming, 1999 to 2001. J Pediatr 2003;143:368–371 [DOI] [PubMed] [Google Scholar]
- 35.Dean H. NIDDM-Y in First Nation children in Canada. Clin Pediatr (Phila) 1998;37:89–96 [DOI] [PubMed] [Google Scholar]
- 36.Lee ET, Begum M, Wang W, et al. Type 2 diabetes and impaired fasting glucose in American Indians aged 5-40 years: the Cherokee diabetes study. Ann Epidemiol 2004;14:696–704 [DOI] [PubMed] [Google Scholar]
- 37.Dabelea D, Hanson RL, Bennett PH, Roumain J, Knowler WC, Pettitt DJ. Increasing prevalence of Type II diabetes in American Indian children. Diabetologia 1998;41:904–910 [DOI] [PubMed] [Google Scholar]
- 38.Baranowski T, Cooper DM, Harrell J, Hirst K, Kaufman FR, Goran M, Resnicow K, STOPP-T2D Prevention Study Group Presence of diabetes risk factors in a large U.S. eight-grade cohort. Diabetes Care 2006;29:212–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dabelea D, Pihoker C, Talton JW, et al. SEARCH for Diabetes in Youth Study Etiological approach to characterization of diabetes type: the SEARCH for Diabetes in Youth Study. Diabetes Care 2011;34:1628–1633 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.