Abstract
Objective
To systematically review evidence from field interventions on the effectiveness of monetary subsidies in promoting healthier food purchases and consumption.
Design
Keyword and reference searches were conducted in five electronic databases: Cochrane Library, EconLit, MEDLINE, PsycINFO and Web of Science. Studies were included based on the following criteria: (i) intervention: field experiments; (ii) population: adolescents 12–17 years old or adults 18 years and older; (iii) design: randomized controlled trials, cohort studies or pre–post studies; (iv) subsidy: price discounts or vouchers for healthier foods; (v) outcome: food purchases or consumption; (vi) period: 1990–2012; and (vii) language: English. Twenty-four articles on twenty distinct experiments were included with study quality assessed using predefined methodological criteria.
Setting
Interventions were conducted in seven countries: the USA (n 14), Canada (n 1), France (n 1), Germany (n 1), Netherlands (n 1), South Africa (n 1) and the UK (n 1). Subsidies applied to different types of foods such as fruits, vegetables and low-fat snacks sold in supermarkets, cafeterias, vending machines, farmers’ markets or restaurants.
Subjects
Interventions enrolled various population subgroups such as school/university students, metropolitan transit workers and low-income women.
Results
All but one study found subsidies on healthier foods to significantly increase the purchase and consumption of promoted products. Study limitations include small and convenience samples, short intervention and follow-up duration, and lack of cost-effectiveness and overall diet assessment.
Conclusions
Subsidizing healthier foods tends to be effective in modifying dietary behaviour. Future studies should examine its long-term effectiveness and cost-effectiveness at the population level and its impact on overall diet intake.
Keywords: Subsidy, Discount, Voucher, Diet, Food
Poor diet quality is among the most pressing health challenges in the USA and worldwide, and is associated with major causes of morbidity and mortality including CVD, hypertension, type 2 diabetes and some types of cancer( 1 ). The US National Prevention Strategy, released in June 2011, considers healthy eating a priority area and calls for increased access to healthy and affordable foods in communities( 2 ).
High prices remain a formidable barrier for many people, especially those of low socio-economic status, to adopt a healthier diet( 3 ). A 2004–2006 survey of major supermarket chains in Seattle found that foods in the bottom quintile of energy density cost on average $US 4·34 per 1000 kJ, compared with $US 0·42 per 1000 kJ for foods in the top quintile( 4 ). The large price differential between nutrient-rich, low-energy-dense foods such as fruits and vegetables and nutrient-poor, energy-dense foods might contribute to poor diet quality and various sociodemographic health disparities( 4 – 7 ).
Increasing attention has been paid to the use of economic incentives in modifying individuals’ dietary behaviour. Fiscal policies (i.e. taxation, subsidies or direct pricing) to influence food prices ‘in ways that encourage healthy eating’ have been recommended by the WHO( 8 , 9 ). In September 2011, Hungary imposed a 10 forint (approximately $US 0·04) tax on packaged foods high in fat, sugar or salt( 10 ). One month later, Denmark implemented a tax of 16 Danish krone (approximately $US 2·80) per kilogram of saturated fat on domestic and imported foods with a saturated fat content exceeding 2·3 %( 11 ). By 2009, thirty-three US states had levied sales taxes on sugar-sweetened soft drinks with an average tax rate of 5·2 %( 12 ). In addition, the Food, Conservation, and Energy Act of 2008 (Public Law H.R.6124, also known as the Farm Bill)( 13 ) required a US Department of Agriculture pilot project to examine the effectiveness of a 30 % price discount on fruits, vegetables and other healthier foods in changing dietary behaviour among low-income residents enrolled in the Supplemental Nutrition Assistance Program( 14 ). Preliminary results may be available in 2013.
In the present study, we review current evidence from field interventions subsidizing healthier foods on their effectiveness in modifying dietary behaviour. A ‘field intervention’ refers to an experiment conducted in the real world rather than in the laboratory. The review focuses on the findings related to the following issues: Are subsidies effective in promoting healthier food purchases and consumption? What level of subsidies is required to be effective? Is there evidence of a dose–response relationship? Does the effectiveness differ across population subgroups? Are subsidies more or less effective than other intervention strategies? Does the impact maintain after the withdrawal of the incentive? Admittedly, it is unrealistic to address all these issues in a single review article as answers to those issues remain tentative, incomplete or even contradictory sometimes. Nevertheless, it serves as a starting point in the direction to synthesize relevant findings.
Four recent review articles are particularly relevant to our study. Kane et al. reviewed the role of economic incentives on a wide range of consumers’ preventive behaviours such as healthy diet, physical exercise and immunization( 15 ). Wall et al. reviewed randomized controlled trials (RCT) that used monetary rewards to incentivize healthy eating and weight control( 16 ). Thow et al. reviewed empirical and modelling studies on the effectiveness of subsidies and taxes levied on specific food items on consumption, body weight and chronic diseases( 17 ). Jensen et al. reviewed the effectiveness of economic incentives in modifying dietary behaviour among schoolchildren( 18 ).
Our study contributes to the literature by systematically reviewing most recent scientific evidence on the effectiveness of monetary subsidies in promoting healthier food purchases and consumption. To synthesize data from a reasonably homogeneous body of literature with relatively rigorous study design, we exclusively focus on: (i) prospective field interventions with a clear experimental design; (ii) monetary subsidies in the form of a price discount or voucher for healthier foods; and (iii) food purchases and intake among adolescent and adult populations.
Methods
Study selection criteria
Studies which met all of the following criteria were included in the review: (i) intervention type: prospective field experiments; (ii) study population: adolescents 12–17 years old or adults 18 years and older; (iii) study design: RCT, cohort studies or pre–post studies; (iv) subsidy type: price discounts or vouchers for healthier foods; (v) outcome measure: food purchases or consumption; (vi) publication date: between 1 January 1990 and 1 May 2012; and (vii) language: articles written in English.
Arguably, children aged 11 years and younger comprise an important population for dietary intervention. Even so, we decided not to include them in the review for the following reasons. Children largely depend on their parents to pay their expenses. Therefore, most of the dietary interventions on children focus on free provision of a healthier meal or fruit/vegetable, nutrition education, role modelling and promotion of physical activities, while children-targeted interventions using a price discount or voucher worth a certain amount of money exchangeable for healthier foods remain scarce. Moreover, there has already been a systematic review on the effectiveness of economic incentives in modifying nutritional behaviour among schoolchildren by Jensen et al.( 18 ).
Search strategy
We searched five electronic bibliographic databases – Cochrane Library, EconLit, MEDLINE, PsycINFO and Web of Science – using various combinations of keywords such as ‘subsidy’, ‘discount’, ‘voucher’, ‘food’ and ‘diet’. A complete search algorithm for MEDLINE is reported in Table 1. Algorithms for other databases are either identical or sufficiently similar. Titles and abstracts of the articles identified through the keyword search strategy were screened against the study selection criteria. Potentially relevant articles were retrieved for evaluation of the full text.
Table 1.
Search strategy for MEDLINE database
| Search history | |
|---|---|
| 1 | Economic |
| 2 | Financial |
| 3 | Monetary |
| 4 | Pecuniary |
| 5 | Fiscal |
| 6 | Incentive |
| 7 | Motivation |
| 8 | Discount |
| 9 | Rebate |
| 10 | Refund |
| 11 | Subsidy |
| 12 | Cash |
| 13 | Voucher |
| 14 | Bonus |
| 15 | Reward |
| 16 | Award |
| 17 | Coupon |
| 18 | Token |
| 19 | Reimbursement |
| 20 | Repayment |
| 21 | Ticket |
| 22 | Gift |
| 23 | Raffle |
| 24 | Lottery |
| 25 | Prize |
| 26 | Money |
| 27 | Price |
| 28 | Food |
| 29 | Diet |
| 30 | Nutrition |
| 31 | Eating |
| 32 | 1 or 2 or 3 or 4 or 5 |
| 33 | 6 or 7 |
| 34 | 32 and 33 |
| 35 | 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 |
| 36 | 34 or 35 |
| 37 | 28 or 29 or 30 or 31 |
| 38 | 36 and 37 |
| Limited to title/abstract, human, English, and between 1 January 1990 and 1 May 2012 |
We also conducted a reference list search (i.e. backward search) and a cited reference search (i.e. forward search) from full-text articles meeting the study selection criteria. Articles identified through this process were further screened and evaluated using the same criteria. We repeated reference searches on all newly identified articles until no additional relevant article was found.
Data extraction and synthesis
A standardized data extraction form was used to collect the following methodological and outcome variables from each included study: intervention country, intervention duration, follow-up duration, intervention strategy, intervention setting, study design, economic incentive, eligible product, targeted population, targeted behaviour, sample size, outcome measure, study results and intervention effectiveness.
Ideally, a formal meta-analysis should be conducted to provide quantitative estimates of the effect of subsidies in promoting healthier diet. This requires intervention type and outcome measure across studies to be sufficiently homogeneous. However, among the twenty interventions included in the present review, few adopted the same experiment strategy and the type of food purchase/intake also differed substantially. The dissimilar nature of intervention strategy and outcome measure precludes meta-analysis. The present work was thus limited to a narrative review of the included studies with general themes summarized.
Study quality assessment
Following Wu et al.( 19 ), the quality of each study included in the review was assessed by the presence or absence of ten dichotomous criteria: (i) a control group was included; (ii) baseline characteristics between the control and intervention groups were similar; (iii) the intervention period was at least 5 weeks; (iv) the follow-up period was at least 3 weeks; (v) an objective measure of food purchases or intake was used; (vi) the measurement tool was shown to be reliable and valid in previously published studies; (vii) participants were randomly recruited with a response rate of 60 % or higher; (viii) attrition was analysed and determined not to differ significantly by respondents’ baseline characteristics between the control and intervention groups; (ix) potential confounders were properly controlled for in the analysis; and (x) intervention procedures were documented in detail in the article. A total study quality score ranging from 0 to 10 was obtained for each study by summing up these criteria. Quality scores helped measure the strength of the study evidence and were not used to determine the inclusion of studies.
Results
Study selection
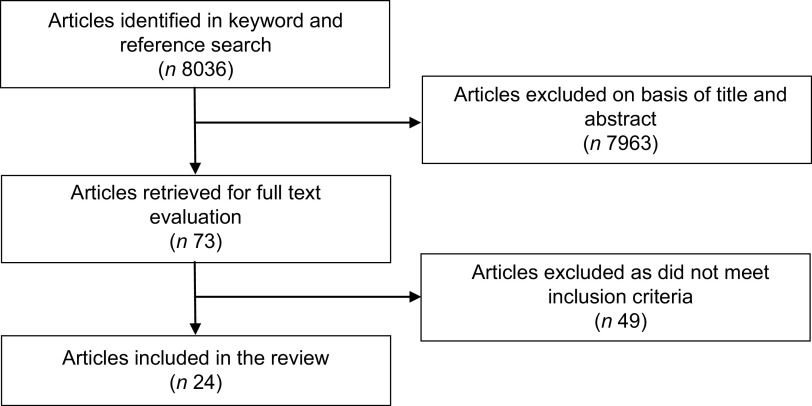
A total of 8036 articles were identified in the keyword and reference search, among which 7963 were excluded in title/abstract screening. The remaining seventy-three articles were further evaluated in full text against the study selection criteria. Among them, thirteen were controlled laboratory experiments( 20 – 24 ), computer simulations( 25 , 26 ) or modelling exercises( 27 – 32 ) rather than field interventions; six exclusively enrolled children participants aged 11 years and younger( 33 – 38 ); ten were cross-sectional observational studies without clear experimental or quasi-experimental designs( 39 – 48 ); seven provided fruits and vegetables in school or other settings for free rather than using a price discount or voucher( 49 – 55 ); seven used economic incentives unrelated to healthier foods (i.e. financial rewards for weight loss( 56 – 60 ) or subsidies on staple or other basic food necessities( 61 , 62 )); four used weight loss rather than food purchases or consumption as the outcome measure( 63 – 66 ); and two were published before 1990( 67 , 68 ). Excluding the above articles yielded a final pool of twenty-four studies( 69 – 92 ) with reported outcomes from twenty distinct field interventions. Figure 1 shows the study selection process.
Fig. 1.
Flowchart showing the selection of studies included in the present review
Basic characteristics of the included studies
Table 2 summarizes the studies included in the review. The twenty interventions were conducted in seven countries: a majority of them (n 14) in the USA, and the remaining six in Canada, France, Germany, Netherlands, South Africa and the UK. Fourteen interventions provided price discounts for healthier food items, and the other six used vouchers worth a certain amount of money exchangeable for healthier foods. Subsidies (i.e. price discounts and vouchers) applied to various types of healthy foods and beverages sold in supermarkets (n 6), cafeterias (n 5), vending machines (n 5), farmers’ markets (n 2), restaurants (n 1) or organic food stores (n 1). Eligible foods mainly consisted of fruits/vegetables and low-fat snacks, and eligible beverages mainly consisted of fruit juice, vegetable soup and low-fat milk. Interventions enrolled different population subgroups such as school or university students, metropolitan transit workers and low-income women. RCT were the most common study design (n 9), followed by pre–post studies (n 8) and cohort studies (n 3). The difference between pre–post and cohort studies is that the latter not only had an intervention group as in the former but also a control group which was followed before and during the intervention.
Table 2b.
Summary of studies included in a review of field experiments on the effectiveness of subsidies in promoting healthy food purchases and consumption: targeted population, targeted behaviour, sample size/unit and intervention strategy
| Study ID | Reference | Targeted population | Targeted behaviour | Sample size/unit | Intervention strategy |
|---|---|---|---|---|---|
| 1 | Jeffery et al. (1994)( 69 ) | University employees | Cafeteria food purchase | 321 employees | The cafeteria intervention consisted of doubling the number of fruit choices, increasing salad ingredient selections by 3, and reducing the prices of fruits and salad by 50 % |
| 2 | Paine-Andrews et al. (1996)( 70 ) | Supermarket shoppers | Supermarket food purchase | N/A | The supermarket intervention consisted of prompting, product sampling and a 20–25 % price discount for low-fat milk, salad dressings and frozen desserts using an interrupted time-series design with switching replications |
| 3 | French et al. (1997)( 71 ) | University students and employees | Vending machine purchase | 9 vending machines | Prices of low-fat snacks in vending machines were reduced by 50 % during the intervention and returned to normal after the intervention |
| 4 | French et al. (1997)( 72 ) | High-school students and employees | Cafeteria food purchase | 2 cafeterias | Prices of fruits, carrot and salad were lowered by about 50 % during the intervention and attractive signs promoting the target items at half price were placed; prices returned to normal after the intervention |
| 5 | Kristal et al. (1997)( 73 ) | Supermarket shoppers | Supermarket grocery purchase | 960 shoppers | Eight supermarkets were randomized to 2 groups; the intervention consisted of 3 components: (i) provision of supermarket flyers identifying fruits/vegetables on sale, recipes and menu ideas for using sale foods and a voucher of $US 0·50 for fruit/vegetable purchases; (ii) store signage to identify fruits/vegetables featured on flyer; and (iii) consciousness-raising activities (e.g. food demonstrations and nutrition-related signage); the control supermarkets remained the same |
| 6 | Anderson et al. (2001)( 74 ) | Low-income women | Farmers’ market produce purchase | 564 women | Participants were assigned to 4 groups: (i) education about the use, storage and nutritional value of fruits/vegetables; (ii) distribution of farmers’ market vouchers ($US 20); (iii) education plus vouchers; and (iv) no intervention |
| 7 | French et al. (2001)( 75 ) | Secondary-school students and employees | Vending machine purchase | 55 vending machines | Four pricing levels of low-fat snacks (0 %, 10 %, 25 %, 50 % discount) and 3 promotional conditions (none, low-fat label and low-fat label plus promotional sign) were crossed in a Latin square design |
| 8 | Bamberg (2002)( 76 ) | University students | Organic food purchase | 320 students | Participants were randomized to 4 groups: (i) a $US 7·50 voucher for organic food purchase; (ii) a stimulation message to form a specific plan when to act; (iii) voucher plus stimulation message; and (iv) no intervention |
| 9 | Hannan et al. (2002)( 77 ) | High-school students and employees | Cafeteria food purchase | 1 cafeteria | Prices on 3 high-fat food items popular with students (i.e. French fries, cookies and cheese sauce) were raised by about 10 %, and prices on 4 lower-fat items (i.e. fresh fruits, low-fat cookies, low-fat cereal bars and low-fat chips) were lowered approximately 25 % |
| 10 | Horgen and Brownell (2002)( 78 ) | Restaurant patrons | Restaurant food purchase | 1 restaurant | The restaurant had 3 consecutive interventions: (i) 20–30 % price discounts for a low-fat grilled chicken sandwich, a low-fat salad with grilled chicken and a low-fat vegetable soup; (ii) health messages; and (iii) price discounts plus health messages |
| 11 | Herman et al. (2006)( 79 ); Herman et al. (2008)( 80 ) | Low-income postpartum women | Fruit/vegetable intake | 602 postpartum women | Participants were assigned to 3 groups: (i) vouchers ($US 40/month) exchangeable for fresh fruits/vegetables in farmers’ market; (ii) vouchers ($US 40/month) exchangeable for fresh fruits/vegetables in supermarket; and (iii) control condition with a minimal non-food incentive |
| 12 | Burr et al. (2007)( 81 ) | Low-income pregnant women | Fruit intake | 190 pregnant women | Participants were randomized to 3 groups: (i) a control group who received usual care; (ii) an advice group given advice and leaflets promoting fruit and fruit juice consumption; and (iii) a voucher group given vouchers exchangeable for daily fruit juice delivered for free |
| 13 | Michels et al. (2008)( 82 ) | University students and employees | Cafeteria food purchase | 1 restaurant | Prices of healthier foods/dishes in cafeteria were reduced by 20 % and educational materials on current knowledge about the relationship between diet and health were distributed during the intervention; prices returned to normal after the intervention |
| 14 | Brown and Tammineni (2009)( 83 ) | Middle/high-school students | Vending machine purchase | 15 schools | Prices of healthier beverages in school vending machines were reduced by 10–25 %, healthier beverages were advertised on vending machine fronts and in school stores, and the types and proportions of healthier beverages were increased |
| 15 | Bihan et al. (2010)( 84 ); Bihan et al. (2012)( 85 ) | Low-income adults | Fruit/vegetable intake | 302 adults | Participants were randomized into 2 groups: (i) dietary advice alone; and (ii) dietary advice plus vouchers (€10–40/month) exchangeable for fresh fruit/vegetables |
| 16 | French et al. (2010)( 86 ); French et al. (2010)( 87 ) | Metropolitan transit workers | Vending machine purchase | 33 vending machines | The number of healthier items was increased to 50 % and prices were lowered by 10 % or more in the vending machines in 2 metropolitan bus garages; 2 control garages offered vending choices at usual availability and prices |
| 17 | Lowe et al. (2010)( 88 ) | Hospital and university employees | Cafeteria food purchase; food intake | 96 employees | Participants were randomly assigned to 2 groups: (i) environmental change only (i.e. introduction of new low-calorie foods and provision of labels for all foods sold); and (ii) environmental change plus 15–25 % price discount for low-calorie foods purchase and education about low-calorie eating |
| 18 | Ni Mhurchu et al. (2010)( 89 ); Blakely et al. (2011)( 90 ) | Supermarket shoppers | Supermarket grocery purchase | 1104 supermarket shoppers | Participants were randomly assigned to 4 groups: (i) 12·5 % price discount on healthier foods; (ii) tailored nutrition education; (iii) discount plus education; and (iv) no intervention |
| 19 | Kocken et al. (2012)( 91 ) | High-school students and employees | Vending machine purchase | 28 schools | Schools were randomly assigned to 2 groups; 3 consecutive interventions, (i) increasing the availability of lower-calorie products in vending machines, (ii) labelling products and (iii) reducing price of lower-calorie products, with phase 3 incorporating all 3 strategies, were introduced to the intervention schools; the control schools remained the same |
| 20 | An et al. (2013)( 92 ) | Health insurance plan members | Food intake | 351 319 HealthyFood participants | HealthyFood programme participants received 10–25 % price discounts for healthier food purchases in supermarkets; non-participants received no discount |
N/A, not applicable.
Table 2c.
Summary of studies included in a review of field experiments on the effectiveness of subsidies in promoting healthy food purchases and consumption: outcome measure, study results and intervention effectiveness
| Study ID | Reference | Outcome measure | Study results | Intervention effectiveness |
|---|---|---|---|---|
| 1 | Jeffery et al. (1994)( 69 ) | Objectively measured cafeteria sales; self-report food purchases | Fruit and salad purchases increased threefold during the intervention and largely returned to normal after the intervention | Combination of price discounts and increased availability effective in fruit and salad consumption |
| Women and those trying to control weight were most responsive to the intervention | ||||
| 2 | Paine-Andrews et al. (1996)( 70 ) | Objectively measured supermarket sales | The combination of prompting, product sampling and price discount was associated with low to moderate increases in the purchases of low-fat milk, salad dressings and frozen desserts | Combination of prompting, product sampling and price discounts effective in low-fat food consumption |
| 3 | French et al. (1997)( 71 ) | Objectively measured vending machine sales | The ratio of low-fat snacks to total purchases increased from 25·7 % to 45·8 % during the intervention and decreased to 22·8 % after the intervention | Price discount effective in low-fat snacks consumption |
| 4 | French et al. (1997)( 72 ) | Objectively measured cafeteria sales | Fruit and carrot sales increased approximately fourfold and twofold during the intervention, respectively | Price discount effective in fruit and carrot consumption |
| No significant effects on salad sales | ||||
| 5 | Kristal et al. (1997)( 73 ) | Self-report fruit/vegetable intake | No evidence was found that the intervention increased shoppers’ consumption of fruits and vegetables | Larger financial incentive needed to induce shoppers to purchase more fruits/vegetables |
| 6 | Anderson et al. (2001)( 74 ) | Self-report fruit/vegetable intake; objectively measured voucher | Both vouchers and education were associated with significant increase in fruit/vegetable intake | Both vouchers and education effective in fruit/vegetable consumption; combination most |
| redemption | Maximum impact of the intervention was achieved through a combination of vouchers and education | effective | ||
| 7 | French et al. (2001)( 75 ) | Objectively measured vending machine sales | Price discounts of 10 %, 25 % and 50 % on low-fat snacks were associated with increases in the percentages of low-fat snack sales by 9 %, 39 % and 93 %, respectively | Price discount effective in fruit and carrot consumption; promotional signage marginally effective |
| Promotional signage was independently but weakly associated with increases in low-fat snack sales | ||||
| Average profits per machine were not affected by intervention | ||||
| 8 | Bamberg (2002)( 76 ) | Objectively measured voucher redemption | Vouchers, stimulation message and a combination of both were all associated with higher probability of organic produce purchases compared with no intervention | Both vouchers and stimulation message effective in organic produce consumption |
| The difference in effectiveness of the 3 interventions was not statistically significant | ||||
| 9 | Hannan et al. (2002)( 77 ) | Objectively measured cafeteria | Fresh fruit sales increased throughout the intervention | Revenue-neutral pricing (i.e. using revenue from |
| sales | Sales of low-fat cookies/chips increased but later declined | taxing less-healthy food to subsidize healthier food purchase) effective in improving diet quality | ||
| Sales of low-fat cereal bars remained stable | ||||
| Four high-fat foods each showed a slow decline in sales | ||||
| 10 | Horgen and Brownell (2002)( 78 ) | Objectively measured restaurant sales | Price discount alone, rather than a combination of price discount and health messages, was associated with increased purchases of healthier food items relative to control items | Price discounts but not health messages effective in healthier food consumption |
| 11 | Herman et al. (2006)( 79 ); Herman et al. (2008)( 80 ) | Self-report fruit/vegetable intake | Fruit and vegetable consumption increased significantly among both the farmers’ market participants (0·33 servings/1000 kJ) and the voucher group (0·19 servings/1000 kJ) | Vouchers effective in fruit/vegetable consumption |
| 12 | Michels et al. (2008)( 82 ) | Self-report fruit/juice intake; clinically measured β-carotene concentration | Consumption of fruit juice and serum β-carotene concentration increased substantially in the voucher group | Vouchers but not education effective in fruit juice consumption |
| Education had no effect on fruit consumption | ||||
| 13 | Burr et al. (2007)( 81 ) | Objectively measured restaurant sales | Healthier food sales increased by 6 % and less-healthy food sales decreased by 2 % during the intervention | Price discounts effective in healthier food consumption with effect maintained beyond |
| After the intervention, healthier food sales increased further to 17 %, and a 2 % decline in less-healthy food sales persisted | promotion period | |||
| 14 | Brown and Tammineni (2009)( 83 ) | Objectively measured vending machine sales | Sales of soft drinks decreased and sales of healthier beverages increased during the intervention | Combination of price discounts, passive marketing and increased availability effective in healthier |
| Total profits increased for a majority of schools during the intervention | beverage consumption | |||
| 15 | Bihan et al. (2010)( 84 ); Bihan et al. (2012)( 85 ) | Self-report fruit/vegetable consumption; clinically measured vitamin intake | Fruit/vegetable consumption increased significantly in both the advice (0·62 times/d) and the voucher group (0·74 times/d) | Both vouchers and dietary advice effective in fruit/vegetable consumption |
| Participants in the voucher group had significantly decreased risk of low fruit/vegetable consumption relative to the advice group | ||||
| No change in vitamin C and β-carotene concentration | ||||
| 16 | French et al. (2010)( 86 ); French et al. (2010)( 87 ) | Objectively measured vending machine sales | Increases in availability (50 %) and price discounts (approximately 31 %) were associated with 10–42 % higher sales of healthier items | Combination of price discounts and increased availability effective in healthier food consumption |
| 17 | Lowe et al. (2010)( 88 ) | Objectively measured cafeteria | No difference between groups in total energy intake | Both price discounts and labeling effective in |
| sales; self-report food intake | %E from fat decreased and %E from carbohydrate increased for both groups, and the change remained significant after intervention | low-calorie food consumption | ||
| 18 | Ni Mhurchu et al. (2010)( 89 ); Blakely et al. (2011)( 90 ) | Objectively measured nutrients purchased; objectively measured healthier food | Price discounts were associated with increase in healthier food purchases by 11 % during the intervention and 5 % after the intervention | Price discounts but not education effective in healthier food consumption |
| purchases | Education had no effect on food purchases | |||
| Neither price discounts nor tailored nutrition education had a significant effect on nutrients purchased | ||||
| 19 | Kocken et al. (2012)( 91 ) | Objectively measured vending machine sales | Availability, labelling and price discounts raised the proportional sales of low-calorie drinks and reduced those of high-calorie foods | Combination of price discount, increased availability and labelling effective in healthier food consumption |
| Labelling alone had no effect on food and drink purchases | ||||
| 20 | An et al. (2013)( 92 ) | Self-report fruit/vegetable consumption | Participants consumed more fruit/vegetables and wholegrain foods, and less high sugar/salt foods, fried foods, processed meats and fast foods, relative to non-participants | Price discounts effective in healthier food consumption |
%E, percentage of energy.
Table 2a.
Summary of studies included in a review of field experiments on the effectiveness of subsidies in promoting healthy food purchases and consumption: intervention country, intervention duration, follow-up duration, study design, eligible item and intervention environment
| Study ID | Reference | Intervention country | Intervention duration (weeks) | Follow-up duration (weeks) | Study design | Economic incentive | Eligible item | Intervention environment |
|---|---|---|---|---|---|---|---|---|
| 1 | Jeffery et al. (1994)( 69 ) | USA | 3 | 3 | Pre–post | Price discount | Fruits, salad | University cafeteria |
| 2 | Paine-Andrews et al. (1996)( 70 ) | USA | 9·5 h | 0 | Pre–post | Price discount | Low-fat milk, low-fat salad dressings, low-fat frozen desserts | Supermarket |
| 3 | French et al. (1997)( 71 ) | USA | 4 | 3 | Pre–post | Price discount | Low-fat snacks | University |
| 4 | French et al. (1997)( 72 ) | USA | 3 | 3 | Pre–post | Price discount | Fruits, carrot, salad | High-school cafeteria |
| 5 | Kristal et al. (1997)( 73 ) | USA | 32 | 0 | RCT | Voucher | Fruits/vegetables | Supermarket |
| 6 | Anderson et al. (2001)( 74 ) | USA | 8 | 0 | Cohort | Voucher | Fruits/vegetables | Farmers’ market |
| 7 | French et al. (2001)( 75 ) | USA | 48 | 0 | RCT | Price discount | Low-fat snacks | Secondary school, worksite |
| 8 | Bamberg (2002)( 76 ) | Germany | 1 | 0 | RCT | Voucher | Organic fruits/vegetables | Organic food store |
| 9 | Hannan et al. (2002)( 77 ) | USA | 31 | 0 | Pre–post | Price discount | Fresh fruits, low-fat cookies, low-fat cereal bars, low-fat chips | High-school cafeteria |
| 10 | Horgen and Brownell (2002)( 78 ) | USA | 16 | 0 | Pre–post | Price discount | Low-fat chicken sandwich, low-fat salad, vegetable soup | Restaurant |
| 11 | Herman et al. (2006)( 79 ); Herman et al. (2008)( 80 ) | USA | 24 | 24 | Cohort | Voucher | Fresh fruits/vegetables | Supermarket, farmers’ market |
| 12 | Burr et al. (2007)( 81 ) | UK | 32 | 0 | RCT | Voucher | 100 % orange juice | Home |
| 13 | Michels et al. (2008)( 82 ) | USA | 5 | 5 | Pre–post | Price discount | Healthier foods | University cafeteria |
| 14 | Brown and Tammineni (2009)( 83 ) | USA | 40 | 0 | Pre–post | Price discount | Healthier beverages | Middle/high school |
| 15 | Bihan et al. (2010)( 84 ); Bihan et al. (2012)( 85 ) | France | 48 | 0 | RCT | Voucher | Fresh fruits/vegetables | Supermarket |
| 16 | French et al. (2010)( 86 ); French et al. (2010)( 87 ) | USA | 72 | 0 | RCT | Price discount | Healthier foods and drinks | Worksite |
| 17 | Lowe et al. (2010)( 88 ) | USA | 12 | 36 | RCT | Price discount | Low-calorie foods | Hospital cafeteria |
| 18 | Ni Mhurchu et al. (2010)( 89 ); Blakely et al. (2011)( 90 ) | New Zealand | 24 | 24 | RCT | Price discount | Healthier foods | Supermarket |
| 19 | Kocken et al. (2012)( 91 ) | Netherlands | 18 | 0 | RCT | Price discount | Low-calorie foods and drinks | High school |
| 20 | An et al. (2013)( 92 ) | South Africa | 132 | 0 | Cohort | Price discount | Healthier foods | Supermarket |
RCT, randomized controlled trial.
Intervention effectiveness
All but one study found subsidies on healthier foods to significantly increase the purchase and consumption of promoted products. The only null finding, reported in Kristal et al., was likely due to its small financial incentive – a voucher worth $US 0·50 towards the purchase of any fruit or vegetable( 73 ). As the authors noted in their conclusion, ‘more powerful interventions are probably necessary to induce shoppers to purchase and consume more fruits and vegetables’.
The level of subsidies varied substantially across interventions. The price discounts ranged from 10 % to 50 %, and the monetary values of vouchers were largely between $US 7·50 and $US 50, except for the $0·50 voucher in Kristal et al.( 73 ). The lower bounds (i.e. 10 % price discount and $US 7·50 voucher) could serve as a conservative estimate for the minimal level of subsidies required to induce a meaningful increase in healthier food purchases or consumption.
There is some preliminary evidence from price discount interventions that the demands for fruits and low-fat snacks are price elastic – a 1 % decrease in price is associated with a larger than 1 % increase in quantity demanded. Jeffery et al. documented a twofold increase of fruit purchases in a university cafeteria when price was reduced by half( 69 ). French et al. reported that the fruit sales in high-school cafeterias increased fourfold following a 50 % price reduction( 72 ). Lowe et al. reported an increase of fruit intake by about 30 % in hospital cafeterias when price was lowered by 15–25 %( 88 ). French et al. found a 50 % price reduction for low-fat snacks sold in university vending machines to be associated with a 78 % increase in sales( 71 ). French et al. reported a fourfold increase in sales of low-fat snacks sold in worksite vending machines when prices decreased by 50 %( 86 ). Evidence for price elasticities of other foods is less consistent. For example, given a 50 % price reduction of salad sold in cafeterias, Jeffery et al. documented a twofold increase in sales( 69 ) while French et al. reported none( 72 ).
Most studies adopted a fixed subsidy level that did not vary across groups or over time, so that the dose–response relationship could not be examined. Two exceptions were French et al. and An et al., which both confirmed a dose–response relationship between the level of price discount and sales/consumption of subsidized foods. In French et al., price reductions of 10 %, 25 % and 50 % on low-fat snacks sold in school and worksite vending machines were associated with an increase in sales by 9 %, 39 % and 93 %, respectively( 75 ). An et al. reported that 10 % and 25 % discounts on healthier food purchases were associated with an increase in daily fruit/vegetable intake by 0·38 and 0·64 servings, respectively( 92 ).
Evidence on the differential effect of subsidies across different populations remains sparse. Blakely et al. is the only study that examined the differential effect of price discount on food purchases across ethnic and socio-economic groups( 90 ). No variation in intervention effect was identified by household income or education, and the evidence for differential effects of price discounts across ethnicities was weak.
A few studies compared subsidies with alternative intervention strategies, namely nutrition education, product labelling, promotional signage (e.g. posters in cafeteria) and stimulation (i.e. a text message to remind/encourage action) or health message (i.e. a text message to introduce the health benefit of nutritious food intake). The results are largely inconclusive. Anderson et al.( 74 ) and Bihan et al.( 84 , 85 ) found that vouchers and nutrition education both increased fruit and vegetable consumption significantly (with similar effect sizes), and Anderson et al. reported that combination of the two had the largest effect. Conversely, Burr et al.( 81 ), Ni Mhurchu et al.( 89 ) and Blakely et al.( 90 ) found no impact of nutrition education on fruit or other healthier food purchases. No effects on healthier food sales were found for health message( 78 ), and some but limited effects were reported for product labelling( 88 , 91 ), promotional signage( 75 ) and stimulation message( 76 ).
Seven interventions included a follow-up period to assess changes in dietary behaviour after the withdrawal of incentives, but their findings diverged. Three found sustained improvement after the intervention – the effect remained the same in the 6-month follow-up reported in Herman et al.( 79 , 80 ), increased by about twofold in the 5-week follow-up in Michels et al.( 82 ) and decreased by half in the 6-month follow-up in Ni Mhurchu et al.( 89 ). Conversely, the other four interventions( 69 , 71 , 72 , 88 ) found no extended effect in the follow-up period.
Study quality
Table 3 reports the results of study quality assessment. On average, studies included in the review met six out of ten quality criteria, but the distribution of qualification differed substantially across criteria. Almost all studies included an objective measure of food purchases or intake, used a measurement tool that was shown to be reliable and valid in previously published studies, and documented intervention procedures in detail. In contrast, nearly none recruited participants randomly with a response rate of 60 % or higher.
Table 3.
Quality assessment of studies included in a review of field experiments on the effectiveness of subsidies in promoting healthy food purchases and consumption
| Item | Criterion of study quality | Mean | sd |
|---|---|---|---|
| 1 | A control group was included | 0·60 | 0·50 |
| 2 | Baseline characteristics between control and intervention groups were similar | 0·25 | 0·44 |
| 3 | The intervention period was at least 5 weeks | 0·75 | 0·44 |
| 4 | The follow-up period was at least 3 weeks | 0·35 | 0·49 |
| 5 | An objective measure of food purchases or intake was used | 0·90 | 0·31 |
| 6 | The measurement tool was shown to be reliable and valid in previously published studies | 0·95 | 0·23 |
| 7 | Participants were randomly recruited with a response rate of 60 % or higher | 0·05 | 0·22 |
| 8 | Attrition was analysed and determined not to differ significantly by respondents’ baseline characteristics between control and intervention groups | 0·35 | 0·49 |
| 9 | Potential confounders were properly controlled for in the analysis | 0·50 | 0·51 |
| 10 | Intervention procedures were documented in detail in the article | 0·90 | 0·31 |
| 11 | Total study quality score by summing up items 1 to 10 | 5·60 | 1·90 |
Note: Items 1 to 10 are all dichotomous variables.
Discussion
The high price of nutrient-rich, low-energy-dense foods relative to nutrient-poor, energy-dense foods might prevent individuals, especially those who have low income, from adopting a healthier diet. In the present study, we systematically reviewed evidence from field interventions on the effectiveness of monetary subsidies in promoting healthier food purchases and consumption. Improved affordability was associated with significant increases in the purchase and consumption of healthier foods.
Economic theory suggests that when the price of healthy diets drops, individuals will substitute healthy foods for unhealthy ones, but as their real income increases due to price reduction, they may spend more on food overall, including unhealthy foods. Among the interventions included in the present review, the amount of subsidies relative to personal income appears to be small. In this case, the income effect is unlikely to play a major role, and the study estimates suggest an unambiguous effect on improved patterns of healthier food purchases and consumption.
The evidence on the effectiveness of subsidies is to some extent compromised by a few major limitations in the reviewed studies. Arguably, the biggest limitation is the external validity of study outcomes. Almost all studies included in the review were limited in scale, had a small or convenience sample rather than a population-representative sample, and were implemented in very specific settings (e.g. one or a few supermarkets, cafeterias, vending machines, farmers’ markets or restaurants), which have substantially limited the generalizability of study results beyond the sample. Moreover, the intervention duration was usually limited to a few weeks and a majority of the studies did not incorporate a follow-up period after the intervention. Therefore, the long-term trends and effectiveness of subsidies cannot be evaluated and whether the effect will sustain after the withdrawal of incentive remains questionable. Separating the effects of subsidies from those of other intervention elements (e.g. prompting, product sampling, increasing the number of healthier food choices) was often infeasible due to the integrated study design. Policy makers are not well informed of the potential for large-scale application of subsidies on healthier foods because none of the reviewed studies explicitly measured cost-effectiveness of the interventions or evaluated the potential impact on the food industry. No study targeted overall diet quality and thus little is known about the impact of subsidies on total diet/energy intake.
In addition to weaknesses of the individual studies, the review itself also suffers from various limitations. Studies included in the review differed substantially by study population, intervention setting, experimental design and outcome measure, which precluded meta-analysis. Only a small proportion of the reviewed studies examined each predefined research question, resulting in a wide range of uncertainties. The literature search was restricted to peer-reviewed journal articles in English published between 1990 and 2012. Although this restriction may potentially increase the likelihood of obtaining concurrent studies with reasonably high quality, publication bias can be a concern. The review exclusively focused on one specific type of economic incentive, namely subsidies in the form of price discounts and vouchers for healthier food purchases, while other forms of economic incentives, such as taxes on less-healthy foods, food stamps for basic necessities or rewards for weight loss, were not examined. Readers interested in the role of taxation in modifying dietary behaviour may refer to the review articles by Caraher and Cowburn( 93 ), Kim and Kawachi( 94 ) and Brownell et al.( 12 ).
The present study confirms findings on the effectiveness of economic incentives in modifying health behaviours from previous review articles. Kane et al.'s meta-analysis of forty-seven RCT estimated that the economic incentives, on average, worked 73 % of the time to improve consumers’ preventive health behaviours( 15 ). All four RCT reviewed in Wall et al. documented a positive effect of monetary incentives on food purchases, food consumption or weight loss( 16 ). Thow et al. reviewed twenty-four relevant studies and concluded that a substantial subsidy or tax on food was likely to influence consumption and improve health( 17 ). Jensen et al. reviewed evidence from thirty articles and found price incentives to be effective for altering children's food and beverage intake at school( 18 ).
Despite the accumulated evidence on the effectiveness of economic incentives in modifying dietary behaviour, policy adoptions remain scarce. Hungary and Denmark are the only countries so far that have imposed a fat tax( 10 , 11 ). In the USA, since the snack food tax in Maine and the District of Columbia was repealed in 2000 and 2001, respectively, no states currently levy taxes on snacks( 94 ). Although a majority of US states have adopted a soft drink tax( 12 ), the tax rate is believed to be too small to induce a meaningful change in beverage consumption( 95 ), and no tax revenue is earmarked for subsidizing healthier food purchases or physical activity programmes( 96 ). Besides the opposition against targeted subsidies and taxation of foods from the food industry( 93 ), concerns on the unintended consequences of these policies may also contribute to the slow and reluctant adoption of economic incentives in improving diet quality( 94 ). For example, a fat tax could be regressive for low-income populations who spend a higher proportion of income on food and consume more energy-dense foods. Although subsidies on low-fat foods are generally observed to increase sales and consumption of those products, improved health outcomes might not be achieved if higher consumption of low-fat foods leads to an increase in total energy intake.
Further research is warranted to advance knowledge about the role of subsidies and other economic incentives in modifying dietary behaviour. Based on the limitations of existing literature, future studies should aim to improve several aspects. A sufficiently large and representative sample should be used to obtain more precise estimates at the population level and facilitate subgroup comparison. More rigorous experimental designs, such as RCT, should be adopted to clearly demonstrate causal effects and prevent contamination of potential confounders. Overall food purchases and total diet/energy intake, in addition to that of the subsidized foods, need to be carefully documented to detect any unintended consequences. Finally, the experiment and follow-up periods need to be sufficiently long to assess the evolution and long-term effectiveness and cost-effectiveness of the intervention.
Conclusions
Subsidizing healthier foods tends to be effective in modifying dietary behaviour. Even so, existing evidence is compromised due to various study limitations: the small and convenience samples of the interventions obscure the generalizability of study results; the absence of overall diet assessment questions the effectiveness in reducing total energy intake; the short intervention and follow-up durations do not allow assessment of long-term impact; and the lack of cost-effectiveness analysis precludes comparison across competing policy scenarios. Future studies are warranted to address those limitations and examine the long-term effectiveness and cost-effectiveness of economic incentives at the population level.
Acknowledgements
Source of funding: This study was funded by the National Cancer Institute (grant no. R21CA161287), the National Institute of Child Health & Human Development (grant no. R21HD071568), and the Anne and James Rothenberg Dissertation Award 2011–2012. Conflicts of interest: The author has no conflicts of interest relating to this manuscript. Acknowledgements: The author thanks Roland Sturm, Susanne Hempel, Roberta Shanman and Christina Huang for their helpful comments and generous assistance in study design and data acquisition.
References
- 1. US Department of Agriculture & US Department of Health and Human Services (2010) Dietary Guidelines for Americans 2010, 7th ed. Washington, DC: US Government Printing Office; available at http://www.health.gov/dietaryguidelines/dga2010/dietaryguidelines2010.pdf [Google Scholar]
- 2. National Prevention Council (2011) National Prevention Strategy. Washington, DC: US Department of Health and Human Services, Office of the Surgeon General; available at http://www.healthcare.gov/prevention/nphpphc/strategy/report.pdf [Google Scholar]
- 3. Darmon N & Drewnowski A (2008) Does social class predict diet quality? Am J Clin Nutr 87, 1107–1117. [DOI] [PubMed] [Google Scholar]
- 4. Monsivais P & Drewnowski A (2007) The rising cost of low-energy-density foods. J Am Diet Assoc 107, 2071–2076. [DOI] [PubMed] [Google Scholar]
- 5. Drewnowski A & Specter SE (2004) Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr 79, 6–16. [DOI] [PubMed] [Google Scholar]
- 6. Drewnowski A & Darmon N (2005) The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr 82, 1 Suppl., 265S–273S. [DOI] [PubMed] [Google Scholar]
- 7. Drewnowski A (2010) The cost of US foods as related to their nutritive value. Am J Clin Nutr 92, 1181–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. World Health Organization (2004) Global strategy on diet, physical activity and health. http://apps.who.int/gb/ebwha/pdf_files/WHA57/A57_R17-en.pdf (accessed May 2012).
- 9. World Health Organization (2008) 2008–2013 Action plan for the global strategy for the prevention and control of noncommunicable diseases. http://whqlibdoc.who.int/publications/2009/9789241597418_eng.pdf (accessed May 2012).
- 10. Cheney C (2011) Battling the couch potatoes, Hungary introduces ‘fat tax’. http://www.spiegel.de/international/europe/battling-the-couch-potatoes-hungary-introduces-fat-tax-a-783862.html (accessed May 2012).
- 11. US Department of Agriculture, Foreign Agricultural Service (2011) Danish fat tax on food. http://gain.fas.usda.gov/Recent%20GAIN%20Publications/Danish%20Fat%20Tax%20on%20Food_Stockholm_Denmark_10-6-2011.pdf (accessed May 2012).
- 12. Brownell KD, Farley T, Willett WC et al. (2009) The public health and economic benefits of taxing sugar-sweetened beverages. N Engl J Med 361, 1599–1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. US Senate and House of Representatives (2008) Food, Conservation, and Energy Act of 2008. http://www.usda.gov/documents/Bill_6124.pdf (accessed May 2012).
- 14. US Department of Agriculture (2012) Healthy Incentives Pilot. http://www.fns.usda.gov/snap/hip/ (accessed May 2012).
- 15. Kane RL, Johnson PE, Town RJ et al. (2004) A structured review of the effect of economic incentives on consumers’ preventive behavior. Am J Prev Med 27, 327–352. [DOI] [PubMed] [Google Scholar]
- 16. Wall J, Mhurchu CN, Blakely T et al. (2006) Effectiveness of monetary incentives in modifying dietary behavior: a review of randomized, controlled trials. Nutr Rev 64, 518–531. [DOI] [PubMed] [Google Scholar]
- 17. Thow AM, Jan S, Leeder S et al. (2010) The effect of fiscal policy on diet, obesity and chronic disease: a systematic review. Bull World Health Organ 88, 609–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jensen JD, Hartmann H, de Mul A et al. (2011) Economic incentives and nutritional behavior of children in the school setting: a systematic review. Nutr Rev 69, 660–674. [DOI] [PubMed] [Google Scholar]
- 19. Wu S, Cohen D, Shi Y et al. (2011) Economic analysis of physical activity interventions. Am J Prev Med 40, 149–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Epstein LH, Dearing KK, Handley EA et al. (2006) Relationship of mother and child food purchases as a function of price: a pilot study. Appetite 47, 115–118. [DOI] [PubMed] [Google Scholar]
- 21. Epstein LH, Handley EA, Dearing KK et al. (2006) Purchases of food in youth. Influence of price and income. Psychol Sci 17, 82–89. [DOI] [PubMed] [Google Scholar]
- 22. Epstein LH, Dearing KK, Paluch RA et al. (2007) Price and maternal obesity influence purchasing of low- and high-energy-dense foods. Am J Clin Nutr 86, 914–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Epstein LH, Dearing KK, Roba LG et al. (2010) The influence of taxes and subsidies on energy purchased in an experimental purchasing study. Psychol Sci 21, 406–414. [DOI] [PubMed] [Google Scholar]
- 24. Giesen JC, Havermans RC, Nederkoorn C et al. (2012) Impulsivity in the supermarket. Responses to calorie taxes and subsidies in healthy weight undergraduates. Appetite 58, 6–10. [DOI] [PubMed] [Google Scholar]
- 25. Waterlander WE, Steenhuis IH, de Boer MR et al. (2012) The effects of a 25% discount on fruits and vegetables: results of a randomized trial in a three-dimensional web-based supermarket. Int J Behav Nutr Phys Act 9, 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Waterlander WE, Steenhuis IH, de Boer MR et al. (2012) Introducing taxes, subsidies or both: the effects of various food pricing strategies in a web-based supermarket randomized trial. Prev Med 54, 323–330. [DOI] [PubMed] [Google Scholar]
- 27. Cash SB, Sunding DL & Zilberman D (2005) Fat taxes and thin subsidies: prices, diet, and health outcomes. Acta Agric Scand Sect C 2, 167–174. [Google Scholar]
- 28. Jensen JD & Smed S (2007) Cost-effective design of economic instruments in nutrition policy. Int J Behav Nutr Phys Act 4, 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lin B, Yen ST, Dong D et al. (2010) Economic incentives for dietary improvement among food stamp recipients. Contemp Econ Policy 28, 524–536. [Google Scholar]
- 30. Smed S, Jensen JD & Denver S (2007) Socio-economic characteristics and the effect of taxation as a health policy instrument. Food Policy 32, 624–639. [Google Scholar]
- 31. Yaniv G, Rosin O & Tobol Y (2009) Junk-food, home cooking, physical activity and obesity: the effect of the fat tax and the thin subsidy. J Public Econ 93, 823–830. [Google Scholar]
- 32. Nordström J & Thunström L (2011) Can targeted food taxes and subsidies improve the diet? Distributional effects among income groups. Food Policy 36, 259–271. [Google Scholar]
- 33. Lowe CF, Horne PJ, Tapper K et al. (2004) Effects of a peer modeling and rewards-based intervention to increase fruit and vegetable consumption in children. Eur J Clin Nutr 58, 510–522. [DOI] [PubMed] [Google Scholar]
- 34. Ponza M, Devaney B, Ziegler P et al. (2004) Nutrient intakes and food choices of infants and toddlers participating in WIC. J Am Diet Assoc 104, 1 Suppl. 1, S71–S79. [DOI] [PubMed] [Google Scholar]
- 35. Siega-Riz AM, Kranz S, Blanchette D et al. (2004) The effect of participation in the WIC program on preschoolers’ diets. J Pediatr 144, 229–234. [DOI] [PubMed] [Google Scholar]
- 36. Nelson JA, Carpenter K & Chiasson MA (2006) Diet, activity, and overweight among preschool-age children enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Prev Chronic Dis 3, A49. [PMC free article] [PubMed] [Google Scholar]
- 37. Gentile DA, Welk G, Eisenmann JC et al. (2009) Evaluation of a multiple ecological level child obesity prevention program: Switch what you Do, View, and Chew. BMC Med 7, 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Horne PJ, Hardman CA, Lowe CF et al. (2009) Increasing parental provision and children's consumption of lunchbox fruit and vegetables in Ireland: the Food Dudes intervention. Eur J Clin Nutr 63, 613–618. [DOI] [PubMed] [Google Scholar]
- 39. Taren DL, Clark W, Chernesky M et al. (1990) Weekly food servings and participation in social programs among low income families. Am J Public Health 80, 1376–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Anliker JA, Winnie M & Drake LT (1992) An evaluation of the Connecticut Farmers’ Market coupon program. J Nutr Educ 24, 185–191. [Google Scholar]
- 41. Balsam A, Webber D & Oehlke B (1994) The farmers’ market coupon program for low-income elders. J Nutr Elder 13, 35–42. [DOI] [PubMed] [Google Scholar]
- 42. Perez-Escamilla R, Ferris AM, Drake L et al. (2000) Food stamps are associated with food security and dietary intake of inner-city preschoolers from Hartford, Connecticut. J Nutr 130, 2711–2717. [DOI] [PubMed] [Google Scholar]
- 43. Swensen AR, Harnack LJ & Ross JA (2001) Nutritional assessment of pregnant women enrolled in the Special Supplemental Program for Women, Infants, and Children (WIC). J Am Diet Assoc 101, 903–908. [DOI] [PubMed] [Google Scholar]
- 44. Kunkel ME, Luccia B & Moore AC (2003) Evaluation of the South Carolina seniors farmers’ market nutrition education program. J Am Diet Assoc 103, 880–883. [DOI] [PubMed] [Google Scholar]
- 45. Ard JD, Fitzpatrick S, Desmond RA et al. (2007) The impact of cost on the availability of fruits and vegetables in the homes of schoolchildren in Birmingham, Alabama. Am J Public Health 97, 367–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kropf ML, Holben DH, Holcomb JP et al. (2007) Food security status and produce intake and behaviors of Special Supplemental Nutrition Program for Women, Infants, and Children and Farmers’ Market Nutrition Program participants. J Am Diet Assoc 107, 1903–1908. [DOI] [PubMed] [Google Scholar]
- 47. Racine EF, Smith Vaughn A & Laditka SB (2010) Farmers’ market use among African-American women participating in the Special Supplemental Nutrition Program for Women, Infants, and Children. J Am Diet Assoc 110, 441–446. [DOI] [PubMed] [Google Scholar]
- 48. Freedman DA, Bell BA & Collins LV (2011) The Veggie Project: a case study of a multi-component farmers’ market intervention. J Prim Prev 32, 213–224. [DOI] [PubMed] [Google Scholar]
- 49. Johnson DB, Beaudoin S, Smith LT et al. (2004) Increasing fruit and vegetable intake in homebound elders: the Seattle Senior Farmers’ Market Nutrition Pilot Program. Prev Chronic Dis 1, A03. [PMC free article] [PubMed] [Google Scholar]
- 50. Bere E, Veierod MB & Klepp KI (2005) The Norwegian School Fruit Program: evaluating paid vs. no-cost subscriptions. Prev Med 41, 463–470. [DOI] [PubMed] [Google Scholar]
- 51. Bere E, Veierod MB, Bjelland M et al. (2006) Free school fruit – sustained effect 1 year later. Health Educ Res 21, 268–275. [DOI] [PubMed] [Google Scholar]
- 52. Bere E, Veierod MB, Skare O et al. (2007) Free school fruit – sustained effect three years later. Int J Behav Nutr Phys Act 4, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Jamelske E, Bica LA, McCarty DJ et al. (2008) Preliminary findings from an evaluation of the USDA Fresh Fruit and Vegetable Program in Wisconsin schools. WMJ 107, 225–230. [PubMed] [Google Scholar]
- 54. Cullen KW, Watson KB & Konarik M (2009) Differences in fruit and vegetable exposure and preferences among adolescents receiving free fruit and vegetable snacks at school. Appetite 52, 740–744. [DOI] [PubMed] [Google Scholar]
- 55. Lachat CK, Verstraeten R, De Meulenaer B et al. (2009) Availability of free fruits and vegetables at canteen lunch improves lunch and daily nutritional profiles: a randomized controlled trial. Br J Nutr 102, 1030–1037. [DOI] [PubMed] [Google Scholar]
- 56. Jeffery RW, Wing RR, Thorson C et al. (1993) Strengthening behavioral interventions for weight loss: a randomized trial of food provision and monetary incentives. J Consult Clin Psychol 61, 1038–1045. [DOI] [PubMed] [Google Scholar]
- 57. Jeffery RW & Wing RR (1995) Long-term effects of interventions for weight loss using food provision and monetary incentives. J Consult Clin Psychol 63, 793–796. [DOI] [PubMed] [Google Scholar]
- 58. Jeffery RW & French SA (1997) Preventing weight gain in adults: design, methods and one year results from the Pound of Prevention study. Int J Obes Relat Metab Disord 21, 457–464. [DOI] [PubMed] [Google Scholar]
- 59. Jeffery RW, Wing RR, Thorson C et al. (1998) Use of personal trainers and financial incentives to increase exercise in a behavioral weight-loss program. J Consult Clin Psychol 66, 777–783. [DOI] [PubMed] [Google Scholar]
- 60. Jeffery RW & French SA (1999) Preventing weight gain in adults: the pound of prevention study. Am J Public Health 89, 747–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Galal OM (2002) The nutrition transition in Egypt: obesity, undernutrition and the food consumption context. Public Health Nutr 5, 141–148. [DOI] [PubMed] [Google Scholar]
- 62. Jensen RT & Miller NH (2011) Do consumer price subsidies really improve nutrition? Rev Econ Stat 93, 1205–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Wing RR, Jeffery RW, Pronk N et al. (1996) Effects of a personal trainer and financial incentives on exercise adherence in overweight women in a behavioral weight loss program. Obes Res 4, 4 57–462. [DOI] [PubMed] [Google Scholar]
- 64. Finkelstein EA, Linnan LA, Tate DF et al. (2007) A pilot study testing the effect of different levels of financial incentives on weight loss among overweight employees. J Occup Environ Med 49, 981–989. [DOI] [PubMed] [Google Scholar]
- 65. Volpp KG, John LK, Troxel AB et al. (2008) Financial incentive-based approaches for weight loss: a randomized trial. JAMA 300, 2631–2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. John LK, Loewenstein G, Troxel AB et al. (2011) Financial incentives for extended weight loss: a randomized, controlled trial. J Gen Intern Med 26, 621–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Cinciripini PM (1984) Changing food selections in a public cafeteria. An applied behavior analysis. Behav Modif 8, 520–539. [Google Scholar]
- 68. Mayer JA, Brown TP, Heins JM et al. (1987) A multi-component intervention for modifying food selections in a worksite cafeteria. J Nutr Educ 19, 277–280. [Google Scholar]
- 69. Jeffery RW, French SA, Raether C et al. (1994) An environmental intervention to increase fruit and salad purchases in a cafeteria. Prev Med 23, 788–792. [DOI] [PubMed] [Google Scholar]
- 70. Paine-Andrews A, Francisco VT, Fawcett SB et al. (1996) Health marketing in the supermarket: using prompting, product sampling, and price reduction to increase customer purchases of lower-fat items. Health Mark Q 14, 85–99. [DOI] [PubMed] [Google Scholar]
- 71. French SA, Jeffery RW, Story M et al. (1997) A pricing strategy to promote low-fat snack choices through vending machines. Am J Public Health 87, 849–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. French SA, Story M, Jeffery RW et al. (1997) Pricing strategy to promote fruit and vegetable purchase in high school cafeterias. J Am Diet Assoc 97, 1008–1010. [DOI] [PubMed] [Google Scholar]
- 73. Kristal AR, Goldenhar L, Muldoon J et al. (1997) Evaluation of a supermarket intervention to increase consumption of fruits and vegetables. Am J Health Promot 11, 422–425. [DOI] [PubMed] [Google Scholar]
- 74. Anderson JV, Bybee DI, Brown RM et al. (2001) 5 a day fruit and vegetable intervention improves consumption in a low income population. J Am Diet Assoc 101, 195–202. [DOI] [PubMed] [Google Scholar]
- 75. French SA, Jeffery RW, Story M et al. (2001) Pricing and promotion effects on low-fat vending snack purchases: the CHIPS Study. Am J Public Health 91, 112–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Bamberg S (2002) Implementation intention versus monetary incentive comparing the effects of interventions to promote the purchase of organically produced food. J Econ Psychcol 23, 573–587. [Google Scholar]
- 77. Hannan P, French SA, Story M et al. (2002) A pricing strategy to promote sales of lower fat foods in high school cafeterias: acceptability and sensitivity analysis. Am J Health Promot 17, 1–6. [DOI] [PubMed] [Google Scholar]
- 78. Horgen KB & Brownell KD (2002) Comparison of price change and health message interventions in promoting healthy food choices. Health Psychol 21, 505–512. [DOI] [PubMed] [Google Scholar]
- 79. Herman DR, Harrison GG & Jenks E (2006) Choices made by low-income women provided with an economic supplement for fresh fruit and vegetable purchase. J Am Diet Assoc 106, 740–744. [DOI] [PubMed] [Google Scholar]
- 80. Herman DR, Harrison GG, Afifi AA et al. (2008) Effect of a targeted subsidy on intake of fruits and vegetables among low-income women in the Special Supplemental Nutrition Program for Women, Infants, and Children. Am J Public Health 98, 98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Burr ML, Trembeth J, Jones KB et al. (2007) The effects of dietary advice and vouchers on the intake of fruit and fruit juice by pregnant women in a deprived area: a controlled trial. Public Health Nutr 10, 559–565. [DOI] [PubMed] [Google Scholar]
- 82. Michels KB, Bloom BR, Riccardi P et al. (2008) A study of the importance of education and cost incentives on individual food choices at the Harvard School of Public Health cafeteria. J Am Coll Nutr 27, 6–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Brown DM & Tammineni SK (2009) Managing sales of beverages in schools to preserve profits and improve children's nutrition intake in 15 Mississippi schools. J Am Diet Assoc 109, 2036–2042. [DOI] [PubMed] [Google Scholar]
- 84. Bihan H, Castetbon K, Mejean C et al. (2010) Sociodemographic factors and attitudes toward food affordability and health are associated with fruit and vegetable consumption in a low-income French population. J Nutr 140, 823–830. [DOI] [PubMed] [Google Scholar]
- 85. Bihan H, Mejean C, Castetbon K et al. (2012) Impact of fruit and vegetable vouchers and dietary advice on fruit and vegetable intake in a low-income population. Eur J Clin Nutr 66, 369–375. [DOI] [PubMed] [Google Scholar]
- 86. French SA, Hannan PJ, Harnack LJ et al. (2010) Pricing and availability intervention in vending machines at four bus garages. J Occup Environ Med 52, Suppl. 1, S29–S33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. French SA, Harnack LJ, Hannan PJ et al. (2010) Worksite environment intervention to prevent obesity among metropolitan transit workers. Prev Med 50, 180–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Lowe MR, Tappe KA, Butryn ML et al. (2010) An intervention study targeting energy and nutrient intake in worksite cafeterias. Eat Behav 11, 144–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Ni Mhurchu C, Blakely T, Jiang Y et al. (2010) Effects of price discounts and tailored nutrition education on supermarket purchases: a randomized controlled trial. Am J Clin Nutr 91, 736–747. [DOI] [PubMed] [Google Scholar]
- 90. Blakely T, Ni Mhurchu C, Jiang Y et al. (2011) Do effects of price discounts and nutrition education on food purchases vary by ethnicity, income and education? Results from a randomized, controlled trial. J Epidemiol Community Health 65, 902–908. [DOI] [PubMed] [Google Scholar]
- 91. Kocken PL, Eeuwijk J, Van Kesteren NM et al. (2012) Promoting the purchase of low-calorie foods from school vending machines: a cluster-randomized controlled study. J Sch Health 82, 115–122. [DOI] [PubMed] [Google Scholar]
- 92. An R, Patel D, Segal D et al. (2013) Eating better for less: a national discount program for healthy food purchases in South Africa. Am J Health Behav 37, 56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Caraher M & Cowburn G (2005) Taxing food: implications for public health nutrition. Public Health Nutr 8, 1242–1249. [DOI] [PubMed] [Google Scholar]
- 94. Kim D & Kawachi I (2006) Food taxation and pricing strategies to ‘thin out’ the obesity epidemic. Am J Prev Med 30, 430–437. [DOI] [PubMed] [Google Scholar]
- 95. Sturm R, Powell LM, Chriqui JF et al. (2010) Soda taxes, soft drink consumption, and children's body mass index. Health Aff (Millwood) 29, 1052–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Jacobson MF & Brownell KD (2000) Small taxes on soft drinks and snack foods to promote health. Am J Public Health 90, 854–857. [DOI] [PMC free article] [PubMed] [Google Scholar]