Abstract
The problem of poor regulatory compliance has been widely reported across private health providers in developing countries. Less known are the underlying reasons for poor compliance, especially with regards to the roles played by front-line regulatory staff, and the regulatory institution as a whole. We designed a qualitative study to address this gap, with the study questions and tools drawing on a conceptual framework informed by theoretical literature on regulation. Data were collected from specialized drug shops (SDSs) in two rural districts in Western Kenya in 2011 through eight focus group discussions, and from regulatory staff from organizations governing the pharmaceutical sector through a total of 24 in-depth interviews.
We found that relationships between front-line regulators and SDS operators were a strong influence on regulatory behaviour, often resulting in non-compliance and perverse outcomes such as corruption. It emerged that separate regulatory streams operated in urban and rural locations, based mainly on differing relationships between the front-line regulators and SDS operators, and on broader factors such as the competition environment and community expectations. Effective incentive structures for regulatory staff were either absent, or poorly linked to performance in regulatory organizations, resulting in divergences between the purposes of the regulatory organization and activities of front-line staff.
Given the rural-urban differences in the practice environment, the introduction of lower retail practice requirements for rural SDSs could be considered. This would allow illegally operated shops to be brought within the regulatory framework, facilitating good quality provision of essential commodities to marginalized areas, without lowering the practice requirements for the better complying urban SDSs. In addition, regulatory organizations need to devise incentives that better link the level of effort to rewards such as professional advancement of regulatory staff.
Keywords: Pharmaceutical services, Medicine retailer, Regulation, Private sector, Kenya
Highlights
-
•
Study explored relationships between regulators and drug shop operators in Kenya.
-
•
Regulatory behaviour of drug shops depended on relationships between operators and regulators.
-
•
The relationships varied depending on the cadre of the regulator and shop location.
-
•
The relationship complexities resulted in corruption and regulatory non-compliance.
-
•
Policy should consider linking regulatory requirements to geographical location of shops.
Introduction
Regulating the private sector allows the government to share out responsibility for health service provision whilst maintaining some control over quality and distribution (Afifi, Busse, & Harding, 2003; Baldwin & Cave, 1999). Until recently, private health services faced relatively little scrutiny, with regulating health providers being seen as part of the process of entrenching professionalization. This has changed for various reasons, including increased demand for regulation due to increased numbers of health professions, more awareness that regulation can lead to monopolization, and increased realization that certain aspects of health care bear similar features to other markets and can be regulated similarly (Graddy, 1991; Kumaranayake, 1998).
Health care regulation aims to control some or all of the following: market entry, competitive practices, remuneration, and standards and quality, and, to ensure safe use of health care services more broadly (Afifi et al., 2003). While debate on health care regulation has become more open in developing countries, the evidence base on which regulations and enforcement strategies work best, and what factors contribute to observed outcomes, remains weak (Kumaranayake, Mujinja, Hongoro, & Mpembeni, 2000). Some argue that regulation in developing countries either reflects the governments' unrealistic expectations of what is achievable, or the desires of professional bodies (Blevins, 1995; Ensor & Weinzierl, 2007). Some evidence, for instance, suggests that while regulation plays a role in protecting the public, certain aspects appear to serve the objectives of professionals and limit competition (Blevins, 1995; Graddy, 1991; Paul, 1984).
Specialized drug shops
Specialized drug shops (SDSs) play an important role in provision of health services in Sub-Saharan Africa because they provide quick and convenient access to medicines, and in some cases, flexible payment terms to clients (Goodman et al., 2007). The scope of SDSs varies across countries, but will usually include registered and unregistered pharmacies and registered and unregistered drug shops (Wafula, Miriti, & Goodman, 2012). Studies have shown SDSs to be popular sources of treatment for fever and malaria, diarrhoea, respiratory diseases, and sexually transmitted illnesses, as well as for chronic conditions such as hypertension (Chuc et al., 2001; Garcia, Gotuzzo, Hughes, & Holmes, 1998; Hetzel et al., 2007; Oparah, Adje, & Enato, 2006). There is increasing interest in how policy makers can work with SDSs to strengthen health systems. However, there are concerns over their performance, with studies showing practices such as dispensing without prescription being common. Interventions to improve their practices have been limited mainly to training, with little effort going towards strengthening regulation (Wafula & Goodman, 2010).
Specialized drug shops are an important part of the Kenyan health system; with estimates suggesting 26–69% of the population visit them for fever (Amin, Marsh, Noor, Ochola, & Snow, 2003; Chuma, Gilson, & Molyneux, 2007; Molyneux, Mung'Ala-Odera, Harpham, & Snow, 1999). In Kenya, pharmacies are the only cadre of SDSs that is recognized by law; however, unregistered SDSs have been widely documented (Barnes et al., 2009). For this reason, we use the term SDSs to refer to both registered and unregistered pharmacies. However, pharmacies that are joined to a clinic and do not serve walk-in clients (clients who have not been seen by the clinician), are not included in the SDS categorization.
Because SDSs are a component of the health system, they are regulated in ways that are similar to other providers. In Kenya, the pharmaceutical sector is governed by several pieces of legislation, the main one being the Pharmacy and Poisons Act of 1959. Others include the Public Health Act of 1961, the Food, Drugs and Chemical Substances Act of 1965, the Narcotic Drugs and Psychotropic Substances Act of 1994, as well as Guidelines for Good Wholesaling and Retail Practice (details on regulations and compliance level published elsewhere) (Wafula, Abuya, Amin, & Goodman, 2013). Two cadres of pharmaceutical qualifications are recognized in Kenya: degree (pharmacists) and diploma in pharmaceutical technology (pharmaceutical technologists). Pharmacists practice following a four year degree course and one year internship, whereas technologists study for three years and undertake a six month internship. The two cadres play a similar role in the retail sector; however, only pharmacists are allowed to engage in pharmaceutical wholesale or importation.
Regulatory enforcement is done by pharmaceutical inspectors (PIs) and public health officers (PHOs). The PIs are employed by the Pharmacy and Poisons Board (PPB, a semi-independent government body that serves as the medicine regulator) to enforce pharmaceutical regulations specifically, and will usually have a degree or diploma in pharmacy qualification. Public health officers, on the other hand, are employed directly by the Ministry of Public Health to enforce a wider range of regulations governing the health sector, including those governing SDSs, as well as community hygiene practices (such as pit latrines) and hotels. The PHOs typically have a diploma qualification in public health, although some have university degree qualification. The PI and PHO roles are defined by the Pharmacy and Poisons Act and the Public health Act respectively, hence the overlap in roles. Professional ethics are enforced by the professional bodies for pharmacists and technologists, but there is no active association for PHOs.
In 2009, we conducted provider and mystery shopper surveys of SDSs in two Kenyan districts. The results showed most SDSs were not complying with regulations, for instance, over half did not keep prescription records, have a refrigerator, or have staff with pharmacy qualifications (survey findings reported elsewhere) (Wafula et al., 2013). Non-compliance was higher in rural locations, for instance, only 12% of rural SDSs had a designated dispensing area, compared to 43% for urban SDSs. However, regulatory inspection frequencies were similarly high in rural and urban areas (over 80% for both). These findings pointed at inadequacies in regulatory enforcement, suggesting a need for a detailed understanding of what happens during inspections, and how this translates into practices. This study sought to understand how the interaction between front-line regulators and SDS operators influences regulatory practices, and how organizational factors influence behaviour of regulatory staff.
Regulation theory: the conceptual framework
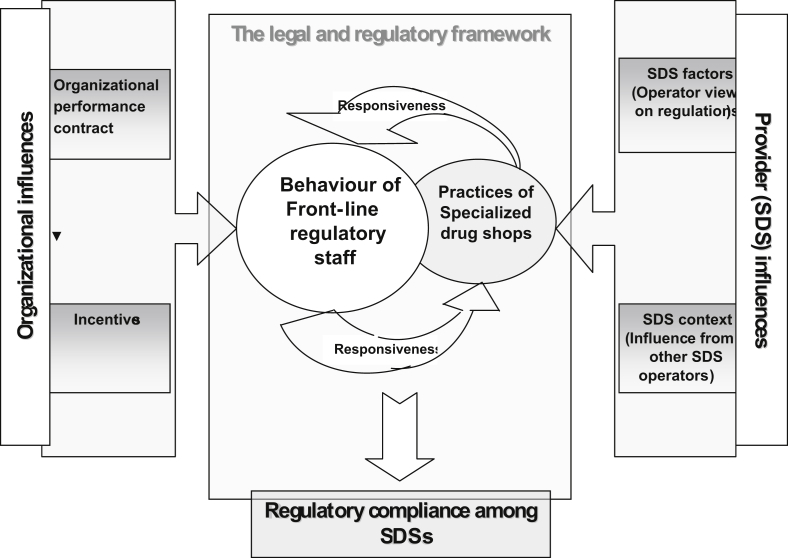
Scholarly work on regulation has evolved mainly along the politico-economy pathway, where regulation was seen as either serving the public interest (the public interest theory) or individual groups (interest group theories) (Den Hertog, 2000; Ogus, 2004). While the public interest theory saw regulation as a tool for correcting market failure, interest group theories depicted it as a tool for serving the interests of politicians, bureaucrats and regulated entities. The latter group include regulatory capture, the Chicago theory, and the public choice theory (Posner, 1974). However, these older theories have increasingly lost ground, with more interest going towards understanding the ingredients of effective regulation (Balleisen & Moss, 2009). There is increasing interest, for instance, in understanding influences on regulatory enforcers, and the interaction between regulators and private providers. Some of the ideas that have shaped recent debates were reviewed and developed into a conceptual framework for the study (see Fig. 1).
Fig. 1.
Conceptual framework – Factors that influence behaviour of front-line regulatory staff.
At the heart of the conceptual framework is the relationship between front-line regulatory staff and SDS operators. We drew on insights from the responsive regulation theory to examine this relationship. Responsive regulation defines regulation, not as a rigid set of rules, but as a tool for addressing the diverse objectives, structure and operations of the regulated entities (Ayres & Braithwaite, 1992). The theory proposes that enforcement should respond to variations in the industry, with severity of sanctions varying with compliance. We chose the theory based on the observation that the SDSs operated in vastly different environments, and that regulatory compliance was varied, despite both rural and urban SDSs having frequent inspections. However, while the responsive regulation theory is a normative presentation of alternative ways of enforcing regulations, we apply its insights to examine whether and how variations in the SDS market environment elicit different regulatory responses.
Away from the enforcement level, we hypothesized that front-line regulatory staff and SDS operators are both subject to other influences. Borrowing from organizational theory, we hypothesized that regulatory staff will be influenced by factors such as incentives and incentive contracts (Meckling & Jensen, 1996; Milgrom & Roberts, 1992). Milgrom and Roberts argued that ‘organizations either must rely on individuals to ignore their own self-interests, with unsurprisingly disappointing results, or else devote ingenuity and resources to bring coherence between individual self-interest and the social or organizational objectives’ (Milgrom & Roberts, 1992). We examined the relationship between the regulatory organizational set-up and behaviour of front-line regulatory staff. This is presented on the left side of the conceptual framework.
Finally, we hypothesized that SDS operators will be influenced by broader market forces, including the nature of competition, SDS operators' perceptions on the relative importance of different regulations, and expectations from the broader community. These sets of factors are presented on the right hand side of the conceptual framework.
Methodology
The study sought to understand how the interaction between front-line regulatory staff and SDS operators influences regulatory compliance among SDSs; how organizational factors influence the behaviour of front-line regulatory staff; and how broader market factors influence the regulatory practices of SDS operators.
Study population and data collection
Data were collected from two districts in Western Kenya – Bungoma South and Kakamega Central – using a combination of in-depth interviews (IDIs) with regulatory staff and focus group discussions (FGDs) with SDS operators. These were held between March and June 2011. The Western region was preferred as SDSs are known to be numerous there, and therefore of high policy importance (Abuya et al., 2007; Tavrow, Shabahang, & Makama, 2003). The two districts were selected because they have both rural and urban settings, thus allowing comparison by location.
The two districts have a high population density (602 for Bungoma, and 723 for Kakamega against a national average of 68 per km2). The commonest causes of morbidity and mortality in the region are malaria, diarrhoea, respiratory diseases, and HIV/AIDS (Ministry of Planning, 2008a, 2008b). Both districts have high poverty levels, with 51 and 54% of individuals living below the poverty line in Bungoma and Kakamega respectively (Government of Kenya, 2005). Although both have a major town, the majority of the population reside in rural locations, which generally have poor roads. Both districts also suffer from low staffing levels, with the doctor-patient ratios of 1:26,613 (Bungoma) and 1:20,835 (Kakamega) being way below the national average of approximately 1:5260 (Ministry of Planning, 2008a, 2008b).
A total of 8 FGDs were held, each including 8–12 individuals. The FGDs sought to understand interactions between regulators and SDSs (see Table 1).
Table 1.
Summary of items included in the data tools.
| Data tool | Items included |
|---|---|
| Focus group discussion topic guide | Experiences with regulatory staff How specialized drug shop (SDS) operators respond to different actions by regulators Influence from clients How SDS operators balance profit incentive and compliance |
| In-depth interview topic guide for front-line staff | Inspections experiences and relationships with SDSs Responsiveness to differences in practice environments of SDSs Responsiveness to different regulatory behaviours of SDSs Effects of organizational incentives on performance Relationships with other front-line staff |
| In-depth interview topic guide for national managers | Understanding of what happens at enforcement level Structure and management of regulatory organization Opinions on how enforcement should be strengthened |
Focus groups were preferred over individual interviews to allow operators to discuss the sensitive topic in a relaxed atmosphere, and enable us to gather information from a large number of providers. SDS operators were purposively selected to capture a wide range of experiences (Kuper, Reeves, & Levinson, 2008), and enable us to test our theoretical assumptions (Seale, 1999). Because the inquiry sought to explore how regulators respond to variations in the market, shop location was a key factor in SDS selection. We also aimed to select a range of SDSs in terms of regulatory compliance drawing on the results of the quantitative surveys conducted in the same districts (Wafula et al., 2013). SDSs were classified as better or poorer performers on the basis of indicators including staff qualification, dispensing practices, and availability of designated dispensing areas. Two FGDs were held in rural and urban locations in each district. The distribution of qualified personnel varied, with urban FGDs having more staff with the required pharmacy qualification. The first author (FW) moderated the discussions, with two field staff observing the group dynamics and taking notes.
In-depth interviews explored a number of regulatory factors (Table 1). Interviewees were selected to represent all levels of pharmaceutical regulation, from the peripheral to the national level. We interviewed 3 pharmaceutical inspectors and eight PHOs working in the Western region of the country. At the higher levels, a total of 13 interviews were conducted with several key organizations, including PPB, the Pharmaceutical Society of Kenya (PSK), the Kenya Pharmaceutical Association (KPA) and the Department of Pharmacy at the Ministry of Medical Services. Individual interviews were preferred for regulators, to capture confidential views, and because organizing FGDs for inspectors would be logistically impractical.
Data analysis and ethical clearance
Interview recordings and field notes were transcribed, and imported into NVIVO 9 for content analysis. To help identify policy relevant findings, a framework analysis approach was adopted (Ritchie & Spencer, 1994). The thematic framework carried three headings that reflected the conceptual framework: (i) relationship between front-line staff and SDSs; (ii) organizational influences, and; (iii) other factors influencing SDS operators.
Institutional ethical approval was provided by the KEMRI/Wellcome Trust Research Programme and the London School of Hygiene and Tropical Medicine (Application No. 5457), with national approval by the KEMRI National Ethical Review Committee (SSC No. 1535). Individual verbal consent was sought from the SDS attendants participating in the individual and group interviews.
Findings
Findings are discussed in three sections; an exploration of relationship dynamics between front-line staff and SDS operators; an examination of organization influences on front-line staff; and finally, a discussion of other factors that influenced behaviour of SDS operators.
Relationship between front-line staff and SDS operators
Most SDS operators believed that outcomes of inspections depended on how they related with regulators. Overall, differences were observed in relationships between the two front-line cadres and SDS operators, with PIs enjoying collegiate relationships with urban SDSs, while PHOs enjoyed fairly good relations with rural SDSs. Variation in relationships appeared to be linked to differences in SDS operators' qualifications, with PIs perceiving rural SDSs as unlicensed outlets run by “quacks” (a term interviewees used to describe unqualified providers). This influenced their interaction, with rural operators describing them as unfriendly and uncompromising.
FGD Participant 3 (rural): ‘when a drug inspector (PI) comes in your chemist, he looks at you as a quack; someone who doesn't know about drugs. Secondly, he will ask about qualifications, and if you say certificate (certificate in pharmacy), he just enters, takes drugs and goes with them. They behave harshly with the people in the rural areas…’
Additionally, rural operators admitted to having little incentive to improve practices, arguing that they were already perceived as perpetual offenders. They complained that PIs made little effort to check for improvements or advise on areas of improvement. This made them believe that the optimal behaviour in the face of regulatory inspections was closing shops and running away.
FGD Participant 1 (rural): ‘poor villagers like us; they don't tell us anything; just to pick the drugs and we go (to the police station). No time for communication. How will you begin discussing? Do they have time? The vehicle is waiting outside (to carry away the drugs)…’
Pharmaceutical inspectors on their part, admitted to being unfriendly towards rural SDSs, arguing that the majority were managed by “quacks”.
The issue of operators running off during inspections was widely reported. Whereas operators argued that inspectors came determined to find fault, the inspectors stated that inspections were not meant to punish those offering a good service. These regulatory “cat-and-mouse games” resulted in situations where some shops were not inspected routinely.
Some inspectors admitted that they felt compelled to be more lenient towards rural providers. One argued that since most qualified operators prefer urban locations, blanket enforcement would result in closure of most rural SDSs, and negatively impact on medicine access. This view, which was shared by some senior regulatory staff, presented a dilemma at policy level, with little agreement on whether or not to show leniency towards rural operators.
Pharmaceutical inspector 1: ‘…If you went to some areas and …the next health centre it is about let's say 30 km…you see it will change your thinking. Even if you are handling somebody….as a human being you may find yourself trying to sympathize with this person…’
In sharp contrast to the case with rural operators, PIs enjoyed cordial relations with urban operators, with the majority of the operators describing them as friendly and professional.
FGD Participant 4 (urban): ‘…they (PIs) are friendlier because they are undergoing some training…and realizing whoever is out there is a colleague…a pharmacist or a technologist.’
The PIs stated that they held professional qualifications in high regard, with some even admitting they may ignore the absence of licenses if staff attending to clients were properly qualified. Here, having professional qualifications was equated to providing good quality service. Aside from qualifications, knowledge on pharmaceutical treatments appeared to influence actions taken by PIs. Here, the inspector would interview the provider to gauge their level of knowledge, and if satisfied, they would allow the individual to continue running the shop without a license.
Unlike PIs who were recognized across all SDSs, PHOs' legitimacy was limited mainly to rural shops. This stemmed from the fact that rural operators received regular visits from PHOs, who had good community penetration. The rural operators described PHOs as understanding, with the PHOs saying that although most rural operators had no pharmacy qualification, they were important in filling the gaps in health provision. In contrast, most urban operators did not see PHOs as legitimate regulators, arguing that they held no pharmacy training. As a result, PHOs described urban operators as ‘arrogant’, particularly those with a pharmacy degree.
A major consequence of the nature of interaction between front-line regulators and SDS operators was corruption, which was reported in three related forms: (a) an institutionalized form, where bribes were embedded in interactions, (b) an aggressive form where enforcers created opportunities to collect bribes, and, (c) a subtle form where operators offered bribes for specific mistakes found during inspections.
The institutionalized form, reported mainly in rural locations, entailed routine payment of bribes. Inspectors rarely asked for bribes directly (after the initial encounters); instead, they expected operators to send money periodically to keep inspections away. Such was the level of entrenchment of the practice that operators admitted using M-PESA to send bribes (M-PESA is a mobile phone money transfer system that leaves the recipient's details on the sender's phone).
FGD Participant 1 (rural): ‘…you build a relationship eventually, and when they know you, then obviously after sometime you M-Pesa some money. You will be in safe books now (laughter)…if you want to be safer, don't wait for him to come or to call you. Tell him (miming phone call) “Mister, today I am sending you 2000 (Shillings), okay!” You are now keeping him away. So, even if they know you, it is not like they will stop expecting money…’
Aside from ignoring infringements, the regulators involved routinely warned operators ‘within their friendship networks’ of impending inspections, thus according them time to close shops.
FGD Participant 8 (rural): ‘So, if an inspector – my friend – tells me that next week is bad! Then I tell this gentleman (points at colleague) that next week, be ready, then he tells his friend then the network continues (laughter). Everybody will close that week. The inspectors will just arrest an unfortunate person who was not in that network…’
Like the previous form, the aggressive form of corruption was reported mainly in rural areas. Here, the operators saw regulators as opportunists who took advantage of the illegal status of businesses to demand bribes. Power relations were clear here, with operators presenting themselves as victims and depicting inspectors as villains, as opposed to the previous form where the operators saw themselves as beneficiaries of the ‘network’.
FGD Participant 5 (rural): ‘…some of the (regulatory) personnel will keep on watching you; when they realize that you are growing, they start setting traps. Sort of interfering with you whereby any little profit that you have gotten, they want to interfere in the name of threats…’
The final form of corruption, reported across both urban and rural locations, was where operators offered bribes to avoid consequences of non-compliance. In this form, bribes were offered to cover irregularities spotted during inspections. The distinguishing feature here is that enforcers and operators did not have established relationships. This form reportedly extended to the national-level enforcers, who made occasional regulatory visits to different parts of the country. Some operators described the national inspectors as being particularly ‘expensive’ to bribe.
Aside from corruption, there were reports of high-handedness among inspectors. Operators complained that inspectors carried away medicines, and that these drugs were rarely traceable afterwards. The PIs, on their part, argued that past experiences with a corrupt judiciary and police had forced them to adopt militant enforcement strategies. They argued that there was little sense in instituting legal proceedings, knowing well that the offenders would get off with small fines. Seizing medicines was thus seen as a more effective form of punishment.
Organizational influences on behaviour of front-line staff
The PIs were generally fewer than PHOs, with the latter having a stronger community presence. The wider community penetration allowed PHOs to have more detailed information on location and practices of SDSs, particularly in remote areas, which is where PHO activities focus primarily. This, in turn, influenced the way PHOs related to operators and the broader communities, with the majority acknowledging that they felt like members of the community. All PHOs were clear that they report to the public health office at the district level.
Unlike PHOs, there was confusion on the reporting structure for PIs because, while the PHOs' chain of command ended with district authorities, PIs reported to district and national (PPB) managers. This resulted in inter-personal variations in reporting behaviour, with some PIs reporting to the district routinely, while others went about their duties without involving the district management. This reduced PI effectiveness, as their activities were not fitted within the overall district health plans and they therefore could not access district resources.
PI 1: ‘…They (rural SDSs) don't respect you because they know you are not empowered logistically. They fear the Nairobi people because they come with big vehicles. Here, you borrow a vehicle, there is no fuel, so you just tell someone “I will come back you will see”. You keep using threats. Because you can't afford to buy police lunch… he can't come! Those Nairobi people come with money, big vehicles, take policemen, do their job and go. You you’re just seen as any ordinary person’
Aside from confusion over reporting, there was an overall lack of clarity over which staff should enforce which regulations, resulting in conflicts between PHOs and PIs. Whereas the PHOs' role in inspecting hygiene and structural aspects of SDSs was accepted, there was disagreement on whether they should inspect pharmaceutical aspects. The PIs accused PHOs of encouraging the mushrooming of unlicensed outlets by giving unqualified personnel permission to operate. The guarded relationship resulted in little collaboration between the two cadres.
PI 1: ‘…most unlicensed people don't know what PPB is! You go there, they show you a license (and say) “I went to the PHO's office I have a license”. The person looks surprised that there is another license they need. In fact most illegal outlets have passed through the hands of PHOs…’
As far as incentives go, both PHOs and PIs felt that little had been done overall with regard to incentivising enforcement. To improve performance, PPB had instituted monthly salary top-ups for PIs, year-end shopping vouchers, as well as a system of performance contracts. The salary top-ups were fixed; they were not pegged on specific performance measures. Although the PIs appreciated these, they conceded that they did not encourage one to surpass targets. Public health officers, on the other hand, received neither top-ups nor vouchers.
Performance contracts were signed by both PHOs and PIs. The contracts outlined goals that individuals were required to achieve over an agreed period. However, the focus of the contracts varied across PIs and PHOs, with the former being more specific to SDSs (for instance, conducting at least 3 successful court cases every month) and the latter touching on broader public health targets (such as pit latrine coverage). However, while continual failure to achieve targets reportedly led to dismissal or other forms of punishment, the linkage between performance evaluation and benefits was relatively unclear. Staff also questioned the usefulness of some performance indicators, for instance, one PI wondered what would happen if good compliance was achieved by operators in an area, and there were no cases to prosecute.
Other factors influencing behaviour of SDS operators
The SDSs were heavily influenced by client demands, which varied with location. In rural areas, operators spoke mainly of helping the community, which they felt they were an integral part of. Selling partial doses of medicines, for instance, was seen as an act of empathy, particularly when directed towards those less able to meet the full treatment costs.
FGD participant 1 (rural): ‘…most of us deal with very poor people. They come with 5 bob (Shillings), and they want a drug that is worth the 5 Shillings, and yet you are not supposed to sell a drug that is not a full dose. And you live with him; you are in a village chemist. If you deny him, that is a problem. So you try all means to give him that medicine that is worth 5 Shillings…’
In urban areas, on the other hand, operators acceded to client demands mainly to ward off competition. There was a general conviction that one either ‘sells or perishes’. In their eyes, failing to satisfy clients' demands simply meant more business for the seller next door.
FGD Participant 6 (urban): ‘I remember when I opened the business, I found a very professional pharmacist and people had run away. I made some good money which was meant for that professional. He had just come from developed countries and he was imagining this is that country. So he went down because people were not ready to listen……people want ‘give me Panadol!’ you give. You don't ask……’
The operators also complained of unfair competition, noting that compliers faced higher costs than those operating outside the law. However, not all urban operators subscribed to the ‘sell or perish’ notion. Some felt that doing so went against professional ethics, arguing that clients appreciated good advice over time, even if it meant refusing to sell inappropriately. There were instances where acceding to client demands resulted in tension between trying to remain professional and staying afloat in the competitive business. Some urban operators believed that qualified individuals were less likely to engage in unlawful behaviour, and that the lay public could differentiate professionals from “quacks”. For that reason, they went the extra mile to provide good care, which included asking questions, scrutinizing prescriptions, making call-backs to prescribers and sending clients for laboratory tests.
Discussion
The problem of poor regulatory compliance has been widely reported among medicine retailers. However, little has been done to understand the underlying reasons, particularly with regard to the role played by regulatory staff. This was the main objective of the study.
The study found relationships to be a strong determinant of regulatory practices overall. The relationships varied across the staff cadres, with PIs and PHOs enjoying good relationships with urban and rural operators respectively. Urban operators responded to formal rules, with their rural counterparts responding more to perceptions of social standing. In the end, the two sets of relationships resulted in separate regulatory streams in urban and rural areas, exemplifying the influence of social and cultural context on regulatory enforcement. The importance of contextual norms in determining success of regulatory interventions has been emphasized elsewhere (Mackintosh & Tibandebage, 2002), and underscores the value of considering pre-existing relationships when designing regulations. The two streams also point at the existence of a responsive regulatory relationship, albeit different from Ayres and Braithwaite's form (Ayres & Braithwaite, 1992). Responsive regulation describes an enforcement system where steps taken by enforcers depend on actions of the regulated entities. While the original theory entails the use of incentives and disincentives to build a compliance culture, the responsiveness here reflected a combination of savvy pursuit of personal goals, and effort to attain the broad public health objective of access in a market characterized by a rigid and unresponsive set of rules.
The first form of responsiveness was linked to self-serving actions, where regulators would collect bribes from operators, who in turn received favourable decisions and inspection warnings. Here, regulations were simply not being adhered to, and rather than face each other on different sides of the law, the operators and regulators opted for a perverse equilibrium from a societal perspective, that would serve their individual goals. This equilibrium, which made entrenching a culture of compliance difficult, led us to refocus our analysis from a qualitative description of reasons underlying gaps between regulations and practices, to an inquiry into what happens when a rigid system of rules is designed to apply uniformly, with little recognition of socio-cultural influences and contextual norms. It appears regulators were resigned to the fact that regulations could simply not be enforced uniformly; this, coupled with the weak incentives and poor monitoring from their organizations, contributed to the corruption reported.
Not all responsiveness was linked to self-serving actions. There were instances where regulators adjusted decisions based on the practice environments of the SDSs. This form of responsiveness, which we call the ‘adaptive’ type, appeared to have had the blessing of some senior staff. Geographical location was the main determinant here, with regulators subscribing to an unwritten consensus to show leniency towards rural SDSs. This is not unique to Kenya; in Sri-Lanka, food and drug inspectors admitted to being lenient towards rural pharmacies, according them more time to meet regulatory requirements, rather than closing them down as required by law (Attanayake & Siyambalagoda, 2003). Such leniency is suggestive of an informal system of ‘levels of practice’, where individuals with lower qualifications are allowed to operate in low-access areas, with their more qualified counterparts operating in the more lucrative areas.
There were cases of regulators advising operators on areas of improvement, and agreeing on timelines within which the changes should be effected. This strategy was built on the thought that individuals have plural motivations for complying (and not-complying), and that appropriate deployment of compliance and deterrent strategies can result in a culture of compliance (Ayres & Braithwaite, 1992; Nielson & Parker, 2009). However, successful deployment of such a strategy needs regulators to make operators believe that penalties will be instituted (if required), a phenomenon referred to as ‘deploying the benign big gun’ under responsive regulation theory. The benign big gun would be ineffective, for instance, in situations where deployment of sanctions relies on activities of others beyond the control of the regulator. In this study, regulators complained of slowness in the judiciary systems, a problem they circumvented by employing a ‘scorched earth policy approach’, where infringing operators would be paralysed through commodity confiscation. In the end, it was fear of losing commodities, rather than facing the law, that rendered the benign big gun effective. Unfortunately, this approach resulted in regulatory cat-and-mouse games, with operators believing that compliance was an all or none phenomenon, and that incremental improvements carried no benefits.
While relationships were central in determining practices, the structure and management of the regulatory organizations were equally important. By virtue of their nature, regulatory organizations are expected to face problems of agency relationships. Agency refers to relationships where principals delegate responsibilities to agents in order to benefit from the latter's ability to execute the tasks (Eisenhardt, 1989). In this study, front-line staff were the agents of the regulatory managers. As predicted, problems of imperfect agency were reported, including managerial dilemmas on incentivising and monitoring performance. While some monetary incentives were provided, these were poorly linked to performance.
Performance contracting, on the other hand, had a more precise formulation, outlining targets that staff were required to achieve over set periods. However, while consequences of persistent failure were well explained, the link between performance evaluation and benefits was relatively unclear. Such systems run the risk of creating scenarios where staff look to attain the set goals, but have little incentive to surpass targets. Unfortunately, designing contracts that show clear linkage between performance and reward is not easy, especially considering that good incentive contracts often have a combination of subjective and objective measures of performance (Baker, Gibbons, & Murphy, 1994; Levin, 2003). This also brings to the fore the problems of evaluating performance in systems where indicators are hard to design. Tying compensation to poorly measured performance outcomes transfers greater risk to front-line staff, which would entitle them to higher compensation (Holmstrom, 1979; Holmstrom & Milgrom, 1991). In Kenya, PI performance measures included indicators such as the number of cases prosecuted per month. Herein lay the problem, as prosecution depended on multiple factors, most of which were outside the control of the inspectors (such as efficiency in the judiciary departments).
Two other important influences on SDS behaviour were client expectations and competition. Client demand influenced practices, albeit in different ways, across the 2 locations. Rural operators described their clientele as mainly interested in low prices and flexibility in quantities of medicines purchased. To rural operators, charging high prices meant less business, regardless of whether the prices were accompanied by better pharmaceutical care or the assurance of a high quality product. Perhaps in response to this, rural operators were engaged in what appeared to be a “race to the bottom” competition, where those most able to sell medicines at the lowest cost, and those most willing to sell medicines in the smallest units possibly won (yet under dosing can result in incomplete cure and resistance). Such competition is bound to result in adverse selection of quality, where operators offering high quality services are driven out of business and replaced by low-quality suppliers, whose product still meets the approval of the market (whose ability to infer quality is limited). Urban operators, on the other hand, were said to have a ‘floor on quality,’ despite the higher competition. The competitive environment had conditioned urban SDSs into offering more services, with operators going out of their way to show clients that they were qualified, resulting in practices such as counselling on medication use. The competition appeared to have improved urban SDS services, but worsened those of rural SDSs.
Two potential limitations with the study were failure to interview certain actors, and the generalizability of the study. One potentially useful set of interviews not done due to logistical constraints, were police superintendent interviews. These interviews would have provided insight on how the regulatory staff work with the police, and the challenges that may arise from the collaboration. As far as generalizability is concerned, data were collected from two districts known to have similar epidemiological profiles and relatively high retail sector activity (Abuya, 2008; Tavrow et al., 2003). Previous work has also shown the Western region of the country to have a relatively good geographic access to public health facilities compared to other parts (Noor, Alegana, Gething, & Snow, 2009). As a result, the findings are unlikely to represent the full range of operator–regulator interactions across rural districts in other parts of the country. However, theoretical insights can be extrapolated beyond the study area; for instance, one might expect the way front-line staff and SDS operators interact to also be an influence regulatory practices in other parts of the country. One might also expect the organizational factors that influenced regulatory staff to apply to regulators working in other parts of the country. What would, perhaps be less appropriate, is applying theoretical arguments developed here to major cities such as Nairobi. It is nonetheless expected that behaviour patterns in larger towns would somewhat resemble those reported across the urban locations of the study districts.
A number of policy implications arise from the study. Firstly, laws should be streamlined to clarify the roles of different front-line staff. Secondly, policy needs to recognize that interactions and relationships at the enforcement level have a strong influence on regulatory practices. Regulations would do well, for instance, to build on the influence PHOs have across the rural locations, where the Pharmacy and Poisons Board's regulatory machinery has failed to have a sustained impact. This may mean either incorporating PHOs into the formal PPB regulatory structure, or devising alternative regulatory arrangements to govern rural SDSs.
More thought should also go towards adopting levels of practice. Such lower levels, often referred to as part II drug shops, are legally recognized in Uganda and Tanzania for instance (Health Research for Action, 2006; Jacobs, Whitworth, Kambugu, & Pool, 2004). Under this arrangement, individuals would be allowed to sell a limited range of medicines in underserved areas, preferably following short dispensing courses. This would ensure public health objectives are met in an environment characterized by rigid statutory provisions. It would also promote equity, as individuals in remote areas would have access to formally regulated SDSs. It may mean shifting the regulation of the lower level SDSs from the professionals-driven pharmaceutical field to the public health field, where regulation would be defined in terms of public health objectives. Aside from ensuring expanded service provision, allowing lower practice levels would bring more SDSs within the law, thus providing an entry point for interventions such as training and providing educational materials. However, unless carefully thought through and communicated, this approach may encounter resistance from pharmacy professionals, who may see it as an encroachment on their profession. A move towards levels of practice would therefore need a consultative approach, with effort going into showing how such a system would benefit professionals in practice.
As far as regulatory organizational management is concerned, policy should explore incentive structures that are clearly tied to the goals of regulation.
Conclusion
This study used FGDs and individual interviews to understand how the nature of interaction between regulators and SDS operators translates into regulatory practices.
Relationships between regulators and operators were found to have a strong influence on regulatory behaviour, often resulting in perverse outcomes such as corruption. It also emerged that separate regulatory streams operated in urban and rural locations, based on the differing nature of relationships, the competition environment and expectations from the community. As a result, we recommended that policy should introduce lower retail practice requirements for rural SDSs in recognition of the vast differences in rural and urban practice environments. This would allow shops operating unlawfully to be brought within the regulatory framework without affecting practice in urban locations.
A more radical approach would be separating the professionals-operated pharmaceutical sector, whose goals include protection of the profession, from the more socially fluid public health sector, whose goals revolve around promoting access to affordable treatments within rural communities. This would result in a situation where pharmacists maintain control of the high business potential areas, while the public health department seeks alternative ways of licensing non-pharmacists to provide essential commodities in rural areas.
As far as operations of front-line staff are concerned, the regulatory system was found to lack effective incentive structures to encourage regulatory enforcement. While there were some incentives for pharmaceutical inspectors, there was lack of clarity on how these related to performance, with enforcers feeling that the level of effort had no bearing on professional advancement. The recommendation is that regulatory organizations should explore ways of linking incentives and professional development to performance.
Acknowledgement
We would like to thank Truphena Onyango and Bealiah Makokha for supporting the data collection processes, and the KEMRI/Wellcome Trust Social Science Group for giving useful comments at different stages of the study. This work was supported by a fellowship grant from the Wellcome Trust to the first author (grant number #083078/Z/07/Z). FW, CM and CG are affiliated with the KEMRI/Wellcome Trust Research Programme, which is funded by the Wellcome Trust (grant # 077092).
References
- Abuya T. Life Sciences Discipline, The Open University; UK: December 2008. A comparative analysis of malaria control programmes targeting delivery of over-the counter anti-malarial drugs in Kenya. (PhD thesis) [Google Scholar]
- Abuya T., Mutemi W., Karisa B., Ochola S.A., Fegan G., Marsh V. Use of over-the-counter malaria medicines in children and adults in three districts in Kenya: implications for private medicine retailer interventions. Malaria Journal. 2007;6:57. doi: 10.1186/1475-2875-6-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Afifi N.H., Busse R., Harding A. Regulation of health services. In: Harding A., Preker A., editors. Private participation in health services. World Bank; Washington DC: 2003. [Google Scholar]
- Amin A.A., Marsh V., Noor A.M., Ochola S.A., Snow R.W. The use of formal and informal curative services in the management of paediatric fevers in four districts in Kenya. Tropical Medicine & International Health. 2003;8:1143–1152. doi: 10.1046/j.1360-2276.2003.01140.x. [DOI] [PubMed] [Google Scholar]
- Attanayake N., Siyambalagoda L. LSHTM; 2003. An inquiry into the regulation of pharmaceuticals and medical practice in Sri Lanka. HEFP working paper 05–03. [Google Scholar]
- Ayres I., Braithwaite J. Oxford University Press; New York: 1992. Responsive regulation: Transcending the deregulation debate. [Google Scholar]
- Baker G., Gibbons R., Murphy K. Subjective performance measures in optimal incentive contracts. Quarterly Journal of Economics. 1994;109(4):1125–1156. [Google Scholar]
- Baldwin R., Cave M. Oxford University Press; Oxford: 1999. Understanding regulation: Theory, strategy and practice. [Google Scholar]
- Balleisen E., Moss D. In: Government and markets: Toward a new theory of regulation. Balleisen Edward, Moss David., editors. Cambridge University Press; New York, NY: 2009. [Google Scholar]
- Barnes J., O’Hanlon B., Feeley F., McKeon K., Gitonga N., Decker C. Abt Associates Inc; Bethesda, MD: 2009. Kenya private health sector assessment. (Private sector partnerships-one project). [Google Scholar]
- Blevins S.A. The Cato Institute; 1995. The medical monopoly: Protecting consumers or limiting competition?http://www.cato.org/pub_display.php?pub_id=1105 Retrieved July 21, 2009. [Google Scholar]
- Chuc N.T., Larsson M., Falkenberg T., Do N.T., Binh N.T., Tomson G.B. Management of childhood acute respiratory infections at private pharmacies in Vietnam. Annals of Pharmacotherapy. 2001;35:1283–1288. doi: 10.1345/aph.10313. [DOI] [PubMed] [Google Scholar]
- Chuma J., Gilson L., Molyneux C. Treatment-seeking behaviour, cost burdens and coping strategies among rural and urban households in Coastal Kenya: an equity analysis. Tropical Medicine & International Health. 2007;12:673–686. doi: 10.1111/j.1365-3156.2007.01825.x. [DOI] [PubMed] [Google Scholar]
- Den Hertog J. General theories of regulation’. In: Bouckaert B., De Geest G., editors. Encyclopedia of law and economics. Vol. III. Edward Elgar; Cheltenham: 2000. pp. 223–270. (The regulation of contracts). [Google Scholar]
- Eisenhardt M.K. Agency theory: an assessment and review. Academy of Management Review. 1989;14(1):57. [Google Scholar]
- Ensor T., Weinzierl S. Regulating health care in low- and middle-income countries: broadening the policy response in resource constrained environments. Social Science & Medicine. 2007;65:355–366. doi: 10.1016/j.socscimed.2007.03.021. [DOI] [PubMed] [Google Scholar]
- Garcia P.J., Gotuzzo E., Hughes J.P., Holmes K.K. Syndromic management of STDs in pharmacies: evaluation and randomised intervention trial. Sexually Transmitted Infections. 1998;74(Suppl. 1):S153–S158. [PubMed] [Google Scholar]
- Goodman C., Brieger W., Unwin A., Mills A., Meek S., Greer G. Medicine sellers and malaria treatment in sub-Saharan Africa: what do they do and how can their practice be improved? American Journal of Tropical Medicine and Hygiene. 2007;77:203–218. [PMC free article] [PubMed] [Google Scholar]
- Government of Kenya (2005). http://opendata.go.ke/Poverty/District-Poverty-Data-KIHBS-2005-6/pnvr-waq2 Accessed August 2012: http://opendata.go.ke/Poverty/District-Poverty-Data-KIHBS-2005-6/pnvr-waq2.
- Graddy E. Interest groups or the public interest–why do we regulate health occupations? Journal of Health Politics, Policy and Law. 1991;16:25–49. doi: 10.1215/03616878-16-1-25. [DOI] [PubMed] [Google Scholar]
- Health Research for Action . 2006. Review of the accredited drug dispensing outlets (ADDO) roll out programme in Tanzania: Report by health research for action (HERA), 19th March. [Google Scholar]
- Hetzel M.W., Iteba N., Makemba A., Mshana C., Lengeler C., Obrist B. Understanding and improving access to prompt and effective malaria treatment and care in rural Tanzania: the ACCESS Programme. Malaria Journal. 2007;6:83. doi: 10.1186/1475-2875-6-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmstrom B. Moral hazard and observability. Bell Journal of Economics and Management Science. 1979;10:7–91. [Google Scholar]
- Holmstrom B., Milgrom P. Multitask principal-agent analysis: incentive contracts, asset ownership, and job design. Journal of Law, Economics, & Organization. 1991;7 (Special Issue) [Google Scholar]
- Jacobs B., Whitworth J., Kambugu F., Pool R. Sexually transmitted disease management in Uganda's private-for-profit formal and informal sector and compliance with treatment. Sexually Transmitted Diseases. 2004;31:650–654. doi: 10.1097/01.olq.0000143087.08185.17. [DOI] [PubMed] [Google Scholar]
- Kumaranayake L. PHP Departmental Publication No. 29, London School of Hygiene and Tropical Medicine; London: 1998. Economic aspects of health sector regulation: Strategic. Choices for low and middle income countries. [Google Scholar]
- Kumaranayake L., Mujinja P., Hongoro C., Mpembeni R. How do countries regulate the health sector? Evidence from Tanzania and Zimbabwe. Health Policy and Planning. 2000;15:357–367. doi: 10.1093/heapol/15.4.357. [DOI] [PubMed] [Google Scholar]
- Kuper A., Reeves S., Levinson W. An introduction to reading and appraising qualitative research. British Medical Journal. 2008;337:a288. doi: 10.1136/bmj.a288. [DOI] [PubMed] [Google Scholar]
- Levin J. Relational incentive contracts. The American Economic Review. 2003;93(3) [Google Scholar]
- Mackintosh M., Tibandebage P. Inclusion by design? Rethinking health care market regulation in the Tanzanian context. The Journal of Development Studies. 2002;39(1):1–20. [Google Scholar]
- Meckling W.H., Jensen M.C. Theory of the firm: managerial behavior, agency costs and ownership structure. In: Buckley Peter, Michie Jonathan., editors. Firms, organizations and contracts, a reader in industrial organization. Oxford University Press; New York: 1996. [Google Scholar]
- Milgrom P., Roberts J. Prentice-Hall; Englewood Cliffs, NJ: 1992. Economics, organization and management. [Google Scholar]
- Ministry of Planning . 2008. Bungoma south district development plan 2008–2012: Ministry of state for planning, national development and vision 2030. [Google Scholar]
- Ministry of Planning . 2008. Kakamega central district development plan 2008–2012: Ministry of state for planning, national development and vision 2030. [Google Scholar]
- Molyneux C.S., Mung'Ala-Odera V., Harpham T., Snow R.W. Maternal responses to childhood fevers: a comparison of rural and urban residents in coastal Kenya. Tropical Medicine & International Health. 1999;4:836–845. doi: 10.1046/j.1365-3156.1999.00489.x. [DOI] [PubMed] [Google Scholar]
- Nielson V.L., Parker C. Testing responsive regulation in regulatory enforcement. Regulation and Governance. 2009;3:376–399. [Google Scholar]
- Noor A.M., Alegana V.A., Gething P.W., Snow R.W. A spatial national health facility database for public health sector planning in Kenya in 2008. International Journal of Health Geographics. 2009;8:13. doi: 10.1186/1476-072X-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogus A. W(h)ither the economic theory of regulation? What economic theory of regulation? In: Jordana J., Levi Faur D., editors. The politics of regulation: Institutions and regulatory reforms for the age of governance. Edward Elgar; 2004. pp. 31–44. [Google Scholar]
- Oparah A.C., Adje D.U., Enato E.F.O. Outcomes of pharmaceutical care intervention to hypertensive patients in a Nigerian community pharmacy. International Journal of Pharmacy Practice. 2006;14:115–122. [Google Scholar]
- Paul C. Physician licensure and the quality of medical care. Atlantic Economic Journal. 1984;12:18–30. [Google Scholar]
- Posner R.A. Theories of economic regulation. Bell Journal of Economics and Management Science. 1974;5:335–358. [Google Scholar]
- Ritchie J., Spencer L. In: Qualitative data analysis for applied policy research in analyzing qualitative data. Bryman Alan, Burgess G. Robert., editors. Routledge; London: 1994. [Google Scholar]
- Seale C. The quality of qualitative research. Qualitative Inquiry. 1999;5(4):465–478. [Google Scholar]
- Tavrow P., Shabahang J., Makama S. Vendor-to-vendor education to improve malaria treatment by private drug outlets in Bungoma District, Kenya. Malaria Journal. 2003;2:10. doi: 10.1186/1475-2875-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wafula F., Abuya T., Amin A., Goodman C. 2013. The policy-practice gap: Describing the gap between regulation on paper and real-life practices among specialized drug shops in Western Kenya. (submitted for publication) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wafula F., Goodman C. Are interventions for improving the quality of services provided by specialized drug shops effective in sub-Saharan Africa? A systematic review of the literature. International Journal for Quality in Health Care. 2010;22:316–323. doi: 10.1093/intqhc/mzq022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wafula F., Miriti E.M., Goodman C.A. Examining characteristics, knowledge and regulatory practices of specialized drug shops in Sub-Saharan Africa: a systematic review of the literature. BMC Health Services Research. 2012;12:223. doi: 10.1186/1472-6963-12-223. [DOI] [PMC free article] [PubMed] [Google Scholar]