Abstract
Cancer is a major health problem and cause of death worldwide that accounted for 7.6 million deaths in 2008, which is projected to continue rising with an estimated 13.1 million deaths in 2030 according to WHO. Breast cancer is the leading cause of cancer-based death among women around the world and its incidence is increasing annually with a similar tendency. In contrast, renal cell carcinoma accounts for only 3% of total human malignancies but it is still the most common type of urological cancer with a high prevalence in elderly men (>60 years of age). There are several factors linked with the development of renal cell cancer only, while others are connected only with breast cancer. Genetic risk factors and smoking are the factors which contribute to carcinogenesis in general. Some evidence exists indicating that vitamin D receptor (VDR) gene polymorphisms are associated with both breast and renal cancer; therefore, we put forward the hypothesis that polymorphisms in the VDR gene may influence both the occurrence risks of these cancers and their prognosis. However, the relationship between VDR polymorphisms and these two specific cancers remains a controversial hypothesis, and consequently needs further confirmation via clinical research together with genetic investigations. Here, we aimed to assess the correlation between the different alleles of VDR gene polymorphisms and renal cell cancer and breast cancer risks separately through a systematic review of the present literature. In contrast, this analysis has revealed that some VDR gene polymorphisms, such as: Bsm1, poly(A), Taq1, Apa1, are to some extent associated with breast cancer risk. Other polymorphisms were found to be significantly associated with renal cell cancer. Namely, they were Fok1, Bsm1, Taq1 and Apa1, which encode proteins participating mainly in proliferation, apoptosis and cell cycle regulation. However, data concerning renal cancer are not sufficient to firmly establish the VDR gene polymorphism association.
Keywords: vitamin D, vitamin D receptor gene polymorphisms, breast cancer, renal cancer
Contents
Introduction
Vitamin D and cancer
Vitamin D receptor
Common VDR polymorphisms and their associated alleles
Exploration of VDR polymorphisms
Ethnic variation is crucial in predicting effects of VDR gene polymorphisms
Vitamin D and breast cancer
Vitamin D and renal cancer
Search methods for the meta-analysis
Results of the meta-analysis
Concluding remarks
1. Introduction
Cancer is the leading cause of death worldwide, and accounted for 7.6 million deaths in 2008. The incidence of cancer continues to rise with an estimated 13.1 million deaths in 2030 (1). Breast cancer is a common disease and the leading cause of death among women around the world, with its incidence is increasing annually. It is estimated that 1 in 12 British women and 1 in 8 American women will develop breast cancer at some time in her life, the overall death ratio among women with this disease has been established at 20%, and the expected time of survival, at 5 years after the diagnosis (2). There are several constant risk factors for breast cancer, namely age, gender, density of breast tissue, benign breast conditions, early menarche, late menopause, previous chest exposure to radiation, exposure to diethylstilbestrol and genetic risk factors (BRCA-1 and BRCA-2) (3,4). As for the risk factors that may differ across patients, they include nulliparity or the first pregnancy after the age of 30, postmenopausal hormone treatment, combined use of estrogen and progesterone, breast feeding, alcohol consumption, postmenopausal obesity and insufficient physical activity (90). When renal cancer is taken into consideration, it accounts for 3% of total human malignancies and is the most common type of heterogeneous urological cancer with high prevalence in elderly men (>60 years old) (5). Because of the high mortality level due to metastasis (Czech Republic, Poland) renal cancer is considered to be one of the most important urological cancers in Central and Eastern Europe (6,89). There are several risk factors linked to the development of renal cancer, such as obesity, smoking, high blood pressure, ethnicity, age and family history or genetic risk factors [the most common one being the von Hippel-Lindau (VHL) syndrome] (7). Therefore, in this review we aimed to assess the correlation between the different alleles of VDR gene polymorphisms and renal cell cancer and breast cancer risks separately, through a systematic review of the present literature.
2. Vitamin D and cancer
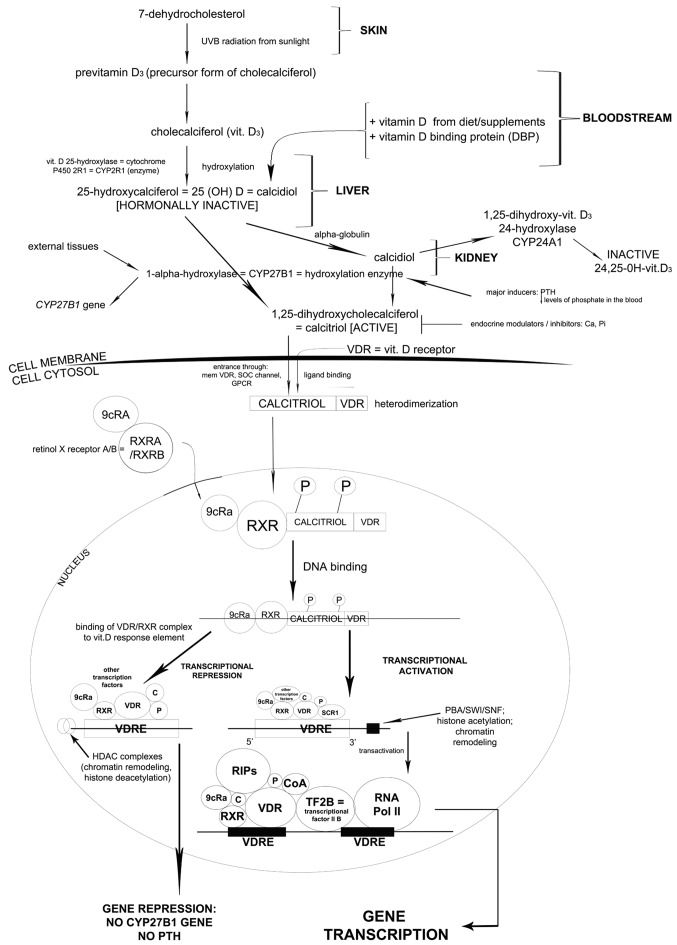
There are two major forms of vitamin D: D2 [calciferol or 1,24-dihydroxyvitamin D(2)] and D3 [calcitriol or 1,25-dihydroxyvitamin D(3)]. Anticancer properties have been attributed primarily to vitamin D3 (8). Vitamin D3 binds to the vitamin D receptor (VDR). This ligand-receptor complex regulates transcription of >60 genes involved in anti-proliferative, pro-differentiating, anti-metastatic and pro-apoptotic effects on cells and the cell cycle (Fig. 1: vitamin D conversion pathways) (9–12). In the mammary gland, vitamin D3 regulates calcium transport during lactation and acts together with mammary cell differentiation hormones and milk protein production (13). Laboratory studies have also demonstrated that vitamin D3 and its analogues inhibit cell proliferation and promote apoptosis in cancer cells in culture (14–18). These findings have led to the development of vitamin D analogues that could serve as potential new therapeutic agents in breast cancer treatment in humans. The observation of a reduced risk of breast cancer among women with high vitamin D status also supports the hypothesis that vitamin D plays a crucial role in cancer development (19–21). However, breast cancer is also known to be strongly influenced by the hormonal milieu and mutations in genes involved in hormone metabolism. The kidney has a unique function in mineral homeostasis especially for calcium and phosphorous. The vitamin D-endocrine system plays a key role in controlling the reabsorption of calcium by the kidney (22,23). The kidney is the major site for synthesis of vitamin D3 (24). Other vitamin D3-dependent proteins and the VDR that are important in calcium reabsorption are also expressed in the kidney (25,26). All in all, biological and epidemiological data suggest that vitamin D3 levels influence the development of renal cancer (27–29).
Figure 1.
7-Dehydrocholesterol undergoes specific alterations in the skin, liver and kidney. As a result calcitriol is formed and enters the cell cytosol through specific channels together with vitamin D receptor (VDR). After heterodimerization, the complex enters the nucleus and as a result, a multi-component complex is formed (phosphorylated calcitriol-VDR complex, retinol X receptor, 9cRa transcription factor) which subsequently binds to DNA. In the presence of HDAC complexes and other transcription factors, CYP27B1 gene responsible for parathormone production is repressed. However, in the presence of PBA/SWI/SNF complex other compounds are added (regulators of interaction, transcriptional factor IIB and most important of all, RNA polymerase II). As a consequence, CYP27B1 transcription occurs. The protein encoded by this gene localizes to the inner mitochondrial membrane where it hydroxylates 25-hydroxyvitamin D3 at the 1α position. This reaction synthesizes 1α,25-dihydroxyvitamin D3, the active form of vitamin D3, which binds to the VDR.
3. Vitamin D receptor
The VDR was discovered in 1969 (30). The VDR receptor gene is located on the long arm of chromosome 12 (12q12–14) with at least five promoter regions, and is composed of at least 11 exons that span 60 kb of DNA (31,32). The first exon is not translated (33), while exons 2–8 encode the VDR protein (Fig. 2). Polymorphisms of the VDR gene have been associated with several forms of cancer and other chronic diseases (30). The associations between the VDR gene polymorphisms and breast and renal cancers have been investigated by a number of studies (20,29,34–36). It has been postulated that the VDR gene polymorphisms may influence both the risk of cancer occurrence and its prognosis. The purpose of this review is to analyze the association of some common VDR gene polymorphisms, such as Taq1, Fok1, Apa1, Bsm1, Cdx2, poly(A) and Bgl1, with breast and renal cancers.
Figure 2.
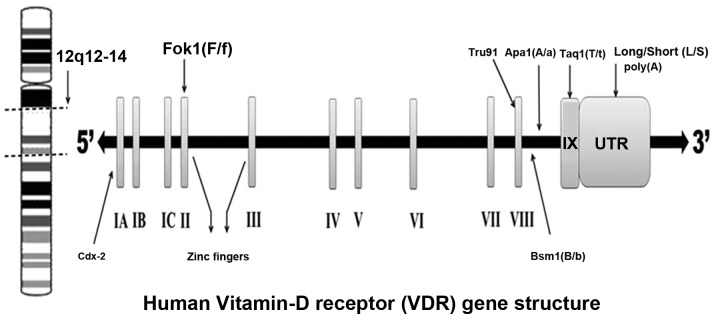
Human vitamin D receptor (VDR) gene polymorphic sites.
4. Common VDR polymorphisms and their associated alleles
Most studies on the VDR gene polymorphisms association with breast and renal cancers have focused on seven types of polymorphisms: Fok1 polymorphism in exon II (37), Bsm1 (38) and Apa1 (39) in intron VIII, Cdx2 (40) in exon I, Taq1 (41) in exon IX, Tru91 (42) in intron VIII, and the poly(A) (43) mono-nucleotide repeat in the 3’-untranslated region (3’-UTR) section of the gene. Individuals are generally classified as tt, Tt or TT for Taq1 polymorphism (T allele: absence of Taq1 restriction site; t allele: presence of Taq1 restriction site). The Fok1 polymorphism is located near the 5’-UTR region of the gene. The f allele for the Fok1 polymorphism shows less transcriptional activity than the F allele (44,45). All other polymorphisms have been found close to the 3’-UTR region of the gene (46). The polymorphisms in the 3’-UTR region of the gene appear to be in linkage disequilibrium (LD), and the allele frequencies for these polymorphisms appear to vary across populations (47). Individuals with the Bsm1 polymorphism are classified as bb, Bb, BB genotypes. With respect to poly(A), a bi-allelic polymorphism, an individual can be classified as: S (short, with <18 A’s) and L (long, with >168 A’s) poly(A) stretches (45). The individuals associated with Apa1 polymorphism are classified as aa, Aa and AA genotypes. In general, most of the polymorphisms in the VDR gene are located in regulatory areas rather than in the coding exons (48).
5. Exploration of VDR polymorphisms
The VDR polymorphisms that have been studied using the restriction fragment length polymorphism (RFLP) technique involve Apa1 (39), Bsm1 (38) and Taq1 (41) restriction polymorphisms at the 3’-end of the VDR gene. The Fok1 polymorphism occurs due to a thymine/cytosine (T/C) change (44). It basically alters an ACG codon to an ATG codon located ten base pairs upstream from the translation start codon, which results in the formation of an additional start codon. If protein translation starts from this altered site, a larger VDR protein with three additional amino acids will be formed (49). Taq1 is a substitution of nucleotide ATT for ATC in exon IX, leading to a synonymous change at codon 252 (isoleucine) (50,51). Although Bsm1 and Apa1 are considered as silent single nucleotide polymorphisms (SNPs) that do not change the sequence of coding amino acids like in Fok1 (52), they may influence gene expression through regulation of mRNA stability. The Cdx2 polymorphism is a guanine (G) to adenine (A) alteration in the promoter region of the VDR gene, specifically at the binding site for an intestinal specific transcription factor known as Cdx2 (53). The A allele binds to the Cdx2 transcription factor with a higher affinity, and yields increased transcriptional activity (40). As a consequence, the A allele may result in a higher VDR expression in the intestine, and therefore in an increased bone mineral density (BMD) through a better intestinal absorption of calcium (35,40,54). The poly(A) polymorphism occurs in the 3’-UTR region of the VDR gene, which is characterized by a variable number of tandem repeats (VNTR) (43). Finally, two polymorphisms, namely A-1012G and Tru91, have been poorly investigated. The A-1012G polymorphism consists in a substitution of A for G (55). The Tru91 is a G (U allele) to A (u allele) polymorphism in the VDR gene (42).
6. Ethnic variation is crucial in predicting effects of VDR gene polymorphisms
Genetic studies based on different ethnic backgrounds provide excellent opportunities to link molecular insight with epidemiological data (35). Variation in DNA sequences occurs frequently in the population, and has a substantial biological impact on the development of certain diseases, including cancer. The Cdx2 polymorphism was first discovered in the Japanese (40), and has recently been studied in a Caucasian population by Fang et al (54). However, the study revealed that the Cdx2 polymorphism A allele occurs more commonly in African (74%) and Asian (43%) populations than among the Caucasians (19%). The data obtained from their research has shown that the f allele for the Fok1 polymorphism occurs less frequently among the Africans (24%) than among the Caucasians (34%) and the Asians (51%), while the frequency of the B allele for Bsm1 is much lower in the Asian (7%) population than among the Caucasians (42%) and the Africans (36%) (35). On the other hand, the Apa1 A allele is exhibited at a higher frequency in the Asian population (74%) than among the Caucasians (44%) and Africans (31%).
The LD describes the co-occurrence of the alleles of adjacent polymorphisms. In consequence, the presence of one type of polymorphism may serve as indication of the presence of another polymorphism that is linked to it. It is noticeable due to a very slight recombination that has occurred between them during evolution. LD is present in the case of both Taq1 and poly(A), since they occur in similar ratios in different ethnic groups, with a lower percentage of the Taq1 T allele among Asians (8%) compared to Caucasians (43%) and Africans (31%); similar results have been observed for the poly(A) S allele, which is less frequent among the Asians (12%) than among the Caucasians (41%) and the Africans (29%) (52). In contrast to the Bsm-Apa-Taq haplotypes, haplotype 3 (bAT) is common among the African population (59%), while haplotype 1 (baT) and haplotype 2 (BAt) are mostly observed in Asian (75%) and Caucasian populations (39%) respectively (35).
7. Vitamin D and breast cancer
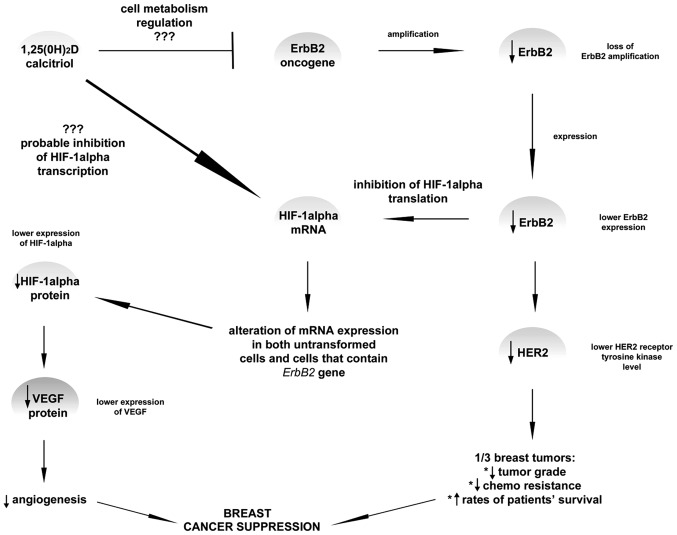
Currently, in vitro, preclinical and clinical findings support the hypothesis that low levels of vitamin D are linked to an increased risk of breast cancer (56). Anti-carcinogenic effects of vitamin D are mediated via the estrogen pathway by downregulation of the estrogen receptor (ER), which inhibits cancer cell proliferation, induces cell apoptosis, and prevents carcinogenesis in vitro and in animal models (57–59). On the other hand, epidemiological data also show that vitamin D supplementation in invasive breast cancer patients did not reduce breast cancer incidence in one trial conducted on post-menopausal women (60). These contradictory findings could be related to tumor heterogeneity, which suggests that effects of vitamin D may only be exhibited in specific subtypes of breast cancer. Therefore, additional functional experiments with vitamin D supplementation should be conducted on specific breast cancer subtypes and polymorphisms in the VDR gene and other gene variants (Fig. 3).
Figure 3.
It is known that vitamin D plays a crucial role in reducing the risk of breast cancer development, basically when the prevention of angiogenesis is taken into account. VEGF is a potent angiogenic factor which was shown in several publications to limit the vessels production due to the 1,25(0H)2D impact via the hypoxia-inducible factor-1α (HIF-α). It has been proposed that dihydroxyvitamin D does not directly affect VEGF expression. In some of the research, ErbB, a gene responsible for breast cancer invasiveness, has been shown to increase HER2 expression. Amplification or overexpression of this gene is perceived as one of the major factors contributing to pathogenesis and progression of certain aggressive types of breast cancer and in recent years it has become a significant biomarker and target of therapy for this disease. However, it was suggested that lower ErbB2 expression leads to the inhibition of HIF-α translation which subsequently leads probably to lower VEGF and HER2 expression. This means that higher rates of patient survival may be achieved. Currently, the role of calcitriol in connection with HIF-1α expression level is still not fully confirmed, however, inhibition mechanism appears to be the most probable among other theory. Moreover, ErbB2 is also probably inhibited by calcitriol; yet, the mechanism of such action is still unknown.
8. Vitamin D and renal cancer
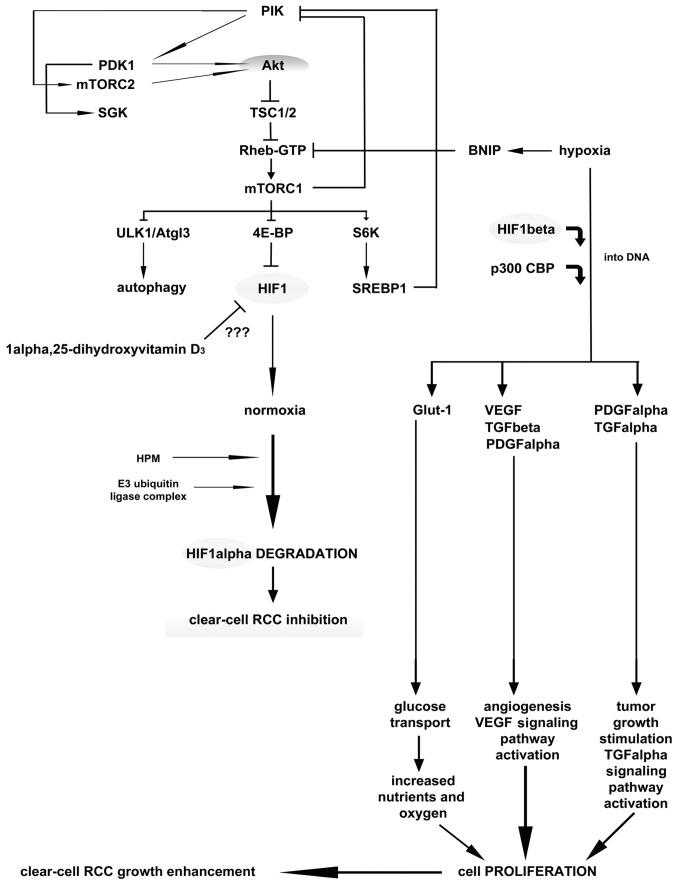
In the kidney, the major site of vitamin D3 formation, metabolism, activity and calcium homeostasis under physiological conditions is the renal proximal tubule (61). Epidemiological data suggest that vitamin D3, obtained either from dietary intake or as a result of the body’s exposure to ultraviolet light, is inversely correlated with renal cancer risk (62,63). Vitamin D3 serum concentrations have been found to be significantly decreased in patients with renal cancer compared to the control population (28,64). However, the exact role of anti-carcinogenic mechanism of vitamin D3 has not been studied widely nor is it completely understood. Nevertheless, it can be postulated that vitamin D3 impedes carcinogenesis via the VDR, and stimulates cell differentiation by inhibiting cell proliferation, inducing apoptosis and suppressing invasiveness, angiogenesis and metastasis (Fig. 4) (63,65,66). The kidney is the most vital organ for vitamin D metabolism and calcium homeostasis, though there is still scarcity of data on the association between dietary vitamin D3, VDR gene polymorphism and renal cancer etiology.
Figure 4.
RCC of clear cell type is the most common form of renal cancer. One of the factors which inhibits hypoxia in RCC is hypoxia-inducible factor-1α (HIF-α). It is unstable in normoxia with its half-life of <10 min. Hypoxia is a widely known mechanism of angiogenesis regulation. As a result of adaptation of cancer cells to hypoxia conditions, cancer cells in RCC gain resistance both to chemotherapy and radiotherapy. HIF-1α enhances cellular oxygen tension which in consequence leads to normoxia and subsequently HIF-1α degradation occurs. HIF transcription complex has been shown to induce the expression of among others, VEGF and PDGFα, which results in cell proliferation and tumor growth. However, the problem of the impact of hypoxia is a matter of different research and this article will not focus on this aspect of RCC. The other vital ATP consumer that contributes to hypoxia inhibition in mRNA translation process. Both mammalian target of rapamycin and pancreatic kinase (Eip2A) with the help of other transcription factors presented in the figure, take part in hypoxia regulation. The first one, which is a large serine/threonine protein kinase is also involved in homeostasis regulation as it controls catabolic and anabolic processes such as oxygen availability and growth factor signaling. mTOR complex 1 (mTORC1) is also responsible for its downstream actions which are autophagy regulation, protein synthesis and metabolic pathways control. Still, it is not clear how exactly vitamin D3 may inhibit the activation of HIF-1α. One of the hypothesis is that it participates in the regulation of blood vessel supply to the tumor, regulated by hypoxia/normoxia state.
9. Search methods for the meta-analysis
Strategies to recover the published data
Most epidemiological studies of breast and renal cancers have been concentrated on seven polymorphisms of the VDR gene that are potentially important for the cancer etiology. We performed a meta-analysis of the published literature using the PubMed Central® (PMC), a biomedical and life sciences journal literature from the National Library of Medicine (NLM). The search was conducted using literature data from January, 1997 until November, 2012. The search employed combinations of keywords ‘VDR gene polymorphisms’ with ‘breast cancer’ and ‘renal cell cancer’, as well as of the keywords: Fok1, Bsm1, Taq1, Apa1, poly(A), Cdx2, Bgl1, A-1012G and Tru91 with ‘breast cancer’ and ‘renal cell cancer’. In the case of breast cancer, 52 results were generated, while only 12 results were found in the case of VDR polymorphisms and renal cancer.
10. Results of the meta-analysis
Fok1 polymorphism vs. breast cancer and renal cancer
Fok1 polymorphism and breast cancer
Most of the case control studies performed on different ethnic populations did not show that the risk of breast cancer was associated with the Fok1 polymorphism (34,67–70). An analysis conducted recently on Chinese women also supported this statement (70). The Fok1 polymorphism was not found to be associated with breast cancer when analyzed separately. However, Fok1 did modulate the increased risk of other VDR genotypes (bb/LL genotype Bsm1 b allele, poly(A) L allele) together with the bb/LL genotype, which resulted in an increased breast cancer risk (68). In one population-based case control study, no effect of the concentration of 25(OH)D serum and VDR genotype was observed, and none of the analyzed polymorphisms were correlated with breast cancer risk (34). Another study conducted among the UK Caucasian population showed similar results, with no association of Fok1 with breast cancer (67). In the investigations conducted on 500 breast cancer cases in post-menopausal women and 500 controls matched by age, ethnicity and blood collection date, similar results were obtained (71). Others have also obtained the same result in their analysis (20). Curran et al (72) have shown in the Australian population that VDR initiation codon Fok1 polymorphism is not associated with breast cancer occurrence. Interestingly, a significantly increased risk of breast cancer was observed in one large study (1,234 cases and 1,676 controls) among carriers of the ff genotype of Fok1 (multivariate OR=1.34) compared with those with the FF genotype (73). In that study, the Fok1 association was influenced by the menopausal status, estrogen, the progesterone receptor status of the tumors, and plasma levels of 25(OH)D or 1,25(OH)2D3. Furthermore, a meta-analysis of 21 case-control studies with Fok1, Bsm1, Apa1 and Taq1 polymorphisms has shown that the Fok1 polymorphism was associated with an increased risk of breast cancer development (ff vs. FF: OR=1.15; 95% CI, 1.03–1.28; the recessive model ff vs. Ff + FF: OR=1.14; 95% CI, 1.03–1.26) (74), while in a sub-analysis a significant association was found between the Fok1 polymorphism and breast cancer in the European population. Current meta-analysis has shown that Fok1 may serve as a diagnostic biomarker for breast cancer susceptibility especially in the European population. Taking all these factors into consideration, the above studies showed an uncertain association of Fok1 with breast cancer. Further studies are still needed to clarify the observations based on the Fok1 polymorphism association with that cancer. Table I summarizes the reference analysis of the Fok1 polymorphism association with breast cancer.
Table I.
Fok1 and breast cancer.
| Population studied | Study type | Polymorphism | Cases/controls | Results | Refs. |
|---|---|---|---|---|---|
| Latinas | CCS | Fok1, Bsm1, poly(A) | 143/300 | No association | (69) |
| Caucasian | CCS | Fok1, Bsm1 | 313/410 | No association | (77) |
| Caucasian | CCS | Fok1, Bsm1, poly(A) | 398/427 | No association | (68) |
| Caucasian | CCS | Fok1, Bsm1, poly(A) | 181/241 | No association | (67) |
| German | PCCS | Fok1, Taq1, Cdx2, VDR-5132 | 1408/2612 | No association | (34) |
| Caucasian | NCCS | Fok1, Bsm1, Taq1, Apa1, poly(A) | 500/500 | No association | (71) |
| Australian | CCS | Fok1, Taq1, Apa1 | 135/410 | No association | (72) |
| USA | CCS | Fok1 | 1234/1676 | The ff genotype associated with breast cancer risk | (73) |
| French Canadian | CCS | Fok1, Bsm1 | Two independent studies (225/463 and 622/974) | The ff genotype linked to higher breast cancer risk | (78) |
| Hispanic, non-Hispanic | CCS | Fok1, Taq1, Bgl1 | 814/910 | No association | (20) |
| Chinese | PCCS | Fok1, Bsm1, CYP24A1 | 2919/2313 | No association | (70) |
CCS, case-control study; PCCS, population-based case-control study; NCCS, nested case-control study.
Fok1 polymorphism and renal cancer
The association of Fok1 with renal cell cancer has not been studied widely. The scarce published data comprise the analysis of Fok1 and its role in renal cell cancer development; however, a recent study yielded contradictory results, it was conducted in Central and Eastern Europe, and showed that the subjects over 60 years of age who were carriers of the f alleles in the Fok1 SNP had reduced renal cancer risk compared to the subjects with the FF genotype (75). However, recent research on the North Indian population has shown contradictory findings, in which an increased number of the Fok1 polymorphism alleles was linked to a high risk of renal cell cancer considering other risk factors, such as: hypertension, smoking and improper body mass index (BMI) (76). These results show the association of Fok1 polymorphism with renal cancer. However, the result varies depending on the ethnic background, so further research is needed for confirmation. Table II summarizes the reference analysis of the Fok1 polymorphism association with renal cancer.
Table II.
Fok1 and renal cancer.
| Population studied | Study type | Polymorphism | Cases/controls | Results | Refs. |
|---|---|---|---|---|---|
| Central and Eastern European | CCS | Fok1, Bsm1, Taq1 | 925/1192 | The f allele associated with renal cancer risk | (75) |
| Indian | CCS | Fok1, Bsm1 | 196/250 | The ff genotype associated with high renal cancer risk | (76) |
CCS, case-control study.
Bsm1 polymorphism vs. breast cancer and renal cancer
Bsm1 polymorphism and breast cancer
A strong association has been found between the bb genotype of the Bsm1 VDR polymorphism and increased breast cancer incidence. A great number of research studies have been published to support this statement, but some conclusions differed across the individual authors and ethnic groups. Research based on UK Caucasian women has shown a 1.8-fold increase of cancer risk for the bb genotype individuals (OR=1.79) (77). In addition, >70% of seven commonly used breast cancer cell lines have been found to possess the risky bb genotype. Guy et al (68) have further confirmed that Bsm1 is associated with a high risk of breast cancer development, and the likelihood of developing breast cancer is nearly twice higher for a woman with the bb genotype than for a woman with BB or Bb genotype (bb genotype OR=1.92; BB genotype OR=1.00; and Bb genotype OR=1.00). Similar results have been reported for the Caucasian women, but not for the African-American women, where this polymorphism increased the risk of breast cancer development in postmenopausal carriers of the bb genotype of Bsm1 (OR=1.53) (78). It is also worth noticing that the smoking status modified this association of Bsm1 genotype and breast cancer risk. Premenopausal Caucasian women who had reported smoking at least once had an increased risk of breast cancer. However, there was no such association in case of the smoking habit among postmenopausal Caucasian women, premenopausal African-American women or postmenopausal African-American women. The respective association between Bsm1 genotypes and breast cancer risk does not vary significantly with oral contraceptive use, hormone replacement therapy, or BMI (78).
Another study has reported that the Bsm1 polymorphism was in LD with the poly(A) sequence in the 3’-non-translated region, and the ‘L’ poly(A) variant was also associated with breast cancer susceptibility similarly to Bsm1 (bb vs. BB genotype OR=2.32) (67). The study by Lowe et al (12) also reported that low levels of circulating 25(OH)D (<50 nM) occurring in association with the bb Bsm1 VDR genotype may increase the risk of breast cancer more than levels of 25(OH)D >50 nM in either the BB or the Bb genotype. Another study shows that VDR polymorphism Bsm1 distributions in the case group and in the control group of patients did not exhibit any statistical difference. On the other hand, the metastatic cancer group with prevalence of the bb genotype (14/38; 37%) was twice as large as the corresponding percentage of control subjects, whereas the percentage of BB women with metastases was half lower than in the control group (2/38; 5%) (79). Moreover, homozygous bb women have been shown to develop metastases four times more often than BB women.
Ingles et al (69) have reported that when the bb genotype was compared with the Bb and BB genotypes separately, it was shown to have a 1.6- and 2.2-fold increased breast cancer risk, respectively. In Taiwanese women, the Bsm1 B allele was also associated with an increased breast cancer risk (80). The data showed that 79% of the breast cancer group and 76% of the benign breast tumor group had the bb genotype compared to 91% of the control population. Only 9% of the control population had the B allele, in contrast to the breast cancer group (21%) and the benign breast tumor group (24%), which supports the B allele association with an increased breast cancer risk. However, a number of studies have also yielded conflicting data on association of the Bsm1 VDR polymorphism with breast cancer risk. Two independent case-control studies conducted on the same population have shown that the Bsm1 Bb + bb genotype is not associated with an increased risk of breast cancer in the French Canadian population (OR=1.22) without interaction with family history (81). Similar results have been obtained by another group, who has shown the absence of any significant association between Bsm1 polymorphisms and breast cancer development on a small group (78 patients) of the Turkish population (82). In Caucasian women, no association was found between polymorphisms in Bsm1 and breast cancer risk, OR=0.93 for BB vs. bb (73). However, these results suggest that the VDR polymorphism may be a mediator of cancer risk, and could be a target for cancer prevention efforts. Some results showed that breast cancer incidence was not associated with any genotype (71). However, women with the Bsm1 bb genotype that consumed >902 mg/day of calcium had lower susceptibility to breast cancer than those with the Bb or BB genotype (OR=0.61). In conclusion, the Bsm1 bb genotype is associated with breast cancer risk in Caucasian and African-American women, despite the fact that this association is influenced by other factors, such as smoking. Table III summarizes the reference analysis of the Bsm1 polymorphism association with breast cancer.
Table III.
Bsm1 and breast cancer.
| Population studied | Study type | Polymorphism | Cases/controls | Results | Refs. |
|---|---|---|---|---|---|
| Caucasian | CCS | Bsm1, Fok1 | 313/410 | The bb genotype is associated with high breast cancer risk | (77) |
| Caucasian | CCS | Bsm1, Fok1, poly(A) | 398/427 | Breast cancer occurrence among women with the bb genotype is twice higher than among women with the BB or Bb genotypes | (68) |
| Caucasian, African-American | PCCS | Bsm1, poly(A) | 1631/1435 | Postmenopausal Caucasian women with the bb genotype are at higher risk of developing breast cancer | (79) |
| Caucasian | CCS | Bsm1, Fok1 | 1180/1547 | No association | (73) |
| Caucasian | CCS | Bsm1, Fok1, poly(A) | 181/241 | Bsm1 is LD with poly(A) and is associated with breast cancer | (67) |
| Caucasian | CCS | Bsm1 | 179/179 | Low level of 25(OH)D and the bb genotype increase breast cancer susceptibility | (12) |
| French Canadian population | CCS | Bsm1, Fok1 | Two independent study (225/463 and 622/974) | Bb + bb was associated with slightly increased risk of breast cancer in both studies | (78) |
| Italian | CCS | Bsm1 | 88/167 | Women with homozygous bb are at higher risk of developing metastases of breast cancer than BB women | (80) |
| Turkish | CCS | Bsm1, Taq1 | 78/27 | No association | (82) |
| Caucasian | NCCS | Bsm1, Fok1, Taq1, Apa1, poly(A) | 500/500 | No association | (71) |
| Taiwanese | CCS | Bsm1, Taq1, Apa1 | 80/169 | The B allele is associated with breast cancer | (81) |
| Latinas | CCS | Bsm1, Fok1, poly(A) | 143/500 | The bb genotype is associated with higher breast cancer risk than BB and Bb | (69) |
| Chinese | PCCS | Fok1, Bsm1, CYP24A1 | 2919/2313 | No association | (70) |
CCS, case-control study; PCCS, population-based case-control study; NCCS, nested case-control study; LD, linkage disequilibrium.
Bsm1 polymorphism and renal cancer
Although many detailed studies have been conducted in the field of renal cell cancer, more data are undoubtedly required to determine the importance of the Bsm1 polymorphism association with renal cell cancer development. Only a few studies have been published that showed its connection with renal cancer. A previously conducted study in the Japanese population showed that the Bsm1 variant did not have any statistically significant effect on the risk of renal cancer (36). However, when the BB genotype of the Bsm1 gene polymorphism was analyzed in Central and Eastern Europe, an individual with a positive family history of cancer had a lower renal cancer risk compared to an individual with the bb allele (75). Similar results have been obtained for the Indian population, showing that Bsm1 polymorphism (bb genotype) can significantly modify the risk of renal cancer (76). All these findings show the potential of Bsm1 in predicting the risk of developing renal cell cancer, though further studies taking into consideration other ethnic groups are needed for confirmation. Table IV summarizes the reference analysis of the Bsm1 polymorphism association with renal cancer.
Table IV.
Bsm1 and renal cancer.
| Population studied | Study type | Polymorphism | Cases/controls | Results | Refs. |
|---|---|---|---|---|---|
| Japanese | CCS | Bsm1, Apa1, Taq1 | 135/150 | Bsm1 variant not found to be associated with renal cancer | (36) |
| Central and Eastern European | CCS | Bsm1, Fok1, Taq1 | 925/1192 | The BB genotype is associated with lower risk of renal cancer occurrence | (75) |
| Indian | CCS | Bsm1, Fok1 | 196/250 | The bb genotype is associated with lower risk of renal cancer | (76) |
CCS, case-control study.
Taq1 polymorphism vs. breast cancer and renal cancer
Taq1 polymorphism and breast cancer
A large number of studies have shown the absence of any association between the Taq1 VDR polymorphism and breast cancer susceptibility. A population-based case-control study (PCCS) has revealed that high sun exposure reduces the risk of advanced breast cancer development among women with light constitutive skin pigmentation (OR=0.53), and that this association does not depend on the Taq1 VDR genotype (20). Similar results showing no significant association between breast cancer risk and the Taq1 genotype have been obtained in different ethnic backgrounds (71,82–84). In the Taiwanese population, where low frequency of breast cancer was found, no association of Taq1 with breast cancer has been established (80). On the other hand, a tendency for a decreased risk of breast cancer has been observed for the Taq1 T allele (OR=0.68), but proper estimation of the potential impact of Taq1 polymorphism on breast cancer was impossible to perform (85). A number of Taq1 analyses comprising the Taq1 polymorphism in combination with dietary factors have also been reported. Women with the TT genotype who consumed >902 mg total calcium per day exhibited lower breast cancer risk compared to genotypes Tt or tt (71). The Taq1 polymorphism association with a significantly increased risk of estrogen receptor positive tumors (OR=1.18) for t allele carriers compared to non-carriers (OR=0.88) has also been reported (34,52). In a case-control study (CCS) of Australian women, a tendency for the Taq1 T allele association with an ∼1.5-fold increased breast cancer risk has been found (72). Finally, for patients with the TT genotype, a significantly increased risk (OR=1.8) for lymph node metastasis has been reported. Furthermore, among patients with the tt genotype, a tendency towards prolonged survival has been noted among ER-positive, tamoxifen-treated patients (86). In conclusion, polymorphisms in the VDR gene may influence tumor progression and tamoxifen treatment response in early-onset breast carcinomas (86). It appears that the T allele is a ‘risk allele’, while the t allele is a ‘protective allele’. Table V summarizes the reference analysis of the Taq1 polymorphism association with breast cancer.
Table V.
Taq1 and breast cancer.
| Population studied | Study type | Polymorphism | Cases/controls | Results | Refs. |
|---|---|---|---|---|---|
| Hispanic, non-Hispanic | CCS | Taq1, Fok1, Bgl1 | 814/910 | No association | (20) |
| Caucasian | NCCS | Taq1, Fok1, Bsm1, Apa1, poly(A) | 500/500 | Women with the TT genotype consuming 902 mg/day calcium have lower risk | (71) |
| Caucasian | CCS | Taq1 | 951/627 | No association | (83) |
| Turkish | CCS | Taq1, Bsm1 | 78/27 | Taq1 polymorphism in VDR gene is not linked to breast cancer susceptibility | (84) |
| Taiwanese | CCS | Taq1, Bsm1, Apa1 | 80/169 | No association | (81) |
| Finnish | CCS | Taq1, Apa1 | 483/482 | The T allele is associated with lower breast cancer incidence | (86) |
| German | PCCS | Taq1, Fok1, Cdx2, VDR-5132 | 1408/2612 | In estrogen receptor positive tumor, the t allele is linked to increased risk of breast cancer | (34) |
| Australian | CCS | Taq1, Fok1, Apa1 | 135/410 | The TT genotype is associated with breast cancer | (72) |
| Swedish | CCS | Taq1 | 111/130 | The tt genotype is associated with prolonged survival in breast cancer patients | (87) |
| Indian | CCS | Taq1, Apa1, Poly(A) | 160/140 | No association | (85) |
CCS, case-control study, PCCS; population-based case-control study; NCCS, nested case-control study; VDR, vitamin D receptor.
Taq1 polymorphism and renal cancer
There is scarce data concerning the effect of the Taq1 polymorphism on renal cancer occurrence and outcome. A lower risk of renal cancer has been observed among individuals with the t allele in the Taq1 gene polymorphism in the Central and Eastern European population (75), and this polymorphism was not differentiated by the tumor stage or grade. Previously, a study of the Japanese population has also been carried out, revealing that: i) the TT genotype was statistically more frequent among renal cancer patients (80.4%); ii) TT frequency was higher compared to rapid tumor growth type group (92.1%) and slow tumor growth type group (73.4%) (87). All these analyses have shown that the T allele is associated with determining the risk of developing renal cancer. On the contrary, a recent study of the Japanese population has shown contradictory results, and has not found any statistical difference (36). Therefore, further research is needed on the basis of cancer stage to define or confirm the role of the T allele in renal cancer risk. Table VI summarizes the reference analysis of the Taq1 polymorphism association with renal cancer.
Table VI.
Taq1 and renal cancer.
| Population studied | Study type | Polymorphism | Cases/controls | Results | Refs. |
|---|---|---|---|---|---|
| Central and Eastern European | CCS | Taq1, Bsm1, Fok1 | 925/1192 | Lower risk is associated with the Taq1 t variant | (75) |
| Japanese | CCS | Taq1 | 102/204 | The TT genotype is more frequent in renal cancer patients | (88) |
| Japanese | CCS | Taq1, Bsm1, Apa1 | 135/150 | No association | (36) |
CCS, case-control study.
Apa1 polymorphism vs. breast cancer and renal cancer
Apa1 polymorphism and breast cancer
The association of Apa1 with breast cancer has not been widely studied. Different approaches towards the Apa1 association analysis have been used, and some studies have revealed that the Aa and aa genotypes were significantly associated with an increased breast cancer risk (OR=1.56) (72). Contradictory results have been obtained among the Taiwanese population (80). Those results have shown that the AA genotype has a tendency to increase cancer risk, whereas decreasing copies of the A allele have been found to be associated with a reduced cancer risk (OR=0.333 for the Aa genotype and OR=0.515 for the aa genotype). In other studies conducted on the Finnish population, a statistically significant difference was observed in the Apa1 genotype distribution between the cases and the controls (85). Women with the VDR variant ‘a’ genotypes had a decreased risk of breast cancer (OR=0.73) compared with women carrying the AA genotype. If the family history of breast cancer was taken into consideration, this association became strong (OR=0.14). The results also suggest that the AA genotype is more common among women with breast cancer, whereas the lowest risk of breast cancer is found in women with the aa genotype (OR=0.03) (85). On the other hand, other research groups have not found such an association (71,84). In conclusion, the Apa1 allele association has not been analyzed widely in different racial groups, but in most of the studies it has been found to be linked with breast cancer risk. Table VII summarizes the reference analysis of the Apa1 polymorphism association with breast cancer.
Table VII.
Apa1 and breast cancer.
| Population studied | Study type | Polymorphism | Cases/controls | Results | Refs. |
|---|---|---|---|---|---|
| Australian | CCS | Apa1, Fok1, Taq1 | 135/410 | The Aa and aa genotypes are associated with breast cancer risk | (72) |
| Taiwanese | CCS | Apa1, Bsm1, Taq1 | 80/169 | The AA genotype is associated with breast cancer risk | (81) |
| Finnish | CCS | Apa1, Taq1, Apa1 | 483/482 | Variant ‘a’ genotype is linked to lower risk | (86) |
| Caucasian | NCCS | Apa1, Bsm1, Fok1, Taq1, poly(A) | 500/500 | No association | (71) |
| Indian | CCS | Apa1, Taq1, poly(A) | 160/140 | No association | (85) |
CCS, case-control study; PCCS, population-based case-control study; NCCS, nested case-control study.
Apa1 polymorphism and renal cancer
Only one study on the Japanese population has analysed the association between renal cancer and the AA genotype of the Apa1 polymorphism in the VDR gene (36). The frequency of the AA genotype has been found to be significantly higher in renal cancer patients (17.0%) than in the control group (7.3%). More than half (52.2%) of the patients with the AA genotype had distant or lymph node metastases compared to the Aa + aa genotypes (6.3%). Moreover, patients with the AA genotype were found to have poor survival rates compared to patients with other genotypes (Aa + aa). In conclusion, these findings suggest that the AA genotype may influence disease progression and prognosis of renal cancer; however, these results are limited to a certain ethnic background. Thus, further research concerning the Apa1 polymorphism for other populations are necessary. Table VIII summarizes the reference analysis of the Apa1 polymorphism association with renal cancer.
Table VIII.
Apa1 and renal cancer.
| Population studied | Study type | Polymorphism | Cases/controls | Results | Refs. |
|---|---|---|---|---|---|
| Japanese | CCS | Taq1, Bsm1, Apa1 | 135/150 | AA genotype is frequent in renal cancer cases | (36) |
CCS, case-control study.
Poly(A) polymorphism vs. breast cancer and renal cancer
Poly(A) polymorphism and breast cancer
The claim concerning the presence of an association between the poly(A) polymorphism and breast cancer occurrence is controversial. In a recent study carried out on the Swedish population, women carrying two short poly(A) alleles (SS genotype) were found to have an increased risk of breast cancer incidence (OR=1.26) (88). There was a statistically significant interaction between the VDR genotype and parity; women with two short alleles (SS) had a halved risk of breast cancer, irrespective of the parity, compared with nulliparous women with two long alleles (LL). On the other hand, homozygosity for the long VDR allele (LL) was associated with a more advanced clinical stage at diagnosis (88). With respect to a previous study, when the LL genotype was compared to the S genotype with an increased number of short poly(A) alleles, a higher risk of developing cancer was associated with the number of S variants (OR=1.5 for the SL genotype and OR=3.2 for the SS genotype) (69). Some other studies carried out on Caucasian women also suggested the association of poly(A) with breast cancer (67). The poly(A) variant L was associated with an increase of breast cancer risk because, poly(A) was in LD with the Bsm1 polymorphism (67). Similar results have also been obtained by another group (OR=1.94 for LL vs. SS genotype) (68). Some studies have also yielded contradictory results for the poly(A) genotype (71). However, women with the poly(A) (LL) repeat who consumed more than 902 mg/day of calcium exhibited decreased risk of breast cancer incidence (71). On the other hand, breast cancer and the poly(A) genotype were not found to be associated in a recent study on a group of Caucasian and African-American women (78). It has been found that the association of poly(A) with breast cancer can be modified by the smoking status, but it did not significantly vary with oral contraceptive use, hormone replacement therapy, or BMI (78). In conclusion, the role of poly(A) is still controversial, but the variant LL allele is associated with breast cancer risk, though further confirmation is undoubtedly needed. Table IX summarizes the reference analysis of the poly(A) polymorphism association with breast cancer.
Table IX.
Poly(A), Cdx2, Bgl1 and breast cancer.
| Population studied | Study type | Polymorphism | Cases/controls | Results | Refs. |
|---|---|---|---|---|---|
| Swedish | PCCS | Poly(A) | 1502/1510 | The SS genotype is associated with breast cancer | (89) |
| Latinas | CCS | Poly(A), Bsm1, Fok1 | 143/500 | Two SS allele of the poly(A) polymorphism are associated with breast cancer risk | (69) |
| Caucasian | CCS | Poly(A), Bsm1, Fok1 | 181/241 | The poly(A) L variant is in LD with Bsm1 and is associated with breast cancer | (67) |
| Caucasian | CCS | Poly(A), Bsm1, Fok1 | 398/427 | The poly(A) LL genotype is associated with breast cancer | (68) |
| Caucasian | NCCS | Poly(A), Bsm1, Fok1, Apa1, Taq1 | 500/500 | Poly(A) LL positive women can decrease breast cancer risk by consuming 902 mg calcium/day | (71) |
| Caucasian, African-American | PCCS | Poly(A), Bsm1 | 1631/1435 | No association with poly(A) | (79) |
| Indian | CCS | Poly(A), Apa1, Taq1 | 160/140 | The long poly(A) L allele is associated with breast cancer | (85) |
| German | PCCS | Cdx2, Fok1, Taq1, VDR-5132 | 1408/2612 | Cdx2 is not associated with breast cancer | (34) |
| Hispanic, non-Hispanic | CCS | Bgl1, Fok1, Taq1 | 814/910 | The Bgl1 BB genotype is associated with the decrease of breast cancer development in a group of women with medium pigmentation | (20) |
CCS, case-control study; PCCS, population-based case-control study; NCCS, nested case-control study; LD, linkage disequilibrium.
Poly(A) polymorphism and renal cancer
No specific data basis has been found so far to demonstrate a direct association of poly(A) with the risk of renal cancer. However, some studies have found a correlation between Taq1 and the poly(A) polymorphism, which are in LD with each other in the Asian, Caucasian and African populations (35). A lower risk of renal cancer has been observed for the t allele of the Taq1 gene polymorphism (75,87). All these studies examined solely the role of the Taq1 polymorphism on its own. However, it is feasible that poly(A) may show an important role in renal cancer development when studied together with the Taq1 polymorphism.
Cdx2 and Bgl1 polymorphism vs. breast cancer and renal cancer
Cdx2 and Bgl1 polymorphism and breast cancer
Undoubtedly, not enough work has been done on the potential functional association between Cdx, Bgl1 and breast cancer risk. No LD has been found between the Cdx2 and other VDR genes (Fok1, Taq1 and VDR-5132) with respect to the breast cancer risk (34). In a PCCS carried out on various racial groups, such as Hispanic, African-American and non-Hispanic Caucasians, similar results were obtained for the linkage of Bgl1 to breast cancer risk (20). High exposure to sunlight was linked with reduced risk of breast cancer among women with light constitutive skin pigmentation (OR=0.53), but not among women with medium or dark pigmentation (20). In conclusion, the data on VDR Cdx and Bgl1 polymorphism are still limited.
Cdx2 and Bgl1 polymorphism and renal cancer
There are no published data so far that would describe the role of Cdx2 and Bgl1 with regard to the risk of developing renal cell cancer. Table IX summarizes the reference analysis of the Cdx2 and Bgl1 polymorphism association with breast cancer.
11. Concluding remarks
In this study we have analyzed the polymorphisms in the VDR gene occurring most commonly in breast cancer and renal cancer. Based on the set of data collected from different studies performed on different ethnic populations, it is not possible to make an authoritative declaration on the role of VDR polymorphisms in breast and renal cancer development and prognosis. However, some polymorphisms have been found to be strongly associated with breast cancer and some with renal cancer. Understanding the role of VDR polymorphisms provides mechanistic insight and may facilitate the development of new preventive strategies for breast and renal cancer.
Acknowledgments
This study was supported by grant TEAM/2010-6/8 of the Foundation for Polish Science Team Programme co-financed by the European Regional Development Fund, Operational Program Innovative Economy 2007–2013.
Abbreviations:
- CCS
case-control study;
- PCCS
population-based case-control study;
- NCCS
nested case-control study;
- OR
odds ratio;
- UV-B
ultraviolet radiation;
- VDR
vitamin D receptor;
- LD
linkage disequilibrium;
- Bsm1 alleles
(B, b);
- poly(A) alleles
[L (long), S (short)];
- Apa1 alleles
(A, a);
- Taq1 alleles
(T, t);
- Fok1 alleles
(F, f);
- RFLP
restriction fragment length polymorphism
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Pharoah PDP, Mackay J. Absolute risk of breast cancer in women at increased risk: a more useful clinical measure than relative risk? Breast. 1998;7:255–259. [Google Scholar]
- 3.Czarnecka AM, Klemba A, Krawczyk T, et al. Mitochondrial NADH-dehydrogenase polymorphisms as sporadic breast cancer risk factor. Oncol Rep. 2010;23:531–535. [PubMed] [Google Scholar]
- 4.Najm MZ, Zaidi S, Siddiqui WA, Husain SA. Immunohistochemical expression and mutation study of Prohibitin gene in Indian female breast cancer cases. Med Oncol. 2013;30:614. doi: 10.1007/s12032-013-0614-8. [DOI] [PubMed] [Google Scholar]
- 5.Porta C, Bellmunt J, Eisen T, Szczylik C, Mulders P. Treating the individual: The need for a patient-focused approach to the management of renal cell carcinoma. Cancer Treat Rev. 2010;36:16–23. doi: 10.1016/j.ctrv.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Hung RJ, Moore L, Boffetta P, et al. Family history and the risk of kidney cancer: a multicenter case-control study in Central Europe. Cancer Epidemiol Biomarkers Prev. 2007;16:1287–1290. doi: 10.1158/1055-9965.EPI-06-0963. [DOI] [PubMed] [Google Scholar]
- 7.Chow WH, Dong LM, Devesa SS. Epidemiology and risk factors for kidney cancer. Nat Rev Urol. 2010;7:245–257. doi: 10.1038/nrurol.2010.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krishnan AV, Trump DL, Johnson CS, Feldman D. The role of vitamin D in cancer prevention and treatment. Endocrinol Metab Clin North Am. 2010;39:401–418. doi: 10.1016/j.ecl.2010.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ali MM, Vaidya V. Vitamin D and cancer. J Cancer Res Ther. 2007;3:225–230. doi: 10.4103/0973-1482.38998. [DOI] [PubMed] [Google Scholar]
- 10.Simboli-Campbell M, Narvaez CJ, Tenniswood M, Welsh J. 1,25-dihydroxyvitamin D-3 induces morphological and biochemical markers of apoptosis in MCF-7 breast cancer cells. J Steroid Biochem Mol Biol. 1996;58:367–376. doi: 10.1016/0960-0760(96)00055-6. [DOI] [PubMed] [Google Scholar]
- 11.Thibault F, Cancel-Tassin G, Cussenot O. Low penetrance genetic susceptibility to kidney cancer. BJU Int. 2006;98:735–738. doi: 10.1111/j.1464-410X.2006.06351.x. [DOI] [PubMed] [Google Scholar]
- 12.Lowe LC, Guy M, Mansi JL, et al. Plasma 25-hydroxy vitamin D concentrations, vitamin D receptor genotype and breast cancer risk in a UK Caucasian population. Eur J Cancer. 2005;41:1164–1169. doi: 10.1016/j.ejca.2005.01.017. [DOI] [PubMed] [Google Scholar]
- 13.Bhattacharjee M, Wientroub S, Vonderhaar BK. Milk protein synthesis by mammary glands of vitamin D-deficient mice. Endocrinology. 1987;121:865–874. doi: 10.1210/endo-121-3-865. [DOI] [PubMed] [Google Scholar]
- 14.Chouvet C, Vicard E, Devonec M, Saez S. 1,25-Dihydroxyvitamin D3 inhibitory effect on the growth of two human breast cancer cell lines (MCF-7, BT-20) J Steroid Biochem. 1986;24:373–376. doi: 10.1016/0022-4731(86)90085-3. [DOI] [PubMed] [Google Scholar]
- 15.Eisman JA, Sutherland RL, McMenemy ML, Fragonas JC, Musgrove EA, Pang GY. Effects of 1,25-dihydroxyvitamin D3 on cell-cycle kinetics of T 47D human breast cancer cells. J Cell Physiol. 1989;138:611–616. doi: 10.1002/jcp.1041380323. [DOI] [PubMed] [Google Scholar]
- 16.James SY, Mackay AG, Colston KW. Vitamin D derivatives in combination with 9-cis retinoic acid promote active cell death in breast cancer cells. J Mol Endocrinol. 1995;14:391–394. doi: 10.1677/jme.0.0140391. [DOI] [PubMed] [Google Scholar]
- 17.Welsh J, Wietzke JA, Zinser GM, et al. Impact of the Vitamin D3 receptor on growth-regulatory pathways in mammary gland and breast cancer. J Steroid Biochem Mol Biol. 2002;83:85–92. doi: 10.1016/s0960-0760(02)00277-7. [DOI] [PubMed] [Google Scholar]
- 18.Sergeev IN. Vitamin D and cellular Ca2+ signaling in breast cancer. Anticancer Res. 2012;32:299–302. [PubMed] [Google Scholar]
- 19.Freedman DM, Looker AC, Chang SC, Graubard BI. Prospective study of serum vitamin D and cancer mortality in the United States. J Natl Cancer Inst. 2007;99:1594–1602. doi: 10.1093/jnci/djm204. [DOI] [PubMed] [Google Scholar]
- 20.John EM, Schwartz GG, Koo J, Wang W, Ingles SA. Sun exposure, vitamin D receptor gene polymorphisms, and breast cancer risk in a multiethnic population. Am J Epidemiol. 2007;166:1409–1419. doi: 10.1093/aje/kwm259. [DOI] [PubMed] [Google Scholar]
- 21.Shao T, Klein P, Grossbard ML. Vitamin D and breast cancer. Oncologist. 2012;17:36–45. doi: 10.1634/theoncologist.2011-0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Friedman PA, Gesek FA. Cellular calcium transport in renal epithelia: measurement, mechanisms, and regulation. Physiol Rev. 1995;75:429–471. doi: 10.1152/physrev.1995.75.3.429. [DOI] [PubMed] [Google Scholar]
- 23.Kumar R. Calcium transport in epithelial cells of the intestine and kidney. J Cell Biochem. 1995;57:392–398. doi: 10.1002/jcb.240570304. [DOI] [PubMed] [Google Scholar]
- 24.Gray R, Boyle I, DeLuca HF. Vitamin D metabolism: the role of kidney tissue. Science. 1971;172:1232–1234. doi: 10.1126/science.172.3989.1232. [DOI] [PubMed] [Google Scholar]
- 25.Tanaka Y, DeLuca HF. Rat renal 25-hydroxyvitamin D3 1- and 24-hydroxylases: their in vivo regulation. Am J Physiol. 1984;246:E168–E173. doi: 10.1152/ajpendo.1984.246.2.E168. [DOI] [PubMed] [Google Scholar]
- 26.Johnson JA, Grande JP, Roche PC, Sweeney WE, Jr, Avner ED, Kumar R. 1 alpha, 25-dihydroxyvitamin D3 receptor onto-genesis in fetal renal development. Am J Physiol. 1995;269:F419–F428. doi: 10.1152/ajprenal.1995.269.3.F419. [DOI] [PubMed] [Google Scholar]
- 27.Wilson RT, Wang J, Chinchilli V, et al. Fish, vitamin D, and flavonoids in relation to renal cell cancer among smokers. Am J Epidemiol. 2009;170:717–729. doi: 10.1093/aje/kwp178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Okamoto T, Fujioka T, Horiuchi S. A study of the metabolism of vitamin D in patients with renal cell carcinoma - with special reference to serum concentration of 1 alpha, 25-(OH)2D and its clinical significance. Nihon Hinyokika Gakkai Zasshi. 1991;82:890–899. doi: 10.5980/jpnjurol1989.82.890. (In Japanese) [DOI] [PubMed] [Google Scholar]
- 29.Fujioka T, Suzuki Y, Okamoto T, Mastushita N, Hasegawa M, Omori S. Prevention of renal cell carcinoma by active vitamin D3. World J Surg. 2000;24:1205–1210. doi: 10.1007/s002680010206. [DOI] [PubMed] [Google Scholar]
- 30.Norman AW. Minireview: vitamin D receptor: new assignments for an already busy receptor. Endocrinology. 2006;147:5542–5548. doi: 10.1210/en.2006-0946. [DOI] [PubMed] [Google Scholar]
- 31.Zhou H, Xu C, Gu M. Vitamin D receptor (VDR) gene polymorphisms and Graves’ disease: a meta-analysis. Clin Endocrinol (Oxf) 2009;70:938–945. doi: 10.1111/j.1365-2265.2008.03413.x. [DOI] [PubMed] [Google Scholar]
- 32.Zmuda JM, Cauley JA, Ferrell RE. Molecular epidemiology of vitamin D receptor gene variants. Epidemiol Rev. 2000;22:203–217. doi: 10.1093/oxfordjournals.epirev.a018033. [DOI] [PubMed] [Google Scholar]
- 33.Tokita A, Matsumoto H, Morrison NA, et al. Vitamin D receptor alleles, bone mineral density and turnover in premenopausal Japanese women. J Bone Miner Res. 1996;11:1003–1009. doi: 10.1002/jbmr.5650110718. [DOI] [PubMed] [Google Scholar]
- 34.Abbas S, Nieters A, Linseisen J, et al. Vitamin D receptor gene polymorphisms and haplotypes and postmenopausal breast cancer risk. Breast Cancer Res. 2008;10:P31. doi: 10.1186/bcr1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Uitterlinden AG, Fang Y, Van Meurs JB, Pols HA, Van Leeuwen JP. Genetics and biology of vitamin D receptor polymorphisms. Gene. 2004;338:143–156. doi: 10.1016/j.gene.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 36.Obara W, Suzuki Y, Kato K, Tanji S, Konda R, Fujioka T. Vitamin D receptor gene polymorphisms are associated with increased risk and progression of renal cell carcinoma in a Japanese population. Int J Urol. 2007;14:483–487. doi: 10.1111/j.1442-2042.2007.01771.x. [DOI] [PubMed] [Google Scholar]
- 37.Gross C, Eccleshall TR, Malloy PJ, Villa ML, Marcus R, Feldman D. The presence of a polymorphism at the translation initiation site of the vitamin D receptor gene is associated with low bone mineral density in postmenopausal Mexican-American women. J Bone Miner Res. 1996;11:1850–1855. doi: 10.1002/jbmr.5650111204. [DOI] [PubMed] [Google Scholar]
- 38.Morrison NA, Yeoman R, Kelly PJ, Eisman JA. Contribution of trans-acting factor alleles to normal physiological variability: vitamin D receptor gene polymorphism and circulating osteocalcin. Proc Natl Acad Sci USA. 1992;89:6665–6669. doi: 10.1073/pnas.89.15.6665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Faraco JH, Morrison NA, Baker A, Shine J, Frossard PM. ApaI dimorphism at the human vitamin D receptor gene locus. Nucleic Acids Res. 1989;17:2150. doi: 10.1093/nar/17.5.2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Arai H, Miyamoto KI, Yoshida M, et al. The polymorphism in the caudal-related homeodomain protein Cdx-2 binding element in the human vitamin D receptor gene. J Bone Miner Res. 2001;16:1256–1264. doi: 10.1359/jbmr.2001.16.7.1256. [DOI] [PubMed] [Google Scholar]
- 41.Morrison NA, Qi JC, Tokita A, et al. Prediction of bone density from vitamin D receptor alleles. Nature. 1994;367:284–287. doi: 10.1038/367284a0. [DOI] [PubMed] [Google Scholar]
- 42.Gong YL, Xie DW, Deng ZL, et al. Vitamin D receptor gene Tru9I polymorphism and risk for incidental sporadic colorectal adenomas. World J Gastroenterol. 2005;11:4794–4799. doi: 10.3748/wjg.v11.i31.4794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ingles SA, Ross RK, Yu MC, et al. Association of prostate cancer risk with genetic polymorphisms in vitamin D receptor and androgen receptor. J Natl Cancer Inst. 1997;89:166–170. doi: 10.1093/jnci/89.2.166. [DOI] [PubMed] [Google Scholar]
- 44.Arai H, Miyamoto K, Taketani Y, et al. A vitamin D receptor gene polymorphism in the translation initiation codon: effect on protein activity and relation to bone mineral density in Japanese women. J Bone Miner Res. 1997;12:915–921. doi: 10.1359/jbmr.1997.12.6.915. [DOI] [PubMed] [Google Scholar]
- 45.Jurutka PW, Remus LS, Whitfield GK, et al. The polymorphic N terminus in human vitamin D receptor isoforms influences transcriptional activity by modulating interaction with transcription factor IIB. Mol Endocrinol. 2000;14:401–420. doi: 10.1210/mend.14.3.0435. [DOI] [PubMed] [Google Scholar]
- 46.Slattery ML. Vitamin D receptor gene (VDR) associations with cancer. Nutr Rev. 2007;65:S102–S104. doi: 10.1111/j.1753-4887.2007.tb00332.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sweeney C, Curtin K, Murtaugh MA, Caan BJ, Potter JD, Slattery ML. Haplotype analysis of common vitamin D receptor variants and colon and rectal cancers. Cancer Epidemiol Biomarkers Prev. 2006;15:744–749. doi: 10.1158/1055-9965.EPI-05-0814. [DOI] [PubMed] [Google Scholar]
- 48.Fang Y, van Meurs JB, d’Alesio A, et al. Promoter and 3’-untranslated-region haplotypes in the vitamin D receptor gene predispose to osteoporotic fracture: the rotterdam study. Am J Hum Genet. 2005;77:807–823. doi: 10.1086/497438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saijo T, Ito M, Takeda E, et al. A unique mutation in the vitamin D receptor gene in three Japanese patients with vitamin D-dependent rickets type II: utility of single-strand conformation polymorphism analysis for heterozygous carrier detection. Am J Hum Genet. 1991;49:668–673. [PMC free article] [PubMed] [Google Scholar]
- 50.Hustmyer FG, DeLuca HF, Peacock M. ApaI, BsmI, EcoRV and TaqI polymorphisms at the human vitamin D receptor gene locus in Caucasians, blacks and Asians. Hum Mol Genet. 1993;2:487. doi: 10.1093/hmg/2.4.487. [DOI] [PubMed] [Google Scholar]
- 51.Bhanushali AA, Lajpal N, Kulkarni SS, Chavan SS, Bagadi SS, Das BR. Frequency of fokI and taqI polymorphism of vitamin D receptor gene in Indian population and its association with 25-hydroxyvitamin D levels. Indian J Hum Genet. 2009;15:108–113. doi: 10.4103/0971-6866.60186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kostner K, Denzer N, Müller CS, Klein R, Tilgen W, Reichrath J. The relevance of vitamin D receptor (VDR) gene polymorphisms for cancer: a review of the literature. Anticancer Res. 2009;29:3511–3536. [PubMed] [Google Scholar]
- 53.Yamamoto H, Miyamoto K, Li B, et al. The caudal-related homeodomain protein Cdx-2 regulates vitamin D receptor gene expression in the small intestine. J Bone Miner Res. 1999;14:240–247. doi: 10.1359/jbmr.1999.14.2.240. [DOI] [PubMed] [Google Scholar]
- 54.Fang Y, van Meurs JB, Bergink AP, et al. Cdx-2 polymorphism in the promoter region of the human vitamin D receptor gene determines susceptibility to fracture in the elderly. J Bone Miner Res. 2003;18:1632–1641. doi: 10.1359/jbmr.2003.18.9.1632. [DOI] [PubMed] [Google Scholar]
- 55.Halsall JA, Osborne JE, Potter L, Pringle JH, Hutchinson PE. A novel polymorphism in the 1A promoter region of the vitamin D receptor is associated with altered susceptibilty and prognosis in malignant melanoma. Br J Cancer. 2004;91:765–770. doi: 10.1038/sj.bjc.6602006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Welsh J. Vitamin D and prevention of breast cancer. Acta Pharmacol Sin. 2007;28:1373–1382. doi: 10.1111/j.1745-7254.2007.00700.x. [DOI] [PubMed] [Google Scholar]
- 57.James SY, Mackay AG, Binderup L, Colston KW. Effects of a new synthetic vitamin D analogue, EB1089, on the oestrogen-responsive growth of human breast cancer cells. J Endocrinol. 1994;141:555–563. doi: 10.1677/joe.0.1410555. [DOI] [PubMed] [Google Scholar]
- 58.Swami S, Krishnan AV, Feldman D. 1alpha,25-Dihydroxyvitamin D3 down-regulates estrogen receptor abundance and suppresses estrogen actions in MCF-7 human breast cancer cells. Clin Cancer Res. 2000;6:3371–3379. [PubMed] [Google Scholar]
- 59.Welsh J. Vitamin D and breast cancer: insights from animal models. Am J Clin Nutr. 2004;80(Suppl 6):1721S–1724S. doi: 10.1093/ajcn/80.6.1721S. [DOI] [PubMed] [Google Scholar]
- 60.Chlebowski RT, Johnson KC, Kooperberg C, et al. Calcium plus vitamin D supplementation and the risk of breast cancer. J Natl Cancer Inst. 2008;100:1581–1591. doi: 10.1093/jnci/djn360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fraser DR, Kodicek E. Unique biosynthesis by kidney of a biological active vitamin D metabolite. Nature. 1970;228:764–766. doi: 10.1038/228764a0. [DOI] [PubMed] [Google Scholar]
- 62.Bosetti C, Scotti L, Maso LD, et al. Micronutrients and the risk of renal cell cancer: a case-control study from Italy. Int J Cancer. 2007;120:892–896. doi: 10.1002/ijc.22374. [DOI] [PubMed] [Google Scholar]
- 63.Karami S, Brennan P, Navratilova M, et al. Vitamin D pathway genes, diet, and risk of renal cell carcinoma. Int J Endocrinol. 2010;2010:879362. doi: 10.1155/2010/879362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Raimondi S, Johansson H, Maisonneuve P, Gandini S. Review and meta-analysis on vitamin D receptor polymorphisms and cancer risk. Carcinogenesis. 2009;30:1170–1180. doi: 10.1093/carcin/bgp103. [DOI] [PubMed] [Google Scholar]
- 65.Trump DL, Hershberger PA, Bernardi RJ, et al. Anti-tumor activity of calcitriol: pre-clinical and clinical studies. J Steroid Biochem Mol Biol. 2004;89–90:519–526. doi: 10.1016/j.jsbmb.2004.03.068. [DOI] [PubMed] [Google Scholar]
- 66.Ordonez-Moran P, Larriba MJ, Pendas-Franco N, Aguilera O, Gonzalez-Sancho JM, Munoz A. Vitamin D and cancer: an update of in vitro and in vivo data. Front Biosci. 2005;10:2723–2749. doi: 10.2741/1731. [DOI] [PubMed] [Google Scholar]
- 67.Bretherton-Watt D, Given-Wilson R, Mansi JL, Thomas V, Carter N, Colston KW. Vitamin D receptor gene polymorphisms are associated with breast cancer risk in a UK Caucasian population. Br J Cancer. 2001;85:171–175. doi: 10.1054/bjoc.2001.1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Guy M, Lowe LC, Bretherton-Watt D, et al. Vitamin D receptor gene polymorphisms and breast cancer risk. Clin Cancer Res. 2004;10:5472–5481. doi: 10.1158/1078-0432.CCR-04-0206. [DOI] [PubMed] [Google Scholar]
- 69.Ingles SA, Garcia DG, Wang W, et al. Vitamin D receptor genotype and breast cancer in Latinas (United States) Cancer Causes Control. 2000;11:25–30. doi: 10.1023/a:1008979417618. [DOI] [PubMed] [Google Scholar]
- 70.Dorjgochoo T, Delahanty R, Lu W, et al. Common genetic variants in the vitamin D pathway including genome-wide associated variants are not associated with breast cancer risk among Chinese women. Cancer Epidemiol Biomarkers Prev. 2011;20:2313–2316. doi: 10.1158/1055-9965.EPI-11-0704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.McCullough ML, Stevens VL, Diver WR, et al. Vitamin D pathway gene polymorphisms, diet, and risk of postmenopausal breast cancer: a nested case-control study. Breast Cancer Res. 2007;9:R9. doi: 10.1186/bcr1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Curran JE, Vaughan T, Lea RA, Weinstein SR, Morrison NA, Griffiths LR. Association of A vitamin D receptor polymorphism with sporadic breast cancer development. Int J Cancer. 1999;83:723–726. doi: 10.1002/(sici)1097-0215(19991210)83:6<723::aid-ijc4>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 73.Chen WY, Bertone-Johnson ER, Hunter DJ, Willett WC, Hankinson SE. Associations between polymorphisms in the vitamin D receptor and breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2005;14:2335–2339. doi: 10.1158/1055-9965.EPI-05-0283. [DOI] [PubMed] [Google Scholar]
- 74.Tang C, Chen N, Wu M, Yuan H, Du Y. Fok1 polymorphism of vitamin D receptor gene contributes to breast cancer susceptibility: a meta-analysis. Breast Cancer Res Treat. 2009;117:391–399. doi: 10.1007/s10549-008-0262-4. [DOI] [PubMed] [Google Scholar]
- 75.Karami S, Brennan P, Hung RJ, et al. Vitamin D receptor polymorphisms and renal cancer risk in Central and Eastern Europe. J Toxicol Environ Health A. 2008;71:367–372. doi: 10.1080/15287390701798685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Arjumand W, Ahmad ST, Seth A, Saini AK, Sultana S. Vitamin D receptor FokI and BsmI gene polymorphism and its association with grade and stage of renal cell carcinoma in North Indian population. Tumour Biol. 2012;33:23–31. doi: 10.1007/s13277-011-0236-8. [DOI] [PubMed] [Google Scholar]
- 77.Guy M, Lowe LC, Bretherton-Watt D, Mansi JL, Colston KW. Approaches to evaluating the association of vitamin D receptor gene polymorphisms with breast cancer risk. Recent Results Cancer Res. 2003;164:43–54. doi: 10.1007/978-3-642-55580-0_3. [DOI] [PubMed] [Google Scholar]
- 78.Trabert B, Malone KE, Daling JR, et al. Vitamin D receptor polymorphisms and breast cancer risk in a large population-based case-control study of Caucasian and African-American women. Breast Cancer Res. 2007;9:R84. doi: 10.1186/bcr1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ruggiero M, Pacini S, Aterini S, Fallai C, Ruggiero C, Pacini P. Vitamin D receptor gene polymorphism is associated with metastatic breast cancer. Oncol Res. 1998;10:43–46. [PubMed] [Google Scholar]
- 80.Hou MF, Tien YC, Lin GT, et al. Association of vitamin D receptor gene polymorphism with sporadic breast cancer in Taiwanese patients. Breast Cancer Res Treat. 2002;74:1–7. doi: 10.1023/a:1016048900049. [DOI] [PubMed] [Google Scholar]
- 81.Sinotte M, Rousseau F, Ayotte P, et al. Vitamin D receptor polymorphisms (FokI, BsmI) and breast cancer risk: association replication in two case-control studies within French Canadian population. Endocr Relat Cancer. 2008;15:975–983. doi: 10.1677/ERC-08-0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Buyru N, Tezol A, Yosunkaya-Fenerci E, Dalay N. Vitamin D receptor gene polymorphisms in breast cancer. Exp Mol Med. 2003;35:550–555. doi: 10.1038/emm.2003.72. [DOI] [PubMed] [Google Scholar]
- 83.Dunning AM, McBride S, Gregory J, et al. No association between androgen or vitamin D receptor gene polymorphisms and risk of breast cancer. Carcinogenesis. 1999;20:2131–2135. doi: 10.1093/carcin/20.11.2131. [DOI] [PubMed] [Google Scholar]
- 84.Chakraborty A, Mishra AK, Soni A, et al. Vitamin D receptor gene polymorphism(s) and breast cancer risk in north Indians. Cancer Detect Prev. 2009;32:386–394. doi: 10.1016/j.canep.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 85.Sillanpää P, Hirvonen A, Kataja V, et al. Vitamin D receptor gene polymorphism as an important modifier of positive family history related breast cancer risk. Pharmacogenetics. 2004;14:239–245. doi: 10.1097/00008571-200404000-00003. [DOI] [PubMed] [Google Scholar]
- 86.Lundin AC, Söderkvist P, Eriksson B, Bergman-Jungeström M, Wingren S. Association of breast cancer progression with a vitamin D receptor gene polymorphism. South-East Sweden Breast Cancer Group. Cancer Res. 1999;59:2332–2334. [PubMed] [Google Scholar]
- 87.Ikuyama T, Hamasaki T, Inatomi H, Katoh T, Muratani T, Matsumoto T. Association of vitamin D receptor gene polymorphism with renal cell carcinoma in Japanese. Endocr J. 2002;49:433–438. doi: 10.1507/endocrj.49.433. [DOI] [PubMed] [Google Scholar]
- 88.Wedrén S, Magnusson C, Humphreys K, et al. Associations between androgen and Vitamin D receptor microsatellites and postmenopausal breast cancer. Cancer Epidemiol Biomarkers Prev. 2007;16:1775–1783. doi: 10.1158/1055-9965.EPI-06-1096. [DOI] [PubMed] [Google Scholar]
- 89.Protzel C, Maruschke M, Hakenberg OW. Epidemiology, aetiology, and pathogenesis of renal cell carcinoma. Eur Urol (Suppl) 2012;11:52–59. [Google Scholar]
- 90.American Cancer Society. Breast Cancer Facts and Figures 2009–2010. American Cancer Society; Atlanta, GA: 2010. [Google Scholar]