Abstract
There is a need for the discovery of novel therapeutic strategies to effectively treat advanced clear cell renal cell carcinoma (ccRCC). Inhibition of stearoyl-coA desaturase 1 (SCD1) in ccRCC reveals antitumor activity, independently, and in synergy with mTOR inhibition. SCD1 may be a potential novel therapeutic target in treating ccRCC.
In a recent issue of Clinical Cancer Research, von Roemeling and colleagues report that inhibition of aberrant SCD1 expression attenuates cell proliferation and induces apoptosis in ccRCC cells via the induction of endoplasmic reticulum (ER) stress response signaling (1). These observations implicate SCD1 as a potential therapeutic target.
The process of lipid biosynthesis is essential for metabolic energy, regulation of cell signaling, and the formation of new membranes and organelles during cell proliferation and growth. A fundamental step in lipid synthesis is the production of saturated fatty acids (SFAs) which subsequently are converted to monounsaturated fatty acids (MUFAs), the major fatty acid constituents in cell lipids (2). Catalytic enzymes central to this regulation of fatty acid composition are the steroyl-CoA desaturases (SCD), also known as fatty acyl-CoA delta-9 desaturases (3). The human genome contains two homologs of SCD (SCD1 and SCD5) among which SCD1 is the best characterized in humans.
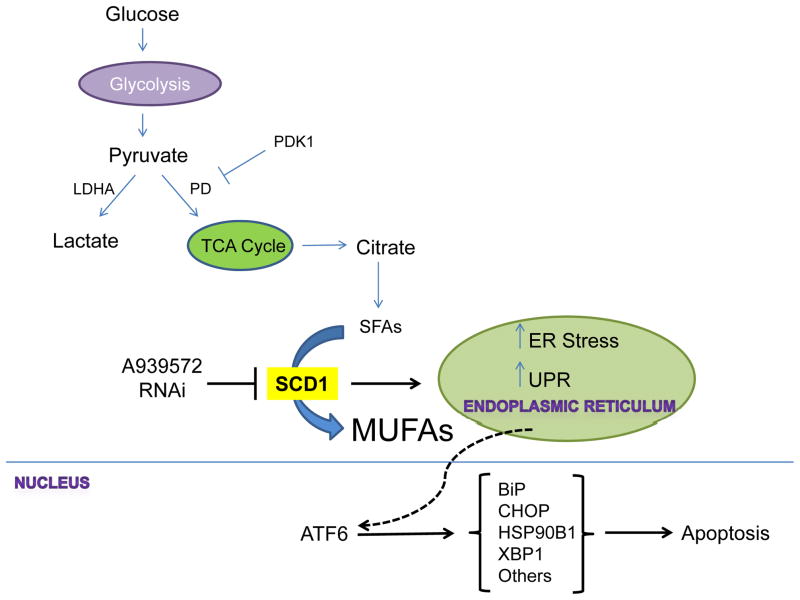
Many cancer cells are characterized by a high rate of aerobic glycolysis resulting in an abundance of pyruvate, which generates citrate upon entry into the TCA cycle. Citrate, through its sequential activation by adenosine triphosphate citrate lyase (ACL), acetyl-CoA carboxylase (ACC) and fatty acid synthase (FAS) can serve as a building block for the de novo synthesis of cellular lipids [Figure 1] (2). Although the main products of glucose-derived fatty acid synthesis are SFAs, an abundance of MUFAs are also found in cancer cells and tissues implicating an essential role for SCD1 in these cells to catalyze the conversion of SFAs into MUFAs. In support of this notion, increased expression of SCD1 has been reported in a number of cancers and cell lines including lung and breast cancer cells, colonic and esophageal carcinomas, hepatocellular adenomas and hepatocellular carcinomas, amongst others (3).
Figure 1.
Glycolysis results in the production of pyruvate, which can be converted to acetyl-CoA (not shown) by pyruvate dehydrogenase (PD). PD activity can be suppressed by pyruvate dehydrogenase kinase (PDK1) whereby pyruvate is then directed towards lactate production by lactate dehydrogenase A (LDHA). Acetyl-CoA enters the TCA cycle and is converted to citrate, a portion of which is diverted towards fatty acid synthesis. Saturated fatty acids (SFAs) are converted to monounsaturated fatty acids (MUFAS) by stearoyl Co-A desaturase (SCD1). SCD1 inhibition by RNAi or A939572 results in the unfolded protein response (UPR) and increased ER stress resulting in the increased production of ATF6, which activates expression of genes mediating stress response pathways (BiP, CHOP, HSP90B1 and XBP1). Under prolonged ER stress the cell responds by initiating apoptosis.
In a recent issue of Clinical Cancer Research, von Roemeling and colleagues report that ccRCC tumors (both early stage and metastatic) express elevated mRNA and protein levels of SCD1 compared to matched normal tissues (1). Knockdown of SCD1 expression with shRNAs, resulted in a dramatic decrease in the proliferation of ccRCC cells lines but did not have a detrimental effect on several independently derived normal renal epithelial cells (NRE). Subsequent analyses revealed that this loss in proliferation is mostly attributed to an increase in apoptosis. Furthermore, treatment of ccRCC cell lines with nanomolar concentrations of A939572, a small molecule inhibitor of SCD1 enzymatic activity, also demonstrated a dose-dependent decrease in proliferation and an increase in apoptosis consistent with results observed from their RNAi experiments. To confirm that decreased tumor cell growth was a specific result of suppressed SCD1 activity, the authors show that a cell culture stable form of oleic acid (OA-BSA), the principle MUFA product of SCD1 mediated SFA hydrogenation, was able to rescue the antiproliferative and apoptotic phenotypes of A939572 treatment.
To establish the underlying mechanism responsible for the decreased proliferation and induction of cell death associated with loss of SCD1 activity, the gene expression changes induced by A939572 treatment were assessed. Pathway analysis revealed increased expression of genes associated with ER stress and the unfolded protein response (UPR), a cellular response that occurs in reaction to the buildup of misfolded and unfolded proteins in the ER (4). von Roemeling and colleagues found that mRNA expression of a number of ER stress markers (BiP, CHOP, HERPUD1, GADD45, CDBPβ) were indeed upregulated in ccRCC cell lines treated with A939572. Moreover, ATF6, a central mediator of the UPR stress response was also found to be activated upon inhibition of SCD1 activity [Figure 1] (4). Importantly, knockdown of ATF6 using shRNAs blocked the induction of ER stress response genes in response to A939572 and rescued the phenotypes induced by A939572 treatment. These observations demonstrate that SCD1’s regulation of proliferation and apoptosis are dependent upon the initiation of ER stress and the UPR.
The clinical significance and potential application of the work by von Roemeling and colleagues is most evident by the observed synergism between SCD1 inhibition with the allosteric mTORC1 inhibitor, temsirolimus. Careful in vitro studies showed that A939572 inhibited proliferation synergistically with temsirolimus but not the multitargeted tyrosine kinase inhibitors (TKIs) pazopanib and sunitinib. Moreover, in vivo combination of A939572 with temsirolimus demonstrated enhanced tumor growth inhibition over either agent alone in a ccRCC cell line xenograft.
Several aspects of the work presented by von Roemeling and colleagues strongly support the practicality of SCD1 as a molecular target in the clinic. First, although inhibition of SCD1 decreased proliferation and induced apoptosis in ccRCCs, no notable effects were observed in NRE cells and only increased blinking and slight mucosal discharge from eyes were observed in immunocompromised animals treated with A939572. This makes SCD1 inhibition an ideal candidate for therapeutic intervention with possibly minimal toxicity to patients. Second, the increased expression of SCD1 in ccRCC makes SCD1, itself, an ideal potential predictive marker to identify patients who will most likely yield a response to pharmacologic inhibition of SCD1. Finally, the induction of ER stress response genes to SCD1 inhibition might serve as a pharmacodynamic marker to assess the effectiveness of anti-SCD1 therapy. Collectively, these observations strongly support SCD1 as a novel molecular target for the treatment of advanced ccRCC that warrants clinical investigation.
Nonetheless, some questions remain. For example, at what stage in tumor development does increased fatty acid synthesis become necessary for sustained tumor growth? Also, given the established role for mTORC1 in regulating lipid metabolism and sterol regulatory element-binding protein 1c (SREBP1c) (5) to what extent does the synergism between SCD1 and mTOR inhibition reflect independent effects upon ER stress or combined downregulation of SCD1 activity? Finally, ccRCC cells deficient in the von Hippel-Lindau tumor suppressor (VHL) gene have constitutively elevated levels of the hypoxia-inducible factor (HIF) even under normoxia (6). HIF’s ability to suppress oxidative phosphorylation, through PDK1, favors the production of lactate and decreases the pool of glucose derived carbon available for lipid synthesis (7–9). Maintenance of fatty acid synthesis by VHL deficient ccRCC cells is therefore mediated by the reductive carboxylation of glutamine in a glutaminase and isocitrate dehydrogenase 1 (IDH1) dependent manner (10). Therefore, whether glutaminase inhibition when combined with SCD1 and mTOR inhibition leads to further therapeutic gains, should be explored. In summary, the observations by von Roemeling and colleagues underscore the notion that cancer cells have altered metabolic demands that can be therapeutically targeted. Additionally, their findings highlight the increased recognition that tumor cells, in contrast to non-transformed cells, are dependent upon de novo fatty acid synthesis (rather than exogenous fatty acids) for maintenance of cellular homeostasis (2).
Acknowledgments
This work was supported by the NIH R01 CA142794 (WYK) and the AACR-Kure It Grant for Kidney Cancer Research (WYK). WYK is a Damon Runyon Merck Clinical Investigator.
Footnotes
The authors do not declare any conflicts of interest.
References
- 1.Roemeling von CA, Marlow LA, Wei JJ, Cooper SJ, Caulfield TR, Tan WW, et al. Stearoyl-CoA desaturase 1 is a novel molecular therapeutic target for clear cell renal cell carcinoma. Clinical Cancer Research. 2013:1–33. doi: 10.1158/1078-0432.CCR-12-3249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Menendez JA, Lupu R. Fatty acid synthase and the lipogenic phenotype in cancer pathogenesis. Nat Rev Cancer Nature Publishing Group. 2007;7:763–77. doi: 10.1038/nrc2222. [DOI] [PubMed] [Google Scholar]
- 3.Igal RA. Stearoyl-CoA desaturase-1: a novel key player in the mechanisms of cell proliferation, programmed cell death and transformation to cancer. Carcinogenesis. 2010;31:1509–15. doi: 10.1093/carcin/bgq131. [DOI] [PubMed] [Google Scholar]
- 4.Ma Y, Hendershot LM. The role of the unfolded protein response in tumour development: friend or foe? Nat Rev Cancer. 2004;4:966–77. doi: 10.1038/nrc1505. [DOI] [PubMed] [Google Scholar]
- 5.Ricoult SJH, Manning BD. The multifaceted role of mTORC1 in the control of lipid metabolism. EMBO reports. 2013;14:242–51. doi: 10.1038/embor.2013.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim WY, Kaelin WG. Role of VHL gene mutation in human cancer. J Clin Oncol. 2004;22:4991–5004. doi: 10.1200/JCO.2004.05.061. [DOI] [PubMed] [Google Scholar]
- 7.Kim J-W, Tchernyshyov I, Semenza GL, Dang CV. HIF-1-mediated expression of pyruvate dehydrogenase kinase: a metabolic switch required for cellular adaptation to hypoxia. Cell Metab. 2006;3:177–85. doi: 10.1016/j.cmet.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 8.Papandreou I, Cairns RA, Fontana L, Lim AL, Denko NC. HIF-1 mediates adaptation to hypoxia by actively downregulating mitochondrial oxygen consumption. Cell Metab. 2006;3:187–97. doi: 10.1016/j.cmet.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 9.Semenza GL, Jiang BH, Leung SW, Passantino R, Concordet JP, Maire P, et al. Hypoxia response elements in the aldolase A, enolase 1, and lactate dehydrogenase A gene promoters contain essential binding sites for hypoxia-inducible factor 1. J Biol Chem. 1996;271:32529–37. doi: 10.1074/jbc.271.51.32529. [DOI] [PubMed] [Google Scholar]
- 10.Metallo CM, Gameiro PA, Bell EL, Mattaini KR, Yang J, Hiller K, et al. Reductive glutamine metabolism by IDH1 mediates lipogenesis under hypoxia. Nature. 2012;481:380–4. doi: 10.1038/nature10602. [DOI] [PMC free article] [PubMed] [Google Scholar]