Abstract
Objective
To assess whether being employed in a smoke-free workplace is associated with living in a smoke-free home in 15 low and middle income countries (LMICs).
Methods
Country-specific individual level analyses of cross-sectional Global Adult Tobacco Survey data (2008–2011) from 15 LMICs was conducted using multiple logistic regression. The dependent variable was living in a smoke-free home; the independent variable was being employed in a smoke-free workplace. Analyses were adjusted for age, gender, residence, region, education, occupation, current smoking, current smokeless tobacco use and number of household members. Individual country results were combined in a random effects meta-analysis.
Results
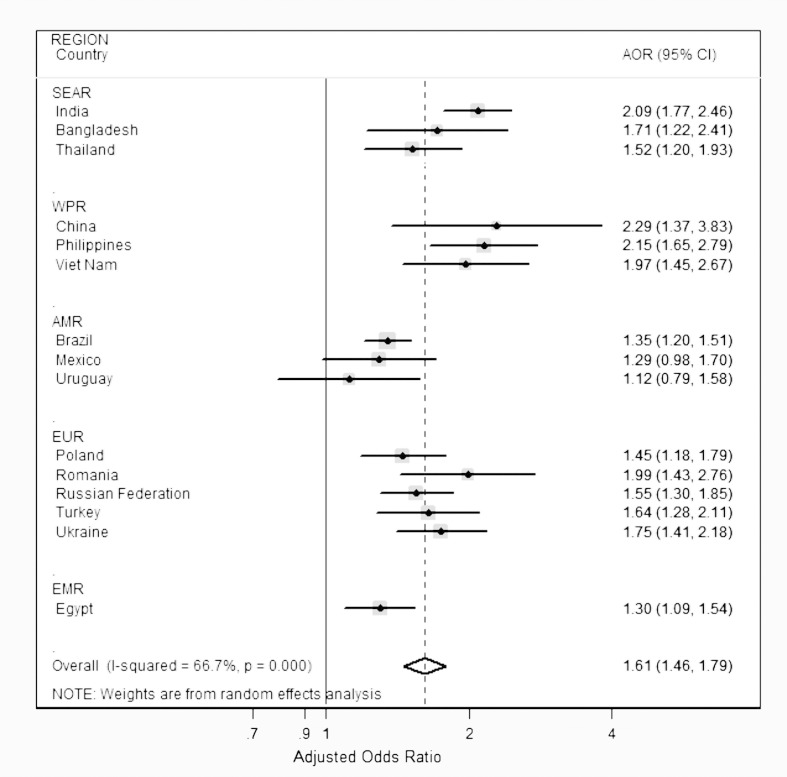
In each country, the percentage of participants employed in a smoke-free workplace who reported living in a smoke-free home was higher than those employed in a workplace not smoke-free. The adjusted odds ratios (AORs) of living in a smoke-free home among participants employed in a smoke-free workplace (vs. those employed where smoking occurred) were statistically significant in 13 of the 15 countries, ranging from 1.12 [95% CI 0.79–1.58] in Uruguay to 2.29 [1.37–3.83] in China. The pooled AOR was 1.61 [1.46–1.79].
Conclusion
In LMICs, employment in a smoke-free workplace is associated with living in a smoke-free home. Accelerated implementation of comprehensive smoke-free policies is likely to result in substantial population health benefits in these settings.
Keywords: Smoke-free policy, Secondhand smoke, Tobacco, Workplace, Low- and middle-income countries, GATS
Highlights
-
•
Individual level Global Adult Tobacco Survey data analyzed for 15 LMICs (2008–2010)
-
•
Studied association of smoke-free workplace policy with living in smoke-free home
-
•
Implementation of smoke-free workplace policy varies greatly across LMICs.
-
•
Smoke-free homes 60% more likely with employment in smoke-free workplaces in LMICs
-
•
100% smoke-free policy in LMICs changes social norms around exposing others to SHS.
Introduction
Approximately 600,000 deaths are attributable to secondhand smoke (SHS) exposure globally each year (Öberg et al., 2011). Adverse health effects from SHS exposure include sudden infant death syndrome and respiratory disorders in children and lung, breast cancer (California Environmental Health Protection Agency, 2005, Johnson et al., 2011), cardiovascular disease and poorer reproductive outcomes in adults (U.S. Department of Health and Human Services, 2006, World Health Organization, 2011). The bulk of the burden from SHS exposure falls on women and children living in low and middle income countries (LMICs), where 80% of the world's smokers reside (World Health Organization, 2013a) and where SHS exposure at home is typically high, ranging from 17% in Mexico to 73% in Viet Nam among countries participating in the Global Adult Tobacco Survey (GATS) (King et al., 2013). Further, SHS exposure at home among non-smokers is higher among females compared with males (King et al., 2013).
Comprehensive smoke-free policies have high levels of public support and have been associated with substantial health benefits (Fong et al., 2006, International Agency for Research on Cancer, 2009, Tang et al., 2003). These include reduced tobacco consumption and increased quit attempts, the virtual elimination of SHS from workplaces, lower hospital admission rates for myocardial infarction and stroke, lower admissions for acute respiratory illness in both children and adults (Millett et al., 2013, Tan and Glantz, 2012), and lower rates of small for gestational age births (Kabir et al., 2013). However, these health benefits are not equitably distributed as only 16% of the world's population are covered by comprehensive smoke-free policies (World Health Organization, 2013b).
Research evidence suggests that smoke-free workplace policies may change social norms about exposing others to SHS in the home (Berg et al., 2012, Cheng et al., 2011, Fong et al., 2006, St. Claire et al., 2012). These findings indicate that early concerns that smoke-free workplace policies would lead to behavioural compensation through an increase in smoking at home have not materialized; rather, results from richer countries (Berg et al., 2012, Cheng et al., 2011, St. Claire et al., 2012) and India (Lee et al., 2013) have consistently found that people employed in a smoke-free workplace are more likely to live in a smoke-free home. Replication of this finding in other LMICs would indicate that implementation of smoke-free policies in these settings will likely result in substantial reductions in tobacco related harm globally. This study examines whether there is an association between being employed in a smoke-free workplace and living in a smoke-free home in 15 LMICs participating in GATS between 2008 and 2011.
Methods
Study design, setting and data
This study involved secondary analysis of GATS data from 15 LMICs. GATS is a nationally representative cross-sectional household survey of non-institutionalized adults aged 15 years and over (World Health Organization, 2013c). It is considered to be the global standard for monitoring adult tobacco use and key tobacco control indicators. GATS employs standardized survey methodology with a few country-specific variations in the questionnaire, and is designed to collect household as well as individual level data. Multi-stage cluster sampling design is employed in GATS to select a nationally representative study sample. Between 2008 and 2011, the first round of GATS was implemented in 17 LMICs in five WHO regions (Centers for Disease Control and Prevention, 2013a). Country-specific, anonymous GATS data for 15 of the 17 LMICs (all but Indonesia and Malaysia) was freely available from the CDC GTSS Data website, which was used for secondary data analysis. Poland and the Russian Federation are now classified as high income countries by the World Bank; however, when first round of GATS was conducted in these countries in 2009, they belonged to the upper middle income category. Therefore, for the purpose of our study, we treated them as middle income countries.
Study participants
We used individual level data from the first round of GATS in each of the 15 LMICs. GATS respondents in each country who reported working indoors (or both indoors and outdoors) but outside their home were included as participants for this study. Observations with missing values in the dependent or independent variables were dropped to obtain a final sample for each country. The proportion of missing cases ranged from 0.1% in Uruguay to 8.5% in China (Table 1). Table 1 describes the total number of participants included in our study from each of the 15 LMICs which ranged from 1174 in Romania to 12,912 in Brazil.
Table 1.
Description of participants living in smoke-free homes among those working indoors in GATS countries (2008–2011). Weighted %.
| SEAR |
WPR |
AMR |
EUR |
EMR |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| India N = 12,561 |
Bangladesh N = 1663 |
Thailand N = 4999 |
Chinaa N = 1711 |
Philippines N = 2083 |
Viet Nam N = 2373 |
Brazilb N = 12,912 |
Mexico N = 2026 |
Uruguayc N = 1805 |
Poland N = 2973 |
Romaniad N = 1174 |
Russian Federatione N = 5426 |
Turkeyf N = 2007 |
Ukrainee N = 2741 |
Egypt N = 4365 |
|
| Smoke-free at work | |||||||||||||||
| Yes | 64.0 | 53.0 | 73.3 | 20.5 | 53.3 | 22.1 | 66.6 | 74.5 | 55.3 | 48.5 | 49.3 | 56.6 | 42.4 | 70.7 | 41.8 |
| No | 41.7 | 34.1 | 58.5 | 9.2 | 28.9 | 11.1 | 58.0 | 68.5 | 51.1 | 33.0 | 31.7 | 43.4 | 28.8 | 55.4 | 33.8 |
| Age group (yrs) | |||||||||||||||
| 15–29 | 53.1 | 40.6 | 63.9 | 11.7 | 43.3 | 12.9 | 62.9 | 75.8 | 43.9 | 42.7 | 39.2 | 51.6 | 31.4 | 60.1 | 30.8 |
| 30–44 | 58.8 | 39.2 | 70.7 | 14.7 | 47.7 | 17.4 | 66.2 | 71.3 | 60.1 | 46.9 | 45.0 | 52.2 | 40.5 | 67.1 | 40.2 |
| 45–59 | 59.9 | 46.3 | 75.8 | 11.5 | 47.0 | 19.1 | 64.1 | 72.2 | 56.4 | 38.9 | 42.1 | 51.0 | 40.0 | 66.6 | 40.2 |
| ≥ 60 | 62.4 | 30.1 | 63.7 | 11.5 | 38.0 | 17.0 | 64.0 | 76.3 | 63.5 | 46.6 | 58.3 | 55.7 | 56.9 | 80.9 | 48.1 |
| Gender | |||||||||||||||
| Male | 56.4 | 40.1 | 64.5 | 11.2 | 42.7 | 14.7 | 65.4 | 72.2 | 54.2 | 44.2 | 44.1 | 52.9 | 38.2 | 64.7 | 35.8 |
| Female | 61.6 | 44.6 | 74.7 | 16.2 | 48.6 | 17.3 | 63.6 | 75.2 | 55.0 | 42.2 | 42.4 | 50.8 | 34.8 | 66.8 | 41.1 |
| Residence | |||||||||||||||
| Urban | 65.4 | 47.4 | 74.0 | 17.2 | 55.8 | 21.9 | 64.8 | 73.2 | 54.4 | 43.4 | 37.7 | 49.9 | 37.8 | 64.7 | 41.3 |
| Rural | 49.0 | 35.9 | 65.6 | 06.8 | 25.6 | 10.8 | 58.2 | 75.0 | 59.1 | 43.0 | 57.8 | 59.3 | 35.3 | 69.8 | 31.1 |
| Education | |||||||||||||||
| Primary | 44.2 | 31.1 | 58.8 | 5.0 | 26.4 | 9.7 | – | 76.0 | 54.7 | 39.7 | – | – | 34.0 | – | 27.4 |
| Secondary | 58.8 | 45.8 | 69.6 | 11.5 | 45.6 | 18.3 | – | 73.5 | 53.6 | 39.9 | 43.9 | 50.7 | 34.1 | 62.7 | 34.6 |
| Tertiary | 71.8 | 67.2 | 81.1 | 18.5 | 59.4 | 22.3 | – | 71.3 | 58.6 | 52.7 | 41.9 | 52.7 | 49.2 | 71.4 | 48.8 |
| Occupation | |||||||||||||||
| Employed | 58.7 | 55.8 | 69.8 | – | 46.8 | 21.1 | 65.4 | 72.9 | 54.4 | 43.3 | 41.9 | 51.7 | 37.1 | 65.6 | 38.0 |
| Self employed | 55.1 | 34.5 | 68.1 | – | 40.7 | 11.4 | 62.0 | 75.0 | 55.8 | 43.3 | 59.1 | 53.4 | 38.8 | 67.8 | 32.3 |
| Current smoking | |||||||||||||||
| Yes | 28.8 | 27.6 | 47.8 | 8.1 | 25.7 | 10.2 | 34.6 | 65.2 | 29.7 | 17.7 | 24.7 | 36.8 | 26.2 | 46.7 | 12.8 |
| No | 63.4 | 49.5 | 76.0 | 16.0 | 52.5 | 18.2 | 70.1 | 75.7 | 63.7 | 58.0 | 53.4 | 63.3 | 47.3 | 76.0 | 48.0 |
| Current smokeless tobacco use | |||||||||||||||
| Yes | 38.8 | 33.6 | 54.1 | 9.3 | 47.4 | 31.8 | 46.9 | 41.1 | – | 63.4 | – | 27.2 | – | 57.0 | 15.9 |
| No | 63.5 | 42.9 | 69.5 | 13.1 | 45.6 | 15.9 | 64.5 | 73.6 | 54.6 | 43.2 | 43.5 | 51.9 | – | 65.8 | 37.7 |
| Percentage of missing cases | 7.1 | 8.2 | 1.6 | 8.5 | 2.2 | 2.8 | 4.0 | 3.6 | 0.1 | 4.2 | 1.5 | 2.7 | 1.5 | 2.6 | 3.3 |
Occupation categories in China differed from those of other LMICs. Five occupation categories were considered for China and hence have not been presented in this table for maintaining uniformity.
In Brazil, education categories were defined differently and were incomparable to those from other GATS countries.
In Uruguay, there were no current smokeless tobacco users in the study population.
In Romania, the category ‘Primary’ for the education variable contained only 1 case and hence, was merged with the category ‘Secondary’. Moreover, the study sample in Romania contained only six cases of current smokeless tobacco users which constituted a negligible proportion and hence has not been presented in the table.
In Russian Federation and Ukraine, the category ‘Primary’ for the education variable contained only 10 and 8 cases respectively and hence, were merged with the category ‘Secondary’.
In Turkey, no data was available on current smokeless tobacco use from the GATS survey.
Measures
The GATS questionnaire includes core questions on tobacco use, SHS exposure at work and in the home, and socio-demographic information. For the present study, the dependent variable was ‘living in a smoke-free home’. A participant was classified as living in a smoke-free home if he/she replied ‘never’ to the question: How often does anyone smoke inside your home? If the participant responded ‘daily’, ‘weekly’, ‘monthly’, or ‘less than monthly’, he/she was considered as not living in a smoke-free home. The independent variable was ‘being employed in a smoke-free workplace’. The participant was classified as employed in a smoke-free workplace if he/she answered ‘no’ to the question: During the past 30 days, did anyone smoke in the indoor areas where you work?
The potential confounders included were: age group, gender, residence, education, occupation, current smoking, current smokeless tobacco (SLT) use and number of household members. A country-specific region variable was also included for India, Thailand, China, Brazil, Poland and Ukraine (this information was not available for other countries). Current SLT use was not included as a covariate for Uruguay, Romania and Turkey as there were only a very small number of users or no data on SLT use was available. In China, the occupation variable consisted of five categories rather than two as the categorization for employment differed substantially from other countries (Centers for Disease Control and Prevention, 2013b). Due to a negligible number of participants educated up to primary level in Romania, Russian Federation and Ukraine, we merged these with the ‘up to secondary level’ education category. See Supplementary Table for a detailed description of the definitions of variables used in this study.
Statistical analysis
We conducted country-specific, individual level data analysis for each LMIC. We tested for bivariate associations between the independent variable with the dependent variable using Chi-square tests. Country-specific multiple logistic regression models were run to estimate the adjusted odds ratio (AOR) and 95% confidence interval (95% CI) of living in a smoke-free home if employed in a smoke-free workplace compared with being employed in a workplace where smoking occurred. The logistic regression models were adjusted for all the covariates described above (with country-specific exclusions) to minimize confounding and ensure comparability of findings across countries. Age and number of household members were treated as continuous variables. In Brazil, the ‘education’ variable was not included in the model because the variable definition was not comparable with other GATS countries (Palipudi et al., 2012), however, we did conduct a sensitivity analysis by including education variable in the model and found that the results were consistent with those obtained without including it in the model.
We tested for multicollinearity between the covariates adjusted for in the analysis for each country. The multicollinearity diagnostics variance inflation factor (VIF) values were all less than five, indicating reasonable independence between the predictor variables for each country-specific model (Glantz and Slinker, 2001). The only exception to this was the covariate ‘education’ in Poland where VIF values were less than 6.5. The variable ‘national region’ was removed from the model in Egypt due to collinearity. Country-specific sampling weights were applied for all analyses to account for the complex study design.
To estimate the overall association of being employed in a smoke-free workplace with living in a smoke-free home across the 15 LMICs, we calculated a pooled AOR and 95% CI using a random effects meta-analysis based on the AOR's from the individual countries (The random effects meta-analysis accounts for heterogeneity between countries, p < 0.0005.). All the statistical analyses were conducted using STATA v.12.0.
Results
Descriptive statistics
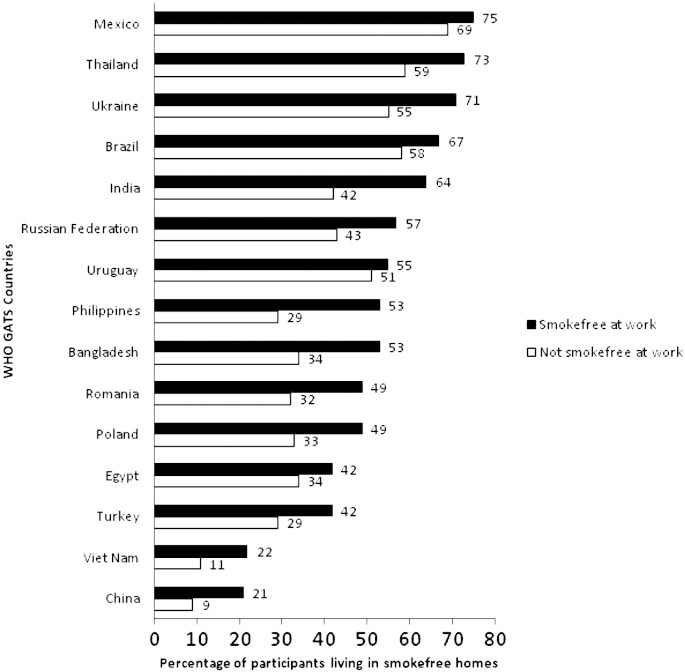
Of the participants employed indoors outside the home, the percentage reporting a smoke-free workplace was 83% in Uruguay, 81% in Mexico, 76% in Brazil, 74% in Thailand, 70% in India, 68% in Ukraine and Philippines, 66% in Romania and Poland, 64% in Russian Federation, 63% in Turkey, 44% in Viet Nam, 40% in Egypt and 35% in Bangladesh and China (data not shown). In all the 15 LMICs, the percentage of participants living in a smoke-free home was higher among those employed in a smoke-free workplace compared with those employed in a workplace where smoking occurred (Fig. 1, Table 1). Among participants employed in a smoke-free workplace, the percentage living in a smoke-free home varied from 21% in China to 75% in Mexico. Among participants employed in a workplace that was not smoke-free, the percentage living in a smoke-free home varied from 9% in China to 69% in Mexico. Table 1 describes the country-specific percentages of participants reporting living in smoke-free homes by their socio-demographic characteristics.
Fig. 1.
Percentage of participants living in smoke-free homes by smoke-free status of the workplace in 15 GATS countries (2008–2011).
Multiple logistic regression analysis
There were significant positive associations between being employed in a smoke-free workplace and living in a smoke-free home in all the LMICs except Uruguay and Mexico (Fig. 2, Table 2). The AOR estimates ranged from 1.12 [0.79–1.58] in Uruguay to 2.29 [1.37–3.83] in China. The pooled AOR for the all-country data was 1.61 [1.46–1.79].
Fig. 2.
Forest plot showing country-specific and pooled adjusted odds ratios (95% CIs) of living in a smoke-free home among those employed in a smoke-free workplace compared with those employed in workplaces where smoking occurred (GATS 2008–2011).
Table 2.
Association of being employed in a smoke-free workplace with living in a smoke-free home among those working indoors in GATS countries (2008–2011) Adjusted Odds Ratio [95% CI]a.
| SEAR |
WPR |
AMR |
EUR |
EMR |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| India N = 12,561 |
Bangladesh N = 1663 |
Thailand N = 4999 |
China N = 1711 |
Philippines N = 2083 |
Viet Nam N = 2373 |
Brazil N = 12,912 |
Mexico N = 2026 |
Uruguay N = 1805 |
Poland N = 2973 |
Romania N = 1174 |
Russian Federation N = 5426 |
Turkey N = 2007 |
Ukraine N = 2741 |
Egyptb N = 4365 |
|
| Smoke-free at work | |||||||||||||||
| Yes |
2.09 [1.77, 2.46] |
1.71 [1.22, 2.41] |
1.52 [1.20, 1.93] |
2.29 [1.37, 3.83] |
2.15 [1.65, 2.79] |
1.97 [1.45, 2.67] |
1.35 [1.20, 1.51] |
1.29 [0.98, 1.70] |
1.12 [0.79, 1.58] |
1.45 [1.18, 1.79] |
1.99 [1.43, 2.76] |
1.55 [1.30, 1.85] |
1.64 [1.28, 2.11] |
1.75 [1.41, 2.18] |
1.30 [1.09, 1.54] |
| No | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Age (yrs) | |||||||||||||||
|
1.02 [1.01, 1.03] |
1.01 [0.99, 1.02] |
1.02 [1.01, 1.04] |
1.00 [0.98, 1.03] |
1.00 [0.99, 1.01] |
1.02 [1.01, 1.03] |
1.01 [1.003, 1.011] |
0.99 [0.98, 1.00] |
1.02 [1.01, 1.03] |
0.99 [0.98, 1.00] |
1.01 [0.99, 1.02] |
0.99 [0.98, 1.00] |
1.02 [1.01, 1.03] |
1.01 [0.99, 1.02] |
1.02 [1.01, 1.03] |
|
| Gender | |||||||||||||||
| Male | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Female |
0.63 [0.53, 0.76] |
0.52 [0.33, 0.83] |
0.93 [0.73, 1.17] |
0.89 [0.46, 1.73] |
0.84 [0.66, 1.07] |
0.73 [0.52,1.02] |
0.84 [0.76, 0.93] |
1.07 [0.82, 1.38] |
0.89 [0.73, 1.09] |
0.71 [0.59, 0.87] |
0.76 [0.57, 1.03] |
0.52 [0.43, 0.63] |
0.62 [0.45, 0.85] |
0.52 [0.41, 0.66] |
0.58 [0.48, 0.71] |
| Residence | |||||||||||||||
| Urban |
1.57 [1.32, 1.85] |
1.28 [0.92, 1.77] |
1.31 [1.04, 1.64] |
2.05 [1.21, 3.48] |
3.06 [2.31, 4.04] |
2.01 [1.46, 2.77] |
1.28 [1.01, 1.63] |
1.03 [0.73, 1.44] |
0.81 [0.60, 1.10] |
1.09 [0.86, 1.39] |
0.48 [0.33, 0.69] |
0.75 [0.60, 0.93] |
1.06 [0.81, 1.38] |
0.77 [0.60, 0.99] |
1.31 [1.08, 1.60] |
| Rural | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Education | |||||||||||||||
| Primary | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | – | 1 (Ref) | 1 (Ref) | 1 (Ref) | – | – | 1 (Ref) | – | 1 (Ref) |
| Secondary |
1.58 [1.34, 1.86] |
1.54 [1.12, 2.13] |
1.86 [1.46, 2.37] |
1.43 [0.70, 2.92] |
1.70 [1.13, 2.56] |
1.60 [1.08, 2.36] |
– | 0.81 [0.57, 1.15] |
0.98 [0.72, 1.33] |
0.76 [0.47, 1.24] |
1 (Ref) | 1 (Ref) | 0.98 [0.77, 1.26] |
1 (Ref) | 1.23 [0.97, 1.57] |
| Tertiary |
2.26 [1.83, 2.78] |
2.90 [1.76, 4.78] |
2.54 [1.92, 3.36] |
1.47 [0.56, 3.87] |
2.39 [1.58, 3.62] |
0.99 [0.33, 3.02] |
– | 0.73 [0.49, 1.10] |
1.06 [0.70, 1.60] |
1.05 [0.63, 1.74] |
1.13 [0.82, 1.55] |
1.04 [0.88, 1.23] |
1.61 [1.14, 2.28] |
1.30 [1.03, 1.65] |
1.60 [1.23, 2.09] |
| Occupation | |||||||||||||||
| Employed | 0.99 [0.85, 1.15] |
1.41 [1.02, 1.93] |
0.86 [0.66, 1.14] |
– |
0.74 [0.55, 0.99] |
1.35 [0.97, 1.87] |
1.05 [0.94, 1.17] |
0.89 [0.61,1.30] |
1.08 [0.78, 1.49] |
1.04 [0.81, 1.35] |
0.44 [0.27, 0.72] |
0.96 [0.71, 1.32] |
0.88 [0.66, 1.16] |
0.86 [0.59, 1.28] |
0.88 [0.67, 1.15] |
| Self employed | 1 (Ref) | 1 (Ref) | 1 (Ref) | – | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Current smoking | |||||||||||||||
| Yes | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| No |
4.49 [3.62, 5.57] |
2.50 [1.81, 3.47] |
3.07 [2.34, 4.02] |
1.67 [0.76, 3.65] |
2.84 [2.05, 3.92] |
2.04 [1.35, 3.06] |
4.53 [3.98, 5.16] |
1.62 [1.20, 2.19] |
4.18 [3.09, 5.66] |
6.07 [4.87, 7.57] |
3.78 [2.74, 5.22] |
3.58 [2.93, 4.37] |
2.47 [1.91, 3.19] |
4.25 [3.38, 5.35] |
7.64 [6.04, 9.67] |
| Current smokeless tobacco use | |||||||||||||||
| Yes | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | – | 1 (Ref) | – | 1 (Ref) | – | 1 (Ref) | 1 (Ref) |
| No |
1.84 [1.54, 2.20] |
1.16 [0.77, 1.75] |
1.64 [0.50, 5.40] |
0.68 [0.09, 5.38] |
1.73 [0.48, 6.31] |
0 .22 [0.03, 1.59] |
2.25 [0.78, 6.48] |
3.12 [0.83,11.68] |
– | 0.36 [0.06, 2.25] |
– | 2.29 [0.78, 6.68] |
– | 0.86 [0.10, 7.72] |
0.90 [0.44, 1.86] |
| Number of household members | |||||||||||||||
|
0.96 [0.93, 0.99] |
0.91 [0.84, 0.99] |
0.94 [0.89, 1.00] |
1.12 [0.88, 1.42] |
0.94 [0.88, 0.99] |
0.90 [0.81, 0.99] |
0.98 [0.95, 1.02] |
0.99 [0.92, 1.06] |
0.99 [0.90, 1.10] |
1.01 [0.93, 1.08] |
1.17 [1.03, 1.32] |
1.09 [1.01, 1.17] |
0.96 [0.90, 1.02] |
1.11 [1.01, 1.21] |
0.91 [0.85, 0.96] |
|
Bold values indicate a significant association between the independent variable and the dependent variable, compared with the reference category (p < 0.05).
Adjusted odds ratios and 95% CIs obtained from country-specific individual-level multiple logistic regression models adjusted for age, gender, place of residence, education, occupation, current smoking, current smokeless tobacco use and number of household members. A country-specific region variable was also included in the models for India, Thailand, China, Brazil, Poland and Ukraine (not shown in the table to maintain uniformity as regions varied by country).
Region variable was excluded from the country-specific regression model in Egypt due to collinearity (VIF > 13).
Female participants were less likely than males to live in a smoke-free home in most LMICs but associations were only significant in India, Bangladesh, Brazil, Poland, Russian Federation, Turkey, Ukraine and Egypt. Participants from urban settings in India, Thailand, China, Philippines, Viet Nam, Brazil and Egypt were significantly more likely to live in a smoke-free home compared with those from the rural settings. In contrast, participants from rural settings were significantly more likely to live in a smoke-free home in Romania, Russian Federation and Ukraine. The likelihood of living in a smoke-free home significantly increased with increasing education level in India, Bangladesh, Thailand, Philippines, Ukraine and Egypt. Non-smokers were consistently more likely to live in a smoke-free home than smokers. No association was observed between SLT use and living in a smoke-free home.
Discussion
This study utilized data from the first round of GATS, conducted in 15 LMICs between 2008 and 2011, to examine whether being employed in a smoke-free workplace is associated with living in a smoke-free home. We found positive associations in all of the 15 LMICs studied (13 out of 15 being statistically significant) in individual level country-specific analysis. The pooled estimate indicated that participants employed in a smoke-free workplace were 60% more likely to live in a smoke-free home compared with those that worked where smoking occurred. These findings are consistent with those from previous studies conducted in high income settings. Cheng et al. (2011) in a longitudinal study conducted in the USA suggested that living in smoke-free homes was four to seven times more likely among those employed in a 100% smoke-free workplace (compared with those employed in workplaces where smoking occurred). Another longitudinal study found similar reductions in smoking at home after the introduction of comprehensive smoke-free policies in Ireland (85% to 80%; p = 0.002) and the UK (82% to 76%; p = 0.003) (Fong et al., 2006). An evaluation of the smoke-free policy introduced in New Zealand in 2004 suggested that SHS exposure at workplaces decreased from 20% to 8% and the proportion of smoke-free homes increased from 64% to 70% between 2003 and 2006 (Edwards et al., 2008).
Article 8 of WHO Framework Convention on Tobacco Control (FCTC) requires parties to adopt and implement measures to reduce exposure to tobacco smoke in indoor workplaces, indoor public places, public transport and other public places (World Health Organization, 2003). However, disparities observed in the implementation and enforcement of Article 8 of FCTC in LMICs (World Health Organization, 2013b) suggest that these benefits are not being fully realized. Our study identified substantial differences in the percentage of participants employed in a smoke-free workplace who were living in a smoke-free home. This varied from 21% in China to 75% in Mexico. These findings highlight the role of other determinants of SHS exposure in the home, including smoking prevalence, the implementation of other tobacco control strategies and cultural norms, which vary considerably in the countries studied. Knowledge and attitudes about the harms of SHS exposure are also likely to play an important role in variations in the adoption of smoke-free homes (Centers for Disease Control and Prevention, 2007). A recent study conducted in United States has shown that clean indoor air laws increase the likelihood of having voluntary smoke-free homes by 3–5% (Cheng et al., 2013). Despite the observed country-specific variations in the strength of association, the consistency of the observed relationship across major LMIC settings is noteworthy and favours comprehensive smoke-free policies as recommended by the WHO (World Health Organization, 2011).
Our study additionally implies that the benefits which arise out of smoke-free workplace policies are not only restricted to the direct health and economic benefits (IARC, 2009), but may also extend to changing societal norms around SHS exposure in the home in LMICs. Highlighting the role of social contingencies and cultural influences in SHS exposure, Hovell and Hughes (2009) suggest that acceptability of smoking demonstrates an attitude of cultural tolerance towards smoking and SHS exposure, which ultimately leads to widespread recognition of smoking and exposing others to tobacco smoke as normative behaviour. Smoke-free policies serve to disrupt such reinforcement of smoking and SHS exposure, thereby aiding effective tobacco control (Hovell and Hughes, 2009). Our findings suggest that smoke-free policies may consistently lead to spreading of smoke-free norms in all of the major LMICs studied, irrespective of country-specific variations in tobacco use and implementation of smoke-free policies. Further, smoke-free policies can bring about behaviour change (quitting or prevention of smoking initiation) through such normative influences (Brown et al., 2009).
Our results show that women were less likely to live in a smoke-free home compared with men in most of the LMICs studied. This is not surprising given the generally higher prevalence of smoking among men in these settings (Giovino et al., 2012). Women and children are usually exposed to SHS due to smoking by spouses or other family members at homes in LMICs, many of which still follow patriarchal norms (Visvanathan et al., 2011), making it likely that women have little authority over allowance of smoking at home (Nichter et al., 2010). Other explanations of high SHS exposure among women may include having no household rules for smoking, poor knowledge about the risks of SHS exposure and misconceptions regarding tobacco use (Nichter et al., 2010). We reiterate the recommendations of Öberg et al. (2011), who favour empowering and educating the women in LMICs to promote smoke-free policies to protect themselves and their families from SHS exposure.
In most of the LMICs studied, participants in urban settings were more likely to live in a smoke-free home compared with those from rural settings. This could partially be explained by the typical enclosed structure of urban dwellings, which prevents smoke from dissipating to the outside environment and make smoke undesirable in this setting, compared with the rural dwellings which typically have more open space, that would allow the smoke to dissipate faster into the surrounding outer environment thereby minimizing discomfort due to the smoke.
Strengths and limitations
We used nationally representative GATS data from 15 LMICs, which include some of the most populous nations of the world. We found a consistent association between being employed in a smoke-free workplace and living in a smoke-free home across these vastly differing cultural settings, which have different smoking prevalence rates and varying implementation of tobacco control policies, including smoke-free policies. Our data were cross-sectional and restricted our ability to determine causal direction. However, previous longitudinal studies conducted in high income countries have demonstrated that persons employed in a smoke-free workplace are more likely to live in a smoke-free home prospectively (Cheng et al., 2011, Cheng et al., 2013, Edwards et al., 2008, Fong et al., 2006). Future longitudinal studies should be undertaken in LMICs to rule out the possibility of reverse causation. Educational and occupational classifications varied and were not always comparable between GATS countries e.g. occupation in China and education in Brazil. For these, we conducted sensitivity analyses after excluding these variables from the analyses and our results remained substantially unchanged. We relied on self-reported measures for exposure to SHS at home and workplaces in the absence of biological markers such as cotinine levels. However, a good correlation has been shown between cotinine levels and self-reported measures in previous studies (Emmons et al., 1994).
Policy implications
The United Nations High Level Meeting on non-communicable diseases (NCDs) in September 2011 recommended establishing tobacco-free workplaces as an important component for NCD prevention and control (United Nations, 2012). Our findings strengthen the case for rapid implementation of smoke-free policies in LMICs involving complete elimination of smoking and SHS exposure from workplaces. However, leadership and action at the national level by governments is the key for strengthening the implementation of smoke-free policies. The Government of Russian Federation recently demonstrated such leadership by enacting new comprehensive tobacco control policies, which resulted in smoke-free policies being extended beyond indoor public places to outdoor public places such as playgrounds and beaches from June 2013 (Campaign for Tobacco-Free Kids, 2013, World Lung Foundation, 2013). From 2014, all the hospitality venues shopping areas, public transport, terminals and ports in Russian Federation are required to be 100% smoke-free.
Conclusion
Associations between being employed in a smoke-free workplace and living in a smoke-free home, previously demonstrated in high income countries, also exist in the LMICs. Accelerating implementation of comprehensive smoke-free public place policies is likely to result in substantial population health gain in these settings.
The following are the supplementary data related to this article.
Definition of variables.
Conflict of interest statement
The authors declare that there are no conflicts of interest.
Sources of funding
This work was supported by a Wellcome Trust Capacity Strengthening Strategic Award to the Public Health Foundation of India and a consortium of UK universities. CM is funded by the National Institute of Health Research and Higher Education Funding Council for England. SAG is funded by the National Cancer Institute (CA-61021). The funding bodies had no involvement in the study design; in the collection, analysis and interpretation of data; and in the decision to submit the article for publication.
Contributions
GPN contributed to data analysis, interpretation of data, drafting the manuscript and revising it critically for intellectual content. JTL contributed to data analysis and interpretation of data. SAG, MA, NP and CM provided technical guidance on study concept & design, interpretation of results, critical comments on the manuscript and gave final approval for submission.
Acknowledgments
GPN is also supported by grant number 1 D43 HD065249 from the Fogarty International Center and the Eunice Kennedy Shriver National Institute of Child Health & Human Development at the National Institutes of Health.
The authors would also like to acknowledge the GATS country surveillance teams; WHO Regional Surveillance Officers; CDC Global Tobacco Control Branch; and the Bloomberg Initiative to Reduce Tobacco Use, a program of Bloomberg Philanthropies, for providing financial support to GATS.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-No Derivative Works License, which permits non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- Berg C.J., Daley C.M., Nazir N., Cully A., Pacheco C.M., Buchanan T., Ahluwalia J.S., Greiner K.A., Choi W.S. Smoke-free policies in the workplace and in the home among American Indians. J. Health Dispar. Res. Pract. 2012;5:81–91. [PMC free article] [PubMed] [Google Scholar]
- Brown A., Moodie C., Hastings G. A longitudinal study of policy effect (smoke-free legislation) on smoking norms: ITC Scotland/United Kingdom. Nicotine Tob. Res. 2009;11:924–932. doi: 10.1093/ntr/ntp087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- California Environmental Health Protection Agency . California Environmental Health Protection Agency Office of Environmental Health Hazard Assessment Air Toxicology and Epidemiology Branch; CA: 2005. Proposed Identification of Environmental Tobacco Smoke as a Toxic Air Contaminant. Part B: Health Effects. [Google Scholar]
- Campaign for Tobacco-Free Kids Country Details for Russia: Smoke Free Status of Indoor Public Places, Workplaces, and Public Transport. 2013. http://www.tobaccocontrollaws.org/legislation/country/russia/sf-indoor [Online] Available: (Accessed June 13 2013)
- Centers for Disease Control and Prevention State-Specific Prevalence of Smoke-Free Home Rules — United States, 1992–2003. MMWR. 2007;56:501–504. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Global Tobacco Surveillance System: Data. 2013. http://nccd.cdc.gov/gtssdata/Ancillary/DataReports.aspx?CAID=3 [Online]. Available: (Accessed May 31 2013)
- Centers for Disease Control and Prevention Global Adult Tobacco Survey: Factsheet China 2010. 2013. http://nccd.cdc.gov/gtssdata/Default/CountryResults.aspx?TYPE=A&SRCH=&SUID=GATS&SYID=RY&CAID=&SCID=TT&QUID=QQ&WHID=&COID=ch&LOID=ch100&DCOL=&DSRT=DEFAULT&DODR=ASC&DSHO=&DCIV=&DCSZ=&FCHL=&FSEL=&FPRL=&FAGL=&FREL=&FDSC=&MPVW= [Online]. Available: (Accessed June 13 2013)
- Cheng K.W., Glantz S.A., Lightwood J.M. Association between smokefree laws and voluntary smokefree-home rules. Am. J. Prev. Med. 2011;41:566–572. doi: 10.1016/j.amepre.2011.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng K.W., Okechukwu C.A., McMillen R., Glantz S.A. Association between clean indoor air laws and voluntary smokefree rules in homes and cars. Tob. Control. 2013 doi: 10.1136/tobaccocontrol-2013-051121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards R., Thomson G., Wilson N., Waa A., Bullen C., O'dea D., Gifford H., Glover M., Laugesen M. After the smoke has cleared: evaluation of the impact of a new national smoke-free law in New Zealand. Tob. Control. 2008;17:e2. doi: 10.1136/tc.2007.020347. [DOI] [PubMed] [Google Scholar]
- Emmons K.M., Abrams D.B., Marshall R., Marcus B.H., Kane M., Novotny T.E., Etzel R.A. An evaluation of the relationship between self-report and biochemical measures of environmental tobacco smoke exposure. Prev. Med. 1994;23:35–39. doi: 10.1006/pmed.1994.1005. [DOI] [PubMed] [Google Scholar]
- Fong G.T., Hyland A., Borland R., Hammond D., Hastings G., Mcneill A., Anderson S., Cummings K.M., Allwright S. Reductions in tobacco smoke pollution and increases in support for smoke-free public places following the implementation of comprehensive smoke-free workplace legislation in the Republic of Ireland: findings from the ITC Ireland/UK Survey. Tob. Control. 2006;15:Siii51–Siii58. doi: 10.1136/tc.2005.013649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giovino G.A., Mirza S.A., Samet J.M., Gupta P.C., Jarvis M.J., Bhala N., Peto R., Zatonski W., Hsia J. Tobacco use in 3 billion individuals from 16 countries: an analysis of nationally representative cross-sectional household surveys. Lancet. 2012;380:668–679. doi: 10.1016/S0140-6736(12)61085-X. [DOI] [PubMed] [Google Scholar]
- Glantz S.A., Slinker B.K. 3rd ed. McGraw-Hill Inc.; New York: 2001. Primer of Applied Regression and Analysis of Variance. [Google Scholar]
- Hovell M.F., Hughes S.C. The behavioral ecology of secondhand smoke exposure: a pathway to complete tobacco control. Nicotine Tob. Res. 2009;11:1254–1264. doi: 10.1093/ntr/ntp133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Agency for Research on Cancer . vol. 13. IARC; Lyon: 2009. IARC handbooks of cancer prevention: tobacco control. (Evaluating the Effectiveness of Smoke-Free Policies). [Google Scholar]
- Johnson K.C., Miller A.B., Collishaw N.E., Palmer J.R., Hammond S.K., Salmon A.G., Cantor K.P., Miller M.D., Boyd N.F. Active smoking and secondhand smoke increase breast cancer risk: the report of the Canadian Expert Panel on Tobacco Smoke and Breast Cancer Risk (2009) Tob. Control. 2011;20:e2. doi: 10.1136/tc.2010.035931. [DOI] [PubMed] [Google Scholar]
- Kabir Z., Daly S., Clarke V., Keogan S., Clancy L. Smoking ban and small-for-gestational age births in Ireland. PLoS One. 2013;8:e57441. doi: 10.1371/journal.pone.0057441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King B.A., Mirza S.A., Babb S.D. A cross-country comparison of secondhand smoke exposure among adults: findings from the Global Adult Tobacco Survey (GATS) Tob. Control. 2013;22:e5. doi: 10.1136/tobaccocontrol-2012-050582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.T., Agrawal S., Basu S., Glantz S.A., Millett C. Association between smoke-free workplace and second-hand smoke exposure at home in India. Tob. Control. 2013 doi: 10.1136/tobaccocontrol-2012-050817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millett C., Lee J.T., Laverty A.A., Glantz S.A., Majeed A. Hospital admissions for childhood asthma after smoke-free legislation in England. Pediatrics. 2013;131:e495–e501. doi: 10.1542/peds.2012-2592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichter M., Greaves L., Bloch M., Paglia M., Scarinci I., Tolosa J.E., Novotny T.E. Tobacco use and secondhand smoke exposure during pregnancy in low- and middle-income countries: the need for social and cultural research. Acta Obstet. Gynecol. Scand. 2010;89:465–477. doi: 10.3109/00016341003592552. [DOI] [PubMed] [Google Scholar]
- Öberg M., Jaakkola M.S., Woodward A., Peruga A., Prüss-Ustün A. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet. 2011;377:139–146. doi: 10.1016/S0140-6736(10)61388-8. [DOI] [PubMed] [Google Scholar]
- Palipudi K.M., Gupta P.C., Sinha D.N., Andes L.J., Asma S., Mcafee T. Social determinants of health and tobacco use in thirteen low and middle income countries: evidence from Global Adult Tobacco Survey. PLoS One. 2012;7:e33466. doi: 10.1371/journal.pone.0033466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St. Claire A.W., Boyle R.G., Schillo B.A., Rode P., Taylor K.A. Smokefree home rules adoption by smokers and nonsmokers: Minnesota, 1999–2010. Am. J. Prev. Med. 2012;43:S197–S204. doi: 10.1016/j.amepre.2012.07.042. [DOI] [PubMed] [Google Scholar]
- Tan C.E., Glantz S.A. Association between smoke-free legislation and hospitalizations for cardiac, cerebrovascular, and respiratory diseases: a meta-analysis. Circulation. 2012;126:2177–2183. doi: 10.1161/CIRCULATIONAHA.112.121301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang H., Cowling D.W., Lloyd J.C., Rogers T., Koumjian K.L., Stevens C.M., Bal D.G. Changes of attitudes and patronage behaviors in response to a smoke-free bar law. Am. J. Public Health. 2003;93:611–617. doi: 10.2105/ajph.93.4.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2006. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. [Google Scholar]
- United Nations Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases. 2012. http://www.who.int/nmh/events/un_ncd_summit2011/political_declaration_en.pdf [Online]. Available: (Accessed June 5 2013)
- Visvanathan N., Duggan L., Wiegersma N., Nisonoff L. 2nd ed. Zed Books Ltd.; New York: 2011. The Women, Gender and Development Reader. [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2003. WHO Framework Convention on Tobacco Control. [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2011. WHO Report on the Global Tobacco Epidemic, 2011: Warning About the Dangers of Tobacco. [Google Scholar]
- World Health Organization Tobacco Factsheet. 2013. http://www.who.int/mediacentre/factsheets/fs339/en/ [Online] Available: (Accessed October 19, 2013)
- World Health Organization Parties to the WHO Framework Convention on Tobacco Control. 2013. http://www.who.int/fctc/signatories_parties/en/index.html [Online]. Available: (Accessed May 23 2013)
- World Health Organization Tobacco Free Initiative (TFI): Global Adult Tobacco Survey (GATS) 2013. http://www.who.int/tobacco/surveillance/gats/en/ [Online]. Available: (Accessed May 31 2013)
- World Lung Foundation World Lung Foundation Congratulates Russian Government on Progress Towards New National Tobacco Control Law. 2013. http://www.worldlungfoundation.org/ht/display/ReleaseDetails/i/22993/pid/6858 [Online]. Available: (Accessed June 13 2013)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Definition of variables.