Abstract
Objective:
The aim of this study was to assess the accuracy of ultrasonography in the diagnosis of chronic lateral ankle ligament injury.
Methods:
A total of 120 ankles in 120 patients with a clinical suspicion of chronic ankle ligament injury were examined by ultrasonography by using a 5- to 17-MHz linear array transducer before surgery. The results of ultrasonography were compared with the operative findings.
Results:
There were 18 sprains and 24 partial and 52 complete tears of the anterior talofibular ligament (ATFL); 26 sprains, 27 partial and 12 complete tears of the calcaneofibular ligament (CFL); and 1 complete tear of the posterior talofibular ligament (PTFL) at arthroscopy and operation. Compared with operative findings, the sensitivity, specificity and accuracy of ultrasonography were 98.9%, 96.2% and 84.2%, respectively, for injury of the ATFL and 93.8%, 90.9% and 83.3%, respectively, for injury of the CFL. The PTFL tear was identified by ultrasonography. The accuracy of identification between acute-on-chronic and subacute–chronic patients did not differ. The accuracies of diagnosing three grades of ATFL injuries were almost the same as those of diagnosing CFL injuries.
Conclusion:
Ultrasonography provides useful information for the evaluation of patients presenting with chronic pain after ankle sprain.
Advances in knowledge:
Intraoperative findings are the reference standard. We demonstrated that ultrasonography was highly sensitive and specific in detecting chronic lateral ligments injury of the ankle joint.
Ankle injuries are among the most common injuries seen in a clinic. Approximately 85% of sprained ankles involve the lateral ligament complex, which is composed of the anterior talofibular ligament (ATFL), the calcaneofibular ligament (CFL) and the posterior talofibular ligament (PTFL). The ATFL followed by the CFL are the most common sites of damage. The PTFL is rarely disrupted in inversion injuries, unless there is concomitant severe ankle dislocation.1,2 After lateral ligament injury, joint incongruity leads to chronic ankle instability in approximately 20% of cases. This may cause degenerative changes progressing towards early ankle osteoarthritis.3 Therefore, it is important to establish a diagnosis and correct the chronic mechanical instability.
Classically, clinical diagnosis of lateral ankle ligament injury is reliant on clinical examination combined with imaging studies, such as stress radiography and MRI. Although stress radiography is quite reliable, the procedure is painful and requires at least local anaesthesia.4 MRI has high accuracy but is expensive.5,6
Some researchers have assessed the value of ultrasonography in detecting injuries of the lateral ankle ligaments and have obtained high sensitivity.7–10 However, the reference standard in these articles is the clinical findings or other imaging studies (e.g. MRI). Studies that use intraoperative or arthroscopy findings as the gold standard are rare, and no differentiation has been made between complete tear and partial tear.5,11 The aim of this prospective study was to investigate the effectiveness of ultrasonography examination in diagnosing lateral ankle ligament injury compared with surgical findings.
METHODS AND MATERIALS
Between January 2010 and November 2012, 485 patients with clinical suspicion of lateral ankle ligament injuries referred to the sports medicine clinic of a tertiary referral hospital after sprain underwent ultrasonography examination of the lateral ankle. All patients whose symptoms had been present for at least 6 weeks complained of lateral ankle pain with or without swelling and had point tenderness over the lateral portion of the ankle on physical examination. Of these, 120 patients (85 males and 35 females) with a mean age of 32 years (range, 15–70 years) and who had been operated on were recruited. The indication for surgery was based on the medical history, the clinical findings and, if relevant, on conventional radiographs or MRI. The results of ultrasound were not used as diagnostic criteria. The preoperative clinical diagnosis was (1) chronic ankle instability, 90 cases; (2) impingement syndrome, including anterior bony impingement and anterior soft-tissue impingement, 8 cases; (3) osteochondral lesions, 5 cases; (4) arthritis, including traumatic arthritis and osteoarthritis, 12 cases; and (5) chronic syndesmotic injury, 5 cases. The duration of symptoms ranged from 6 weeks to 20 years (mean, 2.2 years). A patient undergoing ultrasonography examination within 4 weeks after a recent sprain was classified as an acute-on-chronic patient and one within more than 4 weeks was classified as a subacute–chronic patient. Patients with other combined diseases, such as rheumatoid disease or arthritis, were excluded from the study. Most of the operations were performed as soon as possible after ultrasonography was completed, with a mean ultrasonography-to-surgery interval of 4 days (1–7 days). The institutional ethics review board approved this study, and informed consent was obtained from the patients.
Real-time ultrasound scanning was performed with an iU22 ultrasonography unit (Philips Medical Systems, Bothell, WA) by a senior radiologist who has 7 years' experience in musculoskeletal ultrasonography. A wide-frequency linear array transducer (5–17 MHz) was used. The ultrasound examiner was blinded to the diagnosis and other examination results of the patients. During the examination, subjects were in a supine position with the ankle passively placed in a maximal inversion and plantar flexion position. Both axial and transversal sonography of the lateral ligaments carried out. Particular attention was paid to keeping the ultrasound beam perpendicular to the ligament to avoid artefact. Bilateral examination was performed if required. The sonograms were classified on the basis of severity of the injury to an individual ankle ligament: Grade 0, no injury (Figure 1); Grade 1, stretched or swollen ligament without tear (Figure 2); Grade 2, partial tear (Figures 3 and 4); and Grade 3, complete tear of the ligament (Figures 5–7).
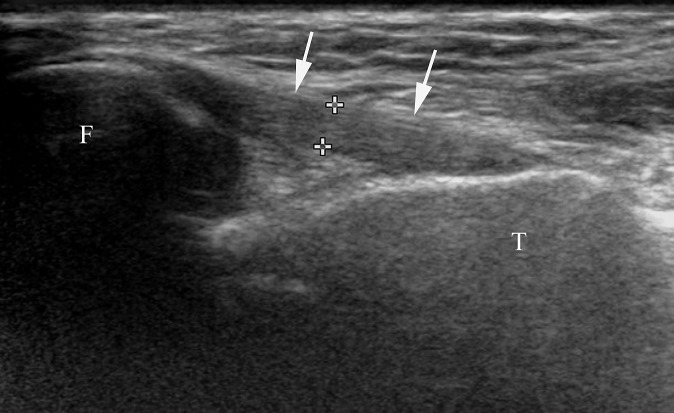
Figure 1.
Ultrasonographic view of a normal anterior talofibular ligament (arrows) about 1.9 mm thick (calipers). F, fibula; T, talus.
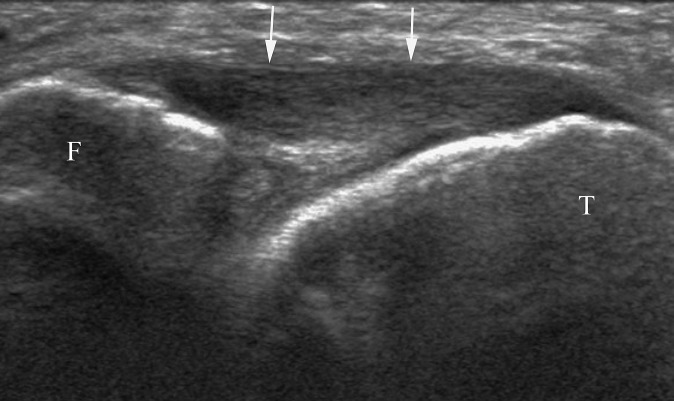
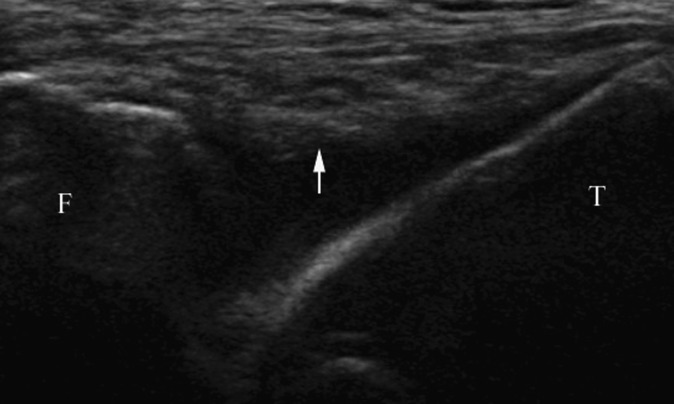
Figure 2.
Sonogram shows a swollen anterior talofibular ligament (arrows). F, fibula; T, talus.
Figure 3.
Transverse sonogram shows a partial tear (arrow) of the anterior talofibular ligament. The ligament is about 2.9 mm thick (calipers). A small amount of fluid (asterisk) in the ankle joint underlines the deep aspect of the ligament. F, fibula; T, talus.
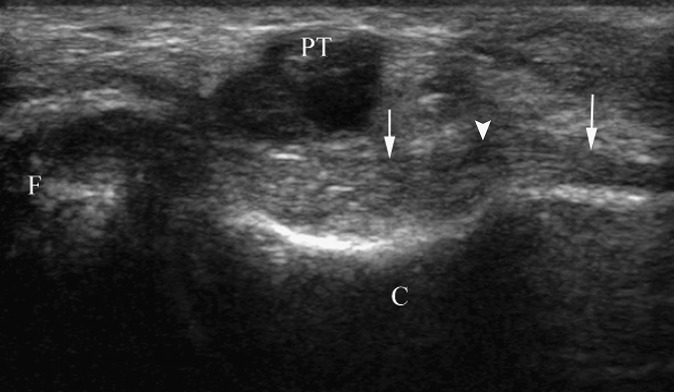
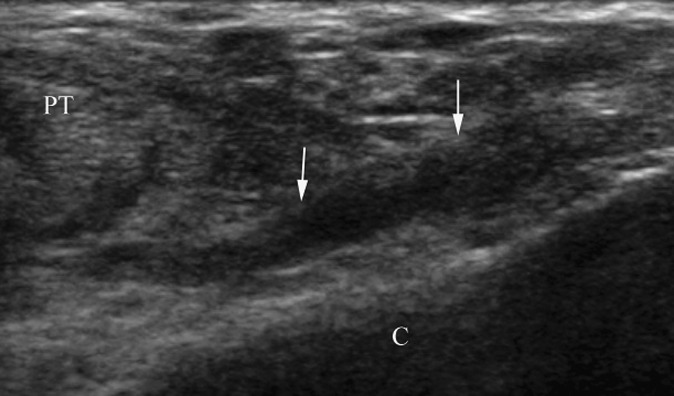
Figure 4.
Sonogram shows a partial tear (arrowhead) of the calcaneofibular ligament (arrows) near the attachment of the calcaneus. C, calcaneus; F, fibula; PT, peroneal tendons.
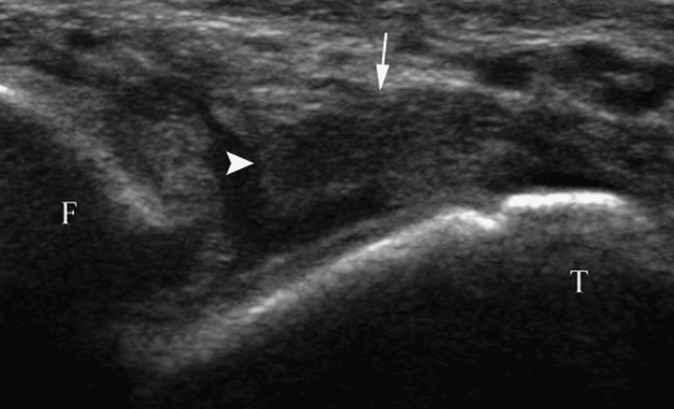
Figure 5.
Sonogram shows a complete tear (arrowhead) of the anterior talofibular ligament (arrow). F, fibula; T, talus.
Figure 7.
A complete tear of the calcaneofibular ligament at the attachment of the calcaneus. Scar tissue (arrows) is seen instead of normal ligament fibre. C, calcaneus, PT, peroneal tendons.
To check the intraobserver reliability and repeatability of the ultrasonography examination, the findings of the radiologist in this study were gauged against those of another musculoskeletal radiologist with similar clinical experience in a preliminary study, which was performed before the present study, with 30 patients (9 females and 21 males). The selection criteria were the same as those used in the present study.
Operations were carried out by an experienced sports medicine surgeon who was blinded to the ultrasonography results. All patients underwent ankle arthroscopy, 42 of whom had open surgery. During the operations, the contour of the ligament was examined and the injury was clarified. The surgical findings were classified into the same grades as those used in the ultrasonography classification. Grade 1, Grade 2 and Grade 3 were defined as lateral ligament injury.
Ultrasonography results were compared with surgical findings, which were used as the standard of reference. The sensitivities, specificities, accuracies and negative and positive predictive values were calculated using the statistical software program SPSS® v. 16.0 (SPSS Inc., Chicago, IL). The level of concordance between the results obtained by the two radiologists in the pilot study was evaluated with the k index. The χ2 test was used to compare the accuracy between ultrasonography diagnosis and findings during surgery of ATFL and CFL injury and of acute-on-chronic and subacute–chronic cases. A p-value ≤ 0.05 was considered statistically significant.
RESULTS
The results of the pilot study showed a high level of concordance between the measurements of the two radiologists in identifying injury of the ATFL [24 (80%) of 30 patients vs 25 (83%) of 30 patients; k = 0.89].
Surgery demonstrated that 94 (78.3%) of 120 patients had a lateral ligament injury. There were 18 sprains, 24 partial and 52 complete tears of the ATFL; 26 sprains, 27 partial and 12 complete tears of the CFL; and 1 complete tear of the PTFL. Ultrasonography demonstrated ATFL injury in 93 out of 94 cases and CFL injury in 61 out of 65 cases (Table 1). The results of ultrasound examination and surgery corresponded in 101 out of 120 cases of ATFL injury and in 100 out of 120 cases in CFL injury, which gave an accuracy of 84.2% and 83.3%, respectively. The sensitivity of diagnosing ATFL and CFL injuries was 98.9% and 93.8%, respectively. The specificity of diagnosing ATFL and CFL injuries was 96.2% and 90.9%, respectively. Ultrasonography had detected the only PTFL tear. Regarding the ultrasonography findings of the ATFL injuries, the sensitivity was not so high in detecting Grade 1 injuries. The sensitivity was low in determining complete tear (Grade 3) of the CFL. The specificity of detection of lateral ligament injury ranged between 87.1% and 99.1%. Generally, the accuracy of detection of ATFL injury was almost the same as that of CFL injury. Only in the Grade 0 group was a statistically significant result found (Table 2). There were 40 acute-on-chronic patients and 80 subacute-chonic patients. We did not find any statistical significance of accuracy for evaluating lateral ligament injury between the acute-on-chronic and subacute–chonic groups (Table 3).
Table 1.
Comparison of ultrasonography and surgical findings
| ATFL |
CFL |
|||
|---|---|---|---|---|
| Surgery (+) | Surgery (−) | Surgery (+) | Surgery (−) | |
| Grade 0 | ||||
| Ultrasonography (+) | 25 | 1 | 50 | 4 |
| Ultrasonography (−) | 1 | 93 | 5 | 61 |
| Grade 1 | ||||
| Ultrasonography (+) | 12 | 3 | 21 | 3 |
| Ultrasonography (−) | 6 | 99 | 5 | 91 |
| Grade 2 | ||||
| Ultrasonography (+) | 21 | 11 | 23 | 12 |
| Ultrasonography (−) | 3 | 85 | 4 | 81 |
| Grade 3 | ||||
| Ultrasonography (+) | 43 | 4 | 6 | 1 |
| Ultrasonography (−) | 9 | 64 | 6 | 107 |
ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament.
Table 2.
Validity of ultrasonography in the diagnosis of anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL) lesions
| Ultrasonography | Location | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) | p-value |
|---|---|---|---|---|---|---|---|
| Grade 0 | ATFL | 96.2 | 98.9 | 96.2 | 98.9 | 98.3 | 0.031 |
| CFL | 90.9 | 93.8 | 92.6 | 92.4 | 92.5 | ||
| Grade 1 | ATFL | 66.7 | 97.1 | 80.0 | 94.3 | 92.5 | 0.801 |
| CFL | 80.8 | 96.8 | 87.5 | 94.8 | 93.3 | ||
| Grade 2 | ATFL | 87.5 | 88.5 | 65.6 | 96.6 | 88.3 | 0.696 |
| CFL | 85.2 | 87.1 | 65.7 | 95.3 | 86.7 | ||
| Grade 3 | ATFL | 82.7 | 94.1 | 91.5 | 87.7 | 89.2 | 0.161 |
| CFL | 50.0 | 99.1 | 85.7 | 94.7 | 94.2 |
NPV, negative predictive value; PPV, positive predictive value.
Table 3.
Accuracy of detecting ligament injury in acute-on-chronic and subacute–chronic groups
| Group | Accuracy (%) | p-value |
|---|---|---|
| ATFL | ||
| Acute-on-chronic | 85.0 | |
| Subacute–chronic | 83.8 | 0.860 |
| CFL | ||
| Acute-on-chronic | 82.5 | |
| Subacute–chronic | 83.8 | 0.862 |
ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament.
DISCUSSION
Lateral ligament injuries are common during ankle sprains, and some patients develop mechanical or functional instability, which can result in chronic ankle instability, including persistent ankle pain, functional instability and swelling.3,12 Chronic ankle instability is a very disabling condition. There is little agreement among surgeons as to the most effective treatment of lateral ligament injuries. Although most patients may recover with conservative treatment, operative treatment leads to a superior long-term outcome in patients with rupture of at least one of the lateral ligaments of the ankle.3,13 In cases where surgery is considered, it is important not only to detect an injury of the lateral ligaments but also to document its exact extent. Accordingly, it is important to choose accurate diagnostic tools and proper treatment procedures to enhance recovery and to prevent chronic joint instability.
MRI can depict lateral ligament injuries of the ankle, including discontinuity or absence, increased signal within the ligament and ligamentous irregularity or waviness with normal thickness and signal intensity.5,6,14,15 MRI showed a sensitivity of 97% and a specificity of 100% for ATFL injuries compared with arthroscopy. 5 However, owing to the poor availability, high costs and high incidence of ankle injuries, MRI has limited indications.
Using optimal ultrasonography frequency, the ligaments can be depicted with excellent resolution. Sonography of normal lateral ligaments shows a band-like structure made up of many fibrillar hyperechoic signals extending on a longitudinal axis plane and an oval shape on short-axis scans.7,16,17 After sprain, the enlargement, focal defect and abnormal lengthening of a ligament should be seen on ultrasonography and as a bony fragment within ligaments, which were all detected in the present study.18
In our study, the ability of ultrasonography to depict ATFL and CFL injuries with a sensitivity of 98.9% and 93.8%, respectively, and a specificity of 93.8% and 90.9%, respectively, was comparable to those of MRI.19 Hua et al11 reported a better result with an accuracy of 95.2% in detecting chronic ATFL injuries. One reason for the difference was that they did not classify “tear” as “partial tear” or “complete tear”. A low sensitivity was found for CFL complete tear (50%) in our research. This may be because of the CFL anatomy. It has a concave course, and the tip of the lateral malleolus is obviously protuberant, which makes evaluation of its malleolar insertion more difficult. Low sensitivity of CFL tears was also found in other studies on MRI.19,20 Among patients found to have lower grade injury on ultrasonography but severe grade on surgery, some cases were detected as scar tissues by macroscopy at operation. The scar tissue or organized haematoma, which fills the defect with echogenic material, may mimic the ligament integrity or partial tear (Figures 6 and 7). Some integrity ligaments and partial tears appeared as complete tears on ultrasonography, which may be partially because of anisotropy. When the ligament was wavy or loose, it was difficult to keep the ultrasound beam perpendicular to the ligament. Even a slight obliquity in the orientation of the ultrasonography beam leads to a hypoechoic appearance of the ligament, which is similar to ligament tear. Torn soft tissue that floats in the intracapsular fluid may also mimic the free end of the severed ligament and can therefore be a cause of misinterpretation.
Figure 6.
The anterior talofibular ligament fibre has been absorbed after tearing. Sonogram shows scar tissue (arrow) instead of the ligament fibre. F, fibula; T, talus.
There was a limitation of this study with operative findings as the standard. An intraligamentous longitudinal split or a small tear on the medial surface of a ligament (Figure 3) cannot be proved by macroscopy or even open surgery. But, ultrasonography can detect the intrinsic quality of ligaments. Some false-positive cases of Grade 2 may not be misdiagnosed when using ultrasonography. As intraligamentous tears or small tears need not require surgical intervention, the discordant findings do not influence the treatment strategy.
Our study may be criticized for a lack of intraobserver reliability of surgical findings since the surgical diagnostic criteria were relatively subjective.
In conclusion, ultrasonography as a convenient technique with low costs and real-time examination showed a satisfactory sensitivity and specificity for detecting lateral ligament injury. However, sonographic evaluation is usually considered to be strongly dependent on the expertise of the technician. Further studies should determine the standard criteria for examination and diagnosis to enable ultrasonography to be used in diagnosing lateral ligament injury and to have a definite role in the guidelines.
REFERENCES
- 1.Garrick JG. The frequency of injury, mechanism of injury, and epidemiology of ankle sprains. Am J Sports Med 1977; 5: 241-2. [DOI] [PubMed] [Google Scholar]
- 2.Boruta PM, Bishop JO, Braly WG, Tullos HS. Acute lateral ankle ligament injuries: a literature review. Foot Ankle 1990; 11: 107-13. [DOI] [PubMed] [Google Scholar]
- 3.Colville MR. Surgical treatment of the unstable ankle. J Am Acad Orthop Surg 1998; 6: 368-77. [DOI] [PubMed] [Google Scholar]
- 4.Frost SC, Amendola A. Is stress radiography necessary in the diagnosis of acute or chronic ankle instability? Clin J Sport Med 1999; 9: 40-5. [DOI] [PubMed] [Google Scholar]
- 5.Oae K, Takao M, Uchio Y, Ochi M. Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. Skeletal Radiol 2010; 39: 41-7. 10.1007/s00256-009-0767-x [DOI] [PubMed] [Google Scholar]
- 6.Cardone BW, Erickson SJ, Den Hartog BD, Carrera GF. MRI of injury to the lateral collateral ligamentous complex of the ankle. J Comput Assist Tomogr 1993; 17: 102-7. [DOI] [PubMed] [Google Scholar]
- 7.Milz P, Milz S, Steinborn M, Mittlmeier T, Reiser M. 13-MHz high frequency ultrasound of the lateral ligaments of the ankle joint and the anterior tibia-fibular ligament. Comparison and results of MRI in 64 patients. [In German.] Radiologe 1999; 39: 34-40. [DOI] [PubMed] [Google Scholar]
- 8.Gremeaux V, Coudreuse JM, Collado H, Cohen M, Bensoussan L, Fondarai J, et al. Comparative study of clinical and ultrasonographic evaluation of lateral collateral ligament sprains of the ankle. J Sports Med Phys Fitness 2009; 49: 285-91. [PubMed] [Google Scholar]
- 9.Guillodo Y, Varache S, Saraux A. Value of ultrasonography for detecting ligament damage in athletes with chronic ankle instability compared to computed arthrotomography. Foot Ankle Spec 2010; 3: 331-4. 10.1177/1938640010378531 [DOI] [PubMed] [Google Scholar]
- 10.Margetić P, Pavić R. Comparative assessment of the acute ankle injury by ultrasound and magnetic resonance. Coll Antropol 2012; 36: 605-10. [PubMed] [Google Scholar]
- 11.Hua Y, Yang Y, Chen S, Cai Y. Ultrasound examination for the diagnosis of chronic anterior talofibular ligament injury. Acta Radiol 2012; 53: 1142-5. 10.1258/ar.2012.120171 [DOI] [PubMed] [Google Scholar]
- 12.Wolfe MW, Uhl TL, Mattacola CG, McCluskey LC. Management of ankle sprains. Am Fam Physician 2001; 63: 93-104. [PubMed] [Google Scholar]
- 13.Pijnenburg AC, Bogaard K, Krips R, Marti RK, Bossuyt PM, van Dijk CN. Operative and functional treatment of rupture of the lateral ligament of the ankle. A randomised, prospective trial. J Bone Joint Surg Br 2003; 85: 525-30. [DOI] [PubMed] [Google Scholar]
- 14.Verhaven EF, Shahabpour M, Handelberg FW, Vaes PH, Opdecam PJ. The accuracy of three-dimensional magnetic resonance imaging in the diagnosis of ruptures of the lateral ligaments of the ankle. Am J Sports Med 1991; 19: 583-7. [DOI] [PubMed] [Google Scholar]
- 15.Gaebler C, Kukla C, Breitenseher MJ, Nellas ZJ, Mittlboeck M, Trattnig S, et al. Diagnosis of lateral ankle ligament injuries. Comparison between talar tilt, MRI and operative findings in 112 athletes. Acta Orthop Scand 1997; 68: 286-90. [DOI] [PubMed] [Google Scholar]
- 16.Milz P, Milz S, Putz R, Reiser M. 13 MHz high-frequency sonography of the lateral ankle joint ligaments and the tibiofibular syndesmosis in anatomic specimens. J Ultrasound Med 1996; 15: 277-84. [DOI] [PubMed] [Google Scholar]
- 17.De Maeseneer M, Marcelis S, Jager T, Shahabpour M, Van Roy P, Weaver J, et al. Sonography of the normal ankle: a target approach using skeletal reference points. AJR Am J Roentgenol 2009; 192: 487-95. 10.2214/AJR.08.1316 [DOI] [PubMed] [Google Scholar]
- 18.Peetrons P, Creteur V, Bacq C. Sonography of ankle ligaments. J Clin Ultrasound 2004; 32: 491-9. 10.1002/jcu.20068 [DOI] [PubMed] [Google Scholar]
- 19.Park HJ, Cha SD, Kim SS, Rho MH, Kwag HJ, Park NH, et al. Accuracy of MRI findings in chronic lateral ankle ligament injury: comparison with surgical findings. Clin Radiol 2012; 67: 313-18. 10.1016/j.crad.2011.08.025 [DOI] [PubMed] [Google Scholar]
- 20.Kumar V, Triantafyllopoulos I, Panagopoulos A, Fitzgerald S, van Niekerk L. Deficiencies of MRI in the diagnosis of chronic symptomatic lateral ankle ligament injuries. Foot Ankle Surg 2007; 13: 171-6. [Google Scholar]