Abstract
Necrotizing fasciitis is a life-threatening soft-tissue infection of bacterial origin, which involves mainly the deep fascia. Early recognition of this condition may be hampered by the uncommon nature of the disease and non-specificity of initial clinical signs and symptoms in less fulminant cases, making the role of imaging important. MRI is the most useful imaging modality in the diagnosis of necrotizing fasciitis. The presence of thick (>3 mm) hyperintense signal in the deep fascia (particularly intermuscular fascia) on fat-suppressed T2 weighted or short tau inversion–recovery images is an important marker for necrotizing fasciitis. Contrast enhancement of the thickened necrotic fascia can be variable, with a mixed-pattern of enhancement being more commonly encountered. Involvement of multiple musculofascial compartments increases the likelihood of necrotizing fasciitis. It is important to remember that T2-hyperintense signal in the deep fascia is not specific to necrotizing fasciitis and can also be seen in cases such as non-infective inflammatory fasciitis or muscle tear. In this pictorial essay, we aim to review the MRI findings in necrotizing fasciitis, discuss its limitations and pitfalls and identify differentiating features from non-necrotizing soft-tissue infections, such as cellulitis and infective myositis/pyomyositis, conditions which may clinically mimic necrotizing fasciitis.
Necrotizing fasciitis is characterized by rapidly progressive deep fascial necrosis resulting from bacterial toxin production.1,2 Necrotizing fasciitis can affect all age groups and can be broadly categorized into two types. Type 1 disease results from polymicrobial infection comprising of gram-negative aerobes and anaerobes, usually encountered in patients with co-morbid conditions such as diabetes mellitus. Type 2 disease is usually monomicrobial, with causative organisms such as Group A Streptococci, and affects otherwise healthy individuals.3 Clinical presentation includes redness, pain and swelling in the affected region along with features of sepsis. The characteristic feature of this condition is severe pain disproportionate to the degree of swelling and erythema. However, these signs and symptoms may be non-specific at initial presentation and may simulate other non-necrotizing soft-tissue infections like cellulitis and myositis. Urgent surgical debridement is an essential management consideration in necrotizing fasciitis, whereas a non-surgical conservative treatment is followed in cases of non-necrotizing soft-tissue infections. The useful role of imaging in diagnosing necrotizing fasciitis has been highlighted in the literature, with reported high sensitivity and specificity of MRI.1,2,4,5 This pictorial essay aims to review the MRI findings in necrotizing fasciitis, discuss its limitations and pitfalls and identify differentiating features from non-necrotizing soft-tissue infections, such as cellulitis and infective myositis/pyomyositis, conditions which may clinically mimic necrotizing fasciitis.
ANATOMICAL CONSIDERATIONS: FASCIA
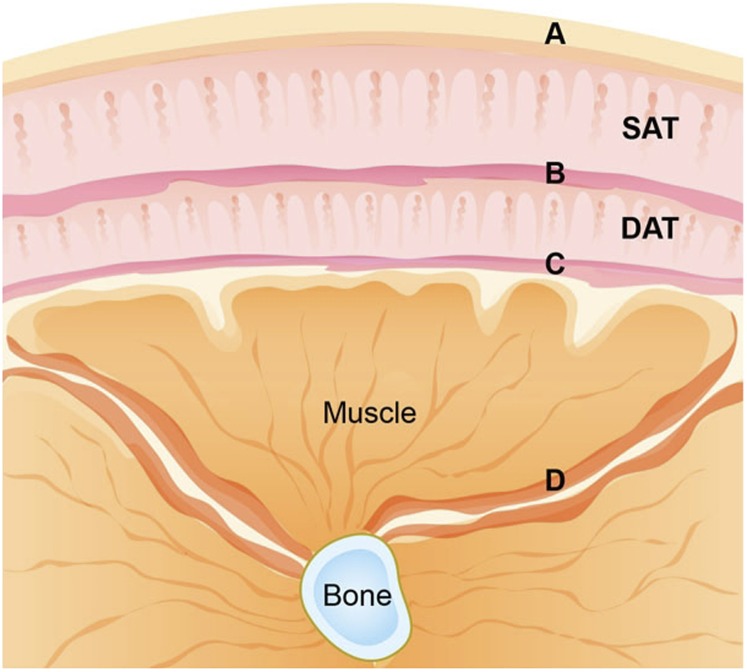
Having a clear concept of the organization of fascial layers is useful to understand the MRI manifestations of necrotizing fasciitis.2 Fasciae are fibroareolar or aponeurotic lamina that invest deeper tissues and organs and can be divided into superficial and deep fascia (Figure 1). The superficial fascia is a layer of adipose tissue that connects the skin and deep fascia. The deep fascia is composed of dense connective tissue that surrounds the muscles and other deeper structures. It consists of an outer investing layer or peripheral layer, which is attached to the epimysial layer of the muscles. Intermuscular fasciae are deeper extensions of the deep fascia that pass in-between the muscles and divide them into various compartments. Involvement of the intermuscular fascia is a better predictor of deep fascial involvement in necrotizing fasciitis.1,2 Recent anatomical research has shown the presence of a membranous layer in the superficial fascia, which is in close proximity to the deep fascia, separated by a layer of deep adipose tissue (Figure 1).6
Figure 1.
Fascial anatomy. Schematic drawing shows the superficial and deep fascia in the leg. A, skin; B, membranous layer of superficial fascia; C, peripheral layer of deep fascia; D, intermuscular layer of deep fascia; DAT, deep adipose tissue; SAT, superficial adipose tissue.
ROLE OF IMAGING
MRI is superior to all other imaging modalities for the detection of soft-tissue infections because of its remarkable soft-tissue imaging capabilities. Therefore, it is the modality of choice in imaging of suspected necrotizing fasciitis. In comparison, the role of other imaging modalities is limited. With radiography, the presence of soft-tissue gas is the only specific sign of necrotizing fasciitis but is seen only in a limited number of cases, in the presence of gas-forming organisms. Otherwise, radiographs may show non-specific findings of soft-tissue swelling and oedema, similar to cellulitis and myositis. CT performs better than radiography, because of its cross-sectional imaging capabilities, and it can reveal intermuscular fluid collections and fascial plane thickening with variable contrast enhancement.7 Ultrasonography may detect fluid collections within the fascial planes and also aid in imaging-guided diagnostic fluid aspiration.8
IDEAL IMAGING SEQUENCES FOR THE INVESTIGATION OF NECROTIZING FASCIITIS
MR sequences useful for the diagnosis of necrotizing fasciitis include T1 weighted fast spin-echo (SE), T2 weighted fat-suppressed fast SE and T1 weighted fat-suppressed gadolinium–diethylenetriaminepentaacetic acid (Gd-DTPA) contrast-enhanced fast SE sequences. In the presence of magnetic field inhomogeneities, T2 weighted fat-suppressed fast SE sequence can be replaced with inversion recovery sequences (such as short tau inversion–recovery or turbo inversion–recovery magnitude), as inversion recovery sequences are less susceptible to magnetic field inhomogeneity. T2 weighted gradient-echo sequence may be useful if there is suspicion of soft-tissue gas, which may be seen as the foci of blooming. The minimum scanning planes are axial and at least one other orthogonal (sagittal/coronal) plane. Gd-DTPA may be withheld in the presence of contraindications such as renal failure.
MRI FINDINGS IN NECROTIZING FASCIITIS
T2-hyperintense signal in the deep fascia (especially intermuscular fascia) is an essential component on MRI for the diagnosis of necrotizing fasciitis.1,2 Deep fascial thickening of >3 mm and extensive deep fascial multicompartment involvement further aid in diagnosis (Figure 2).1 Contrast enhancement can be variable, with the most common being a mixed pattern, where there is deep fascial enhancement along with non-enhancing portions.1
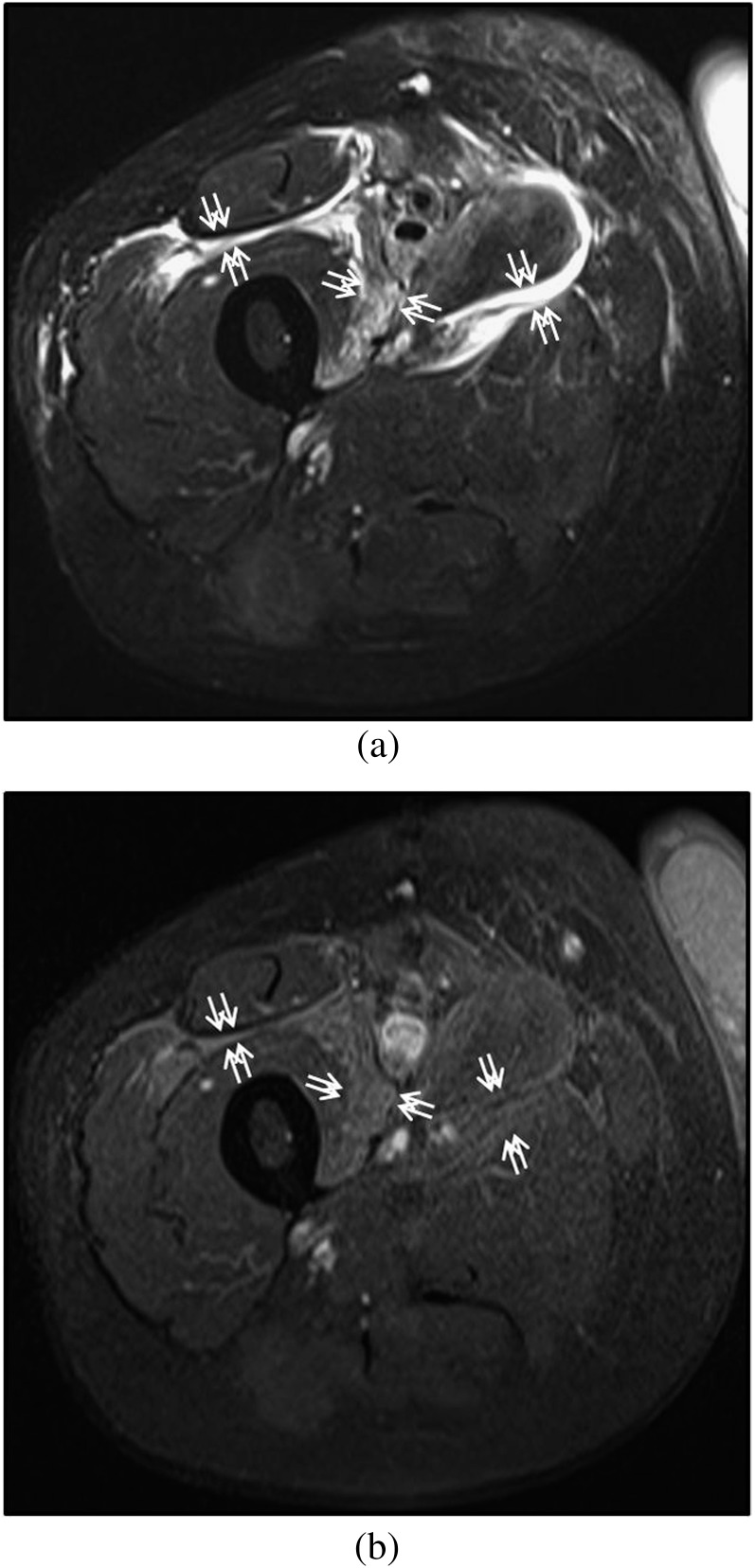
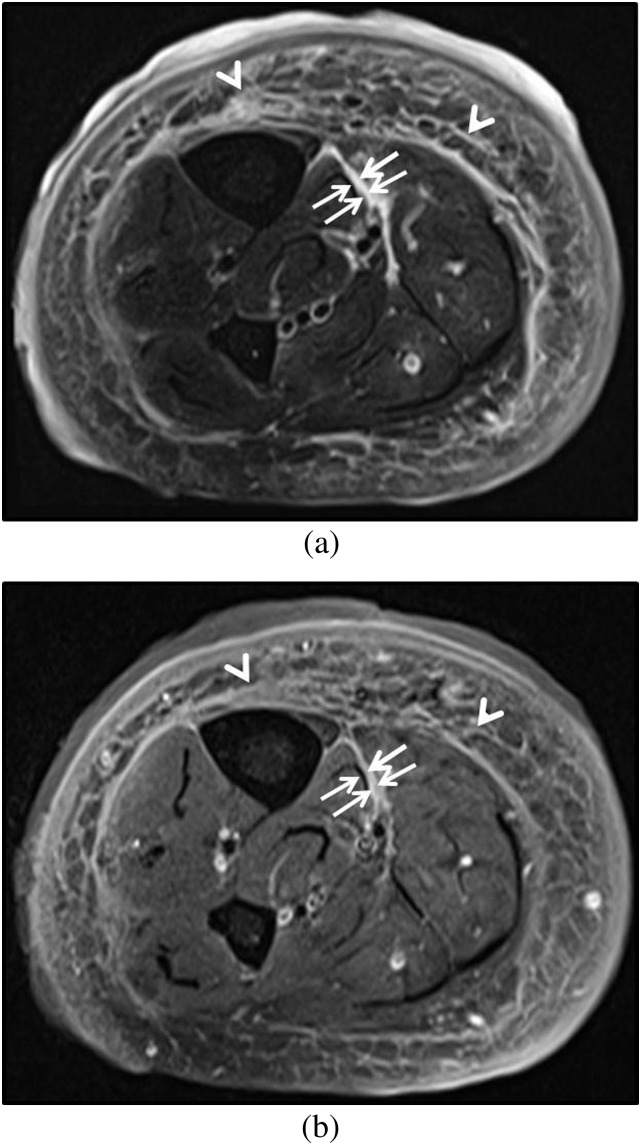
Figure 2.
Necrotizing fasciitis of the thigh in a 50-year-old female. (a) Axial T2 weighted MR image shows thick T2-hyperintense signal (white arrows) within the deep intermuscular fascia in the anterior and medial compartments of the thigh. (b) Axial post-contrast T1 weighted MR image shows absent to mild contrast enhancement (white arrows) in the deep intermuscular fascia at sites of the T2-hyperintense signal. At surgery, necrotic fascia with turbid fluid was found, consistent with necrotizing fasciitis.
T2 hyperintensity in deep fascia
Abnormal signal intensity and thickening of the deep intermuscular fascia is an important marker for necrotizing fasciitis on MRI. Associated signal changes in the superficial fascia may be seen; however, their absence does not exclude the diagnosis.2 In cases of necrotizing fasciitis, underlying fascial inflammation and necrosis leads to fascial thickening, interfascial fluid and perifascial hyperaemic changes resulting in areas of hypointense signal on T1 weighted and hyperintense signal on T2 weighted images (better characterized with fat suppression), with variable degree of contrast enhancement.1,2 In a study involving 30 patients, Kim et al1 reported two broad patterns of deep fascial involvement, namely: (a) partial involvement—whereby abnormal signal and thickening in deep fascia were found only at sites abutting the superficial fascia, (b) extensive involvement—with multicompartment and deeper involvement of the deep fascia, not limited to sites abutting the superficial fascia. In their series, all seven cases of necrotizing fasciitis showed extensive deep fascial involvement, and no case showed partial involvement. They also observed deep fascial thickening of >3 mm in 86% of cases of necrotizing fasciitis in comparison to 30% of cases of non-necrotizing fasciitis. In some cases, foci of hypointense signal (due to gas) may be noted within the fascial layers. These foci of signal void are better appreciated on gradient-echo images because of blooming artefact (Figure 3).
Figure 3.
Necrotizing fasciitis in the right upper limb of a 71-year-old male due to gas-forming organisms (Streptococcus anginosus). Radiograph shows faint air lucencies within the soft tissues (white arrows). (b) Axial T2 weighted MR image shows thick hyperintense signal in the deep intermuscular fascia (white arrows). (c) Axial T1 weighted MR image taken at a more distal level shows few tiny foci of signal void in the superficial fascia (white arrows). (d) Axial gradient-echo image shows blooming artefacts in the superficial fascia (white arrows) compatible with air foci—these are more apparent on the gradient-echo image than the T2 weighted image. (e) Urgent fasciotomy and surgical debridement was performed. Cultures grew Streptococcus anginosus.
Pattern of deep fascial contrast enhancement
A number of studies have highlighted the importance of contrast-enhanced fat-suppressed T1 weighted MRI for its complimentary role to T2 weighted fat-suppressed MR sequences in the diagnosis of necrotizing fasciitis. Variable patterns of enhancement of the deep fascia have been reported. Schmid et al9 reported contrast enhancement in areas of deep fascial T2 hyperintensity as an indicator of necrotizing fasciitis, and postulated that contrast enhancement represents contrast extravasation because of damage to the capillary network within the necrotic fascia. Kim et al1 found deep fascial enhancement with non-enhancing portions in 71% of cases of necrotizing fasciitis. In another series comprising 19 patients, enhancement of the deep fascia was reported in 82% of cases of necrotizing fasciitis.10 Brothers et al5 found the absence of deep fascial contrast enhancement to be associated with fascial necrosis in all their six cases of necrotizing fasciitis (100%). Because of a variable pattern of reported contrast enhancement, the use of T1 weighted fat-suppressed Gd-DTPA contrast-enhanced fast SE sequence has an adjunctive role to T2 weighted fat-suppressed MR sequence in the investigation for necrotizing fasciitis (Figure 4).
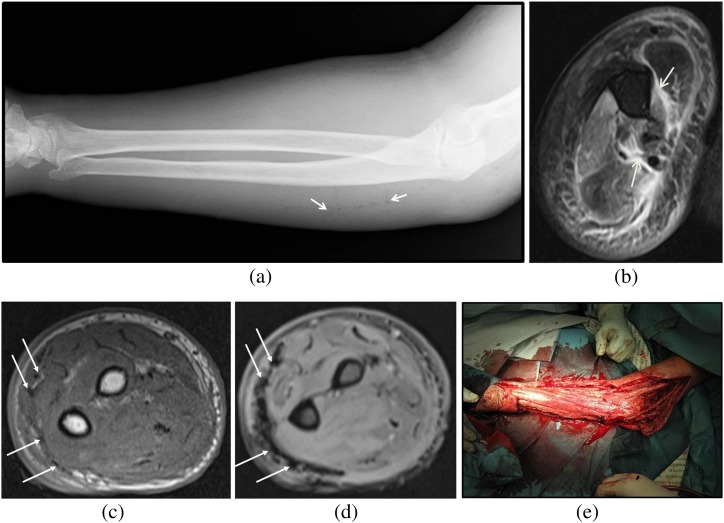
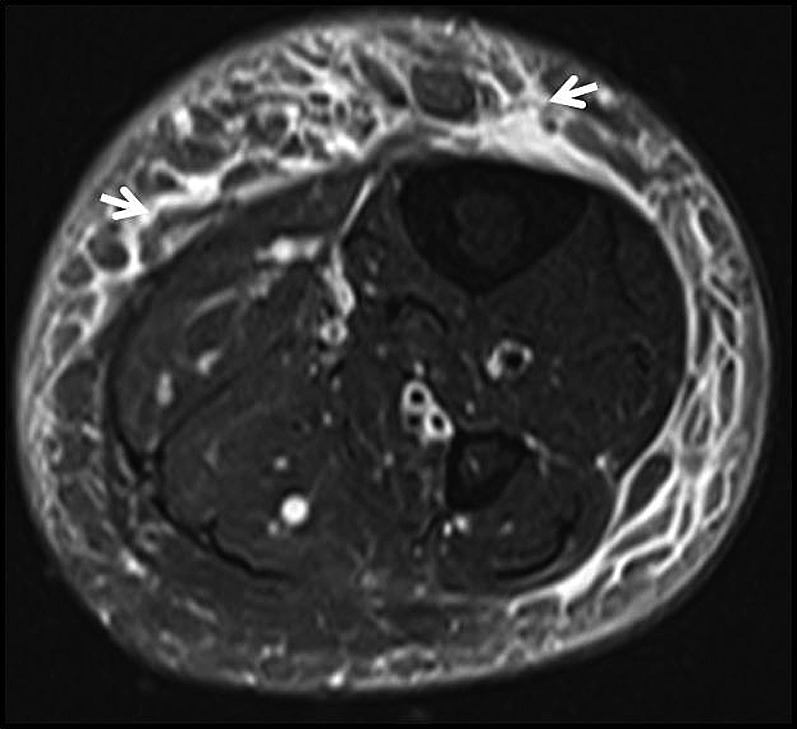
Figure 4.
Necrotizing fasciitis of the leg in a 21-year-old male with no underlying risk factors. (a) Axial fat-suppressed T2 weighted MR image of the mid-calf shows thick hyperintense fluid signal in the intermuscular fascia abutting the gastrocnemius muscle (white arrows). (b) Corresponding axial post-contrast fat-suppressed T1 weighted MR image showing mixed enhancing and non-enhancing areas, corresponding to T2 hyperintensity (white arrows). At surgery, early necrotizing fasciitis involving the fascia between superficial posterior and deep posterior compartments was found.
Muscle signal abnormalities
Muscle signal changes are considered to be reactive changes because of adjacent fascial inflammation and necrosis. These can be seen as either peripheral band-like or diffusely increased hyperintense signal on T2 weighted MR images, and can also show contrast enhancement.1 Rim-enhancing intramuscular collections are usually not a feature of necrotizing fasciitis; however, they may be seen in gradual-onset disease.9
PITFALLS AND LIMITATIONS ON MRI
Malghem et al2 reported the limited significance of mild thickening of the outer portion of the intermuscular (deep) fascia in diagnosing necrotizing fasciitis, especially if seen in continuity with signal abnormalities in the peripheral layer of deep fascia and subcutaneous fat (Figure 5). Signal abnormalities that are predominantly situated in the deeper portion of superficial fascia may appear as involvement of the peripheral layer of deep fascia, mimicking necrotizing fasciitis. Such cases mostly represent cellulitis rather than necrotizing fasciitis (Figure 6). In addition, signal abnormalities in the deep fascia are not specific for necrotizing fasciitis and can be observed in cases such as non-necrotizing infectious fasciitis, inflammatory (non-infective) fasciitis like eosinophilic fasciitis, idiopathic inflammatory myopathy, radiation-induced changes, ruptured popliteal cyst, lymphoedema and muscular/aponeurotic trauma (Figure 7).2
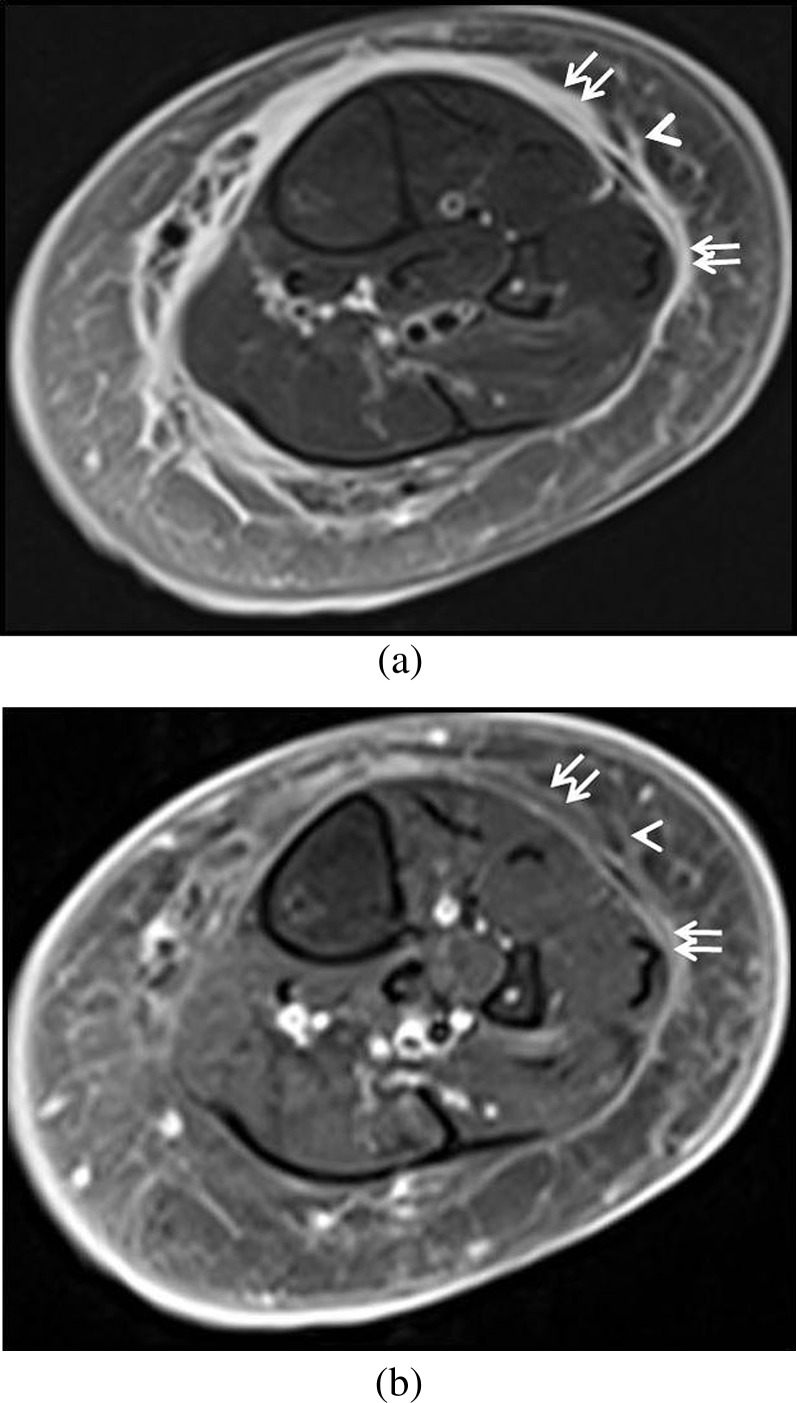
Figure 5.
Pitfalls on MRI. (a) Axial T2 weighted image shows a reticulated pattern of T2-hyperintense signal within the superficial fascia (white arrowheads) with associated thin linear T2-hyperintense signal in deep intermuscular fascia (white arrows). (b) Axial post-contrast T1 weighted image shows moderate contrast enhancement within the superficial fascia (white arrowheads) and at the site of thin linear T2-hyperintense signal in the deep intermuscular fascia (white arrows). Patient improved with intravenous antibiotics and was well at discharge.
Figure 6.
Pitfalls on MRI. (a) Axial T2 weighted MR image shows hyperintense signal located predominantly on outer aspect of the peripheral layer of deep fascia (white arrows) and within superficial fascia (white arrowhead). (b) Axial post-contrast T1 weighted MR image shows mild contrast enhancement in the deeper aspect of the superficial fascia, abutting the outer aspect of the peripheral layer of deep fascia (white arrows) and at sites of T2-hyperintense signal within superficial fascia (white arrowhead). Patient improved with intravenous antibiotics and was well at discharge.
Figure 7.
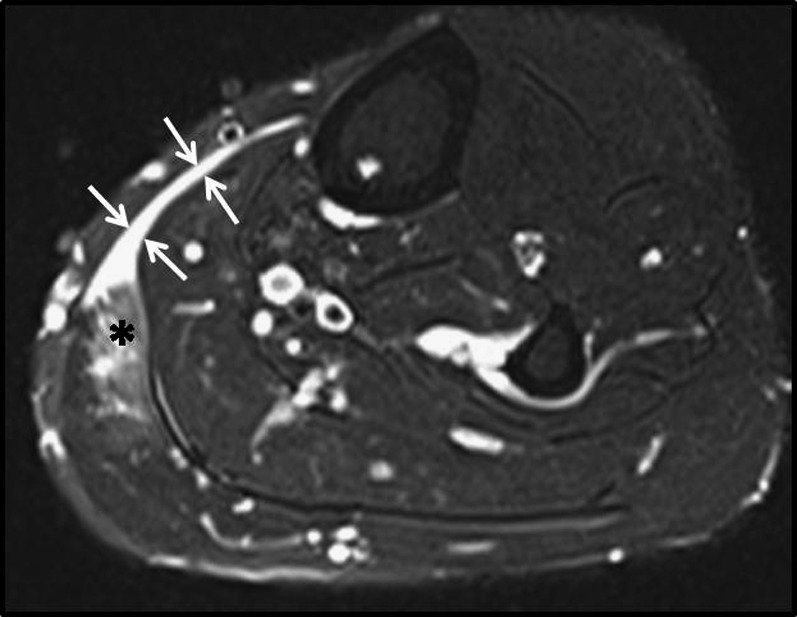
Pitfalls on MRI. Axial T2 weighted fat-suppressed MR image shows a tear of the medial edge of gastrocnemius (black asterisk) with fluid signal in the peripheral deep fascia (white arrows). Patient was managed conservatively.
SOFT-TISSUE INFECTIONS CLINICALLY MIMICKING NECROTIZING FASCIITIS
Cellulitis
Cellulitis is a superficial infection involving the dermis and the superficial fascia. A reticulated pattern of signal abnormalities is present within the superficial fascia, seen as hypointense signal on T1 weighted images and hyperintense signal on T2 weighted images (Figure 8).9 In cases of deep cellulitis, the deeper portion of the superficial fascia may show oedema and fluid collections and may mimic necrotizing fasciitis. Cases of deep cellulitis may be differentiated from necrotizing fasciitis by the absence of involvement of the deep intermuscular fascia.
Figure 8.
Cellulitis of the calf in a 42-year-old male. Axial fat-suppressed T2 weighted MR image shows T2-hyperintense signal with a reticulated appearance in the superficial fascia (arrows).
Infective myositis and pyomyositis
Pyomyositis is a pus-forming bacterial infection of the skeletal muscles. Both pyomyositis and necrotizing fasciitis may have similar clinical presentation of painful swelling and tenderness in the affected region.4 In contrast to necrotizing fasciitis, pyomyositis is predominantly characterized by intramuscular abscess formation (Figure 9). Cases of infective myositis without abscess formation (Stage 1 pyomyositis) can also mimic reactive muscle changes in necrotizing fasciitis (Figure 10).
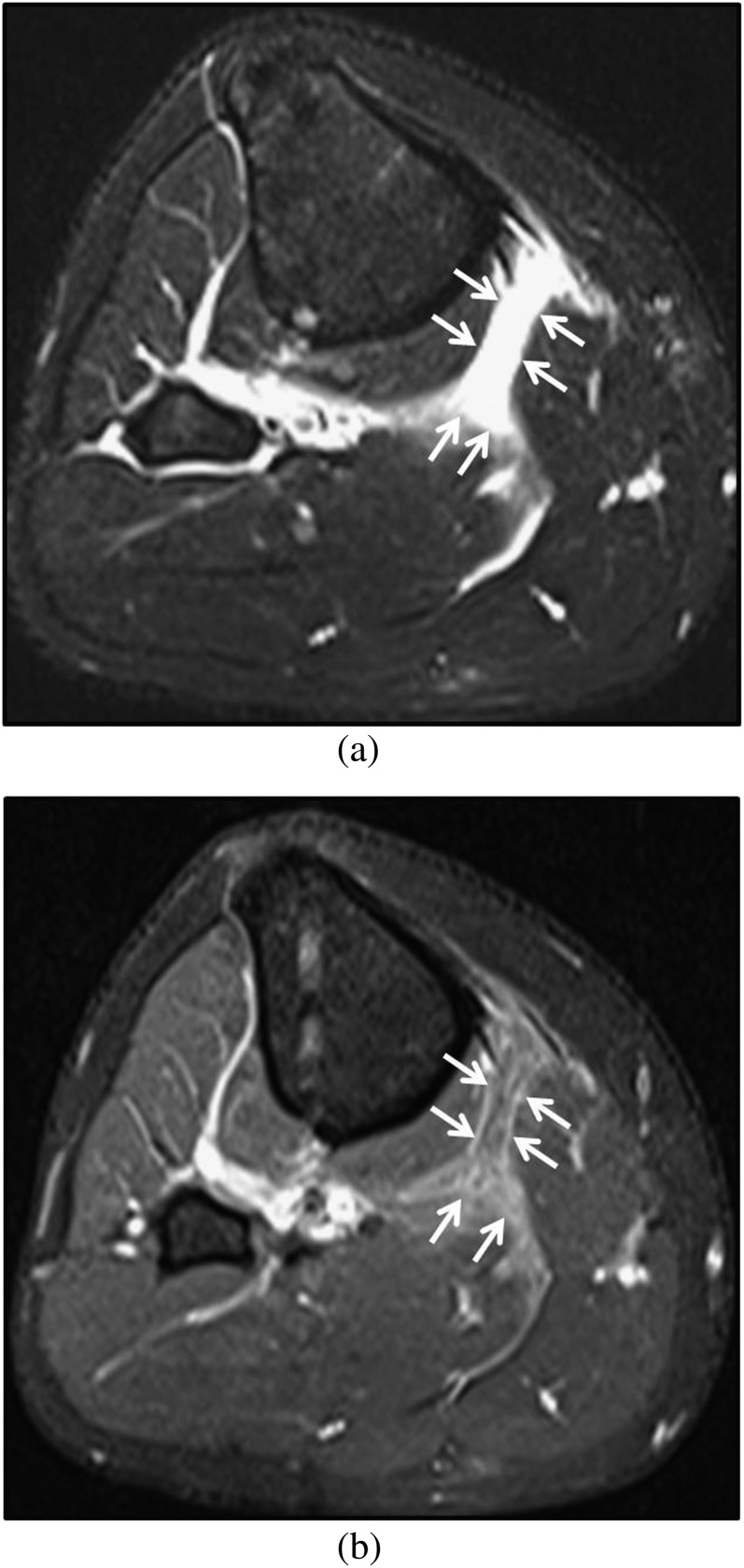
Figure 9.
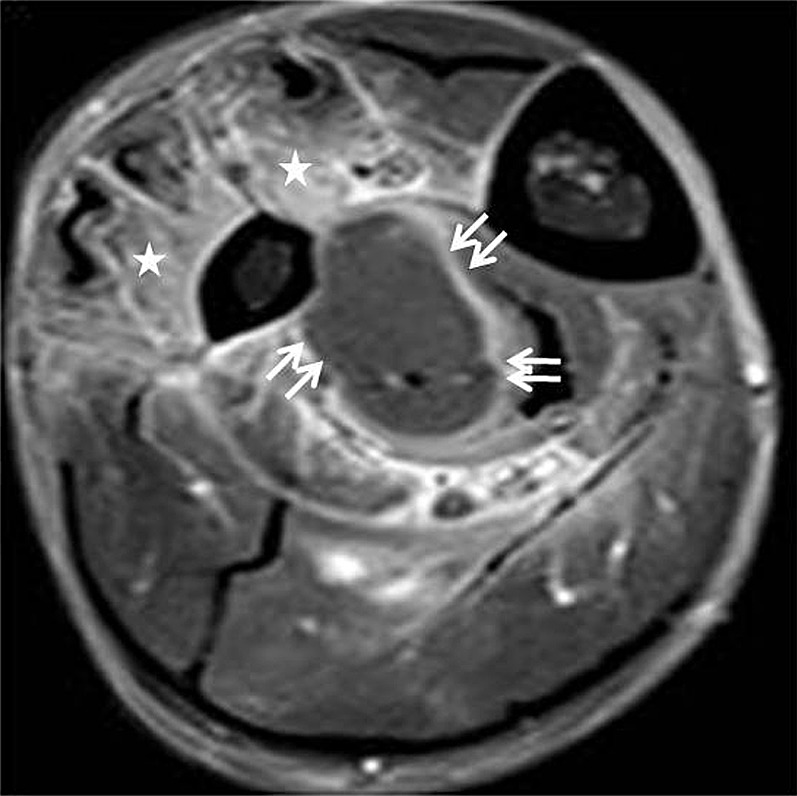
Pyomyositis in a 61-year-old diabetic male. Axial post-contrast fat-suppressed T1 weighted MR image shows a rim-enhancing collection compatible with abscess formation (white arrows) in the deep posterior muscle compartment. Contrast enhancement was also noted in extensor hallucis longus as well as peroneus group of muscles (white stars), compatible with myositis. Patient was managed with drainage and antibiotics.
Figure 10.
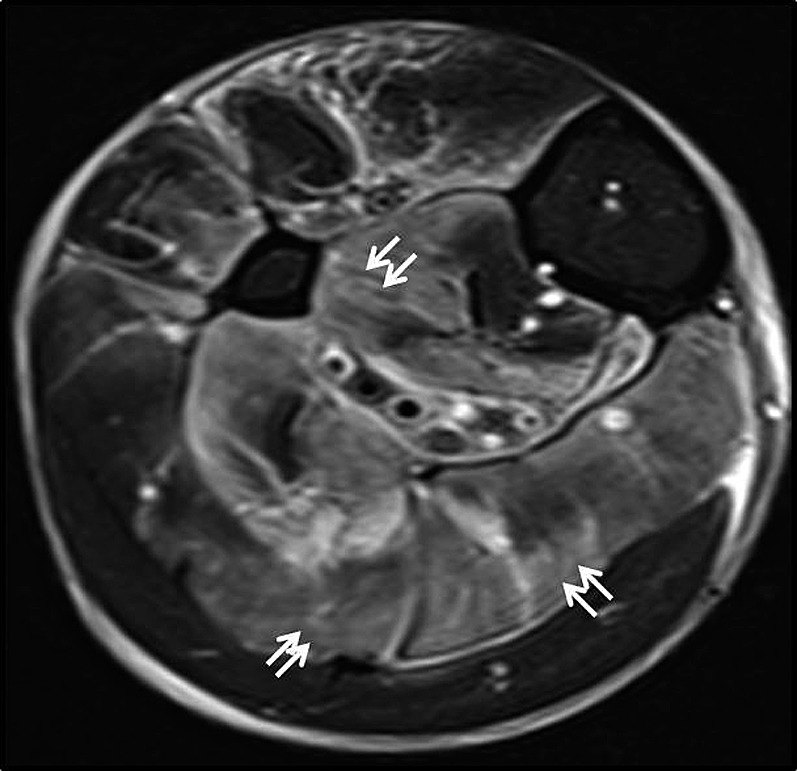
Infective myositis. Axial fat-suppressed T2 weighted MR image shows patchy areas of T2-hyperintense signal involving the soleus muscle (superficial posterior compartment) and also the deep posterior muscle compartment (white arrows). No thick (>3 mm) T2-hyperintense signal was evident in the deep intermuscular fascia. Findings were compatible with myositis. Patient was managed conservatively with antibiotics.
SUMMARY
In summary, MRI is useful in the diagnosis of suspected necrotizing fasciitis. Signal abnormality consisting of linear areas of T2 hyperintensity in the deep intermuscular fascia is an important feature for diagnosis. T1 weighted fat-suppressed Gd-DTPA contrast-enhanced fast SE sequence has an adjunctive role in the investigation for necrotizing fasciitis. Thick intermuscular fascial thickening with multiple sites of involvement are useful findings to differentiate necrotizing fasciitis from extensive cellulitis and infective myositis. Prompt identification of abnormalities suggestive of necrotizing fasciitis on MRI would be helpful to initiate appropriate management in a timely and effective manner.
REFERENCES
- 1.Kim KT, Kim YJ, Won Lee JW, Kim YJ, Park SW, Lim MK, et al. Can necrotizing infectious fasciitis be differentiated from nonnecrotizing infectious fasciitis with MR imaging? Radiology 2011; 259: 816-24. 10.1148/radiol.11101164 [DOI] [PubMed] [Google Scholar]
- 2.Malghem J, Lecouvet FE, Omoumi P, Maldague BE, Vande Berg BC. Necrotizing fasciitis: contribution and limitations of diagnostic imaging. Joint Bone Spine 2013; 80: 146-54. 10.1016/j.jbspin.2012.08.009 [DOI] [PubMed] [Google Scholar]
- 3.Brook I, Frazier EH. Clinical and microbiological features of necrotizing fasciitis. J Clin Microbiol 1995; 33: 2382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chou H, Teo HE, Dubey N, Peh WC. Tropical pyomyositis and necrotizing fasciitis. Semin Musculoskelet Radiol 2011; 15: 489-505. 10.1055/s-0031-1293495 [DOI] [PubMed] [Google Scholar]
- 5.Brothers TE, Tagge DU, Stutley JE, Conway WF, Del Schutte H Jr, Byrne TK. Magnetic resonance imaging differentiates between necrotizing and non-necrotizing fasciitis of the lower extremity. J Am Coll Surg 1998; 187: 416-21. [DOI] [PubMed] [Google Scholar]
- 6.Stecco C, Macchi V, Porzionato A, Duparc F, De Caro R. The fascia: the forgotten structure. Ital J Anat Embryol 2011; 116: 127-38 [PubMed] [Google Scholar]
- 7.Fayad LM, Carrino JA, Fishman EK. Musculoskeletal infection: role of CT in the emergency department. Radiographics 2007; 27: 1723-36. 10.1148/rg.276075033 [DOI] [PubMed] [Google Scholar]
- 8.Jaovisidha S, Leerodjanaprapa P, Chitrapazt N, Nartthanarung A, Subhadrabandhu T, Siriwongpairat P. Emergency ultrasonography in patients with clinically suspected soft tissue infection of the legs. Singapore Med J 2012; 53: 277-82. [PubMed] [Google Scholar]
- 9.Schmid MR, Kossmann T, Duewell S. Differentiation of necrotizing fasciitis and cellulitis using MR imaging. AJR Am J Roentgenol 1998; 170: 615-20. 10.2214/ajr.170.3.9490940 [DOI] [PubMed] [Google Scholar]
- 10.Seok JH, Jee WH, Chun KA, Kim JY, Jung CK, Kim YR, et al . Necrotizing fasciitis versus pyomyositis: discrimination with using MR imaging. Korean J Radiol 2009; 10: 121-8. 10.3348/kjr.2009.10.2.121 [DOI] [PMC free article] [PubMed] [Google Scholar]