Abstract
Objective:
To evaluate three-dimensional (3D) displacements of gastric remnant during adjuvant radiation.
Methods:
From January 2011 to September 2012, patients undergoing adjuvant image-guided intensity-modulated radiation on tomotherapy were included. Megavoltage CT (MVCT) data sets from daily treatment were coregistered with Day 1 MVCT. Residual stomach remnant was delineated on the data set, while the remaining were blinded to previous day contours. Gastric volume and centre of mass (COM) were determined for all data sets. The 3D deviation of COM was calculated for each fraction. Mean 3D and standard deviation (SD) were calculated for each patient and study population, and a 95% confidence interval (CI) was determined. Also, systematic and random errors for patient population and internal target volume (ITV) margin were calculated using the van Herk formula.
Results:
There were 119 images available for 15 patients. Mean volume of remnant was 319 cm3 (146–454 cm3). Gastric remnant expanded in different directions with no specific directional expansion. Average deviations in mediolateral, superoinferior and anteroposterior directions were 9 mm (3–25 mm; SD, 5 mm), 6 mm (3–16 mm; SD, 4 mm) and 5 mm (1–10 mm; SD, 3 mm), respectively, with 95% CI of 18, 15 and 11 mm, and ITV margins of 19.2, 13.5 and 7.8 mm, respectively.
Conclusion:
There is large variation in gastric remnant volume during the course of radiation. Large displacements observed in the present study necessitate the need to investigate adaptive techniques for optimizing intensity-modulated radiotherapy (IMRT) delivery.
Advances in knowledge:
An adaptive strategy needs to be developed to optimize IMRT delivery for adjuvant gastric irradiation.
Gastric cancer is a leading cause of cancer mortality, although the incidence has decreased in the past few years in both males and females.1,2 The antrum or distal stomach is the commonest site (40%), followed by the fundus, cardia, gastroesophageal (GE) junction (35%) and the body of the stomach (25%). However, the relative incidence of the distal lesions has decreased with increase in the proximal/GE junction lesions.3 Unfortunately, most of the lesions are diagnosed at an advanced stage. Of these, only 25–40% of patients are eligible for treatment with curative intent. Of those undergoing upfront curative surgery, a significant proportion present with local recurrence either alone (29%) or in the presence of systemic metastasis (88%).4
Since the results of the Southwest Oncology Group [SWOG 9008/intergroup (INT) 0116], a Phase III randomized trial, adjuvant chemoradiation in combination with systemic chemotherapy has become the standard of care for patients undergoing upfront surgical resection and for patients with features of high risk on histopathology. The updated analysis at 10 years shows a continued strong benefit from adjuvant chemoradiation in terms of overall survival (OS) as well as relapse-free survival (RFS) with hazard ratios of 1.32 (p = 0.004) and 1.51 (p < 0.001), respectively.5,6 While the benefit with adjuvant chemoradiation has been questioned within the setting of D2 dissection, a large proportion of patients continue to undergo upfront D0/1+ resection without perioperative chemotherapy.7,8 Furthermore, recent meta-analysis failed to identify a subgroup of patients that does not benefit from adjuvant radiation even after D2 dissection, and adjuvant chemoradiation is recommended for patients undergoing upfront resection.9
Although adjuvant chemoradiation is associated with survival advantage, it is at the cost of increased acute grade III/IV toxicity. INT 0116 reported 75% incidence of acute grade III/IV toxicity, of which 33% were gastrointestinal (GI) (nausea/vomiting/hepatic) with only 65% patients completing the entire chemoradiation.6 This has been attributed to the large radiation field size used during parallel opposed and conformal radiation. In recent years, multifield three-dimensional (3D) conformal radiotherapy (3DCRT) and intensity-modulated radiotherapy (IMRT) have been used.10 Although there are no randomized studies, few prospective studies10,11 have demonstrated the superiority of IMRT over 3DCRT. Conformal and IMRT techniques reduce bowel, liver and kidney doses, and clinical results have demonstrated reduction in acute grade III/IV GI and haematological toxicity to 26–57% and 16% with 3DCRT and IMRT, respectively.12,13 A large randomized study from China comparing adjuvant chemotherapy and IMRT with chemotherapy alone after D2 gastrectomy reported on toxicity profile of 350 patients with gastric cancers. Although the use of IMRT improved OS and RFS by 10 and 14 months, respectively, the grade III/IV toxicity was no different than the chemotherapy alone arm (6% GI and 7.5% haematological in IMRT-chemotherapy arm vs 7.3% haematological and no grade III/IV GI toxicity in chemotherapy alone arm).14 Given the favourable toxicity profile, IMRT may find increased use within the community; however, as residual gastric remnant is a distensible organ, the chances of inaccurate treatment delivery remains high. A quality assured IMRT technique is hence required. However, although toxicity and control with IMRT have been reported in studies, there are little published data on technical aspects of delivering quality assured IMRT. A major challenge in high precision IMRT delivery is the geometric uncertainty owing to internal organ motion of gastric remnant from respiration and gastric distension as seen in various studies.15 Also, the gastric volume is variable because of the uncertainty in gastric filling, especially in postoperative setting. The present study was initiated to characterize interfraction gastric remnant distension/displacement in patients undergoing image-guided (IG)-IMRT with an aim to determine internal target volume (ITV).
METHODS AND MATERIALS
From January 2011 to September 2012, patients of gastric cancer undergoing adjuvant IG-IMRT with TomoTherapy® (TomoTherapy Inc., Madison, WI) were included in the study. All patients followed a standard protocol of 8 h (overnight) fasting regimen prior to simulation and treatment. Radiotherapy planning was done in supine position with arms overhead and knee rest with intravenous contrast and interslice distance of 5 mm. Prokinetic agent (10 mg of metoclopramide 1 h before treatment) was prescribed to patients, wherein food residue was observed even after fasting on the planning CT scan. Planning was done on TomoTherapy Hi-Art® treatment Planning System (TomoTherapy Inc.). All patients were treated using daily megavoltage CT (MVCT) imaging prior to treatment. Daily MVCT images were obtained with the normal setting (4-mm slices) to include the entire planning target volume (PTV) with a 4–5 cm cranial margin. Inferiorly, the scan was obtained up to the lower pole of the kidneys. Treatment was performed after the approval of a radiation oncologist on the adequacy of match with the planning CT.
For the purpose of the present study, the unregistered MVCT data sets from alternate fractions were transferred to FocalSim workstation v. 4.3.3, and the first day MVCT formed the baseline scan for evaluation of interfraction distension/displacement. All subsequent MVCT images were coregistered with Day 1 MVCT using bony vertebral fusion. Residual stomach remnant was delineated on each of the data sets from the gastroesophageal junction to include the whole of the gastric remnant on the MVCT images, while the remaining were blinded to previous contours. Duodenal stump, lymph node stations and anastamotic site were not included. Gastric volume and centre of mass (COM) were determined for all data sets by the planning software. 3D deviation of COM from baseline was calculated for each fraction to obtain shifts in x [mediolateral (ML)], y [superoinferior (SI)] and z [anteroposterior (AP)] directions for each patient. Mean 3D displacement and standard deviation (SD) were calculated for each patient and the study population, and 95% confidence interval (CI) was determined. The systematic and random errors were calculated as the SD of means and root mean square of the SD for all three directions. The formula of van Herk16,17 was applied to obtain the CTV (clinical target volume) to ITV margins.
RESULTS
A total of 15 patients were treated with adjuvant chemoradiation on helical TomoTherapy from January 2011 to September 2012. The pylorus was the most common site, and most of the patients had undergone a distal gastrectomy. The patient characteristics and baseline surgicopathological details are given in Table 1.
Table 1.
Patient characteristics and surgicopathological details (n = 15)
| Characteristics | n (%) |
|---|---|
| Sex | |
| Males | 11 (73) |
| Females | 4 (27) |
| Site | |
| Antrum | 4 (27) |
| Pylorus | 6 (40) |
| Others | 5 (33) |
| Type of surgery | |
| Distal gastrectomy (subtotal) | 9 (60) |
| Others | 6 (40) |
| Histology | |
| Adenocarcinoma | 10 (67) |
| Signet ring cell carcinoma | 5 (33) |
| T stage | |
| T2b | 4 (27) |
| T3 | 5 (33) |
| T4 | 6 (40) |
| Node | |
| Positive | 10 (67) |
| Negative | 5 (33) |
| Margin positive | 2 (proximal margin) |
Only one patient required prokinetic agent prior to radiotherapy owing to residual food on planning CT scan. The average volume of gastric remnant was 319 cm3 (146–454 cm3). Figure 1 shows the gastric remnant contours for different fractions fused over Day 1 image on MVCT. Figure 2 shows the gastric remnant going out of the contoured gastric remnant during treatment. As a result of gastric remnant volumetric changes, the ML, SI and AP displacements were in the range of 3–25, 3–16 and 1–10 mm, respectively. The mean shifts for the ML (x) direction were <5 mm for almost half of the patients (8/15). For the SI (y) direction, most of the patients had shifts between 5 and 10 mm (8/15); however, they were <5 mm for the majority (9/15) in the AP (z) direction. The maximum motion was in the ML (x) direction, being 25 mm. Also, there was no specific pattern of shifts in either direction for the three dimensions. The mean volume for all the patients and mean shifts in ML (x), SI (y) and AP (z) directions are listed below in Table 2.
Figure 1.
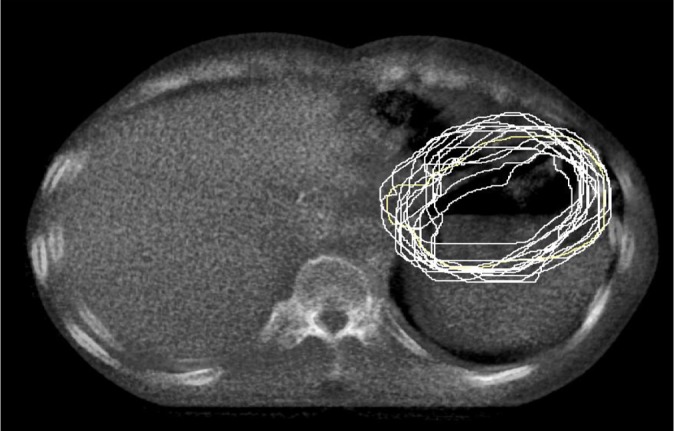
Picture showing gastric remnant contours during course of image-guided intensity-modulated radiotherapy. Megavoltage CT from various fractions is overlaid on Day 1.
Figure 2.
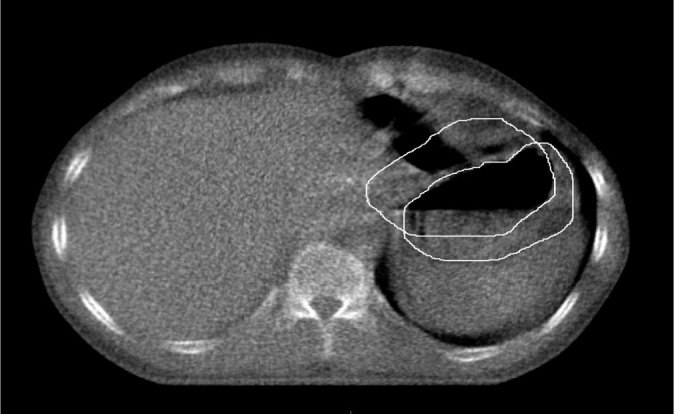
Picture showing the gastric remnant going out of the contoured gastric remnant during daily treatment as seen on megavoltage CT matched with the planning scan.
Table 2.
Mean volume and three-dimensional mean shifts for the gastric remnant for the study population (n = 15)
| Patient ID | Mean volume (cm3) | Mean x shift (mm) | Mean y shift (mm) | Mean z shift (mm) |
|---|---|---|---|---|
| Patient 1 | 438 | 9 | 6 | 4 |
| Patient 2 | 465 | 3 | 3 | 7 |
| Patient 3 | 299 | 5 | 6 | 7 |
| Patient 4 | 280 | 10 | 16 | 6 |
| Patient 6 | 266 | 4 | 5 | 10 |
| Patient 7 | 146 | 25 | 7 | 3 |
| Patient 8 | 255 | 11 | 6 | 5 |
| Patient 9 | 381 | 12 | 4 | 4 |
| Patient 10 | 203 | 8 | 6 | 5 |
| Patient 11 | 399 | 8 | 8 | 7 |
| Patient 12 | 548 | 5 | 4 | 6 |
| Patient 13 | 506 | 5 | 12 | 1 |
| Patient 14 | 514 | 4 | 6 | 2 |
| Patient 15 | 518 | 4 | 9 | 4 |
| Mean displacement | 8 | 7 | 5 | |
| SD | 6 | 4 | 2 | |
ID, identification; SD, standard deviation; x, mediolateral; y, superoinferior; z, anteroposterior.
The SD and mean ± 2SD (95% CI) for all patients in three directions are provided in Table 3. The population systematic and random errors and 3D ITV margins for gastric remnant are detailed in Table 4. The population 3D ITV margins according to van Herk were 19.2, 13.5 and 7.8 mm in the x, y and z directions, respectively. The ITV generated using mean ± 2SD provided 3D ITV margins greater than those obtained using van Herk's formula, and those being 20, 15 and 9 mm, respectively, in the x, y and z directions.
Table 3.
Standard deviation (SD) and mean + 2SD in three directions for the study population
| Patient ID | SD (x) | SD (y) | SD (z) | Mean + 2SD (x) | Mean + 2SD (y) | Mean + 2SD (z) |
|---|---|---|---|---|---|---|
| Patient 1 | 5 | 5 | 2 | 28 | 26 | 22 |
| Patient 2 | 3 | 3 | 4 | 9 | 8 | 16 |
| Patient 3 | 3 | 6 | 4 | 9 | 17 | 15 |
| Patient 4 | 5 | 6 | 4 | 18 | 28 | 15 |
| Patient 5 | 2 | 4 | 1 | 8 | 10 | 3 |
| Patient 6 | 3 | 3 | 5 | 9 | 11 | 18 |
| Patient 7 | 16 | 3 | 2 | 57 | 12 | 17 |
| Patient 8 | 5 | 4 | 3 | 21 | 13 | 10 |
| Patient 9 | 6 | 3 | 8 | 24 | 9 | 10 |
| Patient 10 | 9 | 3 | 3 | 26 | 12 | 12 |
| Patient 11 | 5 | 6 | 5 | 18 | 20 | 17 |
| Patient 12 | 6 | 2 | 3 | 17 | 8 | 12 |
| Patient 13 | 2 | 6 | 3 | 09 | 24 | 7 |
| Patient 14 | 4 | 2 | 1 | 12 | 10 | 4 |
| Patient 15 | 3 | 5 | 4 | 10 | 19 | 12 |
ID, identification; x, mediolateral; y, superoinferior; z, anteroposterior.
Table 4.
The population set-up errors and clinical target volume (CTV) to internal target volume (ITV) margins for three directions
| Displacement | Systematic error (mm) | Random error (mm) | CTV to ITV margin (van Herk) | Mean + 2SD |
|---|---|---|---|---|
| Mediolateral | 6 | 6 | 19.2 | 20 |
| Superoinferior | 4 | 5 | 13.5 | 15 |
| Anteroposterior | 2 | 4 | 7.8 | 9 |
SD, standard deviation.
DISCUSSION
The primary advantage of using IMRT for adjuvant gastric irradiation is the reduction in the acute grade III/IV GI and haematological toxicities such that patients could complete the entire treatment with minimal breaks. Also, it gives good target coverage compared with 3DCRT and conventional techniques.10,12,13,18 There are a number of dosimetric studies and a few clinical studies to support this.14
However, IMRT needs to be planned and executed judiciously as the interfraction movement of stomach/gastric remnant due to respiration and the uncertainty in gastric filling may lead to errors in treatment delivery.19 To account for internal organ motion and set-up errors, an isotropic margin of 10 mm is generally used for PTV expansion.14 From the data generated by the present study, margins required to accommodate 95% of displacements are 19.2, 13.5 and 7.8 mm in ML, SI and AP directions, respectively.16 These margins are more than the total PTV margin of 10 mm used by most of the investigators.
There are only few studies that have evaluated margins to be generated for ITV/PTV, taking into consideration the intrafraction and interfraction motion of the stomach. Mean intrafraction shifts of 9.9, 22.7 and 13.7 mm in the ML (x), SI (y) and AP (z) directions were observed, interfraction shifts being 5, 9.1, 1.3 mm in the three directions. The margins generated using van Herk formula16 were 41, 30 and 50.8 mm, respectively. Wysocka et al20 studied gastric motion in 22 resected gastric cancer patients, using planning CT scan and serial study CT scans at Weeks 1, 3 and 5 of radiotherapy and finding a median interfraction displacement of 6 mm in craniocaudal and of 2 mm in other directions. Unlike sites where soft tissue match can be performed prior to treatment execution (e.g. prostate or pancreas), soft tissue match to account for gastric distension is unlikely because the target volumes encompass both primary and nodal regions. Hence, matching gastric remnant on a daily basis can risk underdosage of nodal basins. While one could consider increased ITV margins for including all displacements, this would increase organ-at-risk doses for vast majority of patients. Although few patients within our study had unacceptable displacement, a significant proportion also had displacements that were <8 mm. Hence, a population-based approach with generous margins may be less than ideal for executing IMRT.
Another feasible option could be to generate multiple executable plans with different ITV margins (e.g. 5, 10 and 15 mm) and treating patients with the most appropriate one according to the volume of gastric remnant of that day, as done for bladder cancer and shown in a study from our institute.21 This could possibly help in reducing normal tissue toxicity as well. While our study provided us with important information regarding gastric distension and its implications on executing IMRT, there are certain drawbacks.
The large shifts reported in our study could possibly be attributed to poor soft-tissue contrast on MVCT scans as compared with the planning scans, especially at the anastamosis site leading to over- and undercontouring. Also, because of the small patient number we would not recommend increasing the ITV margins based on this study, but it is worthy to note that the shifts in all three directions are way beyond the margin given presently for these tumours.
We did not use 4D (four-dimensional) CT for our treatment planning, hence the intrafraction displacements cannot be accounted. There are only few studies on the organ motion due to respiration for treatment of gastric cancers. A study on intrafraction gastric motion found shifts in excess of 1 cm.15 4DCT has been used to generate ITV and account for motion of stomach due to respiration, although for gastric lymphomas (intact stomach). In a prospective dosimetric study, two plans were generated—Plan 1 using 4DCT and PTV margins of 8 mm over ITV and Plan 2 with 2 cm margins over CTV. Margins generated with 4DCT were adequate and also reduced the dose to normal structure, including liver, heart and kidneys, although there was no significant difference in the dose coverage of the CTV between the two plans.22 The results suggest that using a 4DCT-based approach can help to generate individualized plans with high therapeutic ratio; however, 4DCT alone is unlikely to encompass all ranges of gastric distention (i.e. displacement related to food residue or gaseous distension). Probably 4DCT with empty and full stomach scans may help describe the complete range of potential displacement.
CONCLUSION
Clinically unacceptable displacements of the gastric remnant in a significant proportion of patients undergoing IMRT risks target volume underdosage in patients undergoing treatment with the current PTV margins. Increasing the PTV margins for the entire population risks increased dose to the organs at risk. An adaptive strategy needs to be developed to optimize IMRT delivery for patients undergoing adjuvant gastric irradiation.
REFERENCES
- 1.Jemal A, Thomas A, Murray T, Thun M. Cancer statistics, 2002. CA Cancer J Clin 2002; 52: 23-47. [DOI] [PubMed] [Google Scholar]
- 2.Parkin DM, Pisani P, Ferlay J. Global cancer statistics. CA Cancer J Clin 1999; 49: 33-64, 1. [DOI] [PubMed] [Google Scholar]
- 3.Blot WJ, Devesa SS, Kneller RW, Fraumeni JF Jr. Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA 1991; 265: 1287-9. [PubMed] [Google Scholar]
- 4.Gunderson LL, Sosin H. Adenocarcinoma of the stomach: areas of failure in a re-operation series (second or symptomatic look) clinicopathologic correlation and implications for adjuvant therapy. Int J Radiat Oncol Biol Phys 1982; 8: 1-11. [DOI] [PubMed] [Google Scholar]
- 5.Smalley SR, Benedetti JK, Haller DG, Hundahl SA, Estes NC, Ajani JA, et al . Updated analysis of SWOG-directed intergroup study 0116: a phase III trial of adjuvant radiochemotherapy versus observation after curative gastric cancer resection. J Clin Oncol 2012; 30: 2327-33. 10.1200/JCO.2011.36.7136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Macdonald JS, Smalley SR, Benedetti J, Hundahl SA, Estes NC, Stemmermann GN, et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med 2001; 345: 725-30. 10.1056/NEJMoa010187 [DOI] [PubMed] [Google Scholar]
- 7.Bonenkamp JJ, Songun I, Hermans J, Sasako M, Welvaart K, Plukker JT, et al. Randomised comparison of morbidity after D1 and D2 dissection for gastric cancer in 996 Dutch patients. Lancet 1995; 345: 745-8. [DOI] [PubMed] [Google Scholar]
- 8.de Aretxabala X, Konishi K, Yonemura Y, Ueno K, Yagi M, Noguchi M, et al. Node dissection in gastric cancer. Br J Surg 1987; 74: 770-3. [DOI] [PubMed] [Google Scholar]
- 9.Ohri N, Garg MK, Aparo S, Kaubisch A, Tome W, Kennedy TJ, et al. Who benefits from adjuvant radiation therapy for gastric cancer? A meta-analysis. Int J Radiat Oncol Biol Phys 2013; 86: 330-5. 10.1016/j.ijrobp.2013.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Minn AY, Hsu A, La T, Kunz P, Fisher GA, Ford JM, et al. Comparison of intensity-modulated radiotherapy and 3-dimensional conformal radiotherapy as adjuvant therapy for gastric cancer. Cancer 2010; 116: 3943-52. [DOI] [PubMed] [Google Scholar]
- 11.Milano MT, Jani AB, Farrey KJ, Rash C, Heimann R, Chmura SJ. Intensity-modulated radiation therapy (IMRT) in the treatment of anal cancer: toxicity and clinical outcome. Int J Radiat Oncol Biol Phys 2005; 63: 354-61. 10.1016/j.ijrobp.2005.02.030 [DOI] [PubMed] [Google Scholar]
- 12.Kassam Z, Lockwood G, O'brien C, Brierley J, Swallow C, Oza A, et al. Conformal radiotherapy in the adjuvant treatment of gastric cancer: review of 82 cases. Int J Radiat Oncol Biol Phys 2006; 65: 713-19. 10.1016/j.ijrobp.2006.01.001 [DOI] [PubMed] [Google Scholar]
- 13.Milano MT, Garofalo MC, Chmura SJ, Farrey K, Rash C, Heimann R, et al . Intensity-modulated radiation therapy in the treatment of gastric cancer: early clinical outcome and dosimetric comparison with conventional techniques. Br J Radiol 2006; 79: 497-503. 10.1259/bjr/43441736 [DOI] [PubMed] [Google Scholar]
- 14.Zhu WG, Xua DF, Pu J, Zong CD, Li T, Tao GZ, et al. A randomized, controlled, multicenter study comparing intensity-modulated radiotherapy plus concurrent chemotherapy with chemotherapy alone in gastric cancer patients with D2 resection. Radiother Oncol 2012; 104: 361-6. 10.1016/j.radonc.2012.08.024 [DOI] [PubMed] [Google Scholar]
- 15.Watanabe M, Isobe K, Takisima H, Uno T, Ueno N, Kawakami H, et al . Intrafractional gastric motion and interfractional stomach deformity during radiation therapy. Radiother Oncol 2008; 87: 425-31. [DOI] [PubMed] [Google Scholar]
- 16.van Herk M. Errors and margins in radiotherapy. Semin Radiat Oncol 2004; 14: 52-64. [DOI] [PubMed] [Google Scholar]
- 17.van Herk M, Remeijer P, Rasch C, Lebesque JV. The probability of correct target dosage: dose-population histograms for deriving treatment margins in radiotherapy. Int J Radiat Oncol Biol Phys 2000; 47: 1121-35. [DOI] [PubMed] [Google Scholar]
- 18.Leong T, Willis D, Joon DL, Condron S, Hui A, Ngan SY. 3D conformal radiotherapy for gastric cancer–results of a comparative planning study. Radiother Oncol 2005; 74: 301-6. [DOI] [PubMed] [Google Scholar]
- 19.Bussels B, Goethals L, Feron M, Bielen D, Dymarkowski S, Suetens P, et al. Respiration-induced movement of the upper abdominal organs: a pitfall for the three-dimensional conformal radiation treatment of pancreatic cancer. Radiother Oncol 2003; 68: 69-74. [DOI] [PubMed] [Google Scholar]
- 20.Wysocka B, Kassam Z, Lockwood G, Brierley J, Dawson LA, Buckley CA, et al. Interfraction and respiratory organ motion during conformal radiotherapy in gastric cancer. Int J Radiat Oncol Biol Phys 2010; 77: 53-9. [DOI] [PubMed] [Google Scholar]
- 21.Murthy V, Master Z, Adurkar P, Mallick I, Mahantshetty U, Bakshi G, et al. ‘Plan of the day’ adaptive radiotherapy for bladder cancer using helical tomotherapy. Radiother Oncol 2011; 99: 55-60. 10.1016/j.radonc.2011.01.027 [DOI] [PubMed] [Google Scholar]
- 22.Matoba M, Oota K, Toyoda I, Kitadate M, Watanabe N, Tonami H. Usefulness of 4D-CT for radiation treatment planning of gastric MZBCL/MALT. J Radiat Res 2012; 53: 333-7. [DOI] [PubMed] [Google Scholar]


