Abstract
Study Objectives:
The prevalence of obstructive sleep apnea (OSA) in persons with multiple sclerosis (MS) remains unknown, and little information exists regarding the relative contributions of OSA to symptoms of MS-related fatigue in the presence of other clinical and sleep-related confounders. The objectives of this study were to investigate the prevalence of diagnosed OSA and OSA risk among MS patients, and to assess relationships between fatigue severity, OSA, OSA risk, and sleep quality among persons with MS.
Methods:
N = 195 MS patients completed a questionnaire comprised of items regarding OSA diagnosis, sleep quality and quantity, daytime symptoms, and 4 validated scales: the Epworth Sleepiness Scale, Fatigue Severity Scale, Insomnia Severity Index, and STOP-Bang questionnaire. Medical records were also accessed to examine clinical characteristics that may predict fatigue or OSA risk.
Results:
N = 41 patients (21%) carried a formal diagnosis of OSA. N = 110 (56%) of all patients, and 38 (93%) of those with diagnosed OSA had STOP-Bang scores ≥ 3, indicating an elevated OSA risk. In regression models, the most significant predictors of higher FSS scores were higher STOP-Bang scores (p = 0.01), higher number of nocturnal symptoms (p < 0.0001), and higher disability level (p < 0.0001).
Conclusions:
Sleep disturbances, and OSA in particular, may be highly prevalent yet underrecognized contributors to fatigue in persons with MS.
Citation:
Braley TJ; Segal BM; Chervin RD. Obstructive sleep apnea and fatigue in patients with multiple sclerosis. J Clin Sleep Med 2014;10(2):155-162.
Keywords: obstructive sleep apnea, multiple sclerosis, fatigue, STOP-Bang, sleep disturbance
Multiple sclerosis (MS) is an autoimmune disease of the central nervous system that causes myelin destruction and axonal damage in the brain and spinal cord. Multiple sclerosis is the leading cause of non-traumatic neurological disability among young adults, and is associated with a variety of debilitating symptoms, including fatigue.
Fatigue affects up to 90% of multiple sclerosis patients at some point during their disease course.1–4 This highly debilitating symptom imposes significant socioeconomic consequences5 and is a leading cause of diminished quality of life among individuals with MS.3 Although MS-related fatigue is often multifactorial, identification of treatable causes that may contribute to its severity is an essential element of management of this symptom.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Fatigue is one of the most common and debilitating symptoms experienced by persons with multiple sclerosis (MS), but little is known about the potential contributions of obstructive sleep apnea (OSA) or its frequency in patients with MS. The objectives of this study were to investigate the frequency of diagnosed OSA and elevated OSA risk among MS patients in a tertiary care center, and to assess relationships between fatigue severity, OSA, OSA risk, and sleep quality among MS patients.
Study Impact: Our findings suggest that OSA is highly prevalent in patients with MS, particularly among fatigued MS patients. Although a cross-sectional study cannot demonstrate that OSA or other sleep disturbances cause the fatigue that accompanies MS, the associations identified in this study indicate that if cause-and-effect relationships do exist, OSA and disturbed sleep could contribute substantially to fatigue that ranks among the leading complaints of patients with MS.
Obstructive sleep apnea (OSA) may exacerbate fatigue severity in MS. This treatable disorder of sleep and breathing is a known cause of fatigue and related symptoms in general population studies,6 and constitutes a significant risk factor for cardiovascular disease, metabolic syndrome, motor vehicle accidents, reduced productivity, cognitive dysfunction, and poor quality of life.7–14 Yet, despite its impact in the general population, the extent to which OSA contributes to fatigue in persons with MS is poorly understood, and the prevalence of OSA in MS remains unclear. Whereas some contend that the prevalence of OSA is higher in MS patients than in the general population, heterogeneity in subjects studied, sample sizes, and outcome measures have led to highly variable estimates.15–20 Furthermore, no standardized approach has been developed to identify clinical features that may signal OSA risk in individuals with MS. Research on distinguishing features of OSA versus other sleep related predictors of fatigue in MS could help clinicians identify patients most likely to benefit from sleep evaluations, and optimize fatigue management. The purpose of this study was to assess the frequency of diagnosed OSA and elevated OSA risk among MS patients in a tertiary MS center, and to assess relationships between fatigue severity, OSA, OSA risk, and sleep quality among persons with MS in the outpatient setting.
METHODS
Standard Protocol Approvals, Registrations, and Patient Consents
This survey study was approved by the University of Michigan (U-M) Institutional Review Board (IRBMED).
Subjects/Data Collection
All patients age 18 or older with a documented diagnosis of MS who did not have a concomitant neurological disorder that could increase OSA risk (such as stroke, Parkinson disease, or amyotrophic lateral sclerosis) were invited to participate.
Between July 2012 and March 2013, during routine clinic appointments, n = 203 consenting subjects who presented to the U-M Multiple Sclerosis Clinic for follow-up completed a self-administered survey comprised of questions regarding perceived sleep quality, sleep quantity, use of hypnotics and wake promoting agents, daytime symptoms, use of positive airway pressure devices (if applicable), and items adapted from the International Restless Legs Syndrome (RLS) Study Group essential diagnostic criteria.21 Survey items were structured as yes/no questions and categorical responses, in which subjects were asked to circle their one best answer from list of options. Data on nocturnal symptoms that interfere with sleep were collected through multiple choice questions, wherein subjects were allowed to select one or more choices from a list of symptoms including pain, tingling, spasticity, feelings of restlessness, urinary urgency, anxiety, an inability to shut off the mind, muscle twitching, or “other” (which allowed subjects to write in their own response).
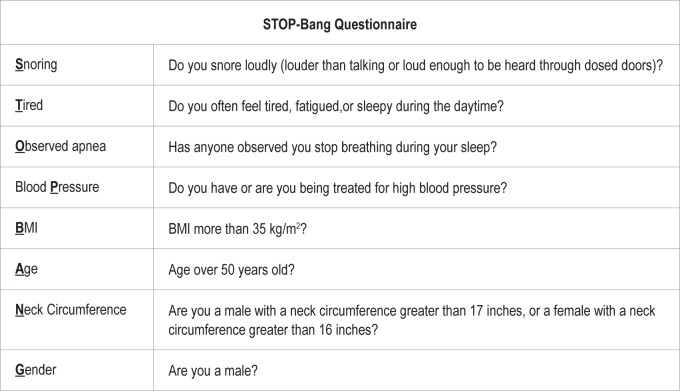
The survey also included 4 validated instruments: the Epworth Sleepiness Scale; the Fatigue Severity Scale; the STOP-Bang questionnaire; and, for subjects who endorsed difficulty sleeping on a separate survey item, the Insomnia Severity Index. The Epworth Sleepiness Scale (ESS) is an 8-item questionnaire that uses 4-point Likert scale items to quantify the likelihood of dozing in sedentary situations.22 Scores ≥ 10 are consistent with excessive daytime sleepiness. The Fatigue Severity Scale (FSS) is a 9-item questionnaire that uses a 7-point Likert scale to assess the impact of fatigue in persons with MS and other chronic diseases. Average FSS scores ≥ 4 are suggestive of fatigue.23 The STOP-Bang questionnaire is a screening tool consisting of 8 questions and measures that form the acronym STOP-Bang (Figure 1). Scores are based on yes/no answers for each item (score: 1/0). STOP-Bang scores ≥ 3 indicate elevated risk for OSA.24,25 The Insomnia Severity Index (ISI) is a 7-item questionnaire with 5-point Likert scale responses designed to assess the nature, severity, and impact of insomnia in adults. Scores ≥ 15 reflect moderate clinical insomnia.26
Figure 1. Items comprising the STOP-Bang questionnaire (adapted from Chung et al.24 and Chung et al.25 with permission from Dr. Francis Chung).
Surveys were administered by qualified study staff (VK, KD, or JR—see Acknowledgments), blinded to subjects' clinical history. Patients completed their surveys in MS clinic examination rooms prior to seeing their MS specialists. Patients had opportunities to discuss questionnaire responses and symptoms with their physicians. In the event that research staff were not available, surveys were administered by the treating MS physician. Medical records were reviewed by the principal investigator (TB) to confirm eligibility and extract additional data on clinical variables that may influence sleep quality or fatigue level. Clinical variables recorded included age, gender, MS subtype (relapsing or progressive), MS disease duration at time of the survey (years), use of disease modifying or immunosuppressive therapy at the time of the survey (yes/no), documented diagnosis of clinical depression or active symptoms of depression as documented by the treating physician during the subject's clinical assessment on the day of the survey (yes/ no), and a dichotomized estimate of disability [defined as Expanded Disability Status Scale score < 6 (lower disability), or ≥ 6 (higher disability)]. Based on a standard neurological examination, the Expanded Disability Status Scale (EDSS) is a composite score that is commonly used to quantify disability level in patients with MS.27 The composite is derived from ratings of 7 functional systems commonly affected in MS: visual, brainstem, pyramidal, cerebellar, sensory, bowel/ bladder, and cerebral function. Scores < 6.0 indicate independent ambulation without the need for an assistive device such as a cane, walker, or wheelchair.
Statistical Methods
Statistical tests were performed using SAS version 9.2. Tests were two-sided with a level of statistical significance set at 0.05.
Bivariate relationships between Epworth scores, FSS scores, STOP-Bang scores, Insomnia Severity Index scores, perceived sleep latency and duration, nocturnal symptoms, and MS-specific characteristics were examined with Spearman correlation tests. Two-sample t-tests, Wilcoxon rank-sum tests, and χ2 tests were used to examine differences in clinical variables and survey responses by OSA risk score (STOP-Bang score ≥ 3 vs. < 3) and OSA diagnosis. For OSA patients with information regarding treatment with continuous or bilevel positive airway pressure (PAP), 2-sample t-tests and Wilcoxon rank-sum tests were performed to compare Epworth and FSS scores, respectively, between compliant PAP users and non-compliant users/non-users.
Multiple linear regression models were constructed to assess sleep-related predictors of FSS scores, taking into account age, gender, BMI, disability status (dichotomized EDSS score), disease modifying therapy use, depression, and presence of restless legs syndrome as potential confounders. To reduce potential effects of multicollinearity between FSS scores and STOP-Bang scores (which includes an item for tiredness), additional regression analyses were conducted with STOP-Bang questionnaires scored with the tiredness item removed.
The population attributable risk percent (PAR%) was calculated to estimate the potential impact of OSA on fatigue in MS. Calculation of a PAR% is based on 2 assumptions: first, that OSA diagnosis or high risk for OSA as reflected by the STOP-Bang (with underlying OSA in many cases) can cause fatigue in MS, and second, that the prevalences of these 2 risk factors in MS are similar to those observed in the current study. The PAR% then uses the excess frequency of the risk factor among fatigued vs. non-fatigued MS patients to estimate the proportion of fatigue (defined here as FSS score ≥ 4) among MS patients that would be eliminated by diagnosis and successful treatment of the underlying OSA or elevated OSA risk.28 For this cross-sectional study, the formula used was:
where Attributable Risk % was derived from odds ratio estimates rather than relative risk and the Prevalence of Exposure was the frequency of OSA diagnosis or high STOP-Bang score among the fatigued subjects.
RESULTS
One hundred percent of invited subjects (203/203) agreed to participate. However, 8 surveys were excluded from the analyses for the following reasons: missing or incomplete survey data (2), diagnosis other than MS (5), and concomitant neurological disease (1).
Baseline Data
Demographic and sleep related characteristics for 195 MS patients are shown in Tables 1 and 2. Mean age was 47 years. Sixty-six percent of the participants were female, consistent with the gender distributions seen in MS in the United States. Mean disease duration was 10.2 years. Sixty-eight percent were on disease modifying therapy. Per medical records, 74% carried a diagnosis of relapsing-remitting MS, while 26% had progressive disease (primary progressive or secondary progressive MS). Forty-one patients (21%) endorsed a formal diagnosis of OSA (63% diagnosed at our center). Thirty-two patients with OSA were prescribed PAP. Of these, 17 reported compliant use (defined here as PAP use ≥ 4 h per night, most nights per week). Fifty-six (30% of 188 responders) answered “yes” to all 4 International Restless Legs Syndrome (RLS) Study Group essential screening questions, meeting clinical diagnostic criteria for RLS.
Table 1.
Demographic and clinical findings
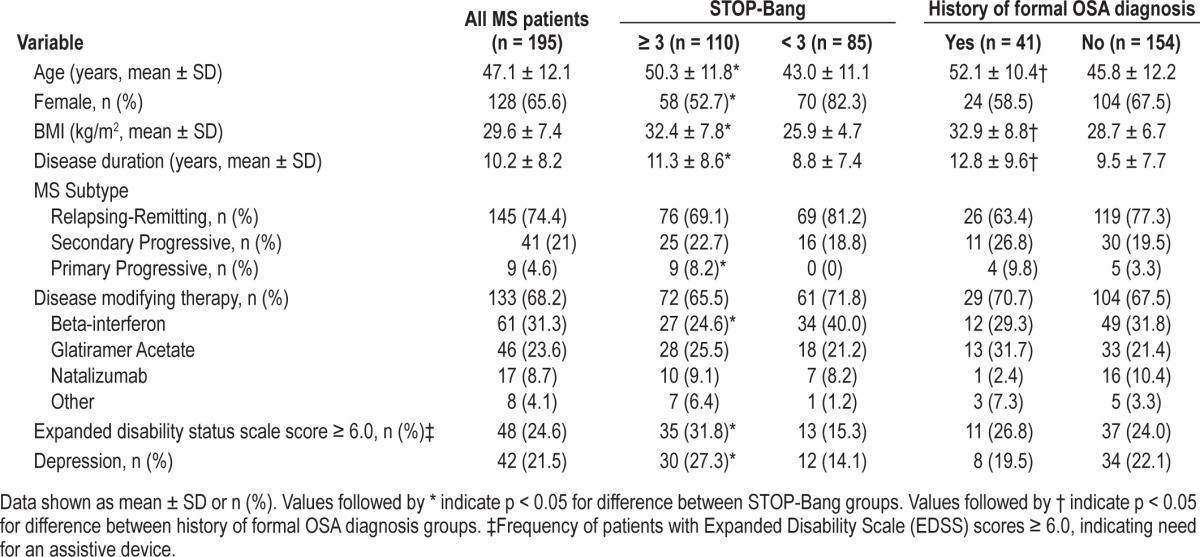
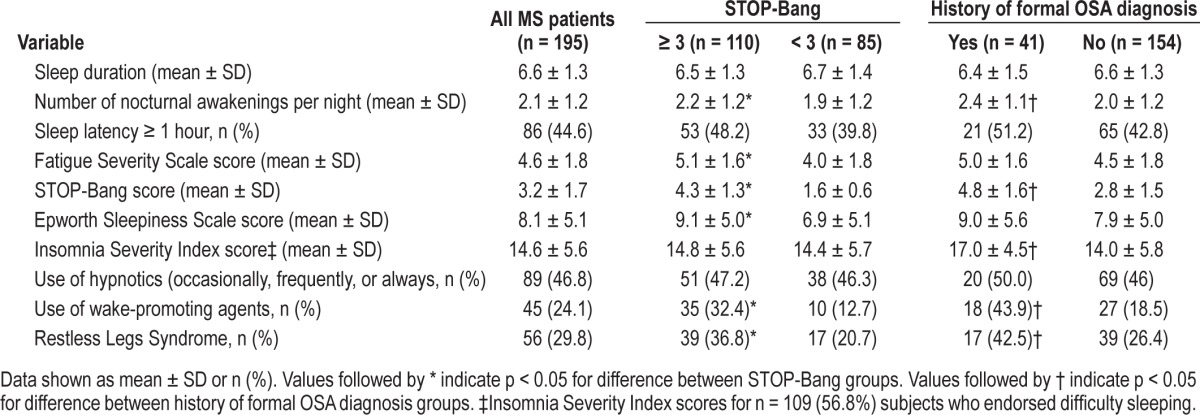
Table 2.
Sleep characteristics, nocturnal behaviors, and daytime symptoms
Eighty-five percent of patients endorsed at least one nocturnal symptom (pain, tingling, spasticity, feelings of restlessness, urinary urgency, anxiety, an inability to shut off the mind, muscle twitching, or other) to interfere with their ability to get a good night's sleep, with 54% of patients endorsing ≥ 3 of these symptoms (not shown in table). Nocturnal symptoms most frequently reported to interfere with sleep included pain, spasms, nocturia, and an inability to shut off one's mind (endorsed by 41%, 40%, 40%, and 50% of subjects, respectively).
Validated Instruments
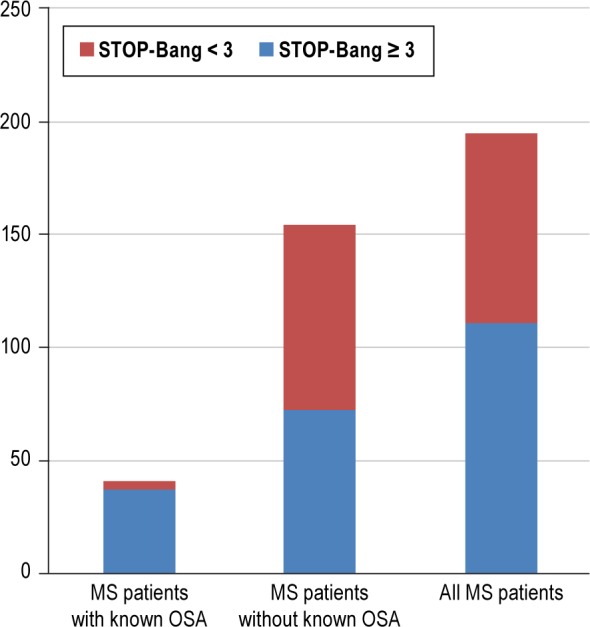
One hundred ten (56%) of all patients, and 38 (93%) of those with diagnosed OSA had STOP-Bang scores ≥ 3 (Figure 2). For all patients, the mean Fatigue Severity Scale score (FSS) and Epworth score were 4.6 (SD 1.8) and 8.1 (SD 5.1), respectively.
Figure 2. Frequency of high STOP-Bang scores among all MS patients, and those with and without a formal diagnosis of OSA.
For 109 patients who endorsed difficulty sleeping, the mean Insomnia Severity Index score was 14.6; 50 (46%) of these subjects had Insomnia Severity Index scores ≥ 15, reflecting moderate clinical insomnia. Mean FSS and Epworth scores among these subjects were 5.0 and 8.7, respectively.
Bivariate Analyses (Tables 1 and 2)
Mean FSS scores were significantly higher in patients with STOP-Bang scores ≥ 3 (5.1 vs. 4.0, p < 0.0001). There was also a trend toward higher FSS scores in patients with documented OSA compared to the remainder of the sample (5.0 vs. 4.5, p = 0.1049).
Moderately strong correlations emerged between the FSS score and the STOP-Bang score, Epworth score, and Insomnia Severity Index score (Table 3). FSS scores also correlated with mean number of perceived nocturnal awakenings and number of nocturnal symptoms. Individual nocturnal symptoms that correlated best with FSS score included pain (rho = 0.39, p < 0.0001), spasms (rho = 0.45, p < 0.0001), and twitching (rho = 0.37, p < 0.0001) (not shown in table).
Table 3.
Correlations (Spearman rho [p-value]) between fatigue and sleep-related measures
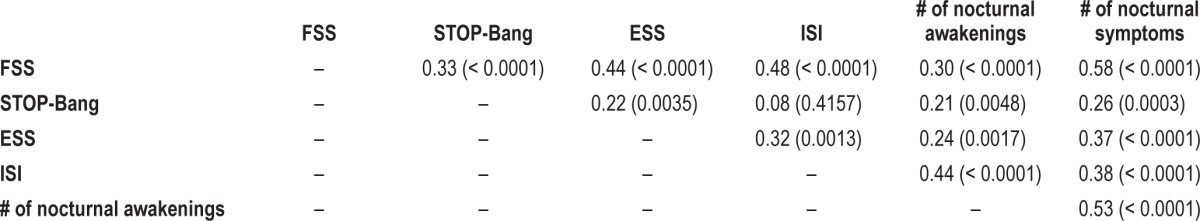
STOP-Bang scores correlated more strongly with FSS scores (rho = 0.33, p < 0.0001), than with Epworth scores (rho = 0.22, p = 0.0035). STOP-Bang scores also correlated with mean number of nocturnal awakenings and number of nocturnal symptoms.
Among patients who carried a diagnosis of OSA, compliant PAP users in comparison to the remaining patients showed no significant differences in FSS scores (p = 0.2819) or Epworth scores (p = 0.2691).
Regression Analyses
Number of nocturnal symptoms (regression parameter = 0.44, SE = 0.07, p < 0.0001), higher EDSS scores (regression parameter = 1.1, SE = 0.27, p < 0.0001), and STOP-Bang scores (regression parameter = 0.25, SE = 0.10, p = 0.01) were the strongest predictors of FSS scores, after adjustment for age, gender, BMI, sleep duration, number of nocturnal awakenings, depression, disease modifying therapy use, and presence of RLS. In separate models adjusted for the same predictor variables, the number of nocturnal symptoms also predicted ESS scores (regression parameter = 0.63, SE = 0.25, p = 0.012), but there was no significant association between the STOP-Bang and ESS scores. Diagnosis of OSA (regression parameter = 3.6, SE = 1.24, p = 0.0049) and number of nocturnal symptoms (regression parameter = 1.37, SE = 0.30, p < 0.0001) most strongly predicted the ISI after controlling for age, gender, BMI, depression, disability status, and presence of RLS.
Modified STOP-Bang Analyses (tiredness item removed)
The proportion of fatigued subjects, as compared to non-fatigued subjects, with elevated STOP-Bang scores remained significantly higher when the tiredness item was removed from the STOP-Bang questionnaire (43% vs. 28%, χ2 p = 0.0389). Twenty-nine patients (74.4%) with a confirmed OSA diagnosis had modified STOP-Bang scores ≥ 3. Correlations between FSS score and modified STOP-Bang score remained significant in Spearman correlation tests (rho = 0.22, p = 0.0028), and in regression models adjusted for depression, EDSS score, sleep duration, disease modifying therapy use, and presence of RLS (regression parameter = 0.15, SE = 0.07, p = 0.0459); but statistical significance diminished in models adjusted further for age, gender, BMI, mean number of nocturnal awakenings, and number of nocturnal symptoms (regression parameter = 0.14, SE = 0.11, p = 0.1805).
Population Attributable Risk Percent (PAR %)
The PAR% for documented OSA as a risk factor for fatigue in MS patients was 11%. The PAR% for elevated OSA risk as defined by the STOP-Bang was 40%.
DISCUSSION
In this study, one-fifth of MS patients surveyed in a large tertiary MS practice carried a formal diagnosis of OSA, and a substantially higher proportion of patients (more than half) were found to be at elevated risk for OSA based on the STOP-Bang questionnaire. Obstructive sleep apnea risk emerged as a significant predictor of fatigue, after adjustment for other important clinical and sleep related predictors of fatigue, including number of nocturnal symptoms and disability status. Although this study was cross-sectional and cannot prove cause and effect, the findings suggest that OSA is highly prevalent in patients with multiple sclerosis, particularly among fatigued MS patients, and that OSA and other causes of disturbed sleep could contribute substantially to fatigue severity.
Obstructive sleep apnea (OSA) is well recognized as a major public health challenge in the United States.29 Despite its importance, its prevalence in persons with MS remains unknown, with estimates ranging from 0% to 58% in published studies (see Table 4 for a summary of these studies).15,17–19 There are several potential reasons for the high variability among these findings and our estimates of OSA frequency. Primary outcome measures differed across studies, most of which were not designed to assess OSA prevalence. Selection bias is also a concern, particularly among studies that utilize laboratory-based research PSG, as these studies have the potential to disproportionately select the most highly motivated or severely affected individuals, thus leading to an overestimation of OSA prevalence. Conversely, subject selection methods, and in particular, enrollment restrictions based on disability status and age in the Ferini-Strambi and Kaynak studies (Table 4) may have led to an underestimation of OSA prevalence among the wider population of all MS patients. Previous studies from our center and others suggest that progressive MS subtypes and increased level of disability are risk factors for OSA in MS.16 Similarly, another risk factor is age, which correlates positively with progressive MS subtypes and disability and is an independent risk factor for OSA.30–32
Table 4.
Summary of published studies that used prospective polysomnography (PSG) in persons with MS
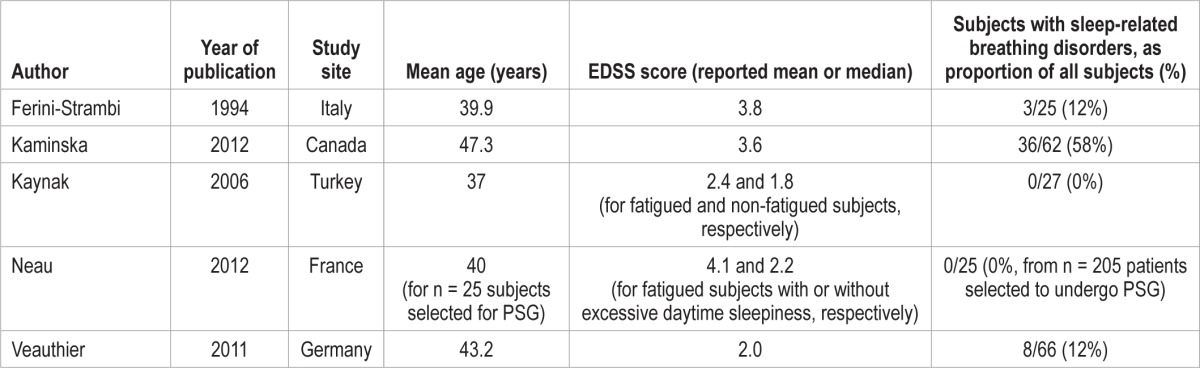
Finally, differences in PSG acquisition and scoring methods may in part explain variability in study results. Though home sleep apnea studies offer a simpler method to diagnose sleep related breathing disorders, these devices have not been validated in patients with MS, and may be insensitive to more subtle or complex sleep related breathing disorders such as upper airway resistance syndrome or central sleep apnea.
Though our estimates of OSA frequency fall within the range of previous estimates, the striking difference between the proportion of patients with an established diagnosis of OSA (21%) and those at risk for OSA based on STOP-Bang scores (56%) is also noteworthy and may reflect suboptimal OSA diagnosis patterns seen in the general population. While symptomatic OSA (defined as OSA in the setting of functional impairment due to hypersomnolence) affects at least 3% adults in the U.S., the prevalence of occult apnea when excessive daytime sleepiness is not required to establish the diagnosis may be as high as 9% for women and 24% for men.29
Under-recognition of other symptoms that may signal OSA—such as fatigue—may also explain the discrepancy we found, particularly in patients who suffer disproportionately from fatigue because of a comorbid condition (MS). Whereas MS-related fatigue is most often described as “a subjective lack of physical and/or mental energy that is perceived by the individual or caregiver to interfere with usual or desired activity,”33 many patients use this term interchangeably with sleepiness, which is classically defined as an increased propensity to fall asleep. Though diurnal sleepiness is a physiological process driven by internal and external circadian influences, excessive sleep drive may result in many of the same consequences as fatigue, including reduced cognitive and psychomotor performance, psychological distress, and reduced quality of life.34 In addition, a shared collection of popular descriptors for both terms—including tiredness, exhaustion, loss of energy, and lassitude—make separation of fatigue and sleepiness particularly challenging. Furthermore, both symptoms may be exacerbated by a number of acute and chronic medical conditions, as well as several sleep disorders.35 Despite traditional emphasis on sleepiness as a primary consequence of sleep apnea, many non-MS subjects who have OSA report that problems with fatigue, tiredness, or lack of energy supersede their problems with sleepiness.6 Moreover, recent data from our group and others suggest that MS patients with sleep problems are more likely than controls without MS to emphasize fatigue, as opposed to sleepiness.36 Our current data support these findings, and provide further evidence that OSA is a consequential yet under-recognized comorbidity in persons with MS, that may more commonly present with fatigue, rather than sleepiness.
Our data also highlight the importance of a step-wise approach in the clinical assessment of fatigued MS patients, and suggest that more effort is needed to determine the most appropriate screening tools to identify MS patients who would most benefit from formal sleep evaluations. The STOP-Bang is a sensitive, reliable screening tool for OSA, frequently used in outpatient sleep clinics and in the evaluation of surgical patients undergoing preoperative workups. Recent studies in the general population suggest that STOP-Bang scores ≥ 3 have a positive predictive value of 75% to 85% to detect OSA.24,37 Dias and authors were the first to study the utility of this instrument in the outpatient MS setting. In an anonymous survey study of MS patients, the authors reported that STOP-Bang scores positively correlated with FSS scores, particularly in males.38 They also noted that 42% of subjects were at high-risk for OSA based on STOP-Bang scores. As their survey was conducted anonymously, no data regarding disease course, disability status, other sleep disturbances, or medical history (to confirm a diagnosis of OSA) were available for the analyses. Our study now confirms some of these findings, even after accounting for other important MS-specific and sleep related variables that can influence fatigue. Although formal validation studies are still necessary to evaluate the specificity and positive predictive value of the STOP-Bang in patients with MS, our study is the first to examine the association between OSA diagnosis and high STOP-Bang scores in patients with MS, and our results provide some of the first data to suggest that the STOP-Bang as a screen for OSA retains validity in the setting of MS. If we assume that the positive predictive value of the STOP-Bang among patients without MS can be extrapolated to those with MS, this would suggest that at least 75% of our 110 subjects with elevated STOP-Bang scores (42% of our entire sample) would have OSA if formally tested with PSG—considerably more than the 41 patients (21%) who carried formal diagnoses of OSA already.
Another covariate that emerged as a strong predictor of FSS score was the number of nocturnal symptoms reported to interfere with sleep. More than half of our patients endorsed multiple nocturnal symptoms. While numerous studies have identified pain as a predictor of poor sleep quality, fatigue, and overall diminished functioning in MS patients,39,40 our findings underscore the point that nocturnal discomfort experienced by MS patients may be described in terms other than pain. More importantly, our data highlight the importance of addressing treatable symptoms that may cause fatigue in patients with MS through reduced sleep efficiency or other mechanisms.
Our study has some limitations. Despite compelling associations between sleep disturbances and fatigue, conclusions about cause-and-effect relationships cannot be drawn from these cross-sectional data. It is also possible that the high prevalence of diagnosed OSA may, in part, reflect referral characteristics of our center. Furthermore, though most (63%) of the 41 respondents who endorsed a diagnosis of OSA had been evaluated at our sleep center (allowing for PI confirmation), the remaining subjects were diagnosed at outside institutions. Some of the latter subjects may not have been formally diagnosed with OSA by clinical overnight PSG. We believe the likelihood of this is low, however, given that most of these subjects also had a diagnosis of OSA listed in their medical chart.
We also chose to focus on subjects who carried a diagnosis of OSA at the time of the survey. While this strategy did not allow assessment of survey responses prior to initiation of OSA treatment such as PAP (which could reduce fatigue or sleepiness), our approach permitted us to minimize selection bias that could obscure OSA prevalence estimates in our clinic population, and allowed a substantially larger sample size. Though no significant associations were noted between PAP use and FSS or Epworth scores, this finding should be interpreted with caution given the limited number of PAP-treated and compliant subjects. This lack of association also may reflect contributions to fatigue from other MS-related features that do not respond to treatment with PAP.
Finally, to reduce respondent burden, we relied on medical records to adjust for depression as a dichotomized variable, as opposed to use of a quantitative depression scale in our analyses. While this method may have provided a less sensitive assessment of the association between depression and fatigue, we believe that it maximized the likelihood of obtaining high quality survey responses most germane to our primary clinical questions within the limited time frame during which surveys could be administered. Also to reduce respondent burden, only subjects who endorsed difficulty sleeping on a single, initial survey question were asked to complete the Insomnia Severity Index. This approach may have limited our ability to detect and characterize all cases of insomnia.
In conclusion, our data provide new evidence that sleep disturbances, and OSA in particular, may be highly prevalent yet under-recognized contributors to fatigue in persons with MS. Clinicians caring for these patients should maintain a low threshold to screen MS patients for OSA, and endeavor to identify underlying nocturnal symptoms that could affect sleep quality and contribute to daytime fatigue. The present study did not involve an epidemiologic cohort sample, and the calculated PAR % must therefore be interpreted as an estimate using available data and assuming that OSA can play a causal role in development of fatigue. However, the PAR % estimates calculated in this study raise the possibility that a substantial portion of MS-related fatigue—between 11% and 40%—could be eliminated by diagnosis and successful treatment of OSA in patients with MS.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Braley has served as site P.I. for several industry-sponsored studies at the University of Michigan, including studies sponsored by Sanofi-Genzyme, Hoffmann-La Roche, Biogen-Idec, and AB Science but received no direct compensation for this work, and these studies were not related to the research presented in this manuscript. She is the recipient of an American Sleep Medicine Foundation Bridge-to-K grant, awarded in 2012. She is also named in a provisional patent, held by the University of Michigan, concerning treatment for obstructive sleep apnea. Dr. Segal is PI for an investigator initiated educational grant from TEVA to support an academic lecture series, serves as mentor for an MS clinical fellowship grant sponsored by Biogen-Idec, and has given grand rounds lecture for Novartis. He has served as a consultant for Biogen-Idec and Genzyme. He is also named in a provisional patent, held by the University of Michigan, concerning treatment for obstructive sleep apnea. Dr. Chervin: NIH, research grants; University of Michigan, research grants; Philips Respironics and Fisher Paykel, support to University of Michigan for educational program in sleep biomedical innovation; Board of Directors, American Academy of Sleep Medicine, American Sleep Medicine Foundation, American Board of Sleep Medicine, Associated Professional Sleep Societies, International Pediatric Sleep Association; Advisory Board (volunteer), Sweet Dreamzzz (not-for-profit community organization); Proctor & Gamble, consultant, through contract established with University of Michigan; MC3, consultant; Zansors, consultant, (not compensated); Zansors, licensed questionnaire (developed by author) from University of Michigan; UpToDate, editor; Cambridge University Press, book editor; Named in copyrighted material and patents, held by the University of Michigan, for sleep apnea and sleep disorder-related diagnosis, assessment, and treatments.
ACKNOWLEDGMENTS
The authors thank Veena Kutty, M.D., Cameron Griffin, Judy Rotthoff, R.N., and Kim Duval, M.A.S., for their assistance in survey administration and data management. Work was performed at the University of Michigan, Ann Arbor, MI.
REFERENCES
- 1.Krupp L. Fatigue is intrinsic to multiple sclerosis (MS) and is the most commonly reported symptom of the disease. Mult Scler. 2006;12:367–8. doi: 10.1191/135248506ms1373ed. [DOI] [PubMed] [Google Scholar]
- 2.Lerdal A, Celius EG, Krupp L, Dahl AA. A prospective study of patterns of fatigue in multiple sclerosis. Eur J Neurol. 2007;14:1338–43. doi: 10.1111/j.1468-1331.2007.01974.x. [DOI] [PubMed] [Google Scholar]
- 3.Janardhan V, Bakshi R. Quality of life in patients with multiple sclerosis: the impact of fatigue and depression. J Neurol Sci. 2002;205:51–8. doi: 10.1016/s0022-510x(02)00312-x. [DOI] [PubMed] [Google Scholar]
- 4.Krupp LB, Alvarez LA, LaRocca NG, Scheinberg LC. Fatigue in multiple sclerosis. Arch Neurol. 1988;45:435–7. doi: 10.1001/archneur.1988.00520280085020. [DOI] [PubMed] [Google Scholar]
- 5.Smith MM, Arnett PA. Factors related to employment status changes in individuals with multiple sclerosis. Mult Scler. 2005;11:602–9. doi: 10.1191/1352458505ms1204oa. [DOI] [PubMed] [Google Scholar]
- 6.Chervin RD. Sleepiness, fatigue, tiredness, and lack of energy in obstructive sleep apnea. Chest. 2000;118:372–9. doi: 10.1378/chest.118.2.372. [DOI] [PubMed] [Google Scholar]
- 7.Peppard PE. Is obstructive sleep apnea a risk factor for hypertension?--differences between the Wisconsin Sleep Cohort and the Sleep Heart Health Study. J Clin Sleep Med. 2009;5:404–5. [PMC free article] [PubMed] [Google Scholar]
- 8.Gottlieb DJ, Yenokyan G, Newman AB, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122:352–60. doi: 10.1161/CIRCULATIONAHA.109.901801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Redline S, Yenokyan G, Gottlieb DJ, et al. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med. 2010;182:269–77. doi: 10.1164/rccm.200911-1746OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Narkiewicz K, Somers VK. The sympathetic nervous system and obstructive sleep apnea: implications for hypertension. J Hypertens. 1997;15:1613–9. doi: 10.1097/00004872-199715120-00062. [DOI] [PubMed] [Google Scholar]
- 11.Ju G, Yoon IY, Lee SD, Kim TH, Choe JY, Kim KW. Effects of sleep apnea syndrome on delayed memory and executive function in elderly adults. J Am Geriatr Soc. 2012;60:1099–103. doi: 10.1111/j.1532-5415.2012.03961.x. [DOI] [PubMed] [Google Scholar]
- 12.Guarnieri B, Adorni F, Musicco M, et al. Prevalence of sleep disturbances in mild cognitive impairment and dementing disorders: a multicenter Italian clinical cross-sectional study on 431 patients. Dement Geriatr Cogn Disord. 2012;33:50–8. doi: 10.1159/000335363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hall MH, Okun ML, Sowers M, et al. Sleep is associated with the metabolic syndrome in a multi-ethnic cohort of midlife women: the SWAN Sleep Study. Sleep. 2012;35:783–90. doi: 10.5665/sleep.1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tregear S, Reston J, Schoelles K, Phillips B. Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clin Sleep Med. 2009;5:573–81. [PMC free article] [PubMed] [Google Scholar]
- 15.Veauthier C, Radbruch H, Gaede G, et al. Fatigue in multiple sclerosis is closely related to sleep disorders: a polysomnographic cross-sectional study. Mult Scler. 2011;17:613–22. doi: 10.1177/1352458510393772. [DOI] [PubMed] [Google Scholar]
- 16.Braley TJ, Segal BM, Chervin RD. Sleep-disordered breathing in multiple sclerosis. Neurology. 2012;79:929–36. doi: 10.1212/WNL.0b013e318266fa9d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaminska M, Kimoff R, Benedetti A, et al. Obstructive sleep apnea is associated with fatigue in multiple sclerosis. Mult Scler. 2012;18:1159–69. doi: 10.1177/1352458511432328. [DOI] [PubMed] [Google Scholar]
- 18.Ferini-Strambi L, Filippi M, Martinelli V, et al. Nocturnal sleep study in multiple sclerosis: correlations with clinical and brain magnetic resonance imaging findings. J Neurol Sci. 1994;125:194–7. doi: 10.1016/0022-510x(94)90035-3. [DOI] [PubMed] [Google Scholar]
- 19.Kaynak H, Altintas A, Kaynak D, et al. Fatigue and sleep disturbance in multiple sclerosis. Eur J Neurol. 2006;13:1333–9. doi: 10.1111/j.1468-1331.2006.01499.x. [DOI] [PubMed] [Google Scholar]
- 20.Neau JP, Paquereau J, Auche V, et al. Sleep disorders and multiple sclerosis: a clinical and polysomnography study. Eur Neurol. 2012;68:8–15. doi: 10.1159/000335076. [DOI] [PubMed] [Google Scholar]
- 21.Allen RP, Picchietti D, Hening WA, Trenkwalder C, Walters AS, Montplaisir J. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003;4:101–19. doi: 10.1016/s1389-9457(03)00010-8. [DOI] [PubMed] [Google Scholar]
- 22.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 23.Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46:1121–3. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 24.Chung F, Subramanyam R, Liao P, Sasaki E, Shapiro C, Sun Y. High STOP-Bang score indicates a high probability of obstructive sleep apnoea. Br J Anaesth. 2012;108:768–75. doi: 10.1093/bja/aes022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108:812–21. doi: 10.1097/ALN.0b013e31816d83e4. [DOI] [PubMed] [Google Scholar]
- 26.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 27.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS) Neurology. 1983;33:1444–52. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- 28.Hennekens CH, Buring JE, Mayrent SL. Boston: Little, Brown; 1987. Epidemiology in medicine. [Google Scholar]
- 29.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 30.Ancoli-Israel S, Kripke DF, Klauber MR, Mason WJ, Fell R, Kaplan O. Sleep-disordered breathing in community-dwelling elderly. Sleep. 1991;14:486–95. doi: 10.1093/sleep/14.6.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A. Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med. 1998;157:144–8. doi: 10.1164/ajrccm.157.1.9706079. [DOI] [PubMed] [Google Scholar]
- 32.Young T, Shahar E, Nieto FJ, et al. Predictors of sleep-disordered breathing in community-dwelling adults: the Sleep Heart Health Study. Arch Intern Med. 2002;162:893–900. doi: 10.1001/archinte.162.8.893. [DOI] [PubMed] [Google Scholar]
- 33.Fatigue Guidelines Development Panel of the Multiple Sclerosis Council for Clinical Practice Guidelines. Fatigue and Multiple Sclerosis. Washington: DC: Paralyzed Veterans of America; 1998. Evidence-Based Management Strategies for Fatigue in Multiple Sclerosis. [Google Scholar]
- 34.Ohayon MM, Reynolds CF, 3rd, Dauvilliers Y. Excessive sleep duration and quality of life. Ann Neurol. 2013;73:785–94. doi: 10.1002/ana.23818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Braley TJ, Chervin RD. Fatigue in multiple sclerosis: mechanisms, evaluation, and treatment. Sleep. 2010;33:1061–7. doi: 10.1093/sleep/33.8.1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Braley TJ, Chervin RD, Segal BM. Fatigue, tiredness, lack of energy, and sleepiness in multiple sclerosis patients referred for clinical polysomnography. Mult Scler Int. 2012;2012:673936. doi: 10.1155/2012/673936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Farney RJ, Walker BS, Farney RM, Snow GL, Walker JM. The STOP-Bang equivalent model and prediction of severity of obstructive sleep apnea: relation to polysomnographic measurements of the apnea/hypopnea index. J Clin Sleep Med. 2011;7:459–65B. doi: 10.5664/JCSM.1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dias RA, Hardin KA, Rose H, Agius MA, Apperson ML, Brass SD. Sleepiness, fatigue, and risk of obstructive sleep apnea using the STOP-BANG questionnaire in multiple sclerosis: a pilot study. Sleep Breath. 2012;16:1255–65. doi: 10.1007/s11325-011-0642-6. [DOI] [PubMed] [Google Scholar]
- 39.Archibald CJ, McGrath PJ, Ritvo PG, et al. Pain prevalence, severity and impact in a clinic sample of multiple sclerosis patients. Pain. 1994;58:89–93. doi: 10.1016/0304-3959(94)90188-0. [DOI] [PubMed] [Google Scholar]
- 40.Ehde DM, Osborne TL, Hanley MA, Jensen MP, Kraft GH. The scope and nature of pain in persons with multiple sclerosis. Mult Scler. 2006;12:629–38. doi: 10.1177/1352458506071346. [DOI] [PubMed] [Google Scholar]