A 37-year-old non-sleepy (Epworth Sleepiness Scale score of 8) female with a history of depression, obesity, and restless leg syndrome underwent a polysomnography (PSG) for evaluation of daytime fatigue and sleepiness. The split-night PSG revealed an apnea-hypopnea index (AHI) of 15/hour. However, vocalizations were noted during the diagnostic portion of the night that disappeared during the later portion of the study. A sample video PSG fragment with the nocturnal vocalizations is presented in Video 1.
QUESTION:
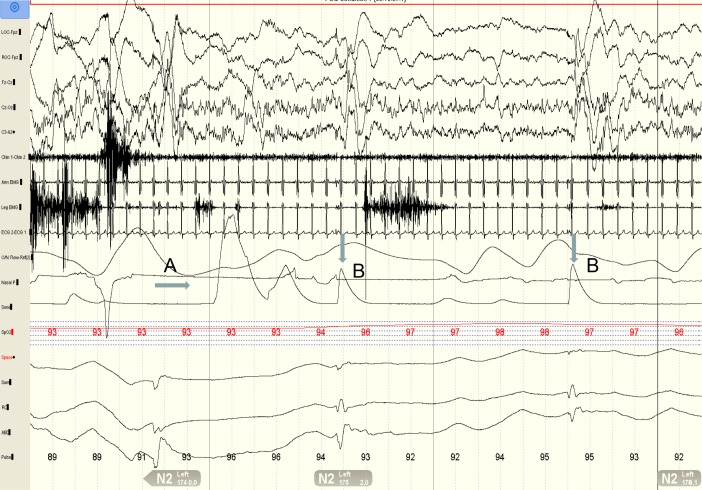
What is the diagnosis based on Video 1 and the PSG fragment presented in Figure 1?
Nocturnal frontal lobe epilepsy
Nocturnal hiccups and catathrenia
Stridor
REM sleep behavior disorder
ANSWER: B. Nocturnal hiccups and catathrenia
DISCUSSION
The video PSG fragment demonstrates the phenomena of both hiccups and catathrenia (Video 1). In the PSG fragment presented in Figure 2, we see the presence of catathrenia (marked by A) followed by hiccups (marked by B).
Figure 2. 30-second PSG fragment showing the presence of a catathrenia event with the sound of moaning/groaning (A) interrupted by 2 hiccups (B).
LOC, ROC: Ocular channels. FZ-CZ, CZ-OZ, C4-A1: Electroencephalographic (EEG) channels. Chin, arm and Leg EMG: chin, arm and leg electromyogram channels. The leg EMG was performed on both the lower extremities on the anterior tibialis muscle, while the arm EMG was performed on the right forearm muscles. ECG: electrocardiogram. CPAP: CPAP flow channel. Sono: Sonogram channel. SpO2: oxygen saturation. SUM: summation of chest and abdominal respiratory inductance plethysmography (RIP) bands. RC and ABD: chest and abdomen RIP bands. HR: heart rate.
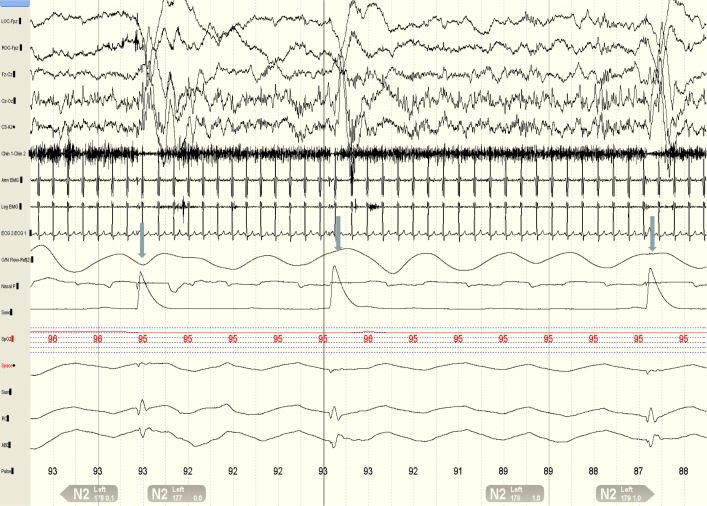
The literature on nocturnal hiccups is scarce. Hiccups usually stop at sleep onset; however, they may occur and persist during sleep. The frequency and periodicity varies based on the sleep stages.1 Occasionally, the frequency of the hiccups may vary in a similar fashion to the heart rate variability during REM sleep.1,2 A notable characteristic feature of nocturnal hiccups is the relationship with the phase of inspiration. During wakefulness, the onset of hiccups precedes the peak inspiratory excursion of the diaphragm, whereas during sleep, the onset coincides with the onset of diaphragmatic excursion leading to “synchrony” between hiccups and inspiration.1,3 In our patient, the hiccups were predominantly noted during stage N2; however, the frequency was variable and did not seem to correlate with the phase of respiration (Figure 3, arrows). The hiccups did not result in arousals or awakenings, and the patient was unaware of them, as was her husband. Though hiccups have been reported to increase sleep latency, decrease sleep efficiency, and decrease stage N3 and REM, this was not noticed in our patient. Data are inconclusive about an association between hiccups and obstructive sleep apnea (OSA).3
Figure 3. 30-second PSG fragment showing the presence of hiccups (arrows) during the early half of exhalation.
LOC, ROC: Ocular channels. FZ-CZ, CZ-OZ, C4-A1: Electroencephalographic (EEG) channels. Chin, arm and Leg EMG: chin, arm and leg electromyogram channels. The leg EMG was performed on both the lower extremities on the anterior tibialis muscle, while the arm EMG was performed on the right forearm muscles. ECG: electrocardiogram. CPAP: CPAP flow channel. Sono: Sonogram channel. SpO2: oxygen saturation. SUM: summation of chest and abdominal respiratory inductance plethysmography (RIP) bands. RC and ABD: chest and abdomen RIP bands. HR: heart rate.
The etiopathogenesis of hiccups is not entirely clear. Furthermore, epidemiological data on the prevalence of intractable hiccups is lacking. A case series of 220 patients noted a higher prevalence among older men.4 Hiccups were thought to be secondary to dysfunction of the respiratory system (i.e., diaphragmatic spasms, phrenic nerve excitation) versus disorders of the gastrointestinal system (gastric distension or reflux) or due to neurological (seizures, post-anoxic syndrome) or psychosomatic causes.2 Interestingly, in our patient, the hiccups subsided after she was placed on omeprazole for gastroesophageal reflux disease (GERD). Current hypothesis suggests that hiccups occur due to a dysfunction in the brainstem neural trigger mechanism leading to paradoxical activation of the “glottic closure complex” soon after the activation of the “inspiratory complex” leading to closure of the glottis during inhalation causing a tonic-phasic inspiratory obstruction sound known as the hiccup.2
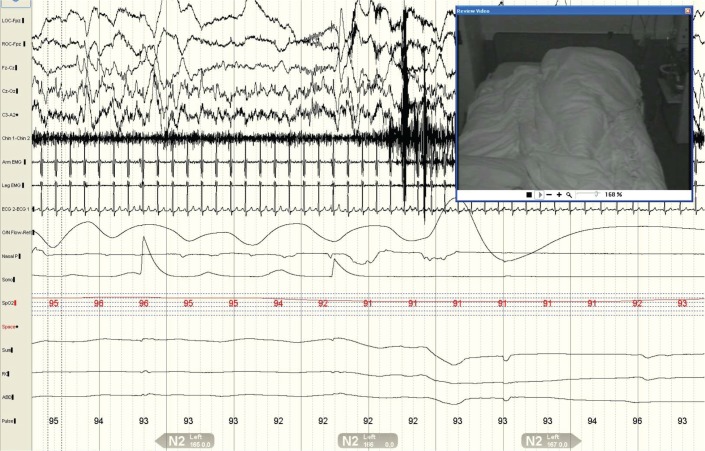
Catathrenia is a chronic disorder characterized by expiratory groaning/moaning during sleep and is categorized as a parasomnia under the International Classification of Sleep Disorders, 2nd edition (ICSD-2).5 It is a rare condition with only 40 cases reported in the literature since its original description in 1983.6 The classic PSG description of catathrenia is a deep inhalation followed by protracted exhalation during which moaning or groaning sounds are produced, usually lasting between 2 and 49 seconds.5,7 Our patient demonstrated these features in the PSG and this is shown in Figure 1 and Figure 2 (marked by A). The response of catathrenia to treatment with either medications or continuous positive airway pressure (CPAP) is variable, with some studies showing improvement or even elimination, while others show no improvement.8–10
Figure 1. 30-second epoch of a video PSG fragment.
LOC, ROC: Ocular channels. FZ-CZ, CZ-OZ, C4-A1: Electroencephalographic (EEG) channels. Chin, arm and Leg EMG: chin, arm and leg electromyogram channels. The leg EMG was performed on both the lower extremities on the anterior tibialis muscle, while the arm EMG was performed on the right forearm muscles. ECG: electrocardiogram. CPAP: CPAP flow channel. Sono: Sonogram channel. SpO2: oxygen saturation. SUM: summation of chest and abdominal respiratory inductance plethysmography (RIP) bands. RC and ABD: chest and abdomen RIP bands. HR: heart rate.
Our patient did well on CPAP to treat her OSA. Hiccups resolved with treatment of her GERD, and catathrenia was not a symptom that bothered her enough to be treated. This case illustrates the importance of simultaneously correlating the PSG tracings with the video and audio recordings to understand the ongoing phenomenon that may not be discernible by reviewing the PSG tracings alone.
CLINICAL PEARLS
Hiccups, though not uncommon during wakefulness, may persist during sleep, resulting in nocturnal sounds.
Catathrenia characterized by moaning and groaning during prolonged exhalation, is part of the spectrum of nocturnal vocalization-nocturnal sounds. As initially described, catathrenia was said to occur predominantly during REM sleep, but it can occur during NREM sleep (in some studies predominately during NREM sleep).
An awareness of these nocturnal sounds is important for a sleep clinician, so as not to confuse it with a different parasomnia or REM sleep behavior disorder.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest. There was no off-label or investigational use.
CITATION
Nannapaneni S; Olson E; Ramar K. Nocturnal vocalization. J Clin Sleep Med 2014;10(2):229-232.
REFERENCES
- 1.Askenasy JJ. Sleep hiccup. Sleep. 1988;11:187–94. doi: 10.1093/sleep/11.2.187. [DOI] [PubMed] [Google Scholar]
- 2.Askenasy JJ. About the mechanism of hiccup. Eur Neurol. 1992;32:159–63. doi: 10.1159/000116815. [DOI] [PubMed] [Google Scholar]
- 3.Arnulf I, Boisteanu D, Whitelaw WA, Cabane J, Garma L, Derenne JP. Chronic hiccups and sleep. Sleep. 1996;19:227–31. [PubMed] [Google Scholar]
- 4.Souadjian JV, Cain JC. Intractable hiccup. Etiologic factors in 220 cases. Postgrad Med. 1968;43:72–7. doi: 10.1080/00325481.1968.11693139. [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Sleep Medicine. 2nd edition. Westchester, IL: American Academy of Sleep Medicine; 2005. International Classification Of Sleep Disorders, Diagnostic and Coding Manual. [Google Scholar]
- 6.De Roeck J, Van Hoof E. Sleep-related expiratory groaning: a case report. J Sleep Res. 1983;12:377. [Google Scholar]
- 7.Abbasi AA, Morgenthaler TI, Slocumb NL, Tippmann-Peikert M, Olson EJ, Ramar K. Nocturnal moaning and groaning-catathrenia or nocturnal vocalizations. Sleep Breath. 2012;16:367–73. doi: 10.1007/s11325-011-0503-3. [DOI] [PubMed] [Google Scholar]
- 8.Guilleminault C, Hagen CC, Khaja AM. Catathrenia: parasomnia or uncommon feature of sleep disordered breathing? Sleep. 2008;31:132–9. doi: 10.1093/sleep/31.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iriarte J, Alegre M, Urrestarazu E, Viteri C, Arcocha J, Artieda J. Continuous positive airway pressure as treatment for catathrenia (nocturnal groaning) Neurology. 2006;66:609–10. doi: 10.1212/01.WNL.0000198503.93340.10. [DOI] [PubMed] [Google Scholar]
- 10.Pevernagie DA, Boon PA, Mariman AN, Verhaeghen DB, Pauwels RA. Vocalization during episodes of prolonged expiration: a parasomnia related to REM sleep. Sleep Med. 2001;2:19–30. doi: 10.1016/s1389-9457(00)00039-3. [DOI] [PubMed] [Google Scholar]