Abstract
Background:
Topical intranasal corticosteroids (INCSs) are used to control disease symptoms in patients with chronic rhinosinusitis with nasal polyposis (CRSwNP). The evidence to recommend INCSs as part of the postoperative care is limited. This study was designed to assess the efficacy of INCSs in the postoperative care of patients undergoing functional endoscopic sinus surgery (FESS) during the 1st year postoperatively.
Methods:
We searched the Cochrane Central Register of Controlled Trials (1995 to May 2012), MEDLINE (January 1948 to May 2012), EMBASE (January 1980 to May 2012), and the reference lists of articles. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed. Randomized controlled trials (RCT) and cohort studies comparing INCSs with placebo or comparing different types of INCSs were included.
Results:
Eleven studies (n = 945 patients) were RCTs and one prospective cohort study (n = 32 patients). As measured by the standardized mean difference (SMD) INCSs had a beneficial effect on symptom scores (SMD, −1.35; 95% CI, −2.05 to −0.64; p = 0.0002; 3 trials; 137 patients) and polyp score (SMD, 0.53; 95% CI, −0.91 to −0.14; p = 0.007; 5 trials; 223 patients). Compared with placebo, the use of INCSs decreased the odds of polyp recurrence (odds ratio, 0.17; 95% CI, 0.06–0.51; p = 0.002; 2 trials; 74 patients). Two RCTs (n = 105) and one cohort study (n = 32) reported normal adrenocorticotropic hormone levels postintervention.
Conclusion:
INCS use is a safe therapy in postoperative management of CRSwNP patients. INCS showed significant improvement in polyp score, patients' symptoms and significant decrease in polyp recurrence in the first year postoperatively.
Keywords: Endoscopic sinus surgery, intranasal corticosteroid, meta-analysis, nasal polyps, polyp recurrence, postoperative care, rhinosinusitis, symptom score, systematic review
Chronic rhinosinusitis with nasal polyposis (CRSwNP) affects 0.5–4% of the world population and is present in ∼20% of patients with CRS.1 Diagnosis of CRSwNP requires the presence of at least two of five symptoms (facial congestion/fullness, facial pain/pressure/fullness, nasal obstruction/blockage, purulent anterior/posterior nasal drainage, and/or hyposmia/anosmia), inflammation (e.g., discolored mucus, edema of middle meatus, or ethmoid area) documented by endoscopy and the presence of polyps in the middle meatus (documented by nasal endoscopy or computed tomography imaging).1,2
Topical treatment with intranasal corticosteroids (INCSs) has been widely used to control disease symptoms in patients with CRSwNP. In a recently published systematic review looking at the effect of INCSs, a substantial positive effect on patients' symptoms was found.2 INCS treatment favors the direct drug delivery to diseased mucosa and has the potential for delivering higher local drug concentrations, minimizing systemic absorption, and systemic side effects.3,4
Effectiveness of INCSs depends on type, dose, delivery method (i.e., nasal spray, drops, direct irrigation of the sinuses, catheters, and atomizer), and length of treatment. INCSs can be classified as modern (mometasone, fluticasone, and ciclesonide) versus first-generation corticosteroids (budesonide, beclomethasone, betamethasone, triamcinolone, and dexamethasone). The standard dose of modern INCSs varies from 200 to 800 μg, although higher doses (e.g., 1200–2800 μg) have been used in randomized trials.
The Canadian Clinical Practice Guidelines for Acute and Chronic Rhinosinusitis recommend the continued use of medical therapy postoperatively (i.e., antibiotics, topical or oral corticosteroids, and saline irrigation) in all patients to help achieve a successful outcome.1 The evidence behind this statement remains limited. INCSs after endoscopic sinus surgery (ESS) has shown variable results.1,5 Our research question is to look at the effect of topical nasal steroids on endoscopic scores and patient symptoms after ESS in patients with CRSwNP.
Our primary objective was to determine the effect of INCSs compared with placebo, another type of topical steroid, or no treatment in adult patients with CRSwNP who have undergone functional ESS (FESS) and polypectomy. The secondary objective was to evaluate the postoperative nasal polyp recurrence in the short (<1 year) and long term (>1 year) if available. Disease recurrence was defined as evidence of nasal polyps on nasoendoscopy or recurrence of sinonasal symptoms.
METHODS
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines6 were followed to develop this systematic review and meta-analysis. The review protocol is available on request.
Types of Studies
This article included randomized controlled trials (RCTs) and moderate-to-good quality prospective comparative cohort trials. The following studies were excluded from the review:
Studies failing to report at least one endoscopic-based outcome measure or one symptom-based outcome measure.
Studies with concomitant use of oral steroids pre- or postoperatively; similarly, studies comparing other type of medications (i.e., antileukotriene and antihistamines).
Studies reporting use of stents, nasal packages, meshes with slow drug (steroids) eluting and steroid impregnated dressings, direct delivery methods into the sinus such as direct cannulation, or irrigation postsurgery.
INCS treatment duration <3 weeks.
Patients with antrochoanal polyps, malignant polyps, cystic fibrosis, or primary ciliary dyskinesia.
Types of Participants
Adult patients (≥18 years old), of either gender, with CRSwNP (according to the Canadian practice guidelines definition) who have undergone FESS and have been followed with endoscopic assessments within the 1st year (minimum 3 months) after surgery were included in this study.
Types of Intervention
INCSs in the immediate postoperative period were used. The following variables were considered as part of the intervention of interest:
Duration of Treatment.
Patients were treated with INCSs once daily for a minimum of 6–8 weeks continuously.
Type of Steroid.
Modern corticosteroids such as mometasone furoate, fluticasone propionate, and fluticasone furoate as well as first-generation corticosteroids including budesonide, ciclesonide, flunisolide, triamcilonone, and betamethasone were used.
Dosing.
Standard dose was classified as 200–800 μg/day and high dose was classified as >800 μg/day.
Topical Delivery Method.
Only nasal delivery methods such as drops, sprays, nebulizer, or irrigations were included. Direct delivery methods into the sinus such as direct cannulation and irrigation postsurgery were excluded because of different indications, duration of treatment, and dosage of corticosteroid.
Comparison.
The comparison group was placebo, other type of INCSs, or no treatment. Studies including oral corticosteroids in the intervention in the entire follow-up period were excluded.
OUTCOME MEASURES
Primary Outcomes
1. Objective findings used postoperative endoscopy scales in the 1st year postoperatively. Endoscopic scores classifying the size of nasal polyps was the most commonly reported scoring system (0 = none, 1 = mild, 2 = moderate, and 3 = severe). More recently validated scales such as the perioperative sinus endoscopy score and Lund-Mackay score were also included when available.
2a. Subjective findings used the Sino-Nasal Outcome Test (SNOT-20, -21, or -22 versions): this scale is composed by rhinologic, ear, and facial symptoms; sleep, and psychological function. The items in the rhinologic symptoms subscale include need to blow nose, sneezing, runny nose, nasal obstruction, cough, postnasal discharge, and thick nasal discharge. Loss of smell or taste was added in the most updated version of this scale (SNOT-22). The scoring system for each item is from 0 to 5 for a maximum score of 110 for the SNOT-22.7
2b. Symptoms score scale: this scale that may include symptoms such as rhinorrhea, stuffiness, nasal obstruction and sneezing is linked to a Likert scale: 0 = none, 1 = mild, 2 = moderate, 3 = severe. The maximum score depends on the number of symptoms assessed.
Secondary Outcomes
Polyp recurrence (time to relapse and recurrence rate) as reported on endoscopy.
INCS safety, by measurement of adrenocorticotropic hormone (ACTH) levels and adverse event reporting.
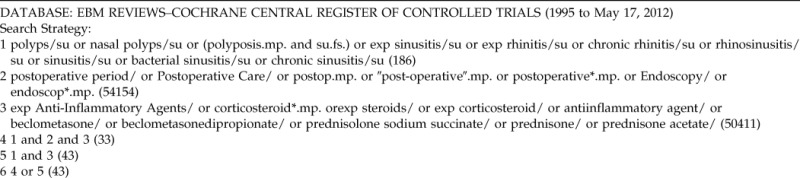
SEARCH METHODS FOR IDENTIFICATION OF STUDIES
Electronic Searches
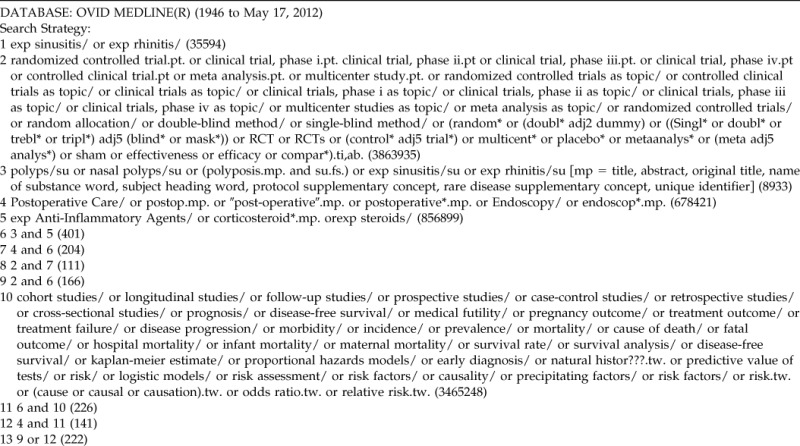
Primary literature sources were obtained by searching the MEDLINE (1948–2012) and EMBASE (1980–2012) electronic databases. Secondary literature sources included the Cochrane Central Register of Controlled Trials (1995–2012) as well as a manual search of the reference list of identified studies. The search strategy and MeSH terms for the three databases are presented in Appendix 1. Publications in any language were included.
Abstracts and proceedings were not included because it would be difficult to assess the study methodology, assess for risk of bias, and rate the quality of evidence.
Data Collection, Data Extraction, and Management
Two reviewers independently screened the titles and abstracts of studies according to the inclusion/exclusion criteria, read full-text papers, and extracted relevant data using a data extraction form. A cross-check was performed to ensure accuracy. Reviewers were not blinded to author, institution, journal of publication, or study results. Any disagreement was resolved by discussion and, if needed, a third reviewer helped to solve disagreements. If additional information was required, corresponding authors from the pertinent studies were contacted.
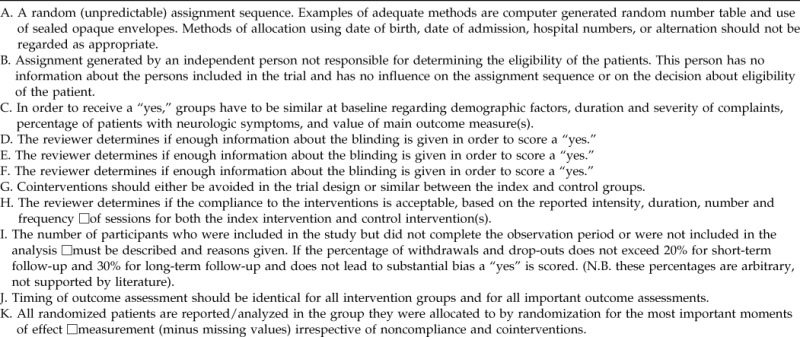
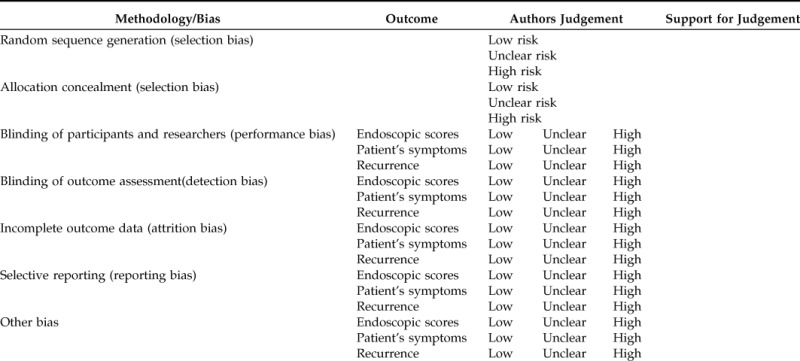
Assessment of Risk of Bias in Included Studies
The quality assessment of included studies was performed by two independent reviewers. The Cochrane tool for bias assessment of RCTs was used.8 This risk of bias tool covers six domains of bias: selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias. Special value was given to blinding of participants and investigators because by nature the primary outcome was at risk for outcome assessor bias and Hawthorne effect.
For the quality assessment we used a tool developed by the Cochrane collaboration back review group.9 The criteria list and the operationalization guide (Appendix 2) were used to assess the quality of each study. The following categories were used to rate the studies according to the number of times “yes” was answered: 1–3, very low quality; 4–6, low quality; 7–9 moderate quality; and 10–11, high quality.
To appraise cohort studies, the Newcastle-Ottawa scale was used.10 Studies with 7–9 stars are considered as high quality, 5–6 stars were moderate quality, 3–4 stars were low quality, and 1–2 stars were very low quality.
Measures of Treatment Effect
Endoscopic evaluation and patient symptoms recorded by validated and nonvalidated scales were considered as continuous variables. The mean and standard deviation (SD) for each scale were recorded in each study. The overall treatment effect was measured by standardized mean difference (SMD). This method assumes that the differences in SD among studies reflect differences in measurement scales and not real differences in variability among participants. Disease recurrence was recorded as a proportion (odds ratio [OR]; 95% confidence interval [CI]) or as a time to event (hazard ratio [HR]; 95% CI) when applicable.
Missing Data
The corresponding authors were contacted to obtain missing values such as p value, SD, CI 95%, and standard error (for calculation of SD in particular cases). If authors did not respond, these studies were excluded from the meta-analysis.
Assessment of Heterogeneity
Given the likelihood of between-study variability, we anticipated moderate-to-high heterogeneity in outcome measurement and reporting across the studies. A random effect model was used to combine results across studies. Heterogeneity was evaluated with the χ2-test and a p value of 0.1 was considered significant. The I2 statistic was used to assess the level of heterogeneity as follows: 0%, no heterogeneity; 25%, low; 50%, moderate; and >75%, severe.
Assessment of Reporting Biases
Testing and adjusting for publication bias was attempted by performing a funnel plot. However, because of the small number of combinable studies per outcome measure, it was difficult to assess reporting bias. Reporting language bias was avoided by including articles published in any language.
Data Synthesis
Data collected were synthesized and analyzed with Review Manager (RevMan) Version 5.1. Copenhagen (The Nordic Cochrane Center, The Cochrane Collaboration, 2011). Meta-analysis using continuous data methods such as weighted SMD for overall endoscopy scores and patient's symptoms scores were used to summarize results across studies. Appropriate calculation of SMD (95% CI) and OR (95% CI) was performed for each comparison group as deemed appropriate. The random effects model was used to estimate the overall estimate from studies in which more than one study had combinable outcome data by virtue of similar or identical assessment, at comparable follow-up times in comparable populations. Similarly, in the same populations, we analyzed the proportion of patients that recurred in the 1st year after surgery in the active treatment group versus placebo.
Subgroup Analysis and Investigation of Heterogeneity
A subgroup analysis was performed to evaluate the efficacy of treatments by grouping patients by corticosteroid type: modern steroids versus first-generation corticosteroids; dose, high dose (>800 μg/day) versus low dose (<200 μg/day) of INCSs and Samter's triad patients.
Sensitivity Analysis
A sensitivity analysis was conducted to assess the robustness of the results. Results were calculated first using all studies and then excluding lower-quality studies. If a study appeared to be an outlier, the influence of individual studies was assessed on the meta-analysis by excluding each study and evaluating variability in the robustness of the overall estimate.
RESULTS
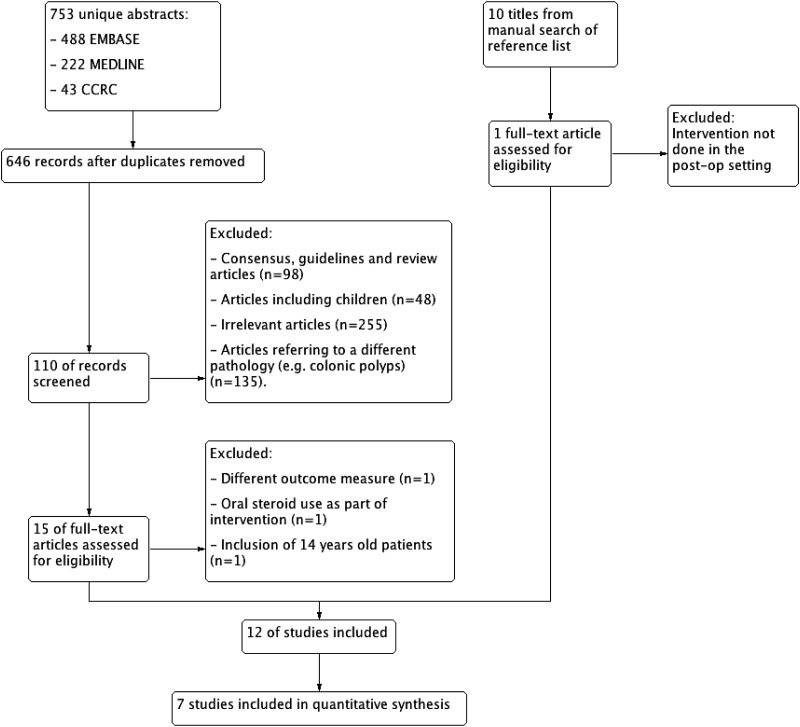
The search strategy identified 753 unique abstracts (488 EMBASE, 222 MEDLINE, and 43 Cochrane central databases). A total of 110 titles and abstracts were reviewed by two independent reviewers. An additional 10 titles were found by performing a manual search of the reference list from the selected articles. The κ-correlation coefficient showed good agreement between reviewers (k = 0.72). Disagreement was resolved by consensus. A total of 16 articles were obtained for full text review. Reasons for exclusion include use of different outcome measures,11 oral steroid use as part of the intervention,12 intervention of interest was not performed in the immediate postoperative care setting,13 and inclusion of patients <18 years of age14 (Fig. 1).
Figure 1.
Study flow diagram.
Included Studies
Thirteen studies involving 977 patients were included in this study. Eleven (n = 945 patients) were RCTs and one was a prospective cohort study (n = 32 patients).15 The intervention included placebo comparison in 85% of cases (n = 945 patients). The outcome measures used in the included studies were polyp size (endoscopic scores) and patient symptoms to report their outcomes. One article reported time to relapse to account for disease recurrence15 and the rest used recurrence rates. For further details, refer to characteristics of included studies in Table 1.
Table 1.
Characteristics of included studies
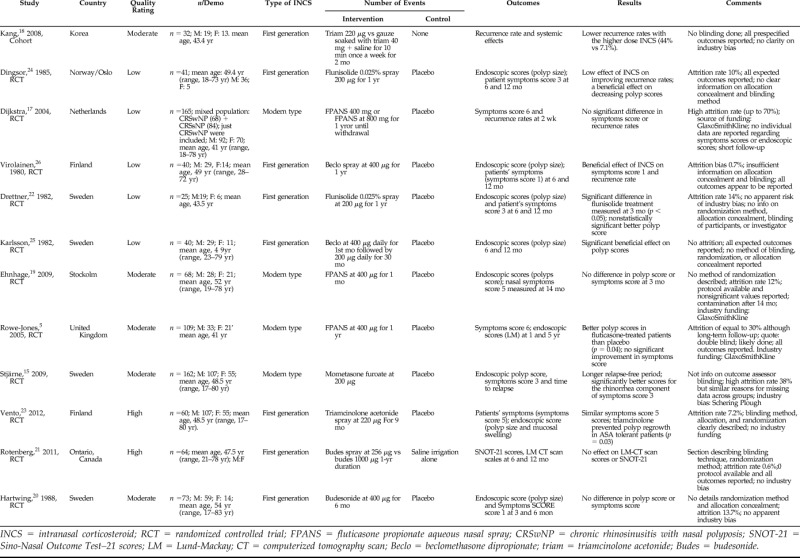
INCS = intranasal corticosteroid; RCT = randomized controlled trial; FPANS = fluticasone propionate aqueous nasal spray; CRSwNP = chronic rhinosinusitis with nasal polyposis; SNOT-21 = Sino-Nasal Outcome Test–21 scores; LM = Lund-Mackay; CT = computerized tomography scan; Beclo = beclomethasone dipropionate; triam = triamcinolone acetonide; Budes = budesonide.
Risk of Bias in Included Studies
The general risk of bias of the included studies was considered to be low. It is worth noting that there was minimal clarity on randomization method, blinding, and allocation concealment in most of the studies published before 1990. This change in reporting may have been improved after the publication of the CONSORT statement and the mandatory registration of the study protocol in clinicaltrials.gov.16 Selection bias was unclear or not specified in 55% of the included RCTs (n = 384, 6/11). All studies were reported as double blind although just 60% (n = 246; 8/13) of them clearly described who was blinded and what blinding method was used. The risk of attrition bias was low for 70% (n = 605, 9/13) and unclear in 15% (n = 169, 2/13). Fifteen percent (n = 274, 2/13) of studies were at high risk of incomplete outcome data with an attrition rate of 38%15 and up to 70%.17 Overall reporting bias assessment was considered as low risk (85%). Just 15% (n = 270; 3/1318–20) of included studies were at high risk of selective reporting. The main reason was a lack in reporting outcomes of interest. In 30% of studies (n = 342) it was unclear if there was funding bias (Schering Plough15 and GlaxoSmithKline).5,17,19
Qualitative Analysis
Modern versus First-Line INCSs.
All studies showed a significant benefit from INCS therapy compared with placebo, with the exception of three that did not find a statistically significant difference.5,17,21 Dijkstra et al.,17 had a high withdrawal rate (64–70%) that may explain the lack of a significant difference. Rotenberg et al.21 published a high-quality study that found no effect from budesonide treatment in comparison with placebo in Samter's triad patients. In the following section we present the results of the studies that did not have combinable data for the meta-analysis.
Endoscopic Scores
First-Generation INCS.
Drettner, et al.22 a moderate-quality study reported a nonstatistically significant better polyp score when comparing flunisolide with placebo at 3 months follow-up (p > 0.05).22 Unfortunately, no exact p value was reported and therefore an SD for the reported scores could not be calculated. The follow-up time was probably too short to detect a significant difference with regard to polyp regrowth.
Modern Type INCSs.
Ehnhage, et al.19 2009, also found no difference in polyp score in fluticasone propionate at 400 μg twice daily treated patients in comparison with placebo.19 Despite being a high-quality article, the intervention was given for a short period of 4 weeks and the patients were followed for only 3 months. These treatments and follow-up times are likely too short to detect an effect on endoscopic scores. Rowe-Jones, et al.5 showed at 1-year follow-up better polyp scores in fluticasone-treated patients than placebo (p = 0.04).5 However, edema and discharge scores were not statistically significant different (p = 0.52 and p =0 .94, respectively). The overall p value of the combined endoscopic score (polyp, edema, and discharge) was also not significant between groups (p = 0.74). The attrition rate of this high-quality study was considerable (31 and 36% at 1 and 5 years, respectively), which may bias the interpretation of the results.
Stjärne, et al.15 reported that subjects who underwent FESS and were treated with mometasone furoate nasal spray resulted in a significantly longer relapse-free period than placebo in both the intention to treat (ITT) and the per protocol data sets.15 For the per protocol analysis, the median time to relapse was 173 days in the mometasone group and 61 days in the placebo group (p = 0.007; HR and 95% CI, 0.72 [0.55–0.93]). Median time to relapse in the ITT population was >175 days in the mometasone group and 125 days in the placebo group (p = 0.049; HR and 95% CI, 0.79 [0.62–0.99]).
Symptoms Scores
In the first-generation INCS trials, two high-quality studies21,23 found no beneficial effect of INCS use reflected on symptom scores. Rotenberg et al.21 used the SNOT-21 to evaluate symptoms in Samter's triad patients after treatment with budesonide 64-μg nasal spray or 1000-μg nasal irrigations and saline nasal irrigation as the control and found no statistically significant difference between the treatment groups21; Vento et al.23 found similar (symptoms score 5: sense of smell, nasal itching, sneezing, runny nose, and nasal blockage) scores in CRSwNP patients treated with triamcinolone 220-μg nasal spray or placebo.23 Drettner et al.22 conducted a moderate-quality trial and found a significant difference (symptoms score 3: stuffy nose, runny nose, and sneezing) with flunisolide treatment compared with placebo measured at 3 months (p < 0.05).22
In the modern-type INCS trials, Dijkstra17 (symptoms score 6 symptoms: blockage, rhinorrhea, anosmia, epistaxis, facial pain, and headache) included a mixed population of patients with and without nasal polyps. The data on the CRSwNP patients were extracted and analyzed. There was no significant difference between the effect of fluticasone compared with placebo on individual symptoms or on the total symptom score.17 In addition, Ehnhage,19 (symptoms score 5: sense of smell, nasal congestion and rhinorrhea, shortness of breath, and cough), found no difference between subjects treated with fluticasone versus placebo at 3 months follow-up.19 Again, this may be attributable to the short follow-up time and short treatment period (4 weeks). Also, in this study after 14 weeks, all patients received INCSs, allowing for contamination and making interpretation of the results difficult. Rowe-Jones5 also found similar scores (symptoms score 5: edema, discharge, nasal mucociliary clearance, olfactory detection, and nasal volumes) between fluticasone and placebo at 1 year of follow-up.5 The only study that found a beneficial effect from the modern-type INCS was published by Stjärne.15 They did find significantly better scores (symptoms score 3: congestion, rhinorrhea, andsense of smell) for the rhinorrhea component of the symptoms score in the ITT data set of the mometasone group (p = 0.04; mean difference [95% CI], 0.15 [0.01–0.30]), although no difference was found for congestion or sense of smell.15
Recurrence Rates
One cohort study was found comparing different doses and types of INCSs. Kang18 (low quality) compared triamcinolone acetonide 220-μg spray twice daily with 40 mg of triamcinolone-soaked packing in the middle meatus weekly, changed every 2 months.18 The difference in recurrence rates was statistically significant, favoring the higher-dose INCS (44% versus 7.1%).
Standard-Dose versus High-Dose INCS.
Two studies compared the use of standard dose of INCS with a significantly higher dose of the same compound (n = 96).18,21 Kang et al.18 found a statistically significant higher recurrence rate of 44% in the standard dose of triamcinolone acetonide spray at 220 μg daily (p < 0.05).18 Rotenberg et al.21 compared budesonide spray at 64 μg versus budesonide irrigation at 1000 μg versus saline irrigation (control group). They found that in Samter's triad patients, there were no statistically or clinically significant differences between groups at any time point (p > 0.05).21
Safety and Side Effects.
Two RCTs (n = 105)19,24 reported normal ACTH levels at baseline and postintervention in all patients. Rotenberg21 reported no clinically significant changes in intraocular pressure measurements during the duration of the study.21 Dingsor24 measured systolic and diastolic pressure before and 1 hour after the intervention were not significantly different.24 One cohort study (n = 32)18 reported normal ACTH levels measured before and 1 hour after removal of corticosteroid-soaked packing gauze.18 The reported adverse events from the included studies were blood-stained mucus,22–25 mild epistaxis,15,17,19 and nasal dryness.22,23,26
META-ANALYSIS
To combine the different scales with similar construct across studies (endoscopic and symptoms scores), it was decided to use the SMD. This method assumes that the differences in SD among studies reflect differences in measurement scales and not real differences in variability among participants. The overall intervention effect is reported in units of SD rather than in units of any of the measurement scales. All of the outcomes are reported at 6–12 months postoperatively. A total of seven articles were included in the meta-analysis.
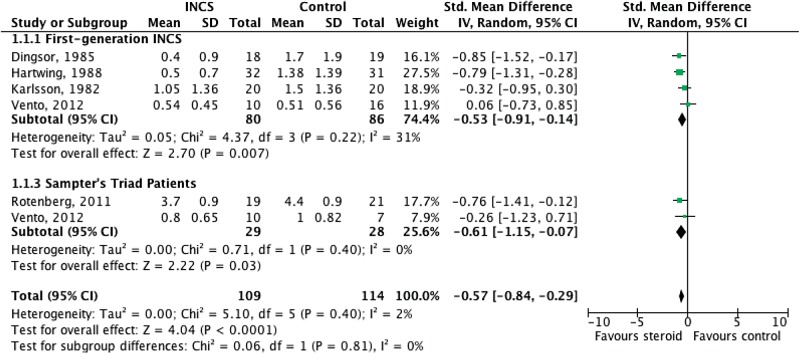
Endoscopic Score—Polyp Size
Of the eight studies comparing INCSs to placebo or control groups (saline irrigation) on endoscopic scores, the results of five trials (n = 223)5,20,23–25 were suitable to combine in the meta-analysis. The pooled results favored the topical steroid group. The combined SMD was −0.53 (95% CI, −0.91 to −0.14; p = 0.007). The I2 was 31%, suggesting low heterogeneity (χ2 = 4.37; degrees of freedom (df) = 3; p = 0.22; Fig. 2).
Figure 2.
Forest plot of comparison: effect of intranasal corticosteroid (INCS) versus placebo on endoscopic score (6–12 months).
Karlsson25 also found a statistically significant difference in polyp regrowth from 6 months of follow-up onward when comparing beclomethasone with placebo (mean estimation from graph values at 6 months, INCS [SD], 1.05(1.36); placebo, 1.5 [1.36]; p = 0.003). SD was calculated from the p value and given means estimated from the graph.23,25
Vento23 reported that triamcinolone in comparison with placebo appeared to prevent polyp regrowth in acetysalicylic acid (ASA)-tolerant patients (p = 0.03) measured at 9 months but not in ASA-intolerant patients (p = 0.28). The corresponding author was contacted and he provided the SD for each group. The mean was calculated by subtracting the mean change from the baseline value. The results from the ASA-tolerant patients were included in the main meta-analysis of patients with CRSwNP.
A subgroup analysis was performed combining ASA-intolerant patients,23 with Samter's triad population,21 assuming both populations were similar.
Symptoms Score
Of the 10 studies comparing INCSs to placebo or to a control group (saline irrigation) on symptoms scores, just 3 trials (n = 137)20,24,26 could be combined for pooled data analyses. The combined SMD of symptoms scores (Fig. 3) showed a significant benefit of INCSs (−1.35; 95% CI, −2.05 to −0.64; p = 0.0002). The I2 was 69%, suggesting moderate heterogeneity (χ2 = 6.46; df = 2; p = 0.04). Similarly, the degree of heterogeneity could be explained because of the use of nonvalidated tools to assess different symptoms score scales.
Figure 3.
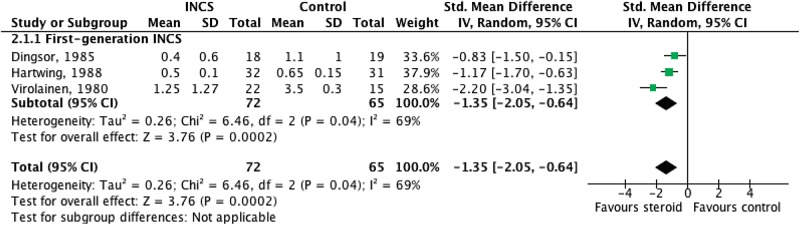
Forest plot of comparison: effect of intranasal corticosteroid (INCS) versus placebo on symptoms score (6–12 months).
Recurrence Rate
Of the six studies comparing INCSs with placebo or to control group (saline irrigation), two studies of moderate-to-high quality in the first generation INCS group (n = 74)24,26 had combinable data on recurrence rate of polyps. The study performed by Dijkstra was excluded because of its very low quality.17 Pooled data analyses on recurrence rates showed beneficial effect in the topical steroid group. The combined results favored the INCS group showing a beneficial effect associated to INCS use, with a combined OR, 0.17; 95% CI, 0.06–0.51; p = 0.002; Fig. 4). The I2 was 0%, suggesting no heterogeneity (χ2 = 1.92; df = 2; p = 0.38).
Figure 4.
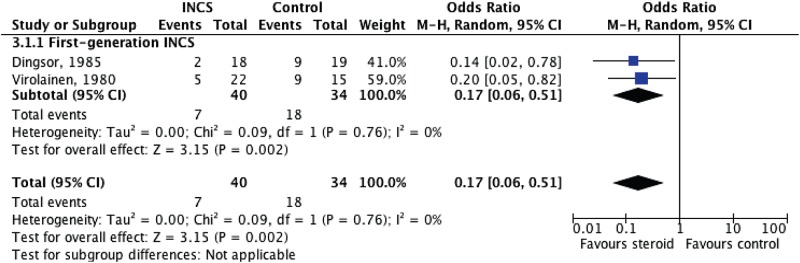
Forest plot of comparison: effect of intranasal corticosteroid (INCS) versus placebo on recurrence rate of polyps.
SENSITIVITY ANALYSIS
After excluding one by one the low-quality studies from the model,24,25 there was no significant change in the overall effect of INCSs on polyp score. The overall SMD for endoscopic score showed a significant protective effect from INCS use: −0.54; 95% CI, −0.93 to −0.15; p = 0.007. In the same manner we removed the low-quality studies from the pooled analysis of symptoms score24,26 and there was no significant change in the overall SMD, maintaining the beneficial effect of INCSs on symptom scores.
DISCUSSION
Summary of Main Results
One of the major challenges to produce an overall effect estimate of topical steroid therapy on nasal symptoms was the inherent heterogeneity with approaches to symptom assessment. To produce meaningful results, it is important to combine studies that are clinically and methodologically similar. We found just three older articles that allowed for pooled analysis showing that the use of INCSs after ESS during the 1st year of follow-up has a beneficial effect on symptom scores measured by symptoms score. In addition to these studies, there were a proportion of trials that were not used to combine data in the quantitative analysis. Interestingly, the majority of recently published trials not included in the quantitative analysis reported no beneficial effect from INCS on nasal symptoms. On the other hand, the SMD of polyp score showed a beneficial effect with INCS. The value of SMD is difficult to interpret, because the scales used to endoscopically assess polyp change were dissimilar.
The combined OR of 0.17 (95% CI, 0.06–0.51) is difficult to interpret. Patients with CRSwNP continuously using INCS 1 year after sinus surgery have odds of 0.17 lower compared with placebo (treated patients are 83% less likely to have polyp recurrence). In other words, the odds to recur in patients receiving placebo is 5.88 times higher than that in patients treated with INCSs.
Pooled analysis from high-quality evidence suggests that the use of INCS in Samter's triad/ASA-intolerant patients had a beneficial effect in endoscopic polyp score. These studies were not included in the meta-analysis of symptoms score because they used completely different outcome measures and the Samter's triad population may have a different spectrum of disease.
A strong conclusion can not be made on first-generation INCS versus modern-type INCSs because of the significant increase in the publication rate of trials using modern INCSs. We assume that the use of first-generation INCSs has increased because they allow for higher-dose administration with a similar side effect profile. The studies comparing low dose versus high dose of INCS were in favor of using higher doses to decrease recurrence rate of polyps. This evidence, however, remains limited.
The systemic bioavailability of INCS varies from <1% to up to 40–50%, which in turn influences the risk of systemic adverse effects.4,27 One of the most sensitive measures of systemic corticosteroid bioactivity is suppression of endogenous cortisol secretion from the adrenal cortex. The studies reporting ACTH levels indicated that INCS treatment had no effect on the hypothalamic–pituitary–adrenal axis, confirming this therapy to be safe. In addition, no significant changes on intraocular pressure and blood pressure changes were reported. Minor local side effects such as mild epistaxis and dryness were also described.
Overall Completeness and Applicability of Evidence
The management of nasal polyps can be challenging and often requires long-term medical treatment to control nasal symptoms. This systematic review and meta- analysis further validates the efficacy of topical nasal steroid therapy in decreasing recurrence of polyps in patients with CRSwNP and improving symptoms and polyp scores. Although there was expected heterogeneity across studies, sensitivity analysis confirmed that the overall positive effect was not the result of any single study. It is important to note that the great majority of studies (12 of 13) were performed in Europe, which may limit the applicability of the results worldwide.
Quality of the Evidence
The overall quality of evidence evaluating the recurrence rate of nasal polyps in this meta-analysis was low to moderate. The main reason may be the lack of reporting standards back in 1980. These randomized trials were downgraded because of lack of blinding, clarity in allocation concealment, and randomization methods (Table 1).
The qualitative analysis showed that the moderate- and high-quality articles available reported controversial and inconsistent findings. This body of evidence prevents us from making a strong statement with regard to polyp recurrence, patient′s symptoms, or endoscopic scores and highlights the need for updated, high-quality, multicenter trials on this topic.
Potential Biases in the Review Process
Publication bias was not evaluated because of the low number of articles included in the pooled analysis of individual outcomes, making it difficult to interpret a symmetric funnel plot.28
Agreements and Disagreements with Other Studies or Reviews
As established in this article, there have been numerous individual studies evaluating the role of topical corticosteroid therapy in patients with nasal polyposis. Aouad and Chiu, in a review of the “state of art” treatment of nasal polyposis, acknowledge the advantage of topical medication in preventing polyp reformation and highlight their use as the mainstay of therapy.29 Two recent systematic reviews with meta-analyses2,30 looking at the first two outcomes have explored the impact of topical steroid therapy in the management of CRSwNP patients with active disease. Similarly, the results of this meta-analysis supported a beneficial effect of INCS use after FESS in polyp and symptom scores.
With regard to safety of INCSs, in general, the effects of INCS on hypothalamic–pituitary–adrenal axis suppression are minimal at 800 μg/day in adults and 400 μg/day in children according to previous reviews.31 For this reason, INCSs, given in recommended dosages, are not expected to cause major systemic adverse effects, a statement that is in agreement with our results. The interindividual susceptibility and variability in adrenal suppression at a given dose of ICS must be taken in consideration and explained to the patients.
CONCLUSIONS
Implications for Practice
The use of INCS is a safe therapy recommended in the postoperative care of patients with CRSwNP after endoscopic surgery that may improve endoscopic polyp score and symptom scores and likely reduces the recurrence of polyps (derived from outdated low-to-moderate–quality evidence).
Implications for Research
A well-designed multicenter randomized trial is needed, with validated disease-specific symptom scales and endoscopic scales to better determine if the use of INCS improves patient symptoms and prevents polyp recurrence after ESS.
Differences between Protocol and Review
A sub-group analysis of patients with Samter's triad was performed to account for disease severity in this population.
ACKNOWLEDGMENTS
Special thanks to Dr. Prakesh Shah and Joseph Bayene for their input during the protocol development stage.
APPENDIX 1
Search Strategy
EMBASE Literature Search Strategy
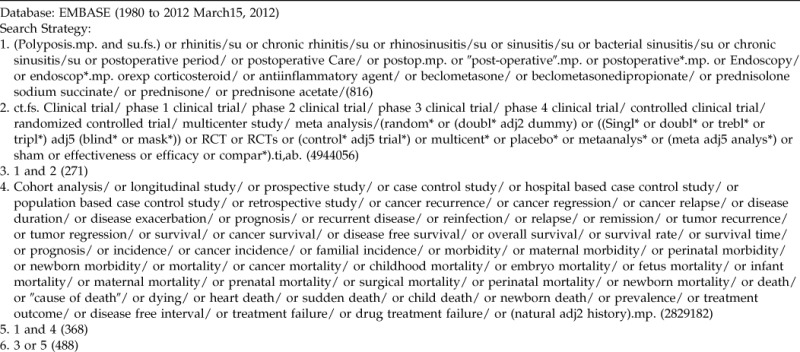
MEDLINE Literature Search Strategy
Cochrane Database Literature Search Strategy
APPENDIX 2
Quality and Bias Assessment Tool
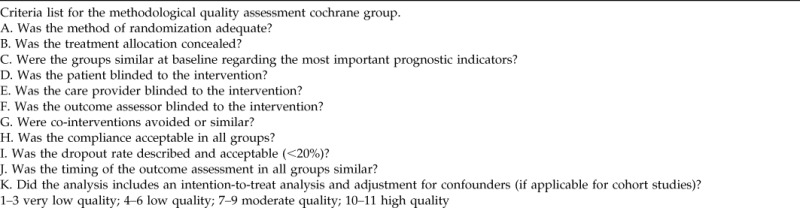
Operationalization of the Criteria List
Bias Assessment Tool
Footnotes
Funded, internally, by the Department of Otolaryngology–Head and Neck Surgery, University of Toronto
Presented at the Canadian Otolaryngology Society Meeting, Banff, Alberta, Canada, June 2–4, 2013
IJ Witterick is Speaker for Merck Canada, GlaxoSmithKline and Consultant for Alcon, Johnson & Johnson, and Pharmascience. The remaining authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Desrosiers M, Evans GA, Keith PK, et al. Canadian clinical practice guidelines for acute and chronic rhinosinusitis. Allergy Asthma Clin Immunol 7:1–38, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rudmik L, Schlosser RJ, Smith TL, Soler ZM. Impact of topical nasal steroid therapy on symptoms of nasal polyposis: A meta-analysis. Laryngoscope 122:1431–1437, 2012. [DOI] [PubMed] [Google Scholar]
- 3. Demoly P. Safety of intranasal corticosteroids in acute rhinosinusitis. Am J Otolaryngol 29:403–413, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Derendorf H, Meltzer EO. Molecular and clinical pharmacology of intranasal corticosteroids: Clinical and therapeutic implications. Allergy 63:1292–1300, 2008. [DOI] [PubMed] [Google Scholar]
- 5. Rowe-Jones JM, Medcalf M, Durham SR, et al. Functional endoscopic sinus surgery: 5 Year follow up and results of a prospective, randomised, stratified, double-blind, placebo controlled study of postoperative fluticasone propionate aqueous nasal spray. Rhinology 43:2–10, 2005. [PubMed] [Google Scholar]
- 6. Liberati A. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. 62:e1–e34, 2009. [DOI] [PubMed] [Google Scholar]
- 7. Browne JP, Hopkins C, Slack R, Cano SJ. The Sino-Nasal Outcome Test (SNOT): Can we make it more clinically meaningful? Otolaryngol Head Neck Surg 136:736–741, 2007. [DOI] [PubMed] [Google Scholar]
- 8. Higgins J, Altman DG, Gotzsche PC. The Cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ 342:1–9, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. van Tulder M, Furlan A, Bombardier C, et al. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine 28:1290–1299, 2003. [DOI] [PubMed] [Google Scholar]
- 10. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605, 2010. [DOI] [PubMed] [Google Scholar]
- 11. Olsson P, Ehnhage A, Nordin S, et al. NAF2S2 Study Group. Quality of life is improved by endoscopic surgery and fluticasone in nasal polyposis with asthma. Rhinology 48:325–330, 2010. [DOI] [PubMed] [Google Scholar]
- 12. Jorissen M, Bachert C. Effect of corticosteroids on wound healing after endoscopic sinus surgery. Rhinology 47:280–286, 2009. [DOI] [PubMed] [Google Scholar]
- 13. Penttilä M, Poulsen P, Hollingworth K, Holmström M. Dose-related efficacy and tolerability of fluticasone propionate nasal drops 400 mg once daily and twice daily in the treatment of bilateral nasal polyposis: A placebo-controlled randomized study in adult patients. Clin Exp Allergy 30:94–102, 2000. [DOI] [PubMed] [Google Scholar]
- 14. Bross-Soriano D, Arrieta-Gomez JR, Prado-Calleros H. Infections after endoscopic polypectomy using nasal steroids. Otolaryngol Head Neck Surg 130:319–322, 2004. [DOI] [PubMed] [Google Scholar]
- 15. Stjärne P, Olsson P, Alenius M. Use of mometasone furoate to prevent polyp relapse after endoscopic sinus surgery. Arch Otolaryngol Head Neck Surg 135:296–302, 2009. [DOI] [PubMed] [Google Scholar]
- 16. Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol 63:e1–e37, 2010. [DOI] [PubMed] [Google Scholar]
- 17. Dijkstra MD, Ebbens FA, Poublon RM, Fokkens WJ. Fluticasone propionate aqueous nasal spray does not influence the recurrence rate of chronic rhinosinusitis and nasal polyps 1 year after functional endoscopic sinus surgery. Clin Exp Allergy 34:1395–1400, 2004. [DOI] [PubMed] [Google Scholar]
- 18. Kang IG, Yoon BK, Jung JH, et al. The effect of high-dose topical corticosteroid therapy on prevention of recurrent nasal polyps after revision endoscopic sinus surgery. Am J Rhinol 22:497–501, 2008. [DOI] [PubMed] [Google Scholar]
- 19. Ehnhage A, Olsson P, Kölbeck KG, et al. Functional endoscopic sinus surgery improved asthma symptoms as well as PEFR and olfaction in patients with nasal polyposis. Allergy 64:762–769, 2009. [DOI] [PubMed] [Google Scholar]
- 20. Hartwig S, Linden M, Laurent C, et al. Budesonide nasal spray as prophylactic treatment after polypectomy (a double blind clinical trial). J Laryngol Otol 102:148–151, 1988. [DOI] [PubMed] [Google Scholar]
- 21. Rotenberg BW, Zhang I, Arra I, Payton KB. Postoperative care for Samter's triad patients undergoing endoscopic sinus surgery: A double-blinded, randomized controlled trial. Laryngoscope 121:2702–2705, 2011. [DOI] [PubMed] [Google Scholar]
- 22. Drettner B, Ebbesen A, Nilsson M. Prophylactive treatment with flunisolide after polypectomy. Rhinology 20:149–158, 1982. [PubMed] [Google Scholar]
- 23. Vento SI, Vento K, Blomgren K, et al. Prevention of relapses of nasal polyposis with intranasal triamcinolone acetonide after polyp surgery: A prospective double-blind, placebo-controlled, randomised study with a 9-month follow-up. Clin Otolaryngol 37:117–123, 2012. [DOI] [PubMed] [Google Scholar]
- 24. Dingsor G, Kramer J, Olsholt R, Søderstrøm T. Flunisolide nasal spray 0.025% in the prophylactic treatment of nasal polyposis after polypectomy. A randomized, double blind, parallel, placebo controlled study. Rhinology 23:49–58, 1985. [PubMed] [Google Scholar]
- 25. Karlsson G, Rundcrantz H. A randomized trial of intranasal beclomethasone dipropionate after polypectomy. Rhinology 20:144–148, 1982. [PubMed] [Google Scholar]
- 26. Virolainen E, Puhakka H. The effect of intranasal beclomethasone dipropionate on the recurrence of nasal polyps after ethmoidectomy. Rhinology 18:9–18, 1980. [PubMed] [Google Scholar]
- 27. Salib RJ, Howarth PH. Safety and tolerability profiles of intranasal antihistamines and intranasal corticosteroids in the treatment of allergic rhinitis. Drug Saf 26:863–893, 2003. [DOI] [PubMed] [Google Scholar]
- 28. Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56:455–463, 2000. [DOI] [PubMed] [Google Scholar]
- 29. Aouad RK, Chiu AG. State of the art treatment of nasal polyposis. Am J Rhinol Allergy 25:291–298, 2011. [DOI] [PubMed] [Google Scholar]
- 30. Fokkens WJ, Lund VJ, Mullol J, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology 50:1–12, 2012. [DOI] [PubMed] [Google Scholar]
- 31. Bruni FM, De Luca G, Venturoli V, Boner AL. Intranasal corticosteroids and adrenal suppression. Neuroimmunomodulation 16:353–362, 2009. [DOI] [PubMed] [Google Scholar]