Abstract
Background:
Fistula-in-ano when complicated by Fournier's gangrene is an unusual finding and always carries high morbidity. This study details our experience in managing 10 cases.
Methods of Study:
Case files of all patients managed in University of Maiduguri Teaching Hospital and Federal Medical Center of Yola and Gombe from January, 2007 to December, 2011 were retrieved from Medical Record Departments and other Hospital Records. These were analyzed for demographic, clinical and pathological variables, the type of treatment and follow-up.
Results:
A total of 10 men with a mean age of 50.5 years (35-60) were managed in the period of study. Nearly, 50% of the patients were farmers, 30% businessmen and 20% were civil servant. 7 (70%) of these patients presented with Fournier's gangrene within 4 weeks of development of fistula-in-ano and the rest within 8 weeks. 4 (40%) of these patients had inadequate drainage of their perianal abscess and 2 (20%) had incision and drainage. Another 4 (40%) had spontaneously rupture of the perianal abscess. 6 (60%) of the fistula-in-ano was submuscular, 30% subcutaneous and 10% were complex or recurrent. Nearly, 20% of patients had fistulotomy and seton application for adequate drainage. Mucosal advancement flap was performed in 5 (50%) and fistulotomy in 3 (30%) patients. Another 30% had fistulotomy and continuing sitz bath.
Conclusion:
Cryptoglandular infection is an important cause of perianal abscesses and fistula-in-ano and if poorly managed results in Fournier's gangrene. Early broad spectrum parenteral antibiotic therapy and primary surgical treatment can prevent Fournier's gangrene.
KEYWORDS: Fistula-in-ano, Fournier's gangrene, perianal abscess
INTRODUCTION
Fistula-in-ano is an abnormal hollow tract lined by unhealthy granulation tissue connecting a primary opening in the anal canal to a secondary opening in the perianal skin.[1] The fistula tract may be single or multiple and may extend from the same primary opening. It is nearly always caused by a previous anorectal abscess, following either poor surgical or spontaneous drainage in the perianal skin. Men are involved in 70% of cases and the majority of cases present initially in the 3rd to the 6th decade, which incidentally coincide with the mean age occurrence of Fournier's gangrene.[1,2,3] Fournier's gangrene, which was first described by Jean Alfred Fournier in 1883, is an infective necrotizing fasciitis of the perineal, genital or perianal regions as a result of subcutaneous vascular thrombosis and resulting in gangrene of the overlying scrotal skin.[2,3] fistula-in-ano and Fournier's gangrene still continue to pose management challenges to surgeons. However, there has been no report on management of this concomitant occurrence of these diseases. This is a retrospective study of all fistulas-in-ano complicated by Fournier's gangrene managed in University of Maiduguri Teaching Hospital and Federal Medical Center Yola and Gombe within a period of 5 years (January 2007 to December 2011) highlighting the causal relationship.
METHODS OF STUDY
The case files of all patients with the diagnosis of fistula-in-ano complicated by Fournier's gangrene during the study period were retrieved from the Central Medical Records Department of these Hospitals. Additional information was obtained from the other hospital's records. Information retrieved includes the demographic data, mode of presentation, type of infecting organisms, co-morbidity illnesses, nature and outcome of treatment. Data analysis was carried out using the statistical package for the social sciences version 16 (SPSS 16) to determine the level of significance and correlations with the variables.
RESULTS
A total of 10 male patients who developed fistula-in-ano and then complicated by Fournier's gangrene with a mean age of 50.5 (50-59) years were managed within the period of 5 years [Table 1]. Nearly, 50% of patients were peasant farmers, 30% businessmen and 20% were civil servant. All patients presented with initial perianal pain, external opening and discharge and then followed by scrotal swelling and high grade fever [Table 2]. Nearly, 70% of these patients presented with Fournier's gangrene within 1-4 weeks of development of fistula-in-ano, which were preceded by perianal abscess and the rest within 8 weeks [Table 3]. 60% of the fistula-in-ano was submuscular (intersphincteric), 30% subcutaneous with straight anterior external opening and 10% were complex or recurrent running curved course from internal posterior to anterior external opening [Figure 1].
Table 1.
Age distribution of 10 patients with fistula-in-ano and Fournier's gangrene
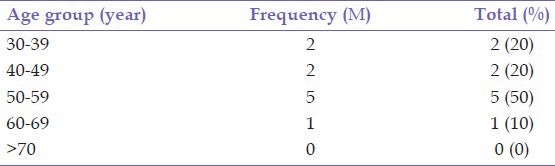
Table 2.
Major clinical features of 10 patients with fistula-in-ano and Fournier's gangrene
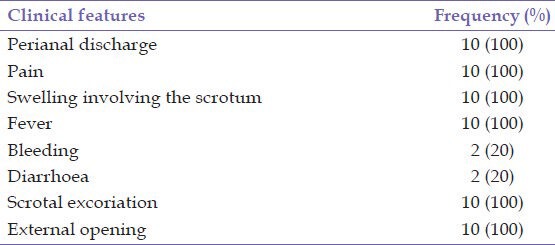
Table 3.
Duration of symptoms prior to presentation of 10 patients with fistula-in-ano and Fournier's gangrene

Figure 1.
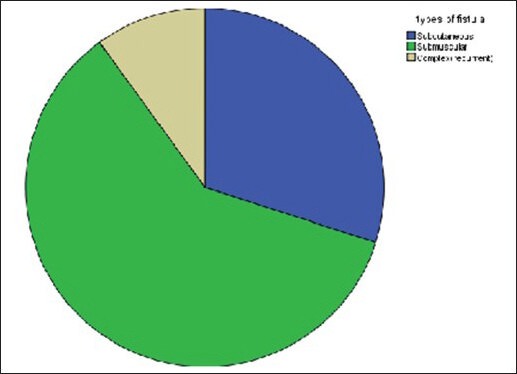
Types of fistula-in-ano with Fournier's gangrene at presentation of the 10 patients
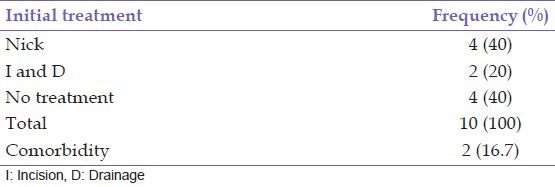
Nearly, 40% of these patients had initial nick for drainage of their perianal abscess and 20% incision and drainage (I and D), but 40% came with spontaneously ruptured perianal abscess, which developed fistula-in-ano and then Fournier's gangrene with no initial treatment [Table 4].
Table 4.
Types of treatment prior to presentation of 10 patients with fistula-in-ano and Fournier's gangrene
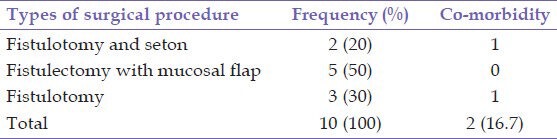
All patients were given adequate intravenous fluid and parenteral antibiotics before definitive treatment. The necrotic scrotal tissue and perianal region were debrided. 20% of patients had fistulotomy and seton (rubber band) application for adequate drainage. In 50% of patients mucosal advancement flap was done to close the internal opening of the fistula, but 30% had fistulotomy and sitz bath [Table 5].
Table 5.
Types of procedure and surgery for 10 patients with fistula-in-ano and Fournier's gangrene
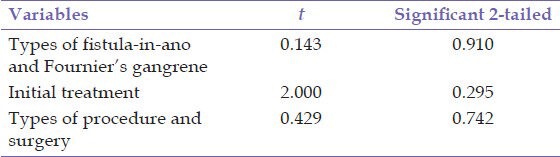
There is a significant relationship between initial treatments, type of fistula-in-ano, durations of the clinical features type of definitive surgical procedure carried out and the outcome [Table 6].
Table 6.
The paired t samples tests of association of durations and the clinical features with other variables
DISCUSSION
Fistula-in-ano commonly result from cryptoglandular fistula.[1,4] If the cryptoglandular abscess is either poorly drained or spontaneously ruptures through the perianal skin, then becomes fistula in 50% of patients.[5] Severe polymicrobial synergistic infection from the gut flora can cause an extensive subfascial tissue necrosis involving the scrotum, Fournier's gangrene [Figure 2], which is an unusual complication of fistula-in-ano. Other common causes of anal fistula include chronic ulcerative colitis, Crohn's disease, tuberculosis, carcinoma of the rectum or anal canal, benign rectal strictures, foreign bodies or diverticulitis.
Figure 2.

Cryptoglandular fistula with Fournier's gangrene
Fournier's gangrene, which was thought to be idiopathic by Jean Alfred Fournier (1883) is now known to have definite etiology and is characterized by obliterative endarteritis causing cutaneous and subcutaneous vascular thrombosis and tissue necrosis, then invaded by polymicrobial enterobacteria.[2] In our region, Staphylococcus and Proteus species are the commonest mixed growth infection and quinolones (ciprofloxacin and ofloxacin) are the most potent antibiotics in treating these infection.[6,7] Urogenital foci such as urethral stricture, indwelling urethral catheter, prostatic message and biopsy are the most common primary adjacent focus of Fournier's gangrene and in Africa immunosuppressive illnesses such as diabetes mellitus, human immunodeficiency virus infection, filarial infestations and low socio-economic status contributed to the high prevalence of the disease.[2,8] In these patients, 50% are in the low socio-economic category, however, 80% of them were otherwise healthy without immunosuppressive illnesses. Usually, Fournier's gangrene is presented in the acute form, but recently it runs an indolent course, which some studies[2,8] attributed it to immunosuppressive comorbidities; however in our series, it's probably due to suboptimal antibiotic therapy and delay in referral. These patients presented with high grade fever associated with rigors and sweating, some of them delirious. Nearly, 60% of the patients either had a perianal nick [Figure 3] or inadequate I and D [Figure 4] and 40% had a prior history of spontaneous rupture and discharge from a perianal abscess with worse clinical symptoms. 60% were submuscular (intersphincteric) fistular-in-ano.
Figure 3.

Nick of perianal abscess and Fournier's gangrene
Figure 4.

Inadequate perineal abscess drainage and Fournier's gangrene
The parks classification system divided fistula-in-ano resulting from cryptoglandular infections as intersphincteric, transsphincteric, suprasphincteric and extrasphincteric, however, the current procedural terminology codes classification include subcutaneous fistula resulting from unhealed anal fissure or anorectal procedures such as hemorrhoidectomy, submuscular fistula (intersphincteric, low transsphincteric) and complex fistular, recurrent (high transsphincteric, suprasphincteric and extrasphinteric, multiple tracts, recurrent).[4,9,10]
Majority of fistula-in-ano can be diagnosed based on clinical history and physical examination, however, in cases associated with multiple or complex problems such as a horse shoe abscesses or recurrent complex fistula-in-ano, rectal cancer or Crohn's disease, diagnostic imaging such as transrectal ultrasound, computed tomography scan or magnetic resonance imaging would be required.[11,12,13]
The parenteral antimicrobials ciprofloxacin and metronidazole were given based on the sensitivity pattern of the microbial pathogens in our region.[6,7] Some of the patients had extensive debridement from the perianal region up to the scrotum and groins leaving the testes bare [Figure 5]. Hypertonic saline soaking (sitz bath) and wound dressing were continued mornings and evenings until the wounds were cleaned and granulated in 2-4 months [Figures 6 and 7]. If patient presented early with cryptoglandular infection and perianal abscess, the abscess is immediately drained by either radial perianal incision or adequate cruciate incision with unroofing the abscess cavity.[4,10] These procedures allow adequate abscess drainage and are performed close to anal verge in order to allow fast healing. It is rare for fistula to heal spontaneously even with antibiotic therapy. In order to heal, the internal opening (crypt) should be obliterated and therefore operative procedure is necessary.[1,4,5,10] If the internal opening identified, the tract should be probed to clarify and a seton suture of silk passed through to serve as a drain until definitive treatment can be done. Nearly, 40% of these patients had a nick of the abscess cavity as primary treatment, which was inadequate I and D and 40% had spontaneous rupture of the abscess cavity. These made perineal spread of the infection rapid and thus prolonged period of patient's management and increased risk of mortality.[2,3,8] Although 20% of the patients had adequate I and D, but yet developed a complication of Fournier's gangrene, probably would have benefited from closure of the internal opening as part of primary treatment.
Figure 5.

Extensive perineal and scrotal debridement with bare testes
Figure 6.

Cleaned granulated scrotal and perineal wound ready for grafting
Figure 7.

Healing anal fistula and scrotal wound with continuing sitz bath
The operative goals for subcutaneous and submuscular fistulae are to open the tract and remove tract lining either by curettage or electrocautery. The complex or recurrent fistulae may be treated by either non-cutting setons, fibrin glue, ablation, rectal mucosal advancement flap, anal fistula plugs or combination of these in order to avoid sphincter muscle division and its attendant fecal incontinence complication.[14,15,16,17] Fistulotomy is a preferred procedure for subcutaneous and submuscular fistulae whether complicated or not and has 3-5% risk of flatus and stool leakage and with more muscle cutting fecal incontinence may develop.[1,4,10] If the sphincter muscle is traversed by the tract seton suture is applied.[15,16,17] 30% of these patients had fistulotomy alone and 20% with seton silk suture application. 50% of these patients had fistulectomy and advancement rectal mucosal flap. The fibrin glues and plugs are not readily available in our center. Majority of the patients had their scrotal wounds healed spontaneously with continuing sitz bath [Figure 7], but those with more extensive perineal wound had mesh skin grafting [Figure 8]. Patients were followed-up over a year with no history of fecal incontinence or fistula recurrence.
Figure 8.

Mesh graft of the perineal and scrotal wound
CONCLUSION
Cryptoglandular infection is an important cause of perianal abscess and fistula-in-ano when poorly managed can lead to Fournier's gangrene, which is a urological emergency. Early adequate parenteral antibiotic therapy, primary surgical treatment including closure of internal opening (crypt) can prevent serious complications like Fournier's gangrene.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Hughes E, Cuthberston AM, Killinback MK. Colorectal Surgery. 1st ed. Medical Division of Longman Group Limited, Robert Stevenson House, 1 – 3 Baxter's place, Leith Walk, Edinburgh EH1 3AF: Publisher Churchill Livingstone; 1983. Anorectal suppuration II, anal fistula; pp. 142–62. [Google Scholar]
- 2.Smith GL, Bunker CB, Dinneen MD. Fournier's gangrene. Br J Urol. 1998;81:347–55. doi: 10.1046/j.1464-410x.1998.00532.x. [DOI] [PubMed] [Google Scholar]
- 3.Laucks SS., 2nd Fournier's gangrene. Surg Clin North Am. 1994;74:1339–52. doi: 10.1016/s0039-6109(16)46485-6. [DOI] [PubMed] [Google Scholar]
- 4.Bleier JI, Moloo H. Current management of cryptoglandular fistula-in-ano. World J Gastroenterol. 2011;17:3286–91. doi: 10.3748/wjg.v17.i28.3286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hämäläinen KP, Sainio AP. Incidence of fistulas after drainage of acute anorectal abscesses. Dis Colon Rectum. 1998;41:1357–61. doi: 10.1007/BF02237048. [DOI] [PubMed] [Google Scholar]
- 6.Gadzama GB, Zailani SB, Abubakar D, Bakari AA. Bacterial pathogens associated with wound infections at the University of Maiduguri Teaching Hospital, Maiduguri, Nigeria. Kanem J Med Sci. 2007;1:26–8. [Google Scholar]
- 7.Zailani SB, Gadzama GB, Abubakar D, Yusuph H, Bakari AA. In vitro antimicrobial susceptibility pattern of bacterial isolates from infected wounds at a tertiary hospital. Borno Med J. 2006;3:28–31. [Google Scholar]
- 8.Saleh E, Wail K, Mohammed A, Elham R, Mohammed F. Fournier's gangrene: Clinical, biochemical, bacteriologic, immunologic study and treatment outcome. Egypt J Surg. 2007;26:63–9. [Google Scholar]
- 9.Parks AG, Gordon PH, Hardcastle JD. A classification of fistula-in-ano. Br J Surg. 1976;63:1–12. doi: 10.1002/bjs.1800630102. [DOI] [PubMed] [Google Scholar]
- 10.Tabry H, Farrands PA. Update on anal fistulae: Surgical perspectives for the gastroenterologist. Can J Gastroenterol. 2011;25:675–80. doi: 10.1155/2011/931316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun MR, Smith MP, Kane RA. Current techniques in imaging of fistula in ano: Three-dimensional endoanal ultrasound and magnetic resonance imaging. Semin Ultrasound CT MR. 2008;29:454–71. doi: 10.1053/j.sult.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 12.Buchanan GN, Halligan S, Williams AB, Cohen CR, Tarroni D, Phillips RK, et al. Magnetic resonance imaging for primary fistula in ano. Br J Surg. 2003;90:877–81. doi: 10.1002/bjs.4125. [DOI] [PubMed] [Google Scholar]
- 13.Sangwan YP, Rosen L, Riether RD, Stasik JJ, Sheets JA, Khubchandani IT. Is simple fistula-in-ano simple? Dis Colon Rectum. 1994;37:885–9. doi: 10.1007/BF02052593. [DOI] [PubMed] [Google Scholar]
- 14.Abbas MA, Lemus-Rangel R, Hamadani A. Long-term outcome of endorectal advancement flap for complex anorectal fistulae. Am Surg. 2008;74:921–4. [PubMed] [Google Scholar]
- 15.McCourtney JS, Finlay IG. Setons in the surgical management of fistula in ano. Br J Surg. 1995;82:448–52. doi: 10.1002/bjs.1800820406. [DOI] [PubMed] [Google Scholar]
- 16.Memon AA, Murtaza G, Azami R, Zafar H, Chawla T, Laghari AA. Treatment of complex fistula in ano with cable-tie seton: A prospective case series. ISRN Surg 2011. 2011 doi: 10.5402/2011/636952. 636952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chung W, Kazemi P, Ko D, Sun C, Brown CJ, Raval M, et al. Anal fistula plug and fibrin glue versus conventional treatment in repair of complex anal fistulas. Am J Surg. 2009;197:604–8. doi: 10.1016/j.amjsurg.2008.12.013. [DOI] [PubMed] [Google Scholar]


