Abstract
Rupture of hepatocellular carcinoma (HCC) is not uncommon and most ruptured HCC present with hemoperitoneum and hemorrhagic shock. Management of ruptured HCC is different than non-ruptured one. Short- and long-term mortality increases following rupture of HCC with increasing chances of tumor dissemination. We describe a case with non-bleeding spontaneous rupture of HCC. A 62-year-old male patient was admitted to our institute hospital with mild to moderate pain in the right upper part of the abdomen. He lost appetite and weight. Ultrasonography of the abdomen was performed and it suggested HCC and ascites. Triple phase computer tomography revealed HCC in segments 6 and 7 of liver with typical radiological characteristics. Portal vein was thrombosed. No extravasation of dye was seen. Ruptured of tumor through liver capsule was seen with necrosis and hemorrhage in the center of the tumor. Non-bleeding ruptured HCC has not been reported in the literature to the best of our knowledge. We herein describe this rare case.
KEYWORDS: Hepatocellular carcinoma, hemoperitoneum, spontaneous rupture
INTRODUCTION
Hepatocellular carcinoma (HCC) is the most common primary malignant tumor of the liver. Spontaneous rupture with potentially fatal hemoperitoneum occurs in 3-15% patients.[1] Pre-disposing factors for HCC rupture are subcapsular location, large tumor, portal hypertension, tumor necrosis, local increase of venous pressure owing to the outflow reduction caused by neoplastic invasion.[2] Survival of ruptured HCC is worse than non-ruptured one. Following rupture, tumor cell disseminate through coelomic cavity and is the reason for poor outcome. Multidisciplinary management with transarterial chemoembolization (TACE) and surgery in selected patients would improve the short-term survival of rupture HCC.
CASE REPORT
A 62-year-old non-diabetic, non-alcoholic male patient attended to our out-patient department with the complaint of dull aching pain in the right upper part of the abdomen. He was suffering from such pain since last 1 month. Pain responded to analgesic. He lost around 3 kg weight in last 1 month. He lost appetite also.
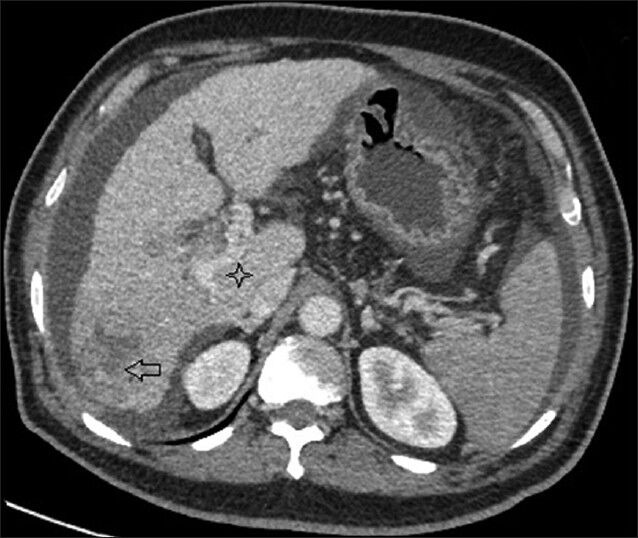
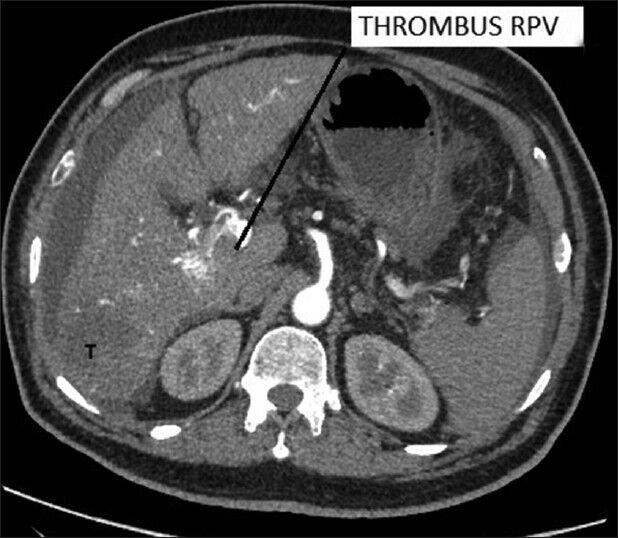
Abdominal ultrasonography was performed, which suggested HCC with ascites. Triple phase contrast enhanced computer tomography (CECT scan) revealed HCC of 12 cm × 15 cm size in segments 6 and 7 of liver [Figure 1]. Computer tomography also showed typical radiological characteristics of HCC (arterial enhancement of liver mass and wash out on delayed phase, arterioportal shunt [Figures 1–3], portal vein thrombosis). There was gross ascites. No extravasation of dye seen. Ruptured tumor through liver capsule [Figure 4] was seen with necrosis and hemorrhage in the center of the tumor.
Figure 1.
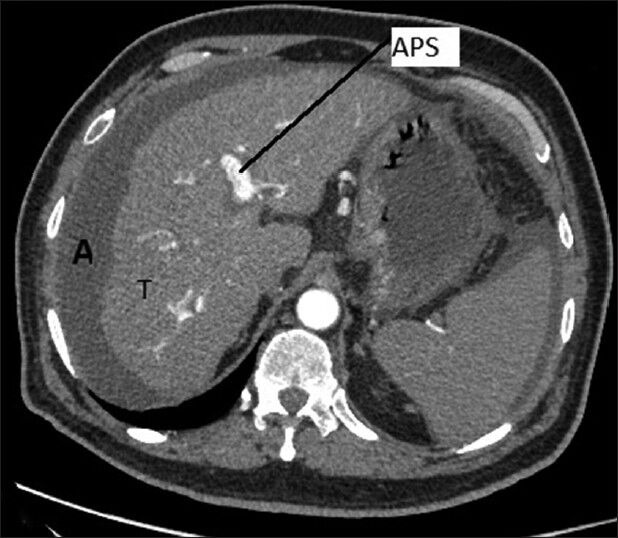
Arterial phase of triple phase contrast enhanced computer tomography revealed mass lesion of 12 cm × 15 cm size in segments 6 and 7 of liver. tumor enhancement (T) in arterial phase and portal vein is visible on arterial phase (arterioportal shunt) and ascites (A)
Figure 3.
Contrast enhanced computer tomography (portal venous phase) on cross section showing wash out of contrast from tumor (arrow) and thrombus in right portal vein (star mark)
Figure 4.
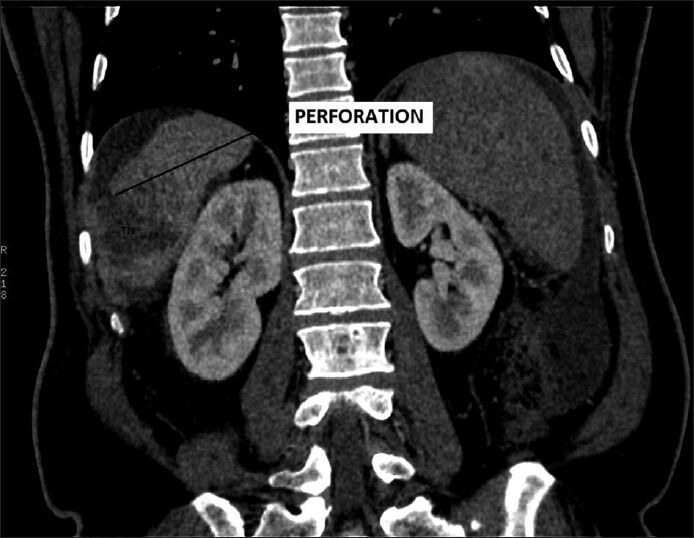
Contrast enhanced computer tomography on coronal section showing rupture of the tumor through liver capsule and hemorrhage and necrosis (TN) noted inside the tumor
Figure 2.
Contrast enhanced computer tomography (arterial phase) on cross section showing tumor (T) enhancement and right portal vein visible with thrombus in it
Patient was admitted for evaluation. His blood pressure and heart rate was normal. Peritoneal tapping was performed for ascetic fluid analysis. Ascetic fluid was clear, exudative in nature with serum to ascetic fluid albumin gradient less than 1.1. Cytological examination ascetic fluid revealed no tumor cell.
On evaluation for chronic liver disease, all viral markers were negative. Upper gastrointestinal endoscopy showed non-bleeding grade II esophageal varices. On biochemical analysis of blood total and direct bilirubins were 1.98 and 0.48 respectively. Liver enzymes were raised (Aspartate transaminase-51 IU/ml and alanine amino transferase -55 IU/ml) with normal total protein and albumin. His hemoglobin was 12.4 g% and cell counts were normal. Alpha fetoprotein was high (424 ng/ml; normal range 0-8.5) and carcinoembryonic antigen was normal.
The disease was in advanced staged to be cured by surgery and portal vein thrombosis excluded TACE from treatment options; therefore, transarterial radioembolization was offered, but patient refused it.
LITERATURE REVIEW
Incidence of HCC parallels the incidence viral hepatitis B or C and more common in Asia and Africa than developed countries.[3] Most rupture of HCC presented with intraperitoneal hemorrhage and shock and patient required emergency treatment.[1] With screening health-care early detection of HCC is increasing and the incidence of ruptured HCC is decreasing. The modern imaging studies improved the rate of pre-operative diagnosis of HCC better planning of the treatment. However, 20-33% of the diagnosis of ruptured tumor is made only during an emergency exploratory laparotomy.[4] Mortality rate of ruptured of bleeding HCC in the acute phase is high (25-75%). Liver failure occurs usually during the acute phase of tumor rupture in 12-42% of patients.[1]
Large and peripherally located tumors are more prone to rupture. Mechanism of rupture of HCC is not exactly known. Hypotheses include rapid growth of the tumor and necrosis, rupture by splitting the overlying non-tumorous liver parenchyma or erosion of a vessel, increased intra-tumor pressure with the occlusion of hepatic veins by tumor thrombi or invasion and coagulopathy.[5] Degeneration of elastin and degradation of type IV collagen render the blood vessels stiff and weak. this vascular dysfunction causing them to split easily when the vascular load increases from hypertension or minor trauma is another hypothesis for of HCC ruptures.[6]
Abdominal pain is the only independent factor relating to rupture of HCC.[7] Doppler ultrasound and computer tomography (CT) scan are useful to exclude of hemoperitoneum and evaluation of tumor. Though CT scan can demonstrate the patency of the portal vein, but it rarely can identify the site of active bleeding.[1] Conventional angiography demonstrates extravasations of contrast from the tumor only in 13% to 35% of cases.[8]
Surgery is the only option of cure of HCC. However long-term survival seems to be unanimously correlated to the stage of the disease, its local spread after rupture and to the residual hepatic reserve.[9] Transarterial embolization is an effective and well-tolerated treatment for the emergency management of hemoperitoneum following rupture of HCC.[2] Liver resection in the setting of non-bleeding HCC rupture has not reported. After the surgical treatment of HCC intraperitoneal dissemination during rupture decrease the long-term survivability.[1]
There is some evidence for a favorable outcome after surgical resection of ruptured HCC presented with hemoperitoneum. Patient presenting with ruptured HCC and hemoperitoneum need immediate medical attention and as the duration between rupture and treatment in such cases is short, so chances of dissemination is low. However, the scenario is different in non-bleeding ruptured HCC as in such case patient usually presents late and duration between rupture and treatment is long, so more chance of dissemination. Further study is needed for recommendation of treatment of such cases.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Lai EC, Lau WY. Spontaneous rupture of hepatocellular carcinoma: A systematic review. Arch Surg. 2006;141:191–8. doi: 10.1001/archsurg.141.2.191. [DOI] [PubMed] [Google Scholar]
- 2.Castells L, Moreiras M, Quiroga S, Alvarez-Castells A, Segarra A, Esteban R, et al. Hemoperitoneum as a first manifestation of hepatocellular carcinoma in western patients with liver cirrhosis: Effectiveness of emergency treatment with transcatheter arterial embolization. Dig Dis Sci. 2001;46:555–62. doi: 10.1023/a:1005699132142. [DOI] [PubMed] [Google Scholar]
- 3.Chedid AD, Klein PW, Tiburi MF, Villwock MM, Bassani LE, Chedid MF. Spontaneous rupture of hepatocellular carcinoma with haemoperitoneum: A rare condition in Western countries. HPB (Oxford) 2001;3:227–30. doi: 10.1080/136518201753242262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vergara V, Muratore A, Bouzari H, Polastri R, Ferrero A, Galatola G, et al. Spontaneous rupture of hepatocelluar carcinoma: Surgical resection and long-term survival. Eur J Surg Oncol. 2000;26:770–2. doi: 10.1053/ejso.2000.1001. [DOI] [PubMed] [Google Scholar]
- 5.Ong GB, Chu EP, Yu FY, Lee TC. Spontaneous rupture of hepatocellular carcinoma. Br J Surg. 1965;52:123–9. doi: 10.1002/bjs.1800520210. [DOI] [PubMed] [Google Scholar]
- 6.Zhu LX, Geng XP, Fan ST. Spontaneous rupture of hepatocellular carcinoma and vascular injury. Arch Surg. 2001;136:682–7. doi: 10.1001/archsurg.136.6.682. [DOI] [PubMed] [Google Scholar]
- 7.Yeh CN, Lee WC, Jeng LB, Chen MF, Yu MC. Spontaneous tumour rupture and prognosis in patients with hepatocellular carcinoma. Br J Surg. 2002;89:1125–9. doi: 10.1046/j.1365-2168.2002.02188.x. [DOI] [PubMed] [Google Scholar]
- 8.Ngan H, Tso WK, Lai CL, Fan ST. The role of hepatic arterial embolization in the treatment of spontaneous rupture of hepatocellular carcinoma. Clin Radiol. 1998;53:338–41. doi: 10.1016/s0009-9260(98)80004-4. [DOI] [PubMed] [Google Scholar]
- 9.Rossetto A, Adani GL, Risaliti A, Baccarani U, Bresadola V, Lorenzin D, et al. Combined approach for spontaneous rupture of hepatocellular carcinoma. World J Hepatol. 2010;2:49–51. doi: 10.4254/wjh.v2.i1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]


