Abstract
Purpose
To describe the efficacy of episcleral brachytherapy in a choroidal melanoma and circumscribed hemangioma arising in both eyes of the same patient.
Case report
We present the case of a 47 year old man who presented decreased visual acuity a few months preceding initial consult. On fundoscopy, he presented a melanotic lesion in the right eye, and a red-orange choroidal mass in the macular area of the left eye.
Material and methods
B scan-ultrasound, fluorescein, and indocyanine green angiography, confirmed the diagnosis of choroidal melanoma in the right eye, and circumscribed choroidal hemangioma in the left eye. Episcleral brachytherapy with 125I was performed in both eyes consecutively.
Results and Conclusions
Bilateral episcleral brachytherapy successfully treated both tumors, preserving the eyes and useful visual function.
Keywords: intraocular tumors, choroidal melanoma, circumscribed choroidal hemangioma, episcleral brachytherapy
Purpose
Choroidal melanoma is the most common primary adult ocular malignancy, with an estimate incidence in the United States of approximately 5 cases per million inhabitants per year [1], with no clear data about its incidence in Europe. Historically, the disease treatment was based on enucleation. However, in the last decades, conservative techniques have been developed demonstrating efficient tumor control. Brachytherapy [2, 3] is the most widely used treatment for small and medium choroidal melanomas, and enucleation nowadays is reserved for an end stage disease, mainly large tumors with poor visual function [4–6].
Circumscribed choroidal hemangioma is a rare benign hamartous vascular tumor. Its incidence is not well known. With respect to the choroidal melanoma, the frequency is said to be 1 out of 15 [7]. They are usually asymptomatic and only when exudation produces retinal edema, and exudative retinal detachment leading to decrease visual acuity, they are diagnosed and treated to prevent the total loss of vision, and the eye itself [8]. Different forms of laser have been applied with a transient effect and recurrence of exudation, but the definitive treatments are based on different forms of external radiation therapy, including external and episcleral brachytherapy [9, 10]. We present a case of simultaneous choroidal melanoma and circumscribed choroidal hemangioma in the same patient, treated consecutively with 125I brachytherapy.
Case report
At the time of diagnosis, the 47 year old male patient had a 5 month history of visual loss in his right eye (OD). The best corrected visual acuity in that eye was 20/60 and less than 20/200 in left eye (OS). Fundus examination revealed a melanotic lesion in superior temporal arcade in OD, and a red-orange choroidal mass in macular area in OS, with inferior exudative retinal detachment (Fig. 1). B scan-ultrasound of OD revealed a nodular choroidal mass 8.5 mm in basal diameter and 2.7 mm of height, with choroidal excavation and kappa angle, suggestive of melanoma. The left eye showed a choroidal nodular mass with high reflectivity, 12.9 mm in basal diameter, and 4.7 mm of height, consistent with hemangioma, with associated retinal detachment. Fluorescein and indocyanine green angiography supported the diagnosis of choroidal melanoma in OD, and circumscribed choroidal hemangioma with exudative retinal detachment in OS. Adjuvant studies (orbital computed tomography scan, nuclear magnetic resonance, liver function test, hepatic scan-ultrasound) proved that there were not extraocular or systemic extensions. Episcleral brachytherapy with 125I was performed with ROPES plaque of 11 mm [11] consecutively in both eyes (Fig. 2). Dose-rate distributions were obtained by the Plaque Simulator BEBIG v 3.56® (GmbH, Berlin, Germany). Treatment duration was calculated using an excel spreadsheet assuming dosimetric contants and functions of the AAPM TG-43 (American Association of Physicists in Medicine Task Group) protocol. The source model used was the 6711, supplied by Amersham Healthcare. The characteristics of the two treatments are detailed in Table 1. After surgical exposure of the scleral surface over the tumor base, transpupillary illumination was used drawing the tumor base. A dummy plaque was sutured, to assure the correct plaque location and margin. Then the definitive radioactive plaque was positioned and the sutures tied. Brachytherapy was performed first on the left eye (choroidal hemangioma) delivering 45 Gy, and 2 weeks later on the right (melanoma), delivering 95 Gy. Between the two treatments cleaning and sterilization of the applicator and sources were performed according to the procedure in the hospital. Both tumors regressed, and retinal detachment disappeared.
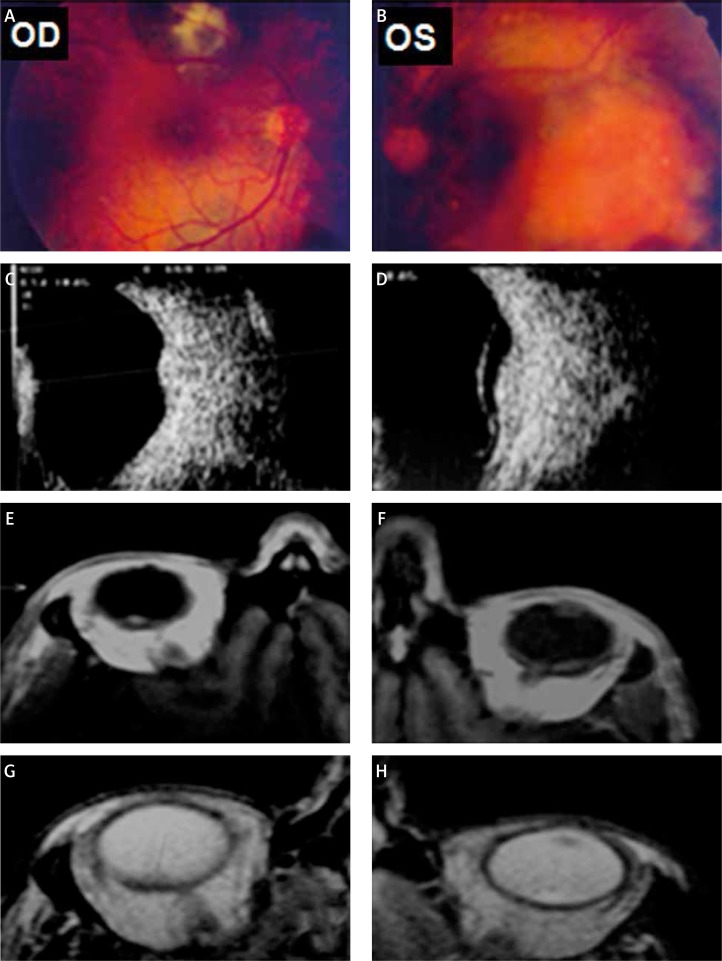
Fig. 1.
Before epiescleral brachytherapy with 125I treatment. Fundus photography of right eye (OD) reveales a melanotic lesion in superior temporal arcade (A), showed as a nodular choroidal mass in B scan-ultrasound (C). Nuclear Magnetic Resonance studies (NMR) of the orbit shows a well-defined mass, hiperintense on T1 (E), and hipointense on T2 (G), without contrast enhancement. Left eye (OS) fundus shows a red-orange choroidal mass in macular area (B), with inferior exudative retinal detachment (D), isointense on NMR-T1 (F), and hiperintense on T2 (H), with high contrast enhancement
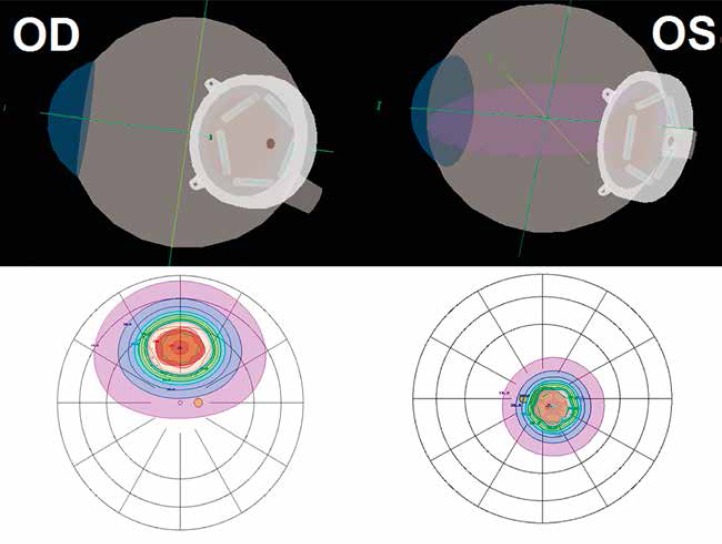
Fig. 2.
Retinal diagram with dose distribution of episcleral brachytherapy with 125I (ROPES plaque of 11 mm) in both eyes
Table 1.
Treatment characteristics
| Circumscribed hemangioma | Choroidal melanoma | |
|---|---|---|
| Prescription point on the central axis (mm) | 4.40 | 4.22 |
| Treatment length (hours) | 71.25 | 190.08 |
| Individual source strength at implant (U) | 4.468 | 3.617 |
| Individual source strength at implant (mCi) | 3.51 | 2.848 |
| Total source strength at implant (U) | 22.34 | 18.08 |
| Total source strength at implant (mCi) | 17.59 | 14.24 |
| Sources number | 5 | 5 |
| Eye | OS | OD |
After twelve years of follow-up, there has not been a tumor recurrence (Fig. 3). Nine years after treatment, a post irradiation cataract appeared in the left eye, and macular edema and hemorrhages in posterior pole of the right eye. The cataract was extracted on the left eye, and visual acuity was recovered up to 20/200. An Anti Vascular Endothelial Growth Factor agent (Avastin®) was injected three times in right eye (every three months), with resolution of the hemorrhages, but still with persistence of slight macular edema on Optical Coherence Tomography examination with recovery and stabilization of the visual acuity up to 20/60 up to last examination.
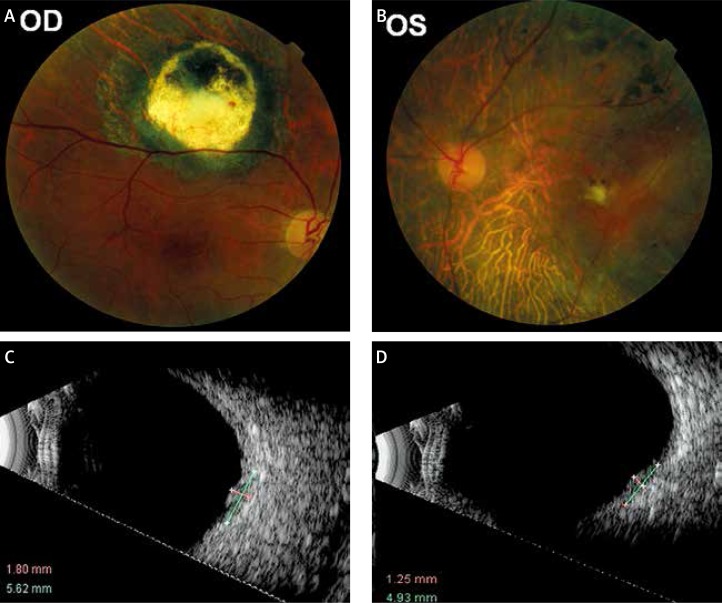
Fig. 3.
Twelve years after epiescleral brachytherapy with 125I. Choroidal melanoma regressed in fundus examination (A), and in B scan-ultrasound (C) of right eye (OD). Circumscribed hemangioma (B) and retinal detachment also disappeared (D) in left eye (OS)
Discussion
Choroidal melanoma is the most common primary intraocular tumor in adults, and circumscribed choroidal hemangioma is a rare clinical entity. Is it not known if there is any association between either tumors, and it is a rare coincidence to find them in the same subject, resulting in bilateral reduced visual function in the patient. Our case involves a young patient with simultaneous tumors in both eyes, and because of this, it was considered a priority to apply local conservative treatment to preserve his eyes, and to retain visual function. In choroidal melanomas, conservative treatment with plaque radiotherapy has proved to be efficient to control local tumors with overall survival comparable to enucleation [5, 6]. These patients may have visual loss secondary to radiation retinopathy, a condition that may result from the exposure to radiation [12], and may be considered a bad prognostic factor, due to high radiation doses to the foveola [13]. Although our patient received a high radiation dose on the posterior pole, he had a well-preserved visual function, after twelve years of following-up. Treatment of choroidal hemangioma is based upon tumor location, the presence of subretinal fluid, symptoms and potential for visual recovery. Because of the large size of the choroidal hemangioma in our patient, we could not use a less aggressive treatment. Epiescleral brachyterapy was an option for treatment, which has been reported to offer excellent results in large tumors [9, 10, 14]. Because of the subfoveal location of the tumor, the patient had some loss of vision in the eye with choroidal hemangioma, upon diagnosis. We used a low dose of radiation, which had lesser risk of complications, and after cataract extraction, the visual acuity of the patient was preserved. Choroidal melanoma has been associated with different systemic or ocular findings, but an association between choroidal melanoma and choroidal hemangioma has never been published.
Conclusions
To our knowledge, this is the first reported case of simultaneous choroidal melanoma and circumscribed choroidal hemangioma in the same patient, treated successfully with 125I brachytherapy, achieving tumor control and preservation of useful visual function in both eyes, for 12 years.
Disclosure
Authors report no conflict of interest.
References
- 1.Singh AD, Turell ME, Topham AK. Uveal melanoma: trends in incidence, treatment, and survival. Ophthalmology. 2011;118:1881–1885. doi: 10.1016/j.ophtha.2011.01.040. [DOI] [PubMed] [Google Scholar]
- 2.Astrahan MA. The retina dose-area histogram: a metric for quantitatively comparing rival eye plaque treatment options. J Contemp Brachytherapy. 2013;5:23–32. doi: 10.5114/jcb.2013.34450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gagne NL, Cutright DR, Rivard MJ. Keeping an eye on the ring: COMS plaque loading optimization for improved dose conformity and homogeneity. J Contemp Brachytherapy. 2012;4:165–175. doi: 10.5114/jcb.2012.30683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aziz S, Taylor A, McConnachie A, et al. Proton beam radiotherapy in the management of uveal melanoma: Clinical experience in Scotland. Clin Ophthalmol. 2009;3:49–55. [PMC free article] [PubMed] [Google Scholar]
- 5.García-Alvarez C, Muiños Y, Saornil MA, et al. Ocular retention in patients with uveal melanoma managed by a multimodality approach. Arch Soc Esp Oftalmol. 2009;84:145–149. doi: 10.4321/s0365-66912009000300007. [DOI] [PubMed] [Google Scholar]
- 6.Margo CE. The Collaborative Ocular Melanoma Study: an overview. Cancer Control. 2004;11:304–309. doi: 10.1177/107327480401100504. [DOI] [PubMed] [Google Scholar]
- 7.Toledo Y, Rúa R, Pérez M. Therapeutic modalities for circumscribed choroidal hemangioma. Rev Cubana Oftalmol. 2010;23:590–607. [Google Scholar]
- 8.Mashayekhi A, Shields CL. Circumscribed choroidal hemangioma. Curr Opin Ophthalmol. 2003;14:142–149. doi: 10.1097/00055735-200306000-00006. [DOI] [PubMed] [Google Scholar]
- 9.López-Caballero C, Saornil MA, De Frutos J, et al. High-dose iodine-125 episcleral brachytherapy for circumscribed choroidal haemangioma. Br J Ophthalmol. 2010;94:470–473. doi: 10.1136/bjo.2009.160184. [DOI] [PubMed] [Google Scholar]
- 10.Andonegui J, Pérez de Arcelus M, Jiménez-Lasanta L. Treatment with photodynamic therapy of circumscribed choroidal hemangioma. Arch Soc Esp Oftalmol. 2010;85:337–340. doi: 10.1016/j.oftal.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 11.Granero D, Pérez-Calatayud J, Ballester F, et al. Dosimetric study of the 15 mm ROPES eye plaque. Med Phys. 2004;31:3330–3336. doi: 10.1118/1.1812605. [DOI] [PubMed] [Google Scholar]
- 12.Giuliari GP, Sadaka A, Hinkle DM, et al. Current treatments for radiation retinopathy. Acta Oncol. 2011;50:6–13. doi: 10.3109/0284186X.2010.500299. [DOI] [PubMed] [Google Scholar]
- 13.Melia BM, Abramson DH, Albert DM, et al. Collaborative Ocular Melanoma Study Group. Collaborative ocular melanoma study (COMS) randomized trial of I-125 brachytherapy for medium choroidal melanoma. I. Visual acuity after 3 years. COMS report no. 16. Ophthalmology. 2001;108:348–366. doi: 10.1016/s0161-6420(00)00526-1. [DOI] [PubMed] [Google Scholar]
- 14.Blasi MA, Tiberti AC, Scupola A, et al. Photodynamic therapy with verteporfin for symptomatic circumscribed choroidal hemangioma: five-year outcomes. Ophthalmology. 2010;117:1630–1637. doi: 10.1016/j.ophtha.2009.12.033. [DOI] [PubMed] [Google Scholar]