Abstract
Objectives
To determine current evidence-based medicine skills and practice among trainees.
Design
Questionnaire study.
Setting
Electronic survey was sent to all obstetrics and gynaecology trainees in East Midlands South Deanery, and responses collected were anonymous.
Participants
All obstetrics and gynaecology trainees in East Midland South Deanery.
Main outcome measures
Self-reported attitude, skills and knowledge in various components of evidence-based medicine.
Results
69 trainees were included in the study of which 35 responded. Among all respondents, almost 72% of trainees use non-evidence-based methods to find answers for their clinical questions, whereas only 18% use appropriate evidence-based medicine practice for such queries. Just 35% of trainees have minimum skills of literature searching. Most of the trainees struggle to understand various components of evidence-based medicine. Nearly 80% of trainees do not have formal education or training with regard to evidence-based medicine.
Conclusions
This study highlights the inadequacy of evidence-based medicine skills among trainees and urges that evidence-based medicine be incorporated in formal training along with specialty study modules.
Keywords: evidence-based medicine, obstetrics and gynaecology, medical education
Background
Questions arise but they do not always get followed up. Most of the trainees use the earliest method to find answers to these clinical questions. The answers are not necessarily evidence based. There is a discrepancy between the amount of research evidence that exists and the use of this evidence within clinical healthcare practice.1 As a consequence, patients might receive suboptimal treatment. They may not get the right answers to their questions. There are various reasons why the best evidence in clinical practice is not always used. The most important reason quoted is time constraints and workload for junior doctors. The knowledge and skills needed for the practice of evidence-based medicine (EBM) are often taught through courses and workshops in classrooms away from daily clinical practice. When this was compared with clinically integrated teaching in EBM, standalone teaching improved knowledge but not skills, attitudes or behaviour, whereas clinically integrated teaching improved knowledge, skills, attitudes and behaviour.2 The study showed, although there is familiarity with the most of EBM-related concepts, there is poor correlation with actual knowledge of EBM. Further educational initiatives should be undertaken to address methods in which EBM skills are reinforced among the trainees.3 There are several barriers to incorporate formal EBM training during clinical practice. These barriers are lack of teaching time due to work load, lack of EBM competency requirements in formal curriculum and hierarchical nature of the medical profession. Teaching EBM in clinical settings is most successful where EBM principles are culturally embedded and form part of everyday clinical practice.4 This study aimed to determine the existing knowledge, skills, attitude and behaviour with regard to practising EBM among obstetrics and gynaecology trainees. This will help to devise a plan to improve EBM skills among the trainees. Obstetrics and gynaecology training is hospital-based seven-year run-through specialty training. It provides good opportunity to train the junior doctors in this specialty with the skills required to practice EBM in daily clinical duties. Hence, we chose to assess skills in one specialty to avoid bias because of differences in training programme and structure.
Method
The survey questionnaire was sent to all obstetrics and gynaecology trainees working in different teaching hospitals attached to East Midland Workforce Deanery (South), UK. The survey was sent using an electronic web-based survey tool. The questions aimed to examine skills, knowledge and attitude regarding different components of EBM and teaching on this subject. The scale used was 1–10 from least to best levels of skills. The responses were collected and analysed anonymously. Responses were based on self-reported reflection of their practice. Reflective learning is the most effective way of adult learning.
Results
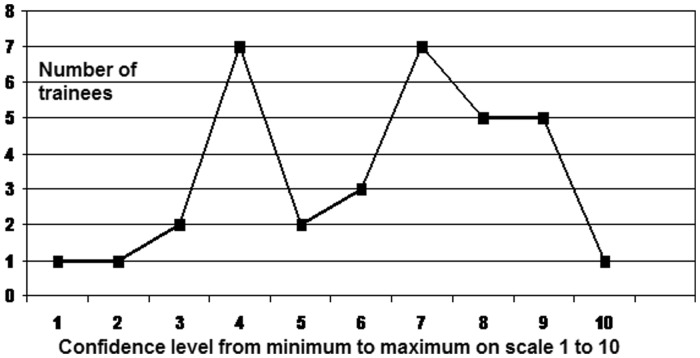
69 trainees were included in the study of which 35 responded. The response rate was 51%. In a typical week, the largest group of trainees (40%) face one to two clinical questions asked by consultants, colleagues or patients to which they do not know the exact answer. 24% of trainees face three to four such questions per week (Figure 1). This suggests trainees face many clinical questions every week, of which they do not know the answers. The next survey question was about the preferred method of answering such questions. To our surprise, the most preferred ways to find such answers are either to ask seniors or to use internet search engines like Google. 35% of trainees ask their seniors, whereas 24% use the search engines Google or Bing. 18% go with PubMed and similar scientific databases. Thus, only 18% use evidence-based methods to answer such questions. We recognize the fact that these search engines may guide to evidence-based articles; however, the normal tendency is to use material from top few search results and top results may not necessarily be high-quality evidence. Most of the trainees do not read journals frequently and hence they are not aware of ongoing research. 21% of trainees do not read the journals at all to find such answers, 58% of people do use journal articles one to three times a month and 9% read journals more often (4–6 times) a month.
Figure 1.
Number of questions faced by trainees per week.
Literature search is a vital skill of EBM; 75% of trainees feel confident about basic literature search, but most of them are not confident using advanced literature search skills, using MeSH terms, combing searches and having a clear search strategy. 35% of trainees feel that their advanced literature search skills rate a bare minimum (0–3 on scale).
There is evidence of inadequate skills to understand the design and limitation of any study. The majority of trainees have barely moderate confidence with regard to understanding the study design and study limitations. The confidence level shows peak at level 3 and 7 on scale of 1–10 where 1 denotes minimum level and 10 is maximum level of confidence. Few trainees are very confident and hence first peak is at level 3. The bimodal presentation is due to a mix of senior and junior trainees who participated in the survey.
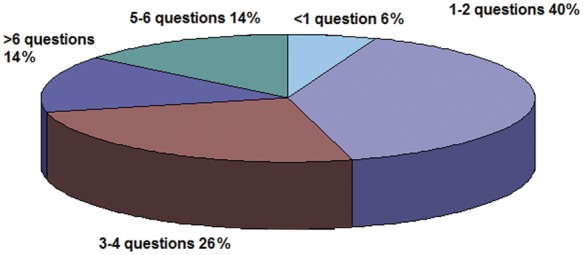
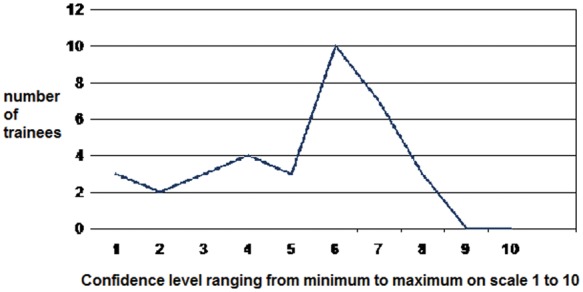
Trainees do not feel very confident about making sense of statistics used in a sample paper (Figure 2). The level of statistical knowledge required to read the paper is minimum to moderate. This suggests most of them struggle to understand the statistics used in the paper and obviously that affects the critical appraisal process. The trainees feel less confident to moderately confident while critically appraising a journal article (Figure 3). The presentation is bimodal as junior trainees feel less confident whereas senior trainees feel moderately confident.
Figure 2.
Reading statistics.
Figure 3.
Critical appraisal of a journal article.
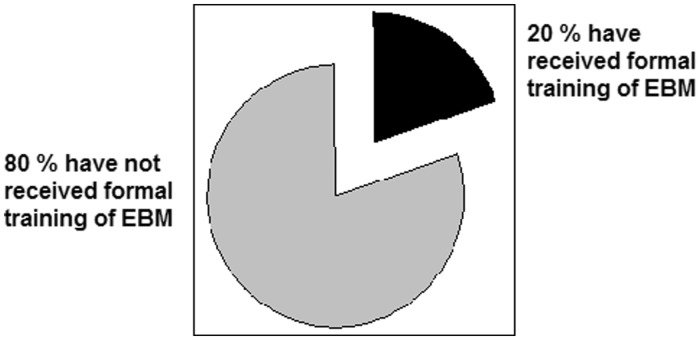
When we asked about formal training or teaching on EBM, 80% did not have any formal teaching (Figure 4). This clearly demonstrates the urgent need to focus on training of EBM.
Figure 4.
Formal training of EBM.
Discussion and conclusion
The survey has highlighted the important issue of inadequate skills of EBM among obstetrics and gynaecology trainees. They face clinical questions in their daily clinical routine, but due to various barriers they do not practise EBM to the full extent. The major barriers to practice of EBM are inability to understand statistical analysis, inadequate facilities for implementation, lack of a single compiled source of literature, relevant literature not being readily available and insufficient time on the job.4 The barriers described in literature are clinical freedom/judgment, limited resources and facilities, patient overload and lack of personal time.5 Our survey highlighted inadequate existing skills and absence of formal EBM training as major barriers. The trainees have positive attitudes towards EBM. They have found the different ways to train themselves. They use EBM resources as and when possible. But still they prefer to use the traditional rather easier methods to find the answers to their clinical questions. They do not feel confident using different EBM tools. 80% of them did not have formal EBM training so clearly they use the sources they are used to. The information received from such sources is not necessarily evidence based and clearly it affects the practice of EBM. Other authors do suggest similar findings and recommendations in other specialties. Formal training of EBM, as well as basic statistical analysis, should form a part of the curriculum to foster an environment favorable to the practice of EBM.6 Insufficient time and lack of skills are important barriers to the practice of EBM. These barriers should be recognized and integrated into EBM training programmes for trainees.7 The major limitation of this study is small number of participants. However, being a small deanery, we had limited choice. Another limitation is the mix of trainees at different levels of training. However, this survey aimed to take a snapshot of EBM skills among trainees. This study suggested that there is positive attitude among trainees. They would like to learn and practice EBM, they get enough opportunity but they are less confident in various areas of EBM. They are less confident in advanced literature search, understanding study design, critically appraising a paper and understanding statistics. Hence, practical use of EBM in clinical practice is still limited. These issues can be addressed by incorporating formal training and structured modules in the curriculum. Various tools may be used to ensure the continued use of EBM in practice. The areas that need to be explored are use of CAT making software, use of Educational Prescriptions, and use of information technology to disseminate EBM knowledge and skills among trainees. Future research should be aimed at producing and validating evidence based tools to promote EBM practice. Such tools are for lifelong learning experience.
This study is a snapshot view of what is happening on ground level. It highlights the inadequacy of EBM skills among trainees. It addresses an important issue of incorporating formal training of EBM along with specialty study modules.
However, it has a few limitations. The sample size is small. The study includes trainees from one specialty only; hence, there might be a question on applicability to other specialties. The response rate to this survey is low. This study, although it suffers from these limitations, creates a foundation for further research in this area.
Declarations
Competing interests
None declared
Funding
None declared
Ethical approval
Not required because it was a survey of trainees regarding current practice and this survey did not include any patient data or any contact to patients.
Guarantor
YBJ
Contributorship
YBJ designed study and survey with the help of other authors. AD modified the survey questions and finalized the design. JK and TS helped in data analysis
Acknowledgements
We would like to thank Post Graduate Educational Manager Jo Priestley (University Hospitals of Leicester) for her help while conducting this research
Provenance
Not commissioned; peer-reviewed by Katrien Oude Rengerink
References
- 1. Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet 2003; 362(9391): 1225–1230 [DOI] [PubMed] [Google Scholar]
- 2. Coomarasamy A, Khan KS. What is the evidence that postgraduate teaching in evidence based medicine changes anything? A systematic review. BMJ 2004; 329(7473): 1017–1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Buscaglia J, Nagula S, Yuan J, et al. The practice of evidence-based medicine (EBM) in gastroenterology: discrepancies between EBM familiarity and EBM competency. Therap Adv Gastroenterol 2011; 4(5): 283–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Oude Rengerink K, Thangaratinam S, Barnfield G, et al. How can we teach EBM in clinical practice? An analysis of barriers to implementation of on-the-job EBM teaching and learning. Med Teach 2011; 33(3): e125–e130 [DOI] [PubMed] [Google Scholar]
- 5. Al Omari M, Khader Y, Jadallah K, Dauod AS, Al-Shdifat AA, Khasawneh NM. Evidence-based medicine among hospital doctors in Jordan: awareness, attitude and practice. J Eval Clin Pract 2009; 15(6): 1137–1141 [DOI] [PubMed] [Google Scholar]
- 6. Mittal R, Perakath B. Evidence-based surgery: knowledge, attitudes, and perceived barriers among surgical trainees. J Surg Educ 2010; 67(5): 278–282 [DOI] [PubMed] [Google Scholar]
- 7. Van Dijk N, Hooft L, Wieringa-de Waard M. What are the barriers to residents’ practicing evidence-based medicine? A systematic review. Acad Med: J Assoc Am Med Coll 2010; 85(7): 1163–1170 [DOI] [PubMed] [Google Scholar]