This case describes a cerebrovascular accident (CVA) in a 33 year old with carotid and vertebral artery stenosis following a presentation of submandibular abscess.
Case report
A 33-year-old male presented to our institution with a left submandibular abscess secondary to dental infection. He had a three-day history of left jaw pain, lethargy, fever and decreased PO intake. He had no significant medical history. Examination findings included moderate to severe trismus and marked left submandibular swelling, and his 38th tooth was tender on palpation. His initial WCC was 18.7 with a neutrophilia and CRP was 153. Contrast CT demonstrated localized abscess in the left submandibular space.
Ultrasound reported a small hypoechoic mass on the medial aspect of the left submandibular gland. He was admitted and commenced on IV ceftriaxone, metronidazole and dexamethasone. His symptoms and biochemical markers improved over the following three days and he was discharged home on oral cephalexin and metronidazole. Drainage was initially considered unnecessary due to the small size of the collection and excellent clinical response.
Forty-eight hours after discharge, the patient re-presented to the same institution with right-sided weakness, confusion and sudden expressive aphasia. On examination, he was afebrile, had a BP of 159/92 and PR of 70. His GCS was 11, and he had a right upper motor neuron seventh nerve palsy and had decreased power in his right arm with hemi-sensory loss. His WCC was 14, CRP 45 and ESR 61. A non-contrast head CT scan was normal.
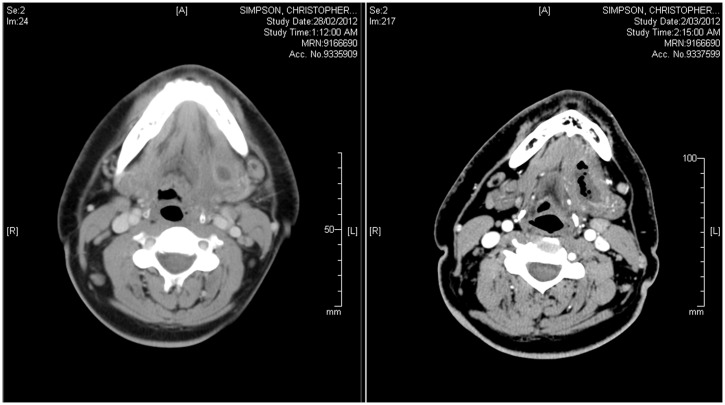
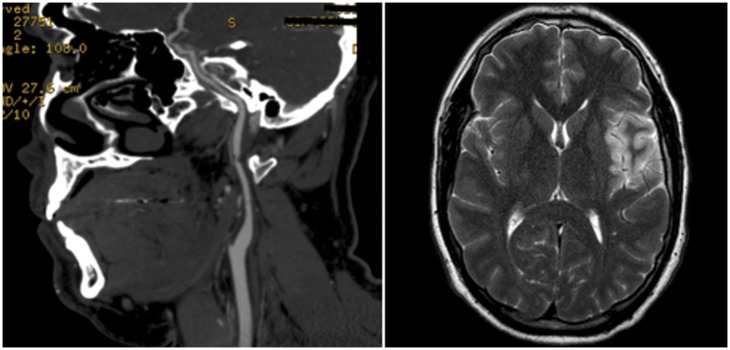
A CT angiogram of the head and neck was performed which demonstrated a tight stenosis (greater than 90%) involving the mid-left internal carotid artery over a distance of approximately 2 to 3 mm (Figure 1). A 1 cm-segment of thrombus was noted in the superior branch of the left MCA at the level of the anterior end of the Sylvian fissure and an abscess was seen involving the floor of mouth and submandibular space (Figure 2). MRI showed acute left inferior frontal cortical infarct in the distribution of the left MCA (Figure 1). It also showed further enlargement of the left submandibular space fluid collection, consistent with abscess formation with a focus of gas.
Figure 1.
Left image is a CT scan identifying the underlying carotid artery stenosis. Right image is an MRI on representation identifying a left MCA infarct.
Figure 2.
Left image is a CT scan on first admission. Right image is CT scan on representation. Although there was a worsening of the submandibular abscess on representation, the carotid sheath was not involved.
The patient was taken to theatre for a left transcervical incision and drainage of abscess and removal of the left submandibular gland. The findings at operation included a large left submandibular gland, adherent to the surrounding fascia. There was a large quantity of necrotic tissue surrounding the gland with fistula extending to the gingival mucosa adjacent to the 38th tooth. The tooth was removed.
Subsequent MRA of the neck performed one week postoperation demonstrated a stable stenosis of the distal left ICA at the level of C1 and, to a lesser extent, the right ICA. There was resolution of the left-sided submandibular fluid collection and the associated inflammatory change. ECHO/Holter monitor screen, thrombophilia screen and cholesterol studies were unremarkable.
Two months later, the patient was admitted for an elective left carotid endarterectomy via a combined transcervical and mandibular osteotomy approach. The findings at operation were a small internal carotid artery with an obvious stenosis, with intimal hyperplasia, 1 cm away from the base of the skull. His postoperative progress was complicated by a 10th, 11th and 12th cranial nerve paresis secondary to postoperative oedema. This improved throughout his postoperative stay with some mild deficit remaining at discharge.
Discussion
In this case report, the patient improved with the initial conservative management but he re-presented with a CVA and an evolving submandibular abscess. Our hypothesis for his CVA is that either the bilateral carotid stenosis was unmasked by antecedent systemic illness, caused by the submandibular abscess, or it was pure coincidence in timing. A Medline and PubMed literature search did not identify any other similar cases.
Odontogenic infection is the most common cause of deep neck abscess, followed by other oropharyngeal infections.1 In this case report, an infection of the 38th tooth was the source of the patient’s submandibular infection. The causative organism in this case was not identified; however, Gram-positive cocci, Gram-positive bacilli and Gram-negative bacilli were present. Specifically, the most common organisms identified in odontogenic infection include Streptococci, Staphylococci, Prevotella, Peptostreptococcus and Bacteroides.2
Inflammation caused by dental caries leads to oedema and hypoxia of the dental pulp resulting in pulp necrosis.3 This environment allows for easy bacterial invasion of the bone tissue. Spread of infection within the bone occurs in all directions until a cortical plate is encountered. If infection perforates the bone above the mylohyoid, fascial space involvement occurs. Spread of infection through fascial planes into deep neck spaces, such as the submandibular space, can result in local abscess formation. Extension of odontogenic infection into the deep neck spaces is an unusual, but potentially life threatening, sequela.3
It’s important to note that in this case, although submandibular abscess was the likely source of sepsis in CS, the abscess did not involve the carotid sheath and impede blood flow to the brain. MRI of the neck confirmed that there was no parapharyngeal space involvement.
Systemic complications of odontogenic infections are highly dependent on the virulence of the organism and the immune status of the patient.4 Infective endocarditis, secondary to odontogenic bacteraemia, is a well-documented complication typically seen in immunocompromised patients with underlying cardiac valve disease.5 Other complications include septicemia, CNS infection, skeletal and respiratory infections albeit rarely in the immunocompetent patient.5
A salient feature of this presentation was the underlying ICA/vertebral artery stenosis, which declared itself as a CVA in the stressed physiological conditions perhaps precipitated by the abscess. CVA in young adults is uncommon with an incidence between 8–21 events per 100,000/year.6 Large artery disease (including premature atherosclerosis) is one of the causes for CVA in young adults, accounting for approximately 20–33% of presentations.7 Other causes include haemorrhagic CVA, dissection of the extracranial arteries, cardiogenic embolism, small-vessel disease (including migraine/drugs) and haematological disease.8 In this case, intracranial bleeding and cerebral aneurysm were excluded by a CT angiogram and the cardiac ECHO, inflammatory markers, vasculitic and coagulopathy screen were normal. MR angiogram excluded a carotid dissection.
This unique case highlights the extent to which concurrent pathologies can be unmasked in the setting of systemic illness.
Declarations
Competing interests
None declared
Funding
None declared
Ethical Approval
Written informed permission to write the paper was obtained from the patient and the institution.
Guarantor
MR
Contributorship
NJ was actively involved in care of this patient and offered direction in the writing of this paper; BA was involved in providing access for an endarterectomy and was co-involved in the care of this patient; SM was the supervising surgeon for the paper.
Acknowledgements
None
Provenance
Submitted; peer reviewed by Joanna Walton
References
- 1. Wang LF, Tai CF, Kuo WR, Chien CY. Predisposing factors of complicated deep neck infections: 12-year experience at a single institution. J Otolaryngol Head Neck Surg 2010; 39: 335–41 [PubMed] [Google Scholar]
- 2. Poeschl WP, Spusta L, Russmueller G, et al. Antibiotic susceptibility and resistance of the odontogenic microbiological spectrum and its clinical impact on severe deep space head and neck infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 110: 151–6 [DOI] [PubMed] [Google Scholar]
- 3. Mahmood MHS, Mahmood SS. Odontogenic neck infections. Journal of Teachers Association 2005; 18: 55–9 [Google Scholar]
- 4. Jiménez Y, Bagán JV, Murillo J, Poveda R. Odontogenic infections. Complications. Systemic manifestations. Med Oral Patol Oral Cir Bucal 2004; 9: 143–7; 139–43 [PubMed] [Google Scholar]
- 5. Parahitiyawa NB, Jin LJ, Leung WK, Yam WC, Samaranayake LP. Microbiology of odontogenic bacteremia: beyond endocarditis. Clin Microbiol Rev 2009; 22: 46–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Marini C, Russo T, Felzani G. Incidence of stroke in young adults: a review. Stroke Res Treat 2011; 2011: 535672–535672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Elliott KE, Thin NN, Tsui JC, Davis M. Unusual cause of neurological symptoms in a young man. J R Soc Med Sh Rep 2011; 2: 314–314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Martin PJ, Enevoldson TP, Humphrey PRD. Causes of ischaemic stroke in the young. Postgrad Med J 1997; 73: 8–16 [DOI] [PMC free article] [PubMed] [Google Scholar]