Abstract
Recent studies have indicated an important role of chemokines such as CCL2 in the development of chronic pain. However, the distinct roles of different chemokines in the development and maintenance of neuropathic pain and in their interactions with neurons have not been clearly elucidated. We found that spinal nerve ligation (SNL) not only induced persistent neuropathic pain symptoms including mechanical allodynia and heat hyperalgesia but also produced sustained CXCL1 upregulation in the spinal cord. Double staining of immunofluorescence and in situ hybridization revealed that CXCL1 was primarily induced in spinal astrocytes. In cultured astrocytes, TNF-α induced robust CXCL1 expression, via the activation of the c-jun N-terminal kinase (JNK). Intrathecal administration of CXCL1 neutralizing antibody transiently reduced SNL-induced pain hypersensitivity, suggesting an essential role of CXCL1 in neuropathic pain sensitization. In particular, intraspinal delivery of CXCL1 shRNA lentiviral vectors, either before or after SNL, persistently attenuated SNL-induced pain hypersensitivity. Spinal application of CXCL1 not only elicited pain hypersensitivity but also induced rapid neuronal activation, as indicated by the expression of phosphorylated ERK and CREB (pERK and pCREB) and c-Fos in spinal cord neurons. Interestingly, CXCR2, the primary receptor of CXCL1, was upregulated in dorsal horn neurons after SNL, and the CXCR2 antagonist SB225002 completely blocked the CXCL1-induced heat hyperalgesia. SB225002 also attenuated SNL-induced pain hypersensitivity. Collectively, our results have demonstrated a novel form of chemokine-mediated glial-neuronal interaction in the spinal cord that can drive neuropathic pain. Inhibition of the CXCL1-CXCR2 signaling may offer a new therapy for neuropathic pain management.
Introduction
Neuroinflammation has been recently recognized for its pivotal role in the pathogenesis of neuropathic pain as well as in inflammatory pain [34,74]. Non-neuronal cells such as glial cells (astrocytes and microglia) turn to be reactive following peripheral nerve injuries and contribute to the enhancement and maintenance of neuropathic pain by releasing growth factors (e.g., BDNF and bFGF) and inflammatory mediators (e.g., proinflammatory cytokines and chemokines) [1,2,18,26,49,58]. Chemokines are a family of functionally related small secreted molecules with the established roles in modulation of numerous biological functions, including leukocyte migration and activation, cell adhesion, and T cell activation and have been demonstrated to regulate neuroinflammation at different anatomical locations, including nerve, dorsal root ganglion (DRG), spinal cord, and brain [46,47,63,74]. Increasing evidence has implicated chemokines in chronic pain processing following nerve injury [2,18].
CXCL1 belongs to CXC family and is also known as keratinocyte-derived chemokines (KC), growth-related oncogene (GRO) or cytokine-induced neutrophil chemoattractant-1 (CINC-1). CXCL1 in rodents plays similar biological roles as interleukin-8 (IL-8) in humans [70]. In the peripheral tissue, CXCL1 is involved in neutrophil chemotaxis and degranulation at early phase of inflammation. Recent studies have shown that spinal nerve ligation and localized inflammation of DRG induced rapid upregulation of CXCL1 in the DRG [40,75]. CXCL1 modulates neuronal excitability of DRG neurons by increasing sodium currents, potassium currents and the function of TRPV1 channels [14,71,77]. It also stimulates calcium influx and calcitonin gene-related peptide (CGRP) release in sensory neurons [56]. Intra-plantar or intra-articular injection of CXCL1 produced mechanical hyperalgesia in rodents [10,22,56] but see [14]. These studies suggest a pro-nociceptive role for CXCL1 in the peripheral nervous system. But it is virtually unknown whether and how central (spinal) CXCL1 would play a role in the genesis of neuropathic pain.
The biological effects of chemokine are mediated via G-protein-coupled chemokine receptors. Chemokines and their respective receptors are often detected in different cell types to mediate cell-cell interactions. In the spinal cord chemokines have been strongly implicated in neuron-to-microglia signaling after nerve injury. For example, CX3CL1 (fractalkine) and its receptor CX3CR1 are expressed by neurons and microglia, respectively [23,41,69,80], and CCL2 and CCR2 are localized to primary sensory neurons and microglia, respectively [3,12,66,78]. Chemokines can also mediate glia-to-neuron signaling, as indicated by respective expression of CCL2 and its receptor CCR2 in astrocytes and neurons [20,21,36]. Distinct expression of chemokines and their receptors is critical to determine whether a particular chemokine is important for neuron-to-glia signaling or glia-to-neuron signaling. CXCR2 is the primary receptor of CXCL1 and has been detected on neurons, microglia, and oligodendrocyte progenitors in the brain [24,51,55,68]. The distinct cellular localization of CXCL1 and CXCR2 in the spinal cord after nerve injury remains unclear. In the present study, we used spinal nerve ligation (SNL) neuropathic pain model to address this issue. Our findings provided new evidence for astrocyte-neuron interactions in the spinal cord and also revealed important roles of CXCL1/CXCR2 in the development and maintenance of neuropathic pain.
Materials and methods
Animals and surgery
Adult ICR mice (outbred, male, 25-35 g) were purchased from the Experimental Animal Center of Nantong University. All animal procedures in this study were performed according to the guidelines of the International Association for the Study of Pain, and were approved by the Animal Care and Use Committee of Nantong University. To produce a spinal nerve ligation, animals were anesthetized with sodium pentobarbital (40-50 mg/kg, i.p.) and the L6 transverse process was removed to expose the L4 and L5 spinal nerves. The L5 spinal nerve was then isolated and tightly ligated with 6-0 silk thread [35]. For sham-operated mice, the L6 transverse process was similarly removed and the L5 spinal nerve was exposed and isolated, but no nerve ligation was carried out.
Drugs and administration
The MAPK inhibitors SP600125, SB203580, and U0126 were purchased from Calbiochem. SB225002, a potent and selective antagonist of CXCR2, was purchased from Tocris. CXCL1 was purchased from R & D. Etanercept, a TNF-α inhibitor, was purchased from Pfizer. For intrathecal injection, spinal cord puncture was made with a 30 G needle between the L5 and L6 level to deliver the reagents to the cerebral spinal fluid [25].
Lentiviral vectors production and intraspinal injection
Three shRNAs targeting the sequence of mice CXCL1 (Gene Bank Accession NM_008176) were designed (shRNA1: 5′-AGT AAC GGA GAA AGA AGA CAG-3′; shRNA2: 5′-GAA GCT CCC TTG GTT CAG AAA-3′; shRNA3: 5′-TCAAGAATGGTCGCGAGGCTT-3′). An additional scrambled sequence was also designed as a negative control (NC) (5′-TTC TCC GAA CGT GTC ACG T-3′). Replication-deficient self-inactivating lentiviral expressing vectors pGCSIL-GFP (LV-shCXCL1 and LV-NC) were generated by Shanghai GeneChem. The final tilter of LV-shCXCL1-1, LV-shCXCL1-2, LV-shCXCL1-3, and LV-NC were 8 × 108 TU/ml, 8 × 108 TU/ml, 1 × 109 TU/ml, and 2 × 109 TU/ml respectively.
The knockdown effect of the three shRNAs was examined on cultured astrocytes and the shRNA with the best knockdown effect was chosen for intraspinal injection. For the injection, animals were anesthetized with pentobarbital sodium (40-50 mg/kg, i.p.) and underwent hemilaminectomy at the L1-L2 vertebral segments. Intraspinal injection was performed unilaterally on the left side. After exposure of the spinal cord, each animal received two injections (0.4 μl; 0.8 mm apart and 0.5 mm deep) of LV-shCXCL1 or LV-NC (1 × 105 TU) along the L4-L5 dorsal root entry zone using a glass micropipette (diameter 80 μm). The tip of glass micropipette reached to the depth of lamina II-IV of the spinal cord. The dorsal muscle and skin were then sutured.
Primary astrocytes cultures
Astrocytes cultures were prepared from cerebral cortexes of neonatal mice (P2). The cerebral hemispheres were isolated and transferred to ice-cold Hank’s buffer and the meninges were carefully removed. Tissues were then minced into ~1 mm pieces, triturated, filtered through a 100 μm nylon screen, and collected by centrifugation at ~3000 g for 5 min. The cell pellets were dispersed with a pipette and resuspended in a medium containing 15% FBS (fetal bovine serum) in low glucose DMEM (Dulbecco’s Modified Eagle’s Medium). After trituration, the cells were filtered through a 10 μm screen and then plated into 6-well plates at a density of 2.5 × 105 cells/cm2, and cultured for 10-12 days. The medium was replaced twice a week with 10% FBS. Once the cells were grown to 95% confluence, 0.15 mM dibutyryl cAMP (Sigma) was added to induce differentiation. Astrocytes used for immunocytochemistry were cultured onto cover glasses at a density of 2.5 × 104 cells/cm2, and differentiation was induced when cells reached 50% confluence. Prior to stimulation with TNF-α, OPTI-MEM was replaced. Astrocytes were incubated with TNF-α for different time periods ranging from 15 min to 4 h depending on the experiment. The treatment of the MAP kinase inhibitor SP600125 (10, 20, 50 μM), PD98059 (20, 50 μM), or SB203580 (10, 20, 50 μM) was started 30 min prior to TNF-α treatment. To test the knockdown effect of LV-shCXCL1, astrocytes were incubated with lentiviral vectors for 3 days and then stimulated with TNF-α for 1 h. After the treatment, the astrocytes were collected for Elisa or real-time PCR.
ELISA
Mouse CXCL1 ELISA kit was purchased from R&D. For in vivo experiments, animals were transcardially perfused with PBS and the lumbar spinal cord segments were dissected. For in vitro experiments, cultured astrocytes were collected after treatment. Spinal cord tissues or astrocytes were homogenized in a lysis buffer containing protease and phosphatase inhibitors. Protein concentrations were determined by BCA Protein Assay (Pierce). For each reaction in a 96-well plate, 100 μg of proteins were used, and ELISA was performed according to manufacturer’s protocol. The standard curve was included in each experiment.
Western blot
Protein samples were prepared in the same way as for ELISA analysis, and 30 μg of proteins were loaded for each lane and separated on SDS-PAGE gel (10%). After the transfer, the blots were incubated overnight at 4oC with polyclonal antibody against CXCR2 (1:50, rabbit, Boster). For loading control, the blots were probed with GAPDH antibody (1:20000, mouse, Sigma). These blots were further incubated with HRP-conjugated secondary antibody, developed in ECL solution, and exposed onto Hyperfilm (Amersham Biosciences) for 1–10 min. Specific bands were evaluated by apparent molecular size. The intensity of the selected bands was analyzed using Image J software (NIH).
Immunohistochemistry and immunocytochemistry
After appropriate survival times, animals were deeply anesthetized with isoflurane and perfused through the ascending aorta with PBS followed by 4% paraformaldehyde with 1.5% picric acid in 0.16 M PB. After the perfusion, the L4-L5 spinal cord segments were removed and postfixed in the same fixative overnight. Spinal cord sections (30 μm, free-floating) were cut in a cryostat and processed for immunofluorescence as we described previously [20]. The sections were first blocked with 2% goat or donkey serum for 1 h at room temperature and then incubated overnight at 4oC with the following primary antibodies: CXCL1 (rabbit, 1: 100, Boster), CXCR2 (rabbit, 1:100, Boster), GFAP antibody (mouse, 1:5000, Millipore), OX-42 antibody (mouse, 1:5000, Serotec), NeuN antibody (mouse, 1:5000, Millipore), phosphorylated ERK antibody (pERK1/2, rabbit, 1:500, Cell Signaling), phosphorylated CREB (pCREB, rabbit, 1:1000, Cell Signaling), c-Fos antibody (rabbit, 1:1000, Santa Cruz), and PKCγ (mouse, 1:500, Santa Cruz). The sections were then incubated for 1 h at room temperature with Cy3- or FITC-conjugated secondary antibodies (1:1000, Jackson ImmunoResearch). For double immunofluorescence, sections were incubated with a mixture of mouse and rabbit primary antibodies followed by a mixture of FITC- and Cy3-congugated secondary antibodies. The stained sections were examined with a Leica fluorescence microscope, and images were captured with a CCD Spot camera. The specificity of CXCL1 and CXCR2 primary antibodies was tested by preabsorption experiment. The spinal cord sections were incubated with a mixture of CXCL1 or CXCR2 primary antibody and the corresponding blocking peptide for CXCL1 (25 μg/ml; Boster) or CXCR2 (25 μg/ml; Boster) overnight, followed by secondary antibody incubation. CXCL1 and CXCR2 immunostaining signal was abolished after absorption (supplemental Fig.1).
For immunocytochemistry, cultured astrocytes, after incubation with TNF-α for 1 h, were fixed with 4% paraformaldehyde for 20 min, and processed for immunofluorescence with CXCL1 (rabbit, 1:500, Santa Cruz) and GFAP (mouse, 1:5000, Millipore) antibody as shown above. After immunostaining, DAPI (Sigma, 0.1 μg/ml) was added for 5 min at room temperature to stain all the nuclei of cells in the cultures.
In situ hybridization
The CXCL1 cDNAs were obtained by RT-PCR and cloned into pGEM-T Easy Vector System I (Promega, USA). As previously described by Pineau et al [54], primers used for the cloning were 5′-GAA CGC TGG CTT CTG ACA AC-3′ and 5′-CGA GAC GAG ACC AGG AGA AA-3′. The sequences were verified by Genebank BLAST analysis. The antisense and sense Digoxigenin-labeled RNA probes were synthesized using the Riboprobe Combination System SP6/T7 (Roche Applied Science).
In situ hybridization was performed according to method described previously [20]. Briefly, the slides were washed in PBS (0.01 M, pH 7.4) and then incubated in proteinase K (1 mg/L) at 37°C for 10 min. After washed in PBS, the sections were prehybridized at 42°C for 2 h, then hybridized with the DIG-labeled probe (1 μg/ml) at 42°C overnight. After hybridization, slides were washed 3 times with 50% formamide in sodium chloride-sodium citrate buffer and then treated with anti-digoxigenin antibody conjugated rhodamine according to the manufacturer’s protocol (Roche Applied Science). The corresponding sense probe was also incubated as control.
To identify the cell types expressing CXCL1 mRNAs, these slides were then incubated with the mouse anti-GFAP antibody overnight at 4°C, and then incubated with FITC-conjugated goat anti-mouse antibody. The signal was detected with a Leica fluorescence microscope, and images were captured with a CCD spot camera.
Real-time PCR
Total RNA was extracted from L5 spinal cord with the Trizol reagent (Invitrogen). One microgram of total RNA was converted into cDNA using PrimeScript RT reagent kit (Takara). The cDNA was amplified using the following primers: CXCL1-forward (5′-GCT TGA AGG TGT TGC CCT CAG -3′) and CXCL1-reverse (5′-AGA AGC CAG CGT TCA CCA GAC-3′), TNF-α-forward (5′-GTT CTA TGG CCC AGA CCC TCA C-3′) and TNF-α-reverse (5′-GGC ACC ACT AGT TGG TTG TCT TTG-3′), GAPDH-forward (5′-TGT TCC TAC CCC CAA TGT G-3′) and GAPDH-reverse (5′-GTG TAG CCC AAG ATG CCC T-3′). The SYBR Premix Ex Taq II kit (Takara) was used for all PCR reactions. The PCR reactions were run on a Rotor-Gene 6000 RT-PCR machine (Corbett Research). The melting curves were performed to validate the utility and specificity of each PCR product. The data were analyzed using Rotor-Gene 6000 series software, and evaluated using the Comparative CT Method (2−δδCT).
Behavioral analysis
Animals were habituated to the testing environment daily for at least two days before baseline testing. The room temperature and humidity remained stable for all experiments. For testing mechanical sensitivity, animals were put in boxes on an elevated metal mesh floor and allowed 30 min for habituation before examination. The plantar surface of each hindpaw was stimulated with a series of von Frey hairs with logarithmically incrementing stiffness (0.02-2.56 grams, Stoelting), presented perpendicular to the plantar surface (2-3 seconds for each hair). The 50% paw withdrawal threshold was determined using Dixon’s up-down method [7]. For testing heat sensitivity, animals were put in plastic boxes and allowed 30 min for habituation before examination. Heat sensitivity was tested by radiant heat using Hargreaves apparatus (IITC Life Science Inc.) and expressed as paw withdrawal latency (PWL). The radiant heat intensity was adjusted so that basal PWL is between 10-14 seconds, with a cut-off of 18 seconds to prevent tissue damage.
Quantification and statistics
The density of specific bands from Western blotting was measured with a computer-assisted imaging analysis system (Image J, NIH). The size of rectangle was fixed for each band and the background near that band was subtracted. The numbers of pERK-, pCREB-, and c-Fos-labeled cells were counted in laminae I-VI of the spinal cord. Three non-adjacent sections were randomly selected, and three to four mice were included in each group. Differences between groups were compared using one-way ANOVA followed by Newman-Keuls post hoc test or using Student’s t-test if only two groups were applied. All data were expressed as mean + SEM. The criterion for statistical significance was P < 0.05.
Results
CXCL1 is upregulated in spinal cord astrocytes after nerve injury
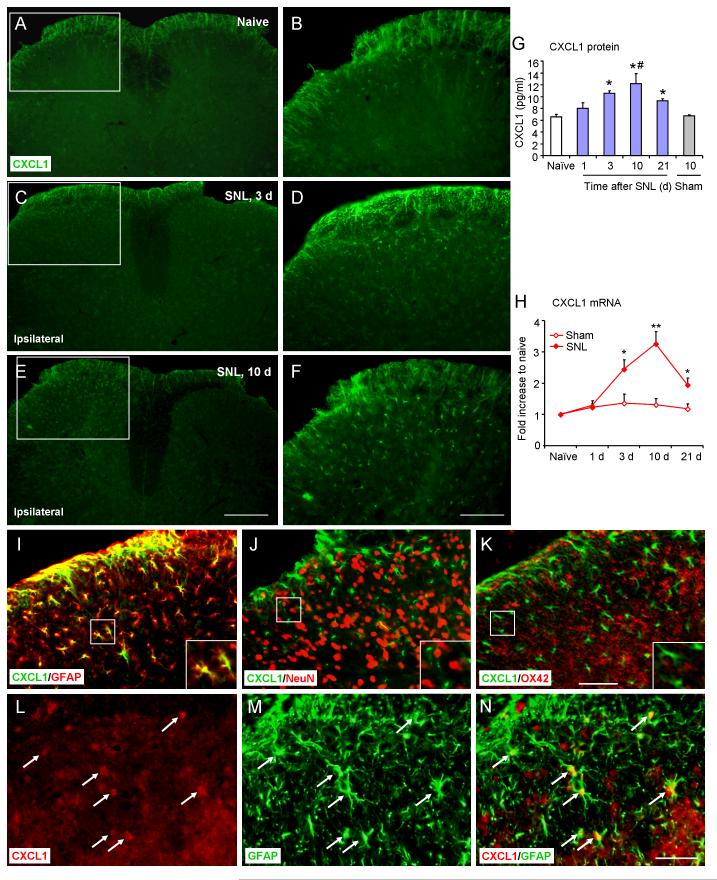
SNL produces rapid and persistent neuropathic pain, starting from 1 day and lasting for more than 3 weeks in rats [35] and mice [32]. To examine CXCL1 expression in the spinal cord, we performed immunostaining in naïve and SNL-operated mice. As shown in Fig. 1, CXCL1 was constitutively expressed in the superficial dorsal horn (Fig. 1A, B). SNL induced a marked increase of CXCL1 expression and many more CXCL1-immunoreactive (IR) cells were found in the ipsilateral than the contralateral spinal cord at 3 days (Fig. 1C, D) and 10 days (Fig. 1E, F). Elisa results showed that CXCL1 expression increased from day 3, peaked at day 10, and maintained at day 21 after SNL (P < 0.05, SNL vs. naïve). CXCL1 expression was also significantly higher in SNL animals than in sham-operated animals at 10 d after operation (P < 0.05, SNL vs. sham, Fig.1G). Real-time PCR showed a parallel and significant increase in CXCL1 mRNA at 3 d, 10 d, and 21 d in SNL animals (P < 0.05 or P< 0.01, SNL vs. sham, Fig. 1H).
Figure 1.
SNL induces CXCL1 upregulation in spinal cord astrocyes. A-F. CXCL1 expression in the spinal cord of naïve animals (A,B) and SNL at 3 d (C, D) and 10 d (E,F). B, D, F, High-magnification images of A, C, E, indicated in the white boxes. Scale bar, 200 μm in E, 100 μm in F. G, Elisa results show time course of CXCL1 expression in the L5 spinal cord after SNL. * P < 0.05, compared to naïve; # P < 0.05, compared to sham-operated control, Student’s t-test. H, Real-time PCR results show time course of CXCL1 mRNA expression in the spinal cord after SNL or sham operation. * P < 0.05, ** P < 0.01, SNL vs. sham, Student’s t-test. I-K, Double staining shows that CXCL1 is colocalized with GFAP, a marker for astrocytes (I), but not with NeuN, a marker for neurons (J) or OX42, a marker for microglia (K). Scale bar, 50 μm. L-N, In situ hybridization of CXCL1 mRNA (L) and immunofluorescence staining of GFAP (M) showed that CXCL1 mRNA is colocalized with GFAP (N). Scale bar, 25 μm.
To define the cellular distribution of CXCL1, we performed double staining of CXCL1 with different cell markers. CXCL1-IR was primarily colocalized with the astrocytic marker GFAP (Fig. 1I) but not with neuronal marker NeuN (Fig. 1J) or microglial marker OX-42 (Fig. 1K).
To further define the cellular localization of CXCL1 in the spinal cord, we performed in situ hybridization using an antisense probe of CXCL1. Because the expression of CXCL1 protein and mRNA is peaked at 10 days after SNL, we picked this time point to check CXCL1 mRNA expression. As shown in Fig.1L-N, CXCL1 mRNA expression was colocalized with GFAP. Collectively, these results suggest that (1) SNL induced persistent CXCL1 increase and (2) CXCL1 was primarily produced by astrocytes.
TNF-α drives spinal CXCL1 expression after nerve injury
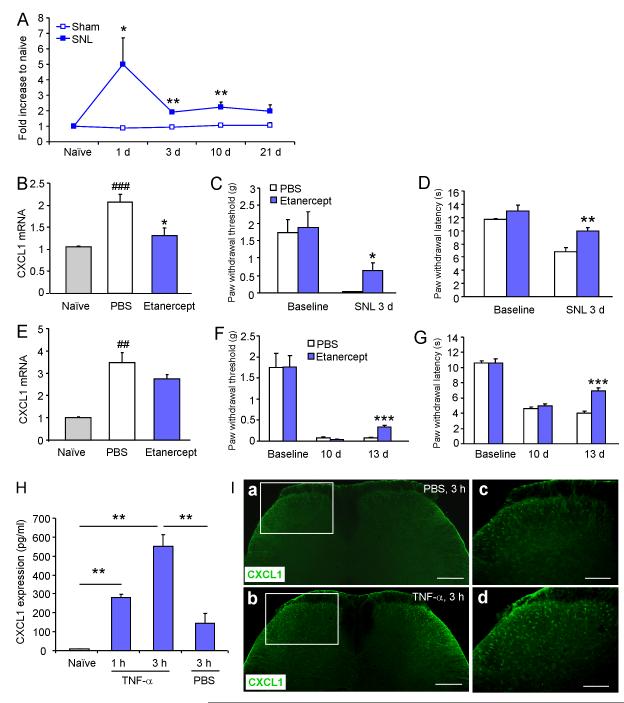
We next explored the possible upstream trigger for CXCL1 upregulation after SNL. The proinflammatory cytokine TNF-α has been implicated in triggering an inflammatory cascade that underlies the development of neuropathic pain after nerve injury [39,62,65,76]. We tested whether CXCL1 upregulation was induced by TNF-α. Real-time PCR analysis showed that SNL induced rapid TNF-α mRNA upregulation at 1 d. The TNF-α mRNA expression was declined from the peak at 3 d, maintained at 10 d, and recovered at 21 d after operation (Fig. 2A). In contrast, CXCL1 mRNA expression was not significant at 1 day but significantly increased at 3 d, 10 d and 21 d. (Fig. 1H). These data suggest that TNF-α mRNA increase precedes CXCL1 mRNA increase following SNL.
Figure 2.
TNF-α triggers the expression of CXCL1 in the spinal cord. A. SNL rapidly increases TNF-α mRNA expression in the spinal cord. * P < 0.05, ** P <0 0.01, SNL vs. sham, student’s t-test. B. Intrathecal injection of etanercept before SNL blocks SNL-induced CXCL1 mRNA increase in the spinal cord at 3 days after SNL. ### P < 0.001; compared with naïve; * P < 0.05, etanercept vs. PBS, Student’s t-test. C, D. Etanercept reduces SNL-induced mechanical allodynia (C) and heat hyperalgesia (D). * P < 0.05, ** P < 0.01, compared with PBS control, student’s t-test. E-G. Intrathecal injection of etanercept at 10 d after SNL does not decrease CXCL1 mRNA expression (E), but attenuated mechanical allodynia (F) and heat hyperalgesia (G). ## P < 0.01, compared with naïve; *** P < 0.001, compared with PBS control, Student’s t-test. E. Elisa shows that intrathecal injection of TNF-α rapidly and dramatically increases CXCL1 expression in the spinal cord at 1 h and 3 h after injection. ** P < 0.01, student’s t-test. F. Immunostaining shows CXCL1 expression in the spinal cord at 3 h after injection of PBS (a, c) and TNF-α (b, d). Scale bar, a, b, 200 μm; c, d, 50 μm
We then checked whether blocking TNF-α could reduce SNL-induced CXCL1 mRNA upregulation. Etanercept, a TNF-α inhibitor was intrathecally injected either before or 10 d after the SNL surgery. A single bolus injection of etanercept (10 μg) before SNL blocked SNL-induced CXCL1 mRNA upregulation at 3 days after SNL (P < 0.05, etanercept vs. PBS; P > 0.05, etanercept vs. naïve, Fig. 2B). SNL-induced mechanical allodynia and heat hyperalgesia were also significantly attenuated by etanercept (Fig. 2C, D). However, intrathecal injection of same dose etanercept at 10 d after SNL had no significant effect on SNL-induced CXCL1 mRNA expression (Fig. 2E), but mildly attenuated mechanical allodynia (Fig. 2F) and heat hyperalgesia (Fig. 2G). These data suggest the spinal TNF-α is required for the induction of CXCL1 upregulation and the development of SNL-induced neuropathic pain.
To test if TNF-α is sufficient to induce CXCL1 upregulation in the spinal cord, we intrathecally injected TNF-α and checked CXCL1 expression. Our previous study showed that i.t. injection of TNF-α induced mechanical allodynia and heat hyperalgesia in mice [20]. CXCL1 level in the spinal cord was significantly increased after TNF-α application, as shown by Elisa (Fig. 2H). TNF-α also increased CXCL1-IR at 3 h, as indicated by immunostaining (Fig. 2I). These results suggest that TNF-α is both required and sufficient for the CXCL1 upregulation in the spinal cord.
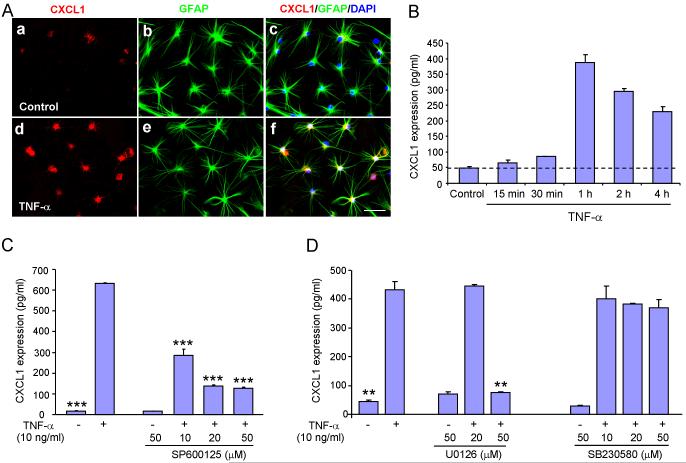
JNK pathway is required for CXCL1 upregulation in cultured astrocytes and spinal cord
To further determine the intracellular signaling that involved in TNF-α-induced CXCL1 expression, we prepared primary astrocyte cultures from cerebral cortexes of neonatal mice (P2). TNF-α incubation for 1 h increased CXCL1 expression (Fig. 3A). Elisa test further showed that TNF-α (10 ng/ml) induced rapid increase of CXCL1 expression, with 1.4-flod increase at 15 min and 8- and 4.7-fold increase at 1 h and 4 h, respectively (Fig. 3B).
Figure 3.
TNF-α induces JNK-dependent CXCL1 upregulation in cultured astrocytes. A. Triple staining of CXCL1 (a, d), GFAP (b, e), and DAPI (c, f) in control (a) and TNF-α-stimulated (d) astrocytes. c, f shows that all DAPI+ cells also express GFAP. Scale bar, 50 μm. B. TNF-α induces time-dependent upregulation of CXCL1 in astrocytes. C. JNK inhibitor SP600125 at the doses of 10 μM, 20 μM, and 50 μM reduces TNF-α-induced CXCL1 upregulation. D. MEK inhibitor PD98059 at the dose of 50 μM reduces TNF-α-induced CXCL1 upregulation, whereas p38 inhibitor SB203580 at all three doses has no effect on TNF-α-induced CXCL1 upregulation, ** P < 0.01, *** P < 0.001, vs. TNF-α treatment, Student’s t-test.
MAPKs are important cellular signaling components and include three major members: JNK (c-jun N-terminal kinase), ERK (extracellular signal-regulated kinase), and p38. To define the role of MAPKs in TNF-α-induced CXCL1 expression, we examined the effects of SP600125 (JNK inhibitor), U0126 (MEK inhibitor), and SB203580 (p38 inhibitor) on CXCL1 expression by Elisa. Pretreatment of SP600125, 30 min before TNF-α treatment, decreased CXCL1 expression by 55%, 78%, and 80% at the doses of 10, 20, and 50 μM, respectively (P < 0.001, compared to TNF-α treatment, Fig. 3C). In contrast, U0126 only suppressed TNF-α-induced CXCL1 expression at a high concentration (50 μM, P < 0.01), whereas SB203580 had no effect at all concentrations (Fig. 3D). These data suggest JNK is critical for mediating TNF-α-induced CXCL1 production.
To investigate whether JNK would also be involved in SNL-induced CXCL1 upregulation and pain hypersensitivity, we intrathecally injected SP600125 (20 nmol) daily for 3 days (from day 8 to day 10 after SNL). SP600125 reversed SNL-induced mechanical allodynia (P < 0.05, supplemental Fig. 2A) and heat hyperalgesia (P < 0.05, supplemental Fig. 2B), and also decreased CXCL1 expression by 36 ± 6 % (supplemental Fig. 2C). Taken together, these data suggest that the TNF-α/JNK pathway is involved in the SNL-induced CXCL1 upregulation in spinal astrocytes.
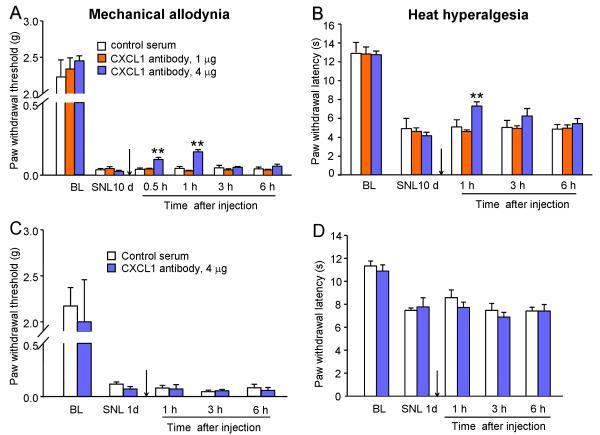
Intrathecal injection of CXCL1 neutralizing antibody transiently attenuates SNL-induced neuropathic pain
To investigate the role of endogenous CXCL1 in the SNL-induced neuropathic pain, we intrathecally injected a CXCL1 neutralizing antibody. As CXCL1 expression is peaked at 10 days after SNL, we first checked the effect of CXCL1 neutralizing antibody at 10 days. The behavioral results showed a dose-dependent inhibition of neuropathic pain by CXCL1 neutralization. CXCL1 neutralizing antibody, at the dose of 4 μg but not 1 μg, transiently (1 h) reduced SNL-induced mechanical allodynia (P < 0.01, compared to control serum, Fig. 4A) and heat hyperalgesia (P < 0.05, compared to control serum, Fig. 4B). In contrast, intrathecal injection of CXCL1 neutralizing antibody (4 μg) at 1 day after SNL did not show effect on either mechanical allodynia (Fig. 4C) or heat hyperalgesia (Fig. 4D), suggesting CXCL1 is not involved in the early phase of SNL-induced neuropathic pain.
Figure 4.
Intrathecal injection of CXCL1 neutralizing antibody, at 10 days after SNL, partially and transiently reverses SNL-induced mechanical allodynia (A) and heat hyperalgesia (B). ** P < 0.01, vs. control serum, one-way ANOVA followed by Newman-Keuls post hoc test. However, intrathecal injection of CXCL1 neutralizing antibody, at 1 day after SNL, has no effect on either mechanical allodynia (C) or heat hyperalgesia (D). Student’s t-test. BL, Baseline.
Intraspinal injection of recombinant lentivirus-CXCL1 shRNA persistently suppresses SNL-induced neuropathic pain
To test the long-term effect of inhibiting CXCL1 on neuropathic pain, we produced CXCL1 shRNA lentivirus vectors to persistently knockdown CXCL1 expression. We first tested the inhibitory effect of the lentiviral vector-expressed shRNAs on TNF-α-induced CXCL1 expression in cultured astrocytes. The astrocytes were preincubated with different strands of LV-shCXCL1 or LV-NC for 3 days and followed by incubation with TNF-α for 1 h. The results showed that the three LV-shCXCL1 differently decreased TNF-α-induced CXCL1 mRNA upregulation by 55%, 71%, and 50% (supplemental Fig. 3A). Based on these data, we chose the LV-shCXCL1-2 for the following in vivo experiments.
We intraspinally infused this LV-shCXCL1 and LV-NC into the L5 spinal cord. Seven days later, GFP expression was observed in the injected side of the dorsal horn (supplemental Fig. 3B). To examine the cell types that expressed the GFP, the sections were immunostained with GFAP, IBA-1, and NeuN. Throughout the dorsal horn of spinal cord, GFP was primarily localized to GFAP-positive astrocytes (supplemental Fig. 3C). A few of GFP expression was observed in IBA-1-positive microglia (supplemental Fig.3D) or in NeuN-positive neurons (supplemental Fig. 3E).
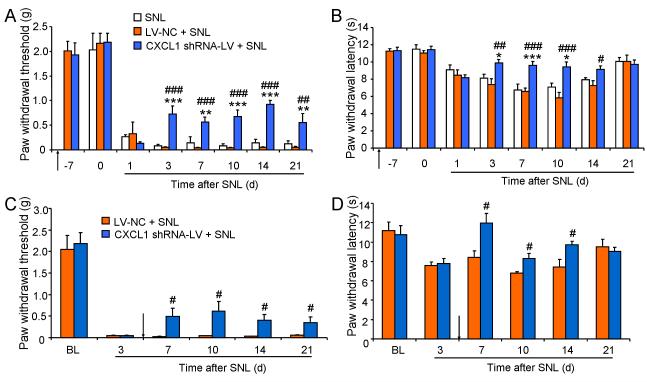
We checked whether pretreatment with LV-shCXCL1 via intraspinal infusion can block the development of SNL-induced pain hypersensitivity. Injection of the vector alone did not affect the baseline paw withdrawal threshold and paw withdrawal latency tested at 7 days after the infusion (Fig. 5A, B). We then performed spinal nerve ligation on these animals and examined mechanical allodynia and heat hyperalgesia. LV-shCXCL1 partly prevented SNL-induced mechanical allodynia: the effect started at 3 days after SNL and maintained for more than 21 days (Fig. 5A). Meanwhile, LV-shCXCL1 reduced SNL-induced heat hyperalgesia for 21 days (Fig. 5B). To confirm the knockdown effect of CXCL1 shRNA lentiviral vector in vivo, we checked CXCL1 mRNA expression at 10 days after SNL (17 days after vectors injection). The CXCL1 mRNA expression was reduced by 45% following the LV-shCXCL1 treatment compared to the LV-NC control.
Figure 5.
Intraspinal injection of recombinant lentivirus-CXCL1 shRNA persistently suppresses SNL-induced neuropathic pain. Intraspinal infusion of CXCL1 shRNA lentiviral vectors 7 days before SNL persistently reduces SNL-induced mechanical allodynia (A) and heat hyperalgesia (B). * P < 0.05; ** P < 0.01; *** P < 0.001, vs. SNL. # P < 0.05; ## P < 0.01; ### P < 0.001, vs. LV-NC + SNL, one-way ANOVA followed by Newman-Keuls post hoc test. Intraspinal infusion of CXCL1 shRNA lentiviral vectors 5 days after SNL also reduces SNL-induced mechanical allodynia (C) and heat hyperalgesia (D). # P < 0.05, vs. LV-NC+ SNL, Student’s t-test
We then checked the reversal effect of LV-shCXCL1. The same amount of LV-shCXCL1 was infused at 5 days after SNL. As shown in Fig. 5C, D, SNL-induced mechanical allodynia was attenuated from 7-21 days. The heat hyperalgesia was also reversed from 7-14 days and fully recovered at 21 days. Taken together, these behavioral data suggest that CXCL1 is critical for SNL-induced neuropathic pain sensitization.
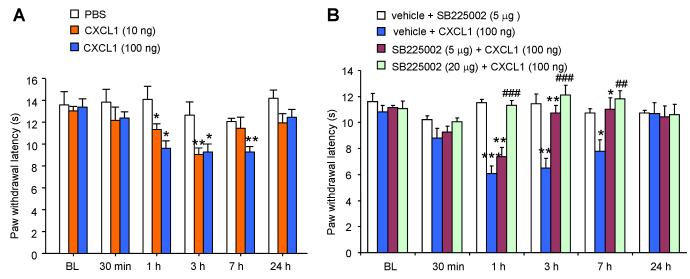
Spinal injection of exogenous CXCL1 induces heat hyperalgesia and activation of spinal cord neurons through CXCR2
We investigated whether CXCL1 is sufficient to produce pain and how it is involved in the modulation of pain hypersensitivity. We first intrathecally injected CXCL1 (10 ng or 100 ng) and tested heat hyperalgesia at different times after injection. As shown in Fig. 6A, CXCL1 produced heat hyperalgesia in a dose-dependent manner. The paw withdrawal latency was decreased at 1 h, maintained at 7 h and recovered after 24 h by CXCL1 at the dose of 100 ng.
Figure 6.
Spinal injection of CXCL1 induces heat hyperalgesia via CXCR2. (A) Intrathecal injection of CXCL1 (10 or 100 ng) induces a dose-dependent heat hyperalgesia. * P < 0.05; ** P < 0.01, vs. PBS, one-way ANOVA followed by Newman-Keuls post hoc test. (B) Intrathecal injection of CXCR2 antagonist, SB225002, 30 min before CXCL1 injection dose-dependently prevented CXCL1-induce heat hyperalgesia. * P < 0.05; ** P < 0.01; *** P < 0.001 vs. corresponding BL (baseline). ## P < 0.01; ### P < 0.001 vs. vehicle + CXCL1 (100 ng), one-way ANOVA followed by Newman-Keuls post hoc test.
CXCR2 is a major receptor of CXCL1 [46,73]. To test if CXCL1-induced pain hypersensitivity is mediated by CXCR2, we intrathecally injected SB225002, a potent and selective CXCR2 antagonist, 30 min before CXCL1 injection and tested heat hyperalgesia. At a low dose (5 μg), SB225002 partially reversed the CXCL1-induced heat hyperalgesia. But at a high dose (20 μg), SB225002 completely blocked the hyperalgesia. SB225002 itself did not change the paw withdrawal latency at all the time points (Fig. 6B).
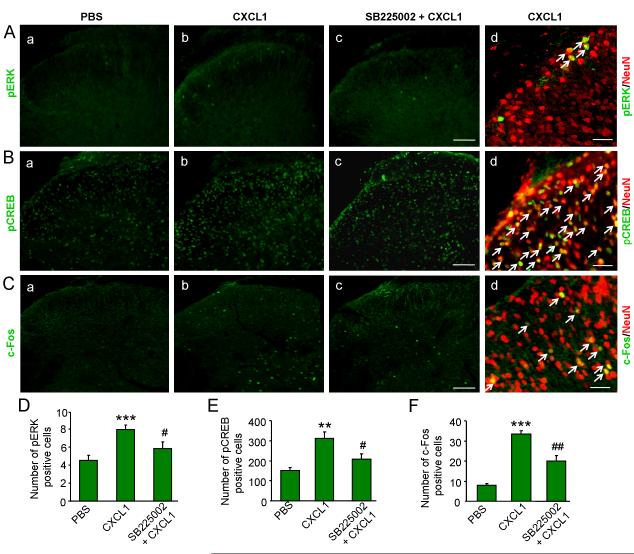
ERK and c-Fos are important markers for neuronal activation and central sensitization following noxious stimulation [17]. In addition, phosphorylated ERK (pERK) can be translocated into the nucleus to activate several transcriptional factors, such as cAMP-response element binding protein (CREB) that is required for the transcription of several pain-related genes. We examined the expression of pERK, pCREB (phosphorylated CREB), and c-Fos at 30 min or 2 h after spinal injection of CXCL1 (100 ng). As shown in Fig.7, CXCL1 increased pERK (Fig. 7A) and pCREB (Fig. 7B) expression in the dorsal horn of the spinal cord at 30 min after injection and c-Fos expression at 2 h after injection (Fig. 7C). Additionally, intrathecal injection of SB225002 (20 μg) 30 min before CXCL1 injection blocked CXCL1-induced pERK and pCREB expression and reduced c-Fos expression (Fig. 7c, D-F). The double immunofluorescence staining showed high colocalization of pERK, pCREB, or c-Fos with NeuN, suggesting the dominant expression of these markers by neurons (Fig. 7d).
Figure 7.
CXCL1 increases the expression of pERK, pCREB and c-Fos in spinal cord neurons. Intrathecal injection of CXCL1 (100 ng) increases pERK expression (A,D) and pCREB expression (B,E) at 30 min and c-Fos expression (C, F) at 2 h after injection, which is blocked by pretreatment with SB225002 (20 μg). Majority of pERK-, pCREB-, or c-Fos immunoreactive cells in spinal cord express the neuronal marker NeuN (d). Scale bar, 100 μm in c, 50 μm in d. ** P < 0.01; *** P < 0.001 vs. PBS. # P < 0.05; ## P < 0.01 vs. CXCL1, one-way ANOVA followed by Newman-Keuls post hoc test.
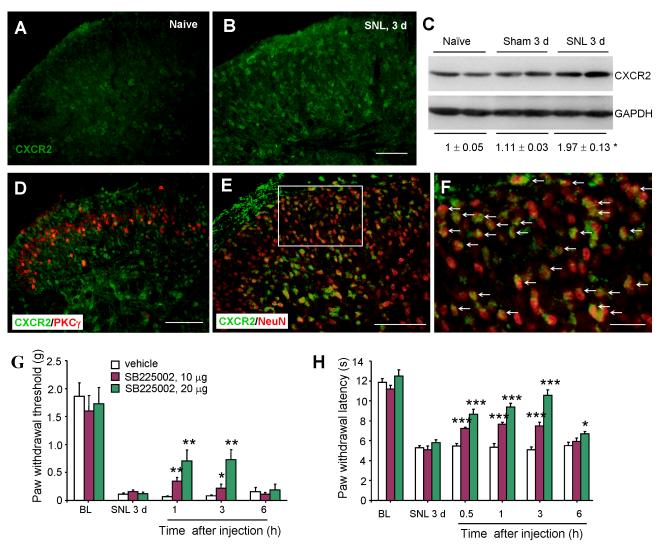
SNL induces CXCR2 upregulation in spinal cord neurons
We further investigated CXCR2 expression and distribution in the spinal cord in a neuropathic pain condition. In naïve animals, CXCR2 was constitutively expressed in the dorsal horn (Fig. 8A). At 3 days after SNL, CXCR2-IR was significantly increased in both superficial and deep dorsal horn (Fig. 8B). Western Blot results further showed CXCR2 was significantly increased in the ipsilateral dorsal horn at 3 days after SNL (P < 0.05, SNL vs. sham, Fig. 8C). To identify the lamina distribution of CXCR2 expression, we did CXCR2 and PKCγ double staining, because PKCγ is expressed mainly in neurons of the inner part of lamina II [43,50]. Most CXCR2-positive cells were found in lamina I and laminae IIi-V (Fig. 8D), but the cells in the outer part of lamina II is less. To further test if CXCR2 was expressed in neurons, we did immunofluorescence double staining of CXCR2 and NeuN and found many CXCR2-IR cells were also NeuN-positive (Fig. 8E, F).
Figure 8.
SNL induces CXCR2 upregulation in spinal cord neurons. CXCR2 is expressed in the spinal cord of naïve animals (A) and increased at 3 d after SNL (B). Scale bar, 100 μm. B. Western blot shows the expression of CXCR2 in the spinal cord in naïve, sham, and SNL animals. SNL increases CXCR2 expression compared to sham control. * P < 0.05, SNL vs. sham, Student’s t-test. D. Double staining of CXCR2 and PKCγ showing the lamina distribution of CXCR2-positive cells. Scale bar, 100 μm. E. Double staining of CXCR2 and NeuN showing the expression of CXCR2 in neurons. Scale bar, 100 μm. F, High-magnification image of E. Scale bar, 25 μm. G, H. Intrathecal injection of SB225002, at 3 days after SNL, dose-dependently reversed SNL-induced mechanical allodynia (G) and heat hyperalgesia (H). * P < 0.05; ** P < 0.01; *** P < 0.001 vs. vehicle, one-way ANOVA followed by Newman-Keuls post hoc test.
To investigate the role of CXCR2 in the SNL-induced neuropathic pain, CXCR2 antagonist, SB225002 (10 μg and 20 μg) was intrathecally injected at 3 days after SNL. SB225002 dose-dependently reduced mechanical allodynia and heat hyperalgesia with the effect maintained for more than 3 h (Fig. 8G, H). The animals with sham operation did not show pain hypersensitivity at 3 days. In addition, intrathecal injection of SB225002 at the dose of 20 μg at 3 days after sham operation did not affect either mechanical allodynia or heat hyperalgesia (Supplemental Fig.4A, B), suggesting the specific role of CXCR2 in SNL-induced neuropathic pain.
Discussion
Neuroinflammation in the spinal cord has been implicated in the development and maintenance of central sensitization and pain hypersensitivity [74]. Accumulating evidence demonstrates that chemokines, such as CCL2 and CX3CL1 are involved in neuroinflammation in the spinal cord and contribute to neuropathic pain processing [2,18]. In addition, astrocytes serve as a main source of inflammatory mediators [58,72]. In this study, we have shown CXCL1, produced by astrocytes, plays an important role in the maintenance of central sensitization and neuropathic pain. We have made the following findings. First, SNL induced slow but persistent CXCL1 upregulation in spinal astrocytes, which is dependent on the TNF-α/JNK pathway. Second, spinal inhibition of CXCL1 partly reversed SNL-induced pain hypersensitivity. However, intraspinal injection of CXCL1-shRNA lentivirus vector either before or after SNL persistently attenuated SNL-induce pain hypersensitivity. Third, spinal application of CXCL1 induced heat hyperalgesia via the activation of CXCR2. CXCL1 also induced CXCR2-dependent neuronal activation and central sensitization (e.g., increase of pERK, pCREB, and c-Fos) in dorsal horn neurons. Finally, SNL induced upregulation of CXCR2 in spinal neurons. Spinal post-treatment of a selective CXCR2 antagonist SB225002 effectively attenuated SNL-induced heat hyperalgesia and mechanical allodynia.
CXCL1 upregulation in spinal astrocytes and the involvement in neuropathic pain
It has been reported that CXCL1 expression is regulated in pathological pain conditions. CXCL1 expression is increased in the DRG at 3 days but not at 7 days after spinal nerve ligation and localized inflammation [40,75]. In addition, McTigue et al. showed that contusion injury of spinal cord induced 30-fold increase of CXCL1 mRNA in the spinal cord at 6 h post injury, which decayed rapidly thereafter [45]. In contrast, our data showed that SNL induced a slow (3 d) but persistent (> 21 d) CXCL1 increase in the spinal cord, indicating CXCL1 may play a distinct role in neuropathic pain
It was reported that CXCL1 is expressed in brain neurons after soman-induced status epilepticus in rats [29]. In our study, both the fluorescence double staining and in situ hybridization combining with immunofluorescence showed that CXCL1 protein and mRNA were predominantly expressed in spinal astrocytes. Several studies also demonstrated an induction of CXCL1 by astrocytes in the central nervous system (CNS) in pathological conditions. Pineau et al. reported that CXCL1 mRNA is upregulated in the spinal astrocytes after spinal cord injury in mice [54]. CXCL1 is induced in brain astrocytes by neuronal injury and intracerebroventricular administration of endothelin-1 [31,37]. In humans, CXCL1 is selectively expressed in hypertropic astrocytes after active multiple sclerosis lesions [52,53]. In addition, several studies show that CXCL1 is produced in cultured astrocytes after incubation with lipopolysaccharide, NOV/CCN3, IL-1β, or infection with the murine encephalomyelitis virus [16,38,52,60].
RNA interference (RNAi), which can induce loss-of function phenotypes by post-transcriptional silencing of gene expression, has shown potential as a therapeutic strategy [64]. Viral vector-mediated RNAi can induce stable and long-term gene silencing [44] and has been shown effective in inhibiting gene expression in a number of diseases [8]. In this study, intrathecal injection of CXCL1 neutralizing antibody only transiently and partly attenuated SNL-induced mechanical allodynia and heat hyperalgesia. In contrast, LV-shCXCL1 showed a markedly and persistent antihyperalgesia and antiallodynia effect in SNL mice, suggesting CXCL1 play an important role in the maintenance of neuropathic pain. It is noteworthy that LV-shCXCL1 alleviated, not completely reversed the SNL-induced pain hypersensitivity, which may attribute to two possibilities. First, intraspinal infusion LV-shCXCL1 0.8 μl (640 TU) did not completely block CXCL1 expression (about 45% knockdown); Second, CXCL1 plays a partial role in the maintenance of neuropathic pain. Our previous studies have shown that SNL induces chemokine CCL2 production, which has been demonstrated to be involved in central sensitization and neuropathic pain [20].
TNF-α/JNK is the upstream of CXCL1 production in astrocytes in neuropathic pain
Our results showed that CXCL1 upregulation started from 3 days after SNL. However, the pain hypersensitivity was induced at 1 day, suggesting CXCL1 upregulation may be secondary to the change of other mediators. Indeed, SNL induced rapid (1 day) TNF-α mRNA increase and TNF-α inhibitor blocked SNL-induced CXCL1 mRNA increase at 3 days after SNL. Intrathecal injection of TNF-α also increased CXCL1 expression at the spinal cord. These data indicate that TNF-α is necessary and sufficient to the CXCL1 upregulation in the spinal cord, especially in the early phase of SNL. Earlier reports demonstrated that antigen-induced hypernociception and the increase of CXCL1 was reduced in TNF receptor 1 (TNFR1) knockout mice [11], further supporting TNF-α is a trigger of CXCL1 production in both spinal cord and peripheral tissue.
JNK is one of the members of MAPK and has been shown to be expressed in astrocytes and upregulated in neuropathic pain conditions [42,81]. TNF-α-induced JNK activation regulates the production of various inflammatory mediators that may directly regulate the neuronal excitability [18,19]. Here we showed that CXCL1 is one of chemokines that was produced by astrocytes following JNK activation in cultured astrocytes. In vivo data further showed that JNK inhibitor reduced SNL-induced pain and CXCL1 expression in the spinal cord. These results indicate CXCL1 is an important downstream of JNK activation in mediating the process of neuropathic pain.
CXCL1/CXCR2 signaling in central sensitization and neuropathic pain
Chemokines act through a family of seven transmembrane G protein-coupled receptors to exert their biological effects. CXCL1 acts through CXCR2 receptor, which also binds other chemokines, such as CXCL2 and CXCL3 [5,61]. The CXCR2 receptor has been detected on neurons [24,68], oligodendrocyte progenitors [51,53], and microglia [15,55] in brain. Several studies suggest that CXCL1-acting through CXCR2 on oligodendrocyte progenitors, promotes oligodendrogenesis in the CNS of rodents and humans [15,51,59,67]. In the DRG, CXCR2 are expressed in neurons and CXCL1 increases the sodium currents, potassium currents in small diameter rat sensory neurons [71,77], suggesting the direct pro-nociceptive effects of CXCL1. In this study, intrathecal injection of CXCL1 induced heat hyperalgesia, which was blocked by pretreatment with CXCR2 antagonist, SB225002. Additionally, CXCR2 was expressed on neurons of the spinal cord. Both immunostaining and western blot showed that SNL increased CXCR2 expression in the spinal cord. Behavioral results further demonstrated that CXCR2 antagonist attenuated SNL-induced pain hypersensitivity at 3 days after SNL in a dose-dependent manner, suggesting the involvement of CXCR2 in neuropathic pain.
Accumulating evidence suggests that proinflammatory cytokines and chemokines may be directly involved in regulating neuronal activity in the dorsal horn [20,21,33]. For example, perfusion of spinal slices with IL-1β or chemokine CCL2 increases the frequency and amplitude of spontaneous postsynaptic currents and markedly enhances NMDA-induced currents in dorsal horn neurons [20,33]. Here, intrathecal injection of CXCL1 induced rapid ERK and CREB activation and c-Fos expression mainly in spinal cord neurons. The ERK pathway plays an important role in neuronal plasticity and central sensitization [27,30]. The translocated pERK activates transcription factors including CREB and regulating gene transcription to maintain central sensitization and nerve-injury pain [28]. CREB binding sites (CREs) are shown in the promoter regions of the genes encoding c-Fos, COX-2, NK-1, prodynorphin, and TrkB, which are important for the genesis of chronic pain. We observed that CXCL1 induced CXCR2-dependent mRNA increase of COX-2 in the spinal cord (unpublished observation), suggesting CXCL1 may be involved in the maintenance of central sensitization and neuropathic pain in part through upregulation of pain-related proteins.
Besides the central effect of CXCL1/CXCR2 on pain, it has been reported that CXCL1/CXCR2 interaction is involved in neutrophil recruitment in the peripheral tissue and mediates carrageenan-induced inflammatory pain [9,10] and paw incision-induced post-incisional pain [4]. Whether spinal nerve ligation could induce the CXCL1/CXCR2-mediated neutrophil accumulation in local tissue and further induce the induction of neuropathic pain needs to be investigated in the future.
Conclusions
Nerve injury has been shown to upregulate several chemokines in the spinal cord to enhance neuropathic pain via neuron-glia interactions. It is of great interest that different chemokines mediate distinct neuron-glia interactions. In the CNS, chemokines and their respective receptors are often detected in different cell types to mediate cell-cell interactions. In the spinal cord, neurons and microglia have been shown to express chmokines (CX3CL1/fractalkine, CCL2, CCL21) and chemokine receptors (CX3CR1, CCR2, CCR7/CXCR3), respectively [3,12,20,21,23,36,41,47,66,69,78,79], indicating an important role of chemokine signaling in neuron-initiated microglial activation. However, astrocytes and neurons have also been shown to express CCL2 and CCR2, respectively [20,21,36], suggesting distinct signaling from astrocytes to neurons. In this study we demonstrated another mechanism of chemokine-mediated astrocyte to neuron signaling, by which astrocytes-produced CXCL1 acts on CXCR2-expressing dorsal horn neurons to elicit central sensitization and maintain neuropathic pain. This is also consistent with the studies demonstrating distinct role of microglia and astrocytes for the development and maintenance of neuropathic pain [6,13,48,57,78,81]. Of interest, nerve injury-induced CXCL1 increase in astrocytes is more persistent than that of CCL2 [20]. Thus, targeting different chemokine signaling could differentially regulate neuropathic pain in different phases. Given an important role of CXCL1/CXCR2 in the maintenance of neuropathic pain, inhibiting CXCL1/CXCR2 and astrocyte signaling may offer a novel therapeutic strategy for treating chronic neuropathic pain.
Supplementary Material
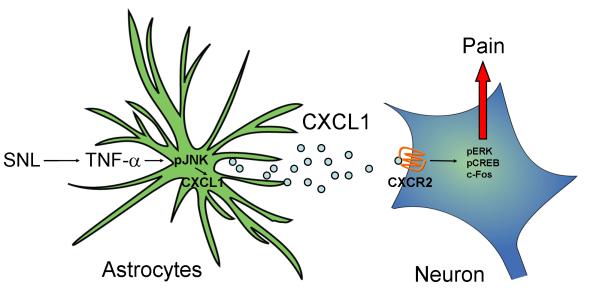
Figure 9.
Schematic shows how CXCL1 and CXCR2 in the spinal cord regulate neuropathic pain. SNL rapidly increases TNF-α expression, which acts on astrocytes to induce JNK activation, leading to the production of CXCL1. Upon release from astrocytes, CXCL1 acts on CXCR2 in neurons and induces the expression of pERK, pCREB, c-Fos, leading to the expression of late-response genes and subsequent maintenance of neuropathic pain.
Acknowledgements
This study was supported by the National Natural Science Foundation of China (NSFC) 31171062, the Program for New Century Excellent Talents NCET-09-0164, the Natural Science Foundation of Jiangsu Province BK2010273 to YJG, and a project funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions. RRJ is supported in part by NIH grants DE17794 and DE22743.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
References
- [1].Abbadie C. Chemokines, chemokine receptors and pain. Trends in immunology. 2005;26:529–534. doi: 10.1016/j.it.2005.08.001. [DOI] [PubMed] [Google Scholar]
- [2].Abbadie C, Bhangoo S, De Koninck Y, Malcangio M, Melik-Parsadaniantz S, White FA. Chemokines and pain mechanisms. Brain research reviews. 2009;60:125–134. doi: 10.1016/j.brainresrev.2008.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Abbadie C, Lindia JA, Cumiskey AM, Peterson LB, Mudgett JS, Bayne EK, DeMartino JA, MacIntyre DE, Forrest MJ. Impaired neuropathic pain responses in mice lacking the chemokine receptor CCR2. Proceedings of the National Academy of Sciences of the United States of America. 2003;100:7947–7952. doi: 10.1073/pnas.1331358100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Carreira EU, Carregaro V, Teixeira MM, Moriconi A, Aramini A, Verri WA, Jr., Ferreira SH, Cunha FQ, Cunha TM. Neutrophils recruited by CXCR1/2 signalling mediate post-incisional pain. European journal of pain (London, England) 2013;17:654–663. doi: 10.1002/j.1532-2149.2012.00240.x. [DOI] [PubMed] [Google Scholar]
- [5].Cartier L, Hartley O, Dubois-Dauphin M, Krause KH. Chemokine receptors in the central nervous system: role in brain inflammation and neurodegenerative diseases. Brain Res Brain Res Rev. 2005;48:16–42. doi: 10.1016/j.brainresrev.2004.07.021. [DOI] [PubMed] [Google Scholar]
- [6].Cavaliere C, Cirillo G, Rosaria Bianco M, Rossi F, De Novellis V, Maione S, Papa M. Gliosis alters expression and uptake of spinal glial amino acid transporters in a mouse neuropathic pain model. Neuron glia biology. 2007;3:141–153. doi: 10.1017/S1740925X07000695. [DOI] [PubMed] [Google Scholar]
- [7].Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL. Quantitative assessment of tactile allodynia in the rat paw. Journal of neuroscience methods. 1994;53:55–63. doi: 10.1016/0165-0270(94)90144-9. [DOI] [PubMed] [Google Scholar]
- [8].Couto LB, High KA. Viral vector-mediated RNA interference. Curr Opin Pharmacol. 2010;10:534–542. doi: 10.1016/j.coph.2010.06.007. [DOI] [PubMed] [Google Scholar]
- [9].Cunha TM, Verri WA, Jr., Schivo IR, Napimoga MH, Parada CA, Poole S, Teixeira MM, Ferreira SH, Cunha FQ. Crucial role of neutrophils in the development of mechanical inflammatory hypernociception. J Leukoc Biol. 2008;83:824–832. doi: 10.1189/jlb.0907654. [DOI] [PubMed] [Google Scholar]
- [10].Cunha TM, Verri WA, Jr., Silva JS, Poole S, Cunha FQ, Ferreira SH. A cascade of cytokines mediates mechanical inflammatory hypernociception in mice. Proceedings of the National Academy of Sciences of the United States of America. 2005;102:1755–1760. doi: 10.1073/pnas.0409225102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Cunha TM, Verri WA, Jr., Valerio DA, Guerrero AT, Nogueira LG, Vieira SM, Souza DG, Teixeira MM, Poole S, Ferreira SH, Cunha FQ. Role of cytokines in mediating mechanical hypernociception in a model of delayed-type hypersensitivity in mice. European journal of pain (London, England) 2008;12:1059–1068. doi: 10.1016/j.ejpain.2008.02.003. [DOI] [PubMed] [Google Scholar]
- [12].Dansereau MA, Gosselin RD, Pohl M, Pommier B, Mechighel P, Mauborgne A, Rostene W, Kitabgi P, Beaudet N, Sarret P, Melik-Parsadaniantz S. Spinal CCL2 pronociceptive action is no longer effective in CCR2 receptor antagonist-treated rats. Journal of neurochemistry. 2008;106:757–769. doi: 10.1111/j.1471-4159.2008.05429.x. [DOI] [PubMed] [Google Scholar]
- [13].DeLeo JA, Tanga FY, Tawfik VL. Neuroimmune activation and neuroinflammation in chronic pain and opioid tolerance/hyperalgesia. Neuroscientist. 2004;10:40–52. doi: 10.1177/1073858403259950. [DOI] [PubMed] [Google Scholar]
- [14].Dong F, Du YR, Xie W, Strong JA, He XJ, Zhang JM. Increased function of the TRPV1 channel in small sensory neurons after local inflammation or in vitro exposure to the pro-inflammatory cytokine GRO/KC. Neurosci Bull. 2012;28:155–164. doi: 10.1007/s12264-012-1208-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Filipovic R, Jakovcevski I, Zecevic N. GRO-alpha and CXCR2 in the human fetal brain and multiple sclerosis lesions. Developmental neuroscience. 2003;25:279–290. doi: 10.1159/000072275. [DOI] [PubMed] [Google Scholar]
- [16].Fischer I, Alliod C, Martinier N, Newcombe J, Brana C, Pouly S. Sphingosine kinase 1 and sphingosine 1-phosphate receptor 3 are functionally upregulated on astrocytes under pro-inflammatory conditions. PLoS One. 2011;6:e23905. doi: 10.1371/journal.pone.0023905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Gao YJ, Ji RR. c-Fos and pERK, which is a better marker for neuronal activation and central sensitization after noxious stimulation and tissue injury? Open Pain J. 2009;2:11–17. doi: 10.2174/1876386300902010011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Gao YJ, Ji RR. Chemokines, neuronal-glial interactions, and central processing of neuropathic pain. Pharmacology & therapeutics. 2010;126:56–68. doi: 10.1016/j.pharmthera.2010.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Gao YJ, Ji RR. Targeting astrocyte signaling for chronic pain. Neurotherapeutics. 2010;7:482–493. doi: 10.1016/j.nurt.2010.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Gao YJ, Zhang L, Samad OA, Suter MR, Yasuhiko K, Xu ZZ, Park JY, Lind AL, Ma Q, Ji RR. JNK-induced MCP-1 production in spinal cord astrocytes contributes to central sensitization and neuropathic pain. J Neurosci. 2009;29:4096–4108. doi: 10.1523/JNEUROSCI.3623-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Gosselin RD, Varela C, Banisadr G, Mechighel P, Rostene W, Kitabgi P, Melik-Parsadaniantz S. Constitutive expression of CCR2 chemokine receptor and inhibition by MCP-1/CCL2 of GABA-induced currents in spinal cord neurones. Journal of neurochemistry. 2005;95:1023–1034. doi: 10.1111/j.1471-4159.2005.03431.x. [DOI] [PubMed] [Google Scholar]
- [22].Guerrero AT, Cunha TM, Verri WA, Jr., Gazzinelli RT, Teixeira MM, Cunha FQ, Ferreira SH. Toll-like receptor 2/MyD88 signaling mediates zymosan-induced joint hypernociception in mice: participation of TNF-alpha, IL-1beta and CXCL1/KC. Eur J Pharmacol. 2012;674:51–57. doi: 10.1016/j.ejphar.2011.10.023. [DOI] [PubMed] [Google Scholar]
- [23].Harrison JK, Jiang Y, Chen S, Xia Y, Maciejewski D, McNamara RK, Streit WJ, Salafranca MN, Adhikari S, Thompson DA, Botti P, Bacon KB, Feng L. Role for neuronally derived fractalkine in mediating interactions between neurons and CX3CR1-expressing microglia. Proceedings of the National Academy of Sciences of the United States of America. 1998;95:10896–10901. doi: 10.1073/pnas.95.18.10896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Horuk R, Martin AW, Wang Z, Schweitzer L, Gerassimides A, Guo H, Lu Z, Hesselgesser J, Perez HD, Kim J, Parker J, Hadley TJ, Peiper SC. Expression of chemokine receptors by subsets of neurons in the central nervous system. J Immunol. 1997;158:2882–2890. [PubMed] [Google Scholar]
- [25].Hylden JL, Wilcox GL. Intrathecal morphine in mice: a new technique. European journal of pharmacology. 1980;67:313–316. doi: 10.1016/0014-2999(80)90515-4. [DOI] [PubMed] [Google Scholar]
- [26].Inoue K. The function of microglia through purinergic receptors: neuropathic pain and cytokine release. Pharmacology & therapeutics. 2006;109:210–226. doi: 10.1016/j.pharmthera.2005.07.001. [DOI] [PubMed] [Google Scholar]
- [27].Ji RR, Baba H, Brenner GJ, Woolf CJ. Nociceptive-specific activation of ERK in spinal neurons contributes to pain hypersensitivity. Nature neuroscience. 1999;2:1114–1119. doi: 10.1038/16040. [DOI] [PubMed] [Google Scholar]
- [28].Ji RR, Strichartz G. Cell signaling and the genesis of neuropathic pain. Sci STKE. 2004;2004:reE14. doi: 10.1126/stke.2522004re14. [DOI] [PubMed] [Google Scholar]
- [29].Johnson EA, Dao TL, Guignet MA, Geddes CE, Koemeter-Cox AI, Kan RK. Increased expression of the chemokines CXCL1 and MIP-1alpha by resident brain cells precedes neutrophil infiltration in the brain following prolonged soman-induced status epilepticus in rats. Journal of neuroinflammation. 2011;8:41. doi: 10.1186/1742-2094-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Karim F, Wang CC, Gereau RWt. Metabotropic glutamate receptor subtypes 1 and 5 are activators of extracellular signal-regulated kinase signaling required for inflammatory pain in mice. J Neurosci. 2001;21:3771–3779. doi: 10.1523/JNEUROSCI.21-11-03771.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Katayama T, Tanaka H, Yoshida T, Uehara T, Minami M. Neuronal injury induces cytokine-induced neutrophil chemoattractant-1 (CINC-1) production in astrocytes. J Pharmacol Sci. 2009;109:88–93. doi: 10.1254/jphs.08298fp. [DOI] [PubMed] [Google Scholar]
- [32].Kawasaki Y, Xu ZZ, Wang X, Park JY, Zhuang ZY, Tan PH, Gao YJ, Roy K, Corfas G, Lo EH, Ji RR. Distinct roles of matrix metalloproteases in the early- and late-phase development of neuropathic pain. Nature medicine. 2008;14:331–336. doi: 10.1038/nm1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Kawasaki Y, Zhang L, Cheng JK, Ji RR. Cytokine mechanisms of central sensitization: distinct and overlapping role of interleukin-1beta, interleukin-6, and tumor necrosis factor-alpha in regulating synaptic and neuronal activity in the superficial spinal cord. J Neurosci. 2008;28:5189–5194. doi: 10.1523/JNEUROSCI.3338-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Kiguchi N, Kobayashi Y, Kishioka S. Chemokines and cytokines in neuroinflammation leading to neuropathic pain. Curr Opin Pharmacol. 2012;12:55–61. doi: 10.1016/j.coph.2011.10.007. [DOI] [PubMed] [Google Scholar]
- [35].Kim SH, Chung JM. An experimental model for peripheral neuropathy produced by segmental spinal nerve ligation in the rat. Pain. 1992;50:355–363. doi: 10.1016/0304-3959(92)90041-9. [DOI] [PubMed] [Google Scholar]
- [36].Knerlich-Lukoschus F, Juraschek M, Blomer U, Lucius R, Mehdorn HM, Held-Feindt J. Force-dependent development of neuropathic central pain and time-related CCL2/CCR2 expression after graded spinal cord contusion injuries of the rat. Journal of neurotrauma. 2008;25:427–448. doi: 10.1089/neu.2007.0431. [DOI] [PubMed] [Google Scholar]
- [37].Koyama Y, Baba A, Matsuda T. Production of monocyte chemoattractant protein-1 and cytokine-induced neutrophil chemoattractant-1 in rat brain is stimulated by intracerebroventricular administration of an endothelin ETB receptor agonist. Neuroreport. 2007;18:1275–1279. doi: 10.1097/WNR.0b013e32825a67f1. [DOI] [PubMed] [Google Scholar]
- [38].Le Dreau G, Kular L, Nicot AB, Calmel C, Melik-Parsadaniantz S, Kitabgi P, Laurent M, Martinerie C. NOV/CCN3 upregulates CCL2 and CXCL1 expression in astrocytes through beta1 and beta5 integrins. Glia. 2010;58:1510–1521. doi: 10.1002/glia.21025. [DOI] [PubMed] [Google Scholar]
- [39].Lee HL, Lee KM, Son SJ, Hwang SH, Cho HJ. Temporal expression of cytokines and their receptors mRNAs in a neuropathic pain model. Neuroreport. 2004;15:2807–2811. [PubMed] [Google Scholar]
- [40].Li H, Xie W, Strong JA, Zhang JM. Systemic antiinflammatory corticosteroid reduces mechanical pain behavior, sympathetic sprouting, and elevation of proinflammatory cytokines in a rat model of neuropathic pain. Anesthesiology. 2007;107:469–477. doi: 10.1097/01.anes.0000278907.37774.8d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Lindia JA, McGowan E, Jochnowitz N, Abbadie C. Induction of CX3CL1 expression in astrocytes and CX3CR1 in microglia in the spinal cord of a rat model of neuropathic pain. J Pain. 2005;6:434–438. doi: 10.1016/j.jpain.2005.02.001. [DOI] [PubMed] [Google Scholar]
- [42].Ma W, Quirion R. Partial sciatic nerve ligation induces increase in the phosphorylation of extracellular signal-regulated kinase (ERK) and c-Jun N-terminal kinase (JNK) in astrocytes in the lumbar spinal dorsal horn and the gracile nucleus. Pain. 2002;99:175–184. doi: 10.1016/s0304-3959(02)00097-0. [DOI] [PubMed] [Google Scholar]
- [43].Malmberg AB, Chen C, Tonegawa S, Basbaum AI. Preserved acute pain and reduced neuropathic pain in mice lacking PKCgamma. Science (New York, NY. 1997;278:279–283. doi: 10.1126/science.278.5336.279. [DOI] [PubMed] [Google Scholar]
- [44].Manjunath N, Wu H, Subramanya S, Shankar P. Lentiviral delivery of short hairpin RNAs. Adv Drug Deliv Rev. 2009;61:732–745. doi: 10.1016/j.addr.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].McTigue DM, Tani M, Krivacic K, Chernosky A, Kelner GS, Maciejewski D, Maki R, Ransohoff RM, Stokes BT. Selective chemokine mRNA accumulation in the rat spinal cord after contusion injury. J Neurosci Res. 1998;53:368–376. doi: 10.1002/(SICI)1097-4547(19980801)53:3<368::AID-JNR11>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- [46].Mennicken F, Maki R, de Souza EB, Quirion R. Chemokines and chemokine receptors in the CNS: a possible role in neuroinflammation and patterning. Trends in pharmacological sciences. 1999;20:73–78. doi: 10.1016/s0165-6147(99)01308-5. [DOI] [PubMed] [Google Scholar]
- [47].Miller RJ, Rostene W, Apartis E, Banisadr G, Biber K, Milligan ED, White FA, Zhang J. Chemokine action in the nervous system. J Neurosci. 2008;28:11792–11795. doi: 10.1523/JNEUROSCI.3588-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Milligan ED, Twining C, Chacur M, Biedenkapp J, O’Connor K, Poole S, Tracey K, Martin D, Maier SF, Watkins LR. Spinal glia and proinflammatory cytokines mediate mirror-image neuropathic pain in rats. J Neurosci. 2003;23:1026–1040. doi: 10.1523/JNEUROSCI.23-03-01026.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Milligan ED, Watkins LR. Pathological and protective roles of glia in chronic pain. Nature reviews. 2009;10:23–36. doi: 10.1038/nrn2533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Neumann S, Braz JM, Skinner K, Llewellyn-Smith IJ, Basbaum AI. Innocuous, not noxious, input activates PKCgamma interneurons of the spinal dorsal horn via myelinated afferent fibers. J Neurosci. 2008;28:7936–7944. doi: 10.1523/JNEUROSCI.1259-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Nguyen D, Stangel M. Expression of the chemokine receptors CXCR1 and CXCR2 in rat oligodendroglial cells. Brain Res Dev Brain Res. 2001;128:77–81. doi: 10.1016/s0165-3806(01)00128-6. [DOI] [PubMed] [Google Scholar]
- [52].Omari KM, John G, Lango R, Raine CS. Role for CXCR2 and CXCL1 on glia in multiple sclerosis. Glia. 2006;53:24–31. doi: 10.1002/glia.20246. [DOI] [PubMed] [Google Scholar]
- [53].Omari KM, John GR, Sealfon SC, Raine CS. CXC chemokine receptors on human oligodendrocytes: implications for multiple sclerosis. Brain. 2005;128:1003–1015. doi: 10.1093/brain/awh479. [DOI] [PubMed] [Google Scholar]
- [54].Pineau I, Sun L, Bastien D, Lacroix S. Astrocytes initiate inflammation in the injured mouse spinal cord by promoting the entry of neutrophils and inflammatory monocytes in an IL-1 receptor/MyD88-dependent fashion. Brain, behavior, and immunity. 2010;24:540–553. doi: 10.1016/j.bbi.2009.11.007. [DOI] [PubMed] [Google Scholar]
- [55].Popivanova BK, Koike K, Tonchev AB, Ishida Y, Kondo T, Ogawa S, Mukaida N, Inoue M, Yamashima T. Accumulation of microglial cells expressing ELR motif-positive CXC chemokines and their receptor CXCR2 in monkey hippocampus after ischemiareperfusion. Brain Res. 2003;970:195–204. doi: 10.1016/s0006-8993(03)02343-6. [DOI] [PubMed] [Google Scholar]
- [56].Qin X, Wan Y, Wang X. CCL2 and CXCL1 trigger calcitonin gene-related peptide release by exciting primary nociceptive neurons. J Neurosci Res. 2005;82:51–62. doi: 10.1002/jnr.20612. [DOI] [PubMed] [Google Scholar]
- [57].Raghavendra V, Tanga F, DeLeo JA. Inhibition of microglial activation attenuates the development but not existing hypersensitivity in a rat model of neuropathy. The Journal of pharmacology and experimental therapeutics. 2003;306:624–630. doi: 10.1124/jpet.103.052407. [DOI] [PubMed] [Google Scholar]
- [58].Ren K, Dubner R. Neuron-glia crosstalk gets serious: role in pain hypersensitivity. Current opinion in anaesthesiology. 2008;21:570–579. doi: 10.1097/ACO.0b013e32830edbdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Robinson S, Tani M, Strieter RM, Ransohoff RM, Miller RH. The chemokine growth-regulated oncogene-alpha promotes spinal cord oligodendrocyte precursor proliferation. J Neurosci. 1998;18:10457–10463. doi: 10.1523/JNEUROSCI.18-24-10457.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Rubio N, Sanz-Rodriguez F. Induction of the CXCL1 (KC) chemokine in mouse astrocytes by infection with the murine encephalomyelitis virus of Theiler. Virology. 2007;358:98–108. doi: 10.1016/j.virol.2006.08.003. [DOI] [PubMed] [Google Scholar]
- [61].Savarin-Vuaillat C, Ransohoff RM. Chemokines and chemokine receptors in neurological disease: raise, retain, or reduce? Neurotherapeutics. 2007;4:590–601. doi: 10.1016/j.nurt.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Schafers M, Svensson CI, Sommer C, Sorkin LS. Tumor necrosis factor-alpha induces mechanical allodynia after spinal nerve ligation by activation of p38 MAPK in primary sensory neurons. J Neurosci. 2003;23:2517–2521. doi: 10.1523/JNEUROSCI.23-07-02517.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Scholz J, Woolf CJ. The neuropathic pain triad: neurons, immune cells and glia. Nature neuroscience. 2007;10:1361–1368. doi: 10.1038/nn1992. [DOI] [PubMed] [Google Scholar]
- [64].Shrey K, Suchit A, Nishant M, Vibha R. RNA interference: emerging diagnostics and therapeutics tool. Biochemical and biophysical research communications. 2009;386:273–277. doi: 10.1016/j.bbrc.2009.06.018. [DOI] [PubMed] [Google Scholar]
- [65].Sommer C, Lindenlaub T, Teuteberg P, Schafers M, Hartung T, Toyka KV. Anti-TNF-neutralizing antibodies reduce pain-related behavior in two different mouse models of painful mononeuropathy. Brain Res. 2001;913:86–89. doi: 10.1016/s0006-8993(01)02743-3. [DOI] [PubMed] [Google Scholar]
- [66].Thacker MA, Clark AK, Bishop T, Grist J, Yip PK, Moon LD, Thompson SW, Marchand F, McMahon SB. CCL2 is a key mediator of microglia activation in neuropathic pain states. European journal of pain (London, England) 2009;13:263–272. doi: 10.1016/j.ejpain.2008.04.017. [DOI] [PubMed] [Google Scholar]
- [67].Tsai HH, Frost E, To V, Robinson S, Ffrench-Constant C, Geertman R, Ransohoff RM, Miller RH. The chemokine receptor CXCR2 controls positioning of oligodendrocyte precursors in developing spinal cord by arresting their migration. Cell. 2002;110:373–383. doi: 10.1016/s0092-8674(02)00838-3. [DOI] [PubMed] [Google Scholar]
- [68].Valles A, Grijpink-Ongering L, de Bree FM, Tuinstra T, Ronken E. Differential regulation of the CXCR2 chemokine network in rat brain trauma: implications for neuroimmune interactions and neuronal survival. Neurobiol Dis. 2006;22:312–322. doi: 10.1016/j.nbd.2005.11.015. [DOI] [PubMed] [Google Scholar]
- [69].Verge GM, Milligan ED, Maier SF, Watkins LR, Naeve GS, Foster AC. Fractalkine (CX3CL1) and fractalkine receptor (CX3CR1) distribution in spinal cord and dorsal root ganglia under basal and neuropathic pain conditions. Eur J Neurosci. 2004;20:1150–1160. doi: 10.1111/j.1460-9568.2004.03593.x. [DOI] [PubMed] [Google Scholar]
- [70].Verri WA, Jr., Cunha TM, Parada CA, Poole S, Cunha FQ, Ferreira SH. Hypernociceptive role of cytokines and chemokines: targets for analgesic drug development? Pharmacology & therapeutics. 2006;112:116–138. doi: 10.1016/j.pharmthera.2006.04.001. [DOI] [PubMed] [Google Scholar]
- [71].Wang JG, Strong JA, Xie W, Yang RH, Coyle DE, Wick DM, Dorsey ED, Zhang JM. The chemokine CXCL1/growth related oncogene increases sodium currents and neuronal excitability in small diameter sensory neurons. Mol Pain. 2008;4:38. doi: 10.1186/1744-8069-4-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Watkins LR, Milligan ED, Maier SF. Glial activation: a driving force for pathological pain. Trends in neurosciences. 2001;24:450–455. doi: 10.1016/s0166-2236(00)01854-3. [DOI] [PubMed] [Google Scholar]
- [73].White FA, Bhangoo SK, Miller RJ. Chemokines: integrators of pain and inflammation. Nat Rev Drug Discov. 2005;4:834–844. doi: 10.1038/nrd1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].White FA, Jung H, Miller RJ. Chemokines and the pathophysiology of neuropathic pain. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:20151–20158. doi: 10.1073/pnas.0709250104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Xie WR, Deng H, Li H, Bowen TL, Strong JA, Zhang JM. Robust increase of cutaneous sensitivity, cytokine production and sympathetic sprouting in rats with localized inflammatory irritation of the spinal ganglia. Neuroscience. 2006;142:809–822. doi: 10.1016/j.neuroscience.2006.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Xu JT, Xin WJ, Zang Y, Wu CY, Liu XG. The role of tumor necrosis factor-alpha in the neuropathic pain induced by Lumbar 5 ventral root transection in rat. Pain. 2006;123:306–321. doi: 10.1016/j.pain.2006.03.011. [DOI] [PubMed] [Google Scholar]
- [77].Yang RH, Strong JA, Zhang JM. NF-kappaB mediated enhancement of potassium currents by the chemokine CXCL1/growth related oncogene in small diameter rat sensory neurons. Mol Pain. 2009;5:26. doi: 10.1186/1744-8069-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Zhang J, De Koninck Y. Spatial and temporal relationship between monocyte chemoattractant protein-1 expression and spinal glial activation following peripheral nerve injury. Journal of neurochemistry. 2006;97:772–783. doi: 10.1111/j.1471-4159.2006.03746.x. [DOI] [PubMed] [Google Scholar]
- [79].Zhao P, Waxman SG, Hains BC. Modulation of thalamic nociceptive processing after spinal cord injury through remote activation of thalamic microglia by cysteine cysteine chemokine ligand 21. J Neurosci. 2007;27:8893–8902. doi: 10.1523/JNEUROSCI.2209-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Zhuang ZY, Kawasaki Y, Tan PH, Wen YR, Huang J, Ji RR. Role of the CX3CR1/p38 MAPK pathway in spinal microglia for the development of neuropathic pain following nerve injury-induced cleavage of fractalkine. Brain, behavior, and immunity. 2007;21:642–651. doi: 10.1016/j.bbi.2006.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Zhuang ZY, Wen YR, Zhang DR, Borsello T, Bonny C, Strichartz GR, Decosterd I, Ji RR. A peptide c-Jun N-terminal kinase (JNK) inhibitor blocks mechanical allodynia after spinal nerve ligation: respective roles of JNK activation in primary sensory neurons and spinal astrocytes for neuropathic pain development and maintenance. J Neurosci. 2006;26:3551–3560. doi: 10.1523/JNEUROSCI.5290-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.