Abstract
Suprascapular nerve (SSN) entrapment is an uncommon cause of posterior shoulder pain. Entrapment can be relieved arthroscopically in some cases.
Keywords: suprascapular nerve entrapment, suprascapular nerve release, suprascapular notch
Suprascapular nerve (SSN) entrapment at the suprascapular notch is an uncommon cause of shoulder pathology that often presents with posterior shoulder pain and wasting of the supraspinatus (SS) and infraspinatus (IS) muscles.11 Because of the rarity of this condition, its diagnosis can be missed for months or years; therefore, proper diagnosis and treatment is crucial to prevent muscle wasting and atrophy.11,17 The anatomy makes it susceptible to static and dynamic compression, yet the vague symptoms accompanying this disorder often make it difficult to correctly diagnose.12 Patients with suprascapular neuropathy often describe dull aching pain 3 to 4 cm medial to the posterolateral corner of the spine of the scapula.12 The Suprascapular Nerve Stretch Test can help guide the physical examination when assessing SSN entrapment (Figure 1).11 This test reproduces posterior shoulder pain by laterally rotating the patient’s head away from the involved shoulder while the clinician depresses/retracts the involved shoulder with his or her other hand.11 Magnetic resonance imaging (MRI) scans can assess soft tissue causes of entrapment as well as associated pathology.17 Clinical suspicion from the history and physical examination should help establish a diagnosis of suprascapular neuropathy, and nerve conduction studies are used to confirm the diagnosis.12
Figure 1.
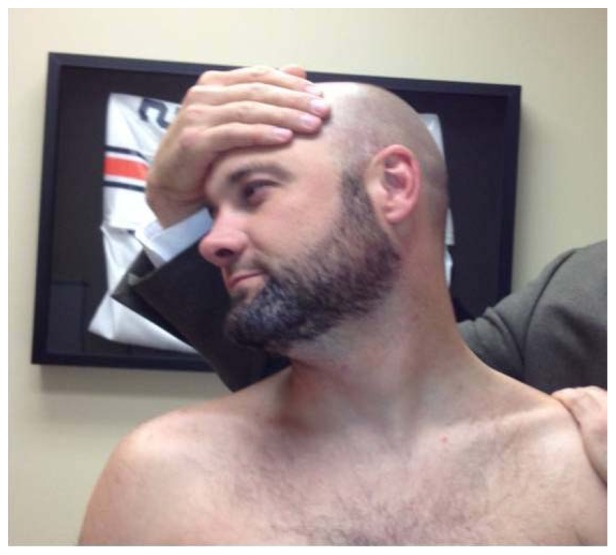
Lafosse Suprascapular Nerve Stretch Test.13
There are 6 anatomic variations of the suprascapular notch.15,16 A type V notch has a partially ossified transverse scapular ligament (TSL), and a type VI notch is a completely ossified TSL.15,16
A second classification system analyzed 423 cadaveric scapulas to classify the varying morphology into 5 types: type I, no discrete notch (8.3%); type II, notch with longer transverse than vertical diameter (41.85%); type III, notch with longer vertical diameter (41.85%); type IV, a bony foramen (7.3%); and type V, a notch and a bony foramen (0.7%) (Table 1).13
Table 1.
Suprascapular notch types13
| Type | Description | Frequency, % |
|---|---|---|
| I | No discrete notch | 8.3 |
| II | Notch having a greater transverse diameter | 41.85 |
| III | Notch having a greater vertical diameter | 41.85 |
| IV | Bony foramen | 7.3 |
| V | Both a notch and a bony foramen | 0.7 |
Case Report
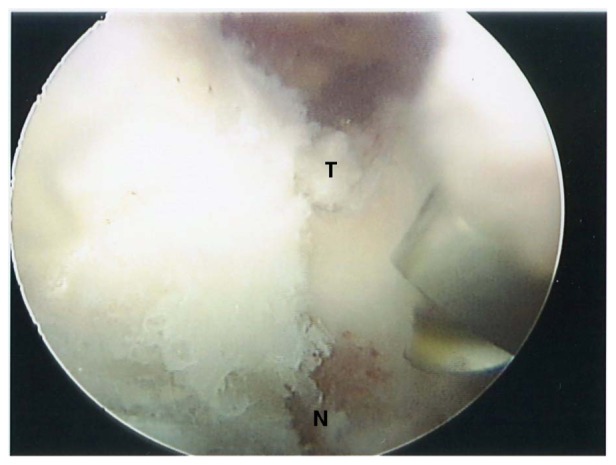
A 51-year-old man presented with increasing posterior shoulder pain with slight atrophy of the SS and IS. He had break-away weakness of the SS and IS without sensory deficits. Radiography revealed a small area of calcific tendinitis in the supraspinatus tendon (Figure 2). The MRI showed no rotator cuff tear, perilabral cyst, or other mass. A nerve conduction study revealed mononeuropathy of the SSN.
Figure 2.

Small calcification laterally at the supraspinatus insertion.
At surgery, a posterior lateral portal was established in the subacromial space for visualization. Using a lateral portal in the subacromial space, a shaver was used to debride the calcium deposits on the SS tendon. This was a very small area that was superficial at the lateral insertion of the SS tendon.
Arthroscopic dissection to the SSN began with identification of the coracoacromial ligament (CA) ligament progressing to the coracoid process, the coracoclavicular ligament (CC) ligaments, the posterior aspect of the conoid ligament, and the TSL. The suprascapular artery was identified and retracted medially. With a 70° scope, the SSN was identified on the anterior aspect of the scapula. The trajectory was followed and it came out in a foramen in the supraspinatus fossa adjacent to the base of the coracoid process. This was a congenital foramen and not an ossified ligament (Figure 3). An arthroscopic burr was introduced. Meticulous debridement of the bone was performed. A trough was created in the bone to free the SSN with the shield of the burr toward the nerve to protect it at all times (Figures 4-6). The nerve was probed, inspected, and released from the notch (Figure 7).
Figure 3.

Suprascapular foramen (circle) with the suprascapular nerve (N) and bone (B) superiorly where transverse scapular ligament normally sits.
Figure 4.
Creating a trough (T) in the notch for the suprascapular nerve (N) inferiorly within the foramen.
Figure 6.
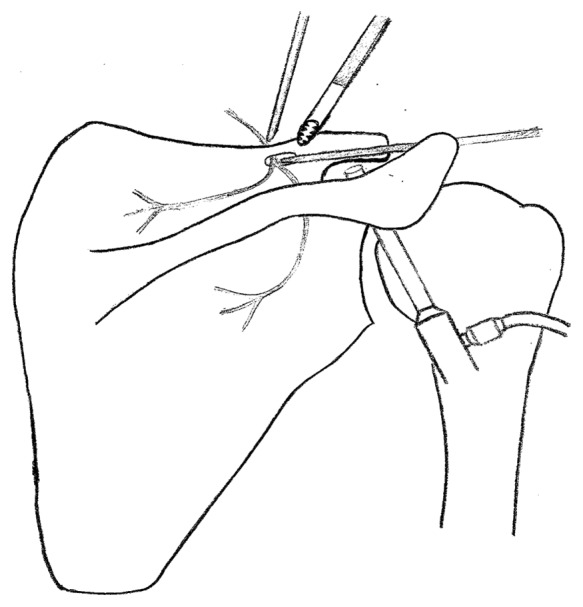
Decompress the suprascapular nerve entrapped in the bony foramen. Switching stick anterior to the scapula from the more medial portal and another posterior to the bony foramen coming from the lateral portal to protect and hold the nerve inferomedially.
Figure 7.

The suprascapular nerve (N) freed up and mobilized with a probe.
Figure 5.
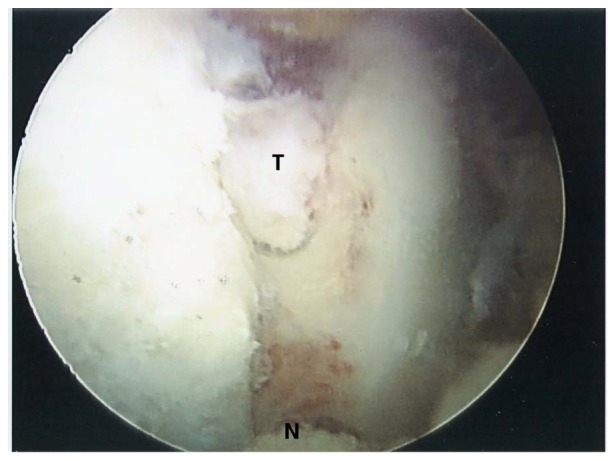
Trough (T) being created for the suprascapular nerve (N).
At 6 months postoperatively, the patient had recovered nearly 100% of his SS and IS strength with manual muscle testing. No postoperative electromyography (EMG) was performed because symptoms improved.
Discussion
The SSN is a sensorimotor nerve that originates from the upper trunk of the brachial plexus and is deep to the omohyoid and trapezius before traveling under the TSL in the suprascapular notch, giving 2 motor branches to the SS muscle.17,18 It terminates in the IS muscle.18 The sensory branches supply the acromioclavicular and glenohumeral joints.4 When compression occurs at the spinoglenoid notch, minimal pain is noted, but isolated infraspinatus atrophy may be seen.18 Primary compression is seen when there is stretching or tenting of the nerve.11 Secondary compression is associated with massive, retracted rotator cuff tears.11
There are many possible causes for compression of the SSN.4,5,7,9,11,14,18 Hypertrophy and/or ossification of the TSL or a narrowed bony foramen can predispose the nerve to entrapment.1,4,15,16,18 Frequent protraction may predispose the nerve to compression/traction injury specifically with cross-body adduction and internal rotation.2
Traction injury due to repetitive overhead activities (volleyball players) is common.10,22 Massive rotator cuff tears may stretch the nerve, and a 39% SSN neuropathy incidence has been found in massive cuff tears.11
Subscapularis muscle fibers may also play a role in SSN pathology.4 In 5 of 32 cadaver shoulders the subscapularis completely covered the anterior surface of the suprascapular notch.4
SSN compression can also occur at the spinoglenoid notch, causing isolated infraspinatus weakness.2,17 Spinoglenoid cysts often associated with labral pathology can also cause entrapment.18,21 Enlarged spinoglenoid notch veins can also cause SSN compression.6,19 Massive rotator cuff repair may improve suprascapular neuropathy by decreasing the tension/traction of the nerve.8,20 Pain relief may occur in patients with suprascapular notch release; however, strength returns are often less predictable.3,12
Footnotes
The authors report no potential conflicts of interest in the development and publication of this manuscript.
References
- 1. Agrawal V. Arthroscopic decompression of a bony suprascapular foramen. Arthroscopy. 2009;25(3):325-328 [DOI] [PubMed] [Google Scholar]
- 2. Aiello I, Serra G, Traina GC, Tugnoli V. Entrapment of the suprascapular nerve at the spinoglenoid notch. Ann Neurol. 1982;12(3):314-316 [DOI] [PubMed] [Google Scholar]
- 3. Antoniadis G, Richter HP, Rath S, Braun V, Moese G. Suprascapular nerve entrapment: experience with 28 cases. J Neurosurgery. 1996;85:1020-1025 [DOI] [PubMed] [Google Scholar]
- 4. Bayramoglu A, Demiryurek D, Tuccar E, et al. Variations in anatomy at the suprascapular notch possibly causing suprascapular nerve entrapment: an anatomical study. Knee Surg Sports Traumatol Arthrosc. 2003;11:393-398 [DOI] [PubMed] [Google Scholar]
- 5. Bigliani LU, Dalsey RM, McCann PD, April EW. An anatomical study of the suprascaular nerve. Arthroscopy. 1990;6:301-305 [DOI] [PubMed] [Google Scholar]
- 6. Caroll KW, Helms CA, Otte MT, Moelken SMC, Fritz R. Enlarged spinoglenoid notch veins causing suprascapular nerve compression. Skeletal Radiol. 2003;32(2):72-77 [DOI] [PubMed] [Google Scholar]
- 7. Cohen SB, Dines DM, Moorman CT. Familial calcification of the superior transverse scapular ligament causing neuropathy. Clin Orthop. 1997;334:131-135 [PubMed] [Google Scholar]
- 8. Costouros JB, Porramatikul M, Lie DT, Warner JJ. Reversal of suprascapular neuropathy following arthroscopic repair of massive supraspinatus and infraspinatus rotator cuff tears. Arthroscopy. 2007;23:1152-1161 [DOI] [PubMed] [Google Scholar]
- 9. Duparc F, Coquerel D, Ozeel J, Noyon M, Geronmetta A, Michot C. Anatomical basis of the suprascapular nerve entrapment and clinical relevance of the supraspinatus fascia. Surg Radiolog Anat. 2010;32(3):277-284 [DOI] [PubMed] [Google Scholar]
- 10. Ferretti A, De Carli A, Fontana M. Injury of the suprascapular nerve at the spinoglenoid notch. The natural history of infraspinatus atrophy in volleyball players. Am J Sports Med. 1998;26(6):759-763 [DOI] [PubMed] [Google Scholar]
- 11. Lafosse L, Piper K, Lanz U. Arthroscopic suprascapular nerve release: indications and technique. J Shoulder Elbow Surg. 2011;20:S9-13 [DOI] [PubMed] [Google Scholar]
- 12. Moen T, Babatunda O, Hsu S, Ahmad C, Levine W. Suprascapular neuropathy: what does the literature show? J Shoulder Elbow Surg. 2012;21:835-846 [DOI] [PubMed] [Google Scholar]
- 13. Natsis K, Totlis T, Tsikaras P, Appell HJ, Skandalakis P, Koebke J. Proposal for classification of the suprascapular notch: a study on 423 dried scapulas. Clin Anat. 2007;20(2):135-139 [DOI] [PubMed] [Google Scholar]
- 14. Polguj M, Jedrzejewski K, Podgorski M, Topol M. Morphometric study of the suprascapular notch: proposal of classification. Surg Radiol Anat. 2011;33(9):781-787 [DOI] [PubMed] [Google Scholar]
- 15. Rengachary SS, Burr D, Lucas S, Hassanein KM, Mohn MP, Matszke H. Suprascapular entrapment neuropathy; a clinical, anatomical and comparative study; part 2, anatomical study. Neurosurgery. 1979;5:447-451 [DOI] [PubMed] [Google Scholar]
- 16. Rengachary SS, Burr D, Lucas S, Brackett CE. Suprascapular entrapment neuropathy: a clinical, anatomical, and comparative study. Part 3: comparative study. Neurosurgery. 1979;5:452-455 [DOI] [PubMed] [Google Scholar]
- 17. Romeo AA, Ghodadra NS, Salata MJ, Provencher MT. Arthroscopic suprascapular nerve decompression: indications and surgical technique. J Shoulder Elbow Surg. 2010;19:S118-S123 [DOI] [PubMed] [Google Scholar]
- 18. Shah AA, Butler RB, Sung SY, Wells JH, Higgins LD, Warner JP. Clinical outcomes of suprascapular nerve decompression. J Shoulder Elbow Surg. 2011;20(6):975-982 [DOI] [PubMed] [Google Scholar]
- 19. Van Meir N, Fourneau I, Debeer P. Varicose veins at the spinoglenoidal notch: an unusual cause of suprascapular nerve compression. J Shoulder Elbow Surg. 2011;20(7):e21-e24 [DOI] [PubMed] [Google Scholar]
- 20. Warner JJP, Krushell RJ, Masquelet A, Gerber C. Anatomy and relationships of the suprascapular nerve: anatomical constraints to mobilization of the supraspinatus and infraspinatus muscles in the management of massive rotator-cuff tear. J Bone Joint Surg Am. 1992;74(1):36-45 [PubMed] [Google Scholar]
- 21. Westerheide KJ, Dopirak RM, Karzel RP, Snyder SJ. Suprascapular nerve palsy secondary to spinoglenoid cysts: results of arthroscopic treatment. Arthroscopy. 2006;22:721-727 [DOI] [PubMed] [Google Scholar]
- 22. Witvrouw E, Cools A, Lysens R, et al. Suprascapular neuropathy in volleyball players. Br J Sports Med. 2000;34(3):174-180 [DOI] [PMC free article] [PubMed] [Google Scholar]


