Abstract
Context:
Low back injuries are the most common injury in golf. Best practice guidelines for rehabilitation and prevention of these injuries are helpful for health care professionals and all golfers.
Objective:
To establish a best practice clinical model for low back pain in golfers from diagnosis through treatment and rehabilitation to return to golf.
Evidence Acquisition:
The PubMed database and Google Scholar were searched from 1993 to 2012 with the following keywords: golf and low back injury, low back injury, golf and low back pain, golf injury prevention, golf modern swing, muscles in golf swing, low back rehabilitation, diaphragm, and core stability. All studies addressed in some manner the rehabilitation, prevention, or return to sport from low back injury, preferably in direct relation to golf, as well as muscle firing patterns used during the golf swing.
Results:
Best practice for rehabilitation and prevention of low back injury in golf appears to be through a multidisciplinary approach.
Conclusion:
Movement patterns, muscle imbalances, and type of swing utilized all have a direct effect on the forces applied to the spine during the golf swing and need to be assessed to prevent or rehabilitate injury. Understanding the golf swing and how the body works during the swing is necessary.
Keywords: golf, low back pain, injury, swing, rehabilitation
There are more than 26 million golfers in the United States, with an estimated 25% over the age of 65.34,38 According to Integrated Business Systems, the game was continuing to grow at a rate of 0.6% in 2011, with an outlook more favorable for the future as baby boomers retire and have more disposable income.15 Golf is a robust industry that is continuing to grow, especially among the over-65-year-old demographic.
As people age, spinal mobility and the ability to absorb forces applied to the spinal column decrease, making older golfers more susceptible to injury.39 There has been much research on the frequency and incidence of golf injuries, and as new retirees seek golf as a leisure activity, the need for injury prevention and effective golf rehabilitative programs has never been higher.
Low back pain is the number one injury sustained by golfers, accounting for up to 34.5% of all injuries.23,25,26,31,34,43 Since the average injury lasts between 2 and 4 weeks,36,43 it is costly to the golf industry, the health care system, and the workforce at large.
The direct annual costs of back pain, as related to physician services, medical devices, medications, hospital services, and diagnostic tests, for example, are estimated to be $91 billion.8 Of the practitioners involved with treating injured golfers, the general practitioner, physical therapist, and chiropractor are the most commonly sought health care professionals.26
Back Pain and Golf
Most golfers report back pain developing over time rather than from one traumatic incident.26,27
The impact and follow-through phase of the golf swing account for the most injuries when compared to other phases.26 The modern swing, separating the hips and shoulders as much as possible during the backswing (X-factor), gains more power and finishes in lumbar hyperextension (reverse-C position) (Figure 1),49 which increases pressure on the spine.25,36 Adding to injury potential during follow-through are the eccentrically contacting abdominal muscles to slow rotation and the increased pressure on the annulus of the intervertebral disc.3
Figure 1.
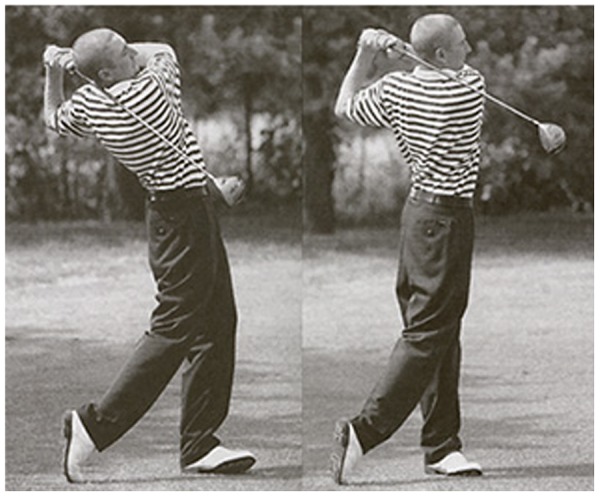
(left) Reverse-C finish; (right) straight I position.
Interestingly, golfers without low back pain do not have a significantly different lumbar hyperextension angle than do those with back pain at the end of the golf swing.41 Therefore, the relevance of lumbar hyperextension in low back injury remains unknown. This study did not differentiate between classic or modern swing types, which may be a factor (Table 1).
Table 1.
Modern golf swing versus classic golf swing
| Swing Phase | Classic Swing | Modern Swing |
|---|---|---|
| Address | Similar to modern | Similar to classic |
| Backswing | Body moves in relative unison | Separate hips and shoulders |
| Top of backswing | Shoulder/hip rotation relatively same Body sway to trail side | X-factor (shoulder/hips separate as much as possible) Pivot on trail leg |
| Downswing | Entire body starts downswing as 1 unit | Hips start downswing, followed by shoulders and then arms |
| Impact | Shoulder/hip relatively equal Minimal trunk flexion toward trail side | Hips open to target more than shoulders Increased lateral trunk flexion toward trail side |
| Follow-through | Lumbar spine neutral | Reverse C (lumbar hyperextension) |
Three-dimensional analysis offers a new look at the golf swing and human movement in general.24 Muscle firing patterns related to the kinematic sequencing of the golf swing contribute to swing efficiency and risk of low back injury with torsional, shear, and overall load change with different body positioning. Rehabilitation and prevention efforts must focus on movement pattern and muscle imbalance correction as well as technical swing changes.
Common Low Back Conditions in Golfers
The golf swing produces large loads in the spine, particularly during downswing to follow-through. These loads approach that of professional football linemen hitting a sled and are well above the force needed to prolapse intervertebral discs in cadavers.36 These intense loads can strain muscles, injure facet joints and lumbar discs, and cause spondylolysis.14,36,39 In older populations, vertebral and rib stress fractures are more likely than they are in younger populations, owing to osteoporosis.36
For a right-handed golfer, the left external oblique, L2 paraspinal musculature (rotatores thoracis, semispinalis thoracis, spinalis thoracis, iliocostalis thoracis, longissimus thoracis), and rectus abdominis are the core muscles that initiate the takeaway from address39 (Figure 2). At the top of the backswing, the right-sided external obliques, paraspinal muscles, and abdominals initiate the highest load of the swing and are dominant through impact. Not surprisingly, the right lumbar region in right-handed golfers is most commonly injured.39
Figure 2.
Swing sequence. General overview of golf swing from address (top left) to top of backswing (top right) to follow-through (bottom right).
Paraspinal muscle injury is common in golfers. In the modern swing, increases in angular displacement of the spine, lateral bending, shear, compression, and torsional forces24,27 require the paraspinal muscles to stabilize the spine during peak effort.39 The risk for paraspinal muscle tears and strains are inherent, as the paraspinal muscles are compromised by fatigue and stress imbalances, especially in the amateur golfer. Tears can be seen through a number of diagnostic tools, such as magnetic resonance imaging.39 Conservative treatment can consist of rest with cessation of golf and initiation of core strengthening and movement pattern correction; it should also include evaluation of golf swing mechanics.
The reverse-C position (Figure 1) has the potential to cause facet irritation.25 In older populations with spinal degenerative changes, this position creates additional stress on at-risk facets. Facet arthropathy is usually treated with corticosteroids and rest from golf during initiation of therapy.39
There are few studies on return to sport after disc herniation; one study reports a 79% return rate in an average of less than 5 months.17 The mean age of these subjects was 21 years. Discogenic back pain is usually treated conservatively with a hiatus from golf, use of nonsteroidal anti-inflammatories, and physical therapy.39
Spondylolysis (stress fracture of the pars interarticularis) is most common in young athletes. It is also seen in adult golfers because the lumbar neural arch is vulnerable to fatigue failure with overuse.29 Poor swing mechanics, poor endurance, and muscular imbalance can increase susceptibility to overuse injury.3 Spondylolysis treatment is usually conservative, consisting of no golf, core strengthening, and correction of muscle length imbalances.39
Early Rehabilitation
The rehabilitation process for golfers with low back pain should include a multidisciplinary team that works together to maximize return to golf safely. A team consisting of a physiatrist and physical therapist and a Professional Golf Association (PGA) teaching professional working together produced a 98% return to sport rate, with 2 patients winning state amateur titles.33 Physicians’ utilization of diagnostic tools such as magnetic resonance imaging, ultrasound, or other imaging/testing help to establish a diagnosis. Subsequent treatment through medication, injections, and so on help treat the symptoms. With pain reduced or absent, early rehabilitation starts.
Without low back pain, golfers have up to twice as much trunk flexion velocity during the downswing, using the abdominal muscles.21 Therefore, core stability training is an integral part of a rehabilitation program for a golfer with low back pain.
To initiate core control correctly, diaphragmatic breathing, pelvic tilting (progressing from supine to quadruped to standing), pelvic floor exercises, and neurodevelopmental rolling techniques are recommended to activate and train the core. These start after the acute pain phase of injury.
The activation of the diaphragm, pelvic floor, and abdominals is central to stabilization of the trunk during respiration and postural activity20,46 and should be incorporated into a golfer’s rehabilitation program early on. The importance of breathing control while swinging or putting is widely accepted in the golfing community. Incorporating diaphragmatic training early, including swing programs, allows for functional transition from clinic to course.
Transversus abdominis and multifidus training is necessary in any golf rehabilitation program.9,12,22 Hip abductors, erector spinae, and quadratus lumborum also contribute to core stability. It is difficult to isolate one muscle as the “most important” during the golf swing. Core stability is a fluid continuous motion among many parts.46 If one part is not functioning properly, the entire motion is compromised biomechanically.
Once the golfer has mastered fundamental and basic core control, more challenging exercises can be integrated. The transverse abdominis is most active during elbow-toe (plank) contralateral arm and leg lifts (Figure 3).32 The multifidus was most active during back bridges (Figure 4), the rectus abdominis in curl-ups (Figure 5), and the erector spinae in back bridge single-leg lift exercises (Figure 6).32 Side planks (Figure 7) address quadratus lumborum weakness, and bird dog exercises (Figure 8) target the spinal extensors.46
Figure 3.
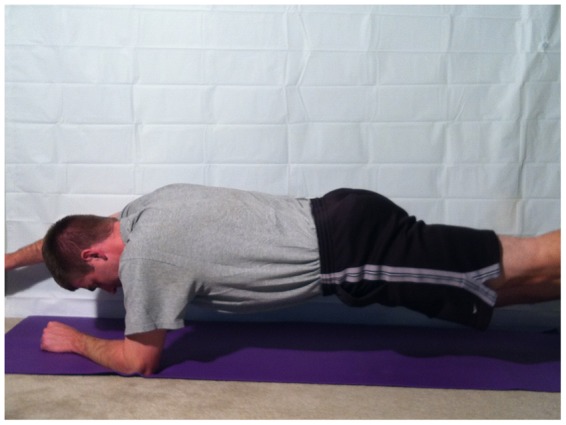
Contralateral arm and leg lift plank.
Figure 4.

Bridge.
Figure 5.
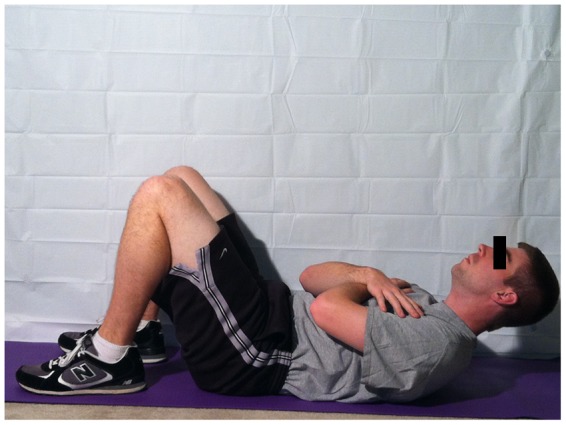
Curl-up.
Figure 6.

Bridge with single-leg lift.
Figure 7.

Side plank.
Figure 8.

Bird dog.
These exercises focus on direct isolation of core muscles; progression should be toward early sport-specific core training (eg, half kneeling on a line with rotations and standing rotations) (Figure 9). These can be completed in a low-to-high, high-to-low, and straight-across-midline manner to train all 3 planes of movement. Exercises should be completed with different intensities, loads, and volumes to maximize training benefit depending on the phase of the periodized program. Focus should be on core initiation (not extremity initiation), which is the correct golf swing sequencing.3
Figure 9.
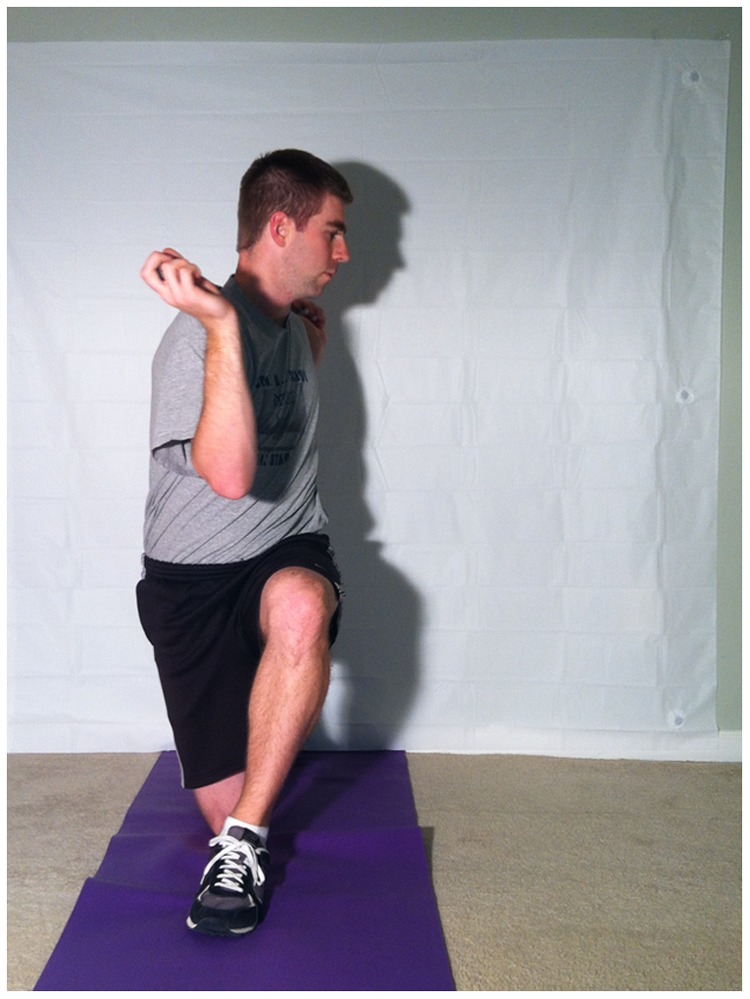
Half-kneel straight-line rotations.
Golf-Specific Movement Screening
During rehabilitation and early performance training, movement pattern and golf-specific screening are needed. The Functional Movement Screen is not golf specific but can be used for general movement pattern screening. This has been used to identify poor movement patterns that put professional football players at risk for injury.19
The Titleist Performance Institute level 1 screen40 is growing in popularity among health care, fitness, and PGA professionals, but there is no proven gold standard for performance/injury screening in golf. The sooner imbalances and swing faults are identified and corrected, the less likely the golfer will be injured.
The Selective Functional Movement Assessment, which identifies dysfunctional movements, should be used to assess golfers at this stage in rehabilitation if not completed earlier. The assessment isolates movement dysfunction to determine if the faulty movement pattern is due to a stability or mobility deficit, leading to appropriate treatment (SFMA seminar manual, February 2012; Titleist Performance Institute, medical professional seminar manual, February 2012.).
Most studies on golf injuries have been done on those with handicaps < 5.23 The 50th percentile of US golfers have a handicap between 14.0 and 14.9 for men28 and 27.0 and 27.9 for women,47 so the ability to apply findings to the amateur golfer may be limited.
Late Rehabilitation
Swing faults and physical imbalances should be prioritized on the basis of their correlation and the individual golfer. Core strength is essential along with scapular and hip stabilization in preventing injury in the golf swing.7,18 The gluteus medius muscles stabilize the pelvis and provide a base trunk rotation.2 Gluteus medius inhibition may increase lateral hip movement during the swing, potentially causing increased lateral bending at impact.40
The basic exercises of early rehabilitation are an appropriate start for core weakness and instability. Shoulder mobility, scapular stability, thoracic rotation/extension, hip mobility/stability, ankle mobility, balance, and shoulder deceleration control all should be assessed as well.
During core stability training, the activity level of core muscles is enhanced when exercises are performed on an unstable surface.16 Bosu balls, balance discs, or exercise physio balls elicit higher levels of stability training. The unilateral nature of golf enhances the importance of training in a balanced fashion. Retesting every few months for muscular imbalance is recommended, as imbalances contribute to the development of back pain and are common in golf.44
Training on unsteady surfaces, however, changes primary muscle use patterns. During a curl-up exercise on an unstable surface, for example, the activity of the external obliques increases while transversus abdominis activity decreases, compared to a curl-up on a stable surface.16 Golf-specific drills for performance should not be performed solely on unsteady surfaces; the patterns used for training on unsteady surfaces are different from those used on the course.
Prevention
The core muscles are constantly used during the swing, creating a high potential for fatigue and injury.35 Compensatory muscles that may secondarily assist the fatiguing core are also at risk.35 A golf screening process can identify these areas of compensation and correlate them with present swing faults to determine the limitations that put a golfer at higher risk for injury.
Consider a right-handed golfer failing an overhead squat due to tight soleus muscles (spine angle is not parallel to tibial angle). The right-handed golfer also demonstrates hip extension into the hand space during the golf swing (early extension swing fault; Figure 10). A failed overhead squat correlates with early extension 99% of the time and is one of the top 2 swing faults associated with low back pain.40 Additionally, this golfer has decreased external rotation in the right shoulder (trail arm).
Figure 10.

(left) Early extension; (right) no early extension.
Early extension is not a result of shoulder external rotation limitation but is associated with tight soleus muscles. Therefore, the soleus mobility deficit should be addressed first. Most golf-related injuries occur on the lead side of the body, emphasizing the importance of addressing the soleus deficit first, as the shoulder limitation is on the trail side.41
Particular attention should be given to the golf swing and its relationship to particular injuries when prioritizing a prevention plan.37 For example, range-of-motion deficits in lead hip internal rotation and lumbar spine extension correlate to low back pain while finger-to-floor distance testing hamstring length does not.30,42
While the benefits of physical correction and swing changes in reducing pain and recurrence have not been quantified, a fundamental understanding of how physical limitations will affect a golfer’s swing is important.12,26 This understanding ensures the proper prioritization to prevent injury.
The most important aspect of any injury prevention or rehabilitation program is educating the target audience to ensure compliance. Golf educational programs should include information about injury prevention strategies.5 Golfers should understand that avoiding injury starts before they ever set foot on the course.
PGA Professionals’ Role
The PGA golf professional can play an integral role in the rehabilitation process with an understanding of the biomechanics of the golf swing and the muscles and joints involved (Titleist Performance Institute, medical professional seminar manual, February 2012). The top 3 swing faults related to low back pain in golfers are early extension (hips come forward into the hand space during the swing) (Figure 10), reverse spine angle (use of the erector spinae into extension during the backswing) (Figure 11), and reverse-C finish (see Figure 1).
Figure 11.

(left) Reverse spine angle; (right) correct spine angle.
The modern swing is most commonly taught today because the X-factor creates optimal power.1 It has less external and internal oblique activity than the classical swing but has higher activation of both erector spinae, especially in the follow-through phase.1 Golfers with low back pain have more activity in the external obliques owing to an inability to activate the erector spinae fully.6 A golfer who uses the modern swing and has a history of low back pain is likely to have pain recur because of his or her swing and the body’s inability to adapt to the increased erector spinae demand.
The classic swing produces less angular displacement, lateral bending, shear, compression, and torsional forces of the lumbar spine compared to the modern swing.34 Some research asserts that the X-factor is not required to produce optimal swing speed.45 Therefore, the classic swing is an attractive alternative for golfers with back pain.
Switching to a hybrid swing is another alternative. A golfer incorporates the X-factor during the backswing but a neutral spine during the finish, thereby protecting the lumbar facets.25
Shorter backswings are another option to reduce trunk muscle activation and reduce back injury without negatively affecting swing accuracy or club head velocity.4 The short swing, however, increases shoulder muscle activation and may increase risk for shoulder injury.3,4
Video feedback training for golf performance has been effective in helping train a golfer’s swing form.13 Increasing hip rotation and decreasing shoulder turn during the backswing while decreasing trunk flexion and lateral flexion during the downswing may decrease low back pain and reduce the risk of reinjury as well.11
Simple Prevention
Having a proper club fit to body specifications, playing consistently, pushing a cart instead of pulling, and utilizing a long putter may decrease stress and strain on the lumbar spine throughout a round of golf.27,34
Carrying a golf bag with a single strap may be hazardous to the lower back, shoulder, and ankle.10 The dual “backpack strap” distributes the clubs more evenly across both shoulders.
Increased bodyweight is a significant risk factor for low back pain among golfers.31 In the overweight population, weight loss and diet counseling need to be a part of rehabilitation and injury prevention/education.
Conclusion
A multidisciplinary team is the best approach to prevention, rehabilitation, and performance training for golfers.
Technical flaws and physical imbalances contribute to the development of back pain in golfers. Unless both are addressed, golfers may continually cycle through periods of injury.
When the PGA/LPGA or certified golf medical/fitness professionals are not geographically available to work together, resources (eg, http://www.athleteslocker.com) exist for professionals to work remotely to assess and suggest physical and swing changes based on current client status and appropriate goals.
Footnotes
The author declared the following potential conflict of interest: He developed and currently runs the website www.athleteslocker.com.
References
- 1. Aggarwal A, Shenoy S, Sandhu JS. Comparison of lumbar and abdominal muscle activation during two types of golf swing: an EMG analysis. Int J Sport Med. 2008;4(12):59-71 [Google Scholar]
- 2. Bechler JR, Jobe FW, Pink M, Perry J, Ruwe PA. Electromyographic analysis of the hip and knee during the golf swing. Clin J Sport Med. 1995;5(3):162-166 [DOI] [PubMed] [Google Scholar]
- 3. Brandon B, Pearce PZ. Training to prevent golf injury. Curr Sports Med Rep. 2009;8(3):142-146 [DOI] [PubMed] [Google Scholar]
- 4. Bulbulian R, Ball KA, Seaman DR. The short golf backswing: effects on performance and spinal health implications. J Manipulative Physiol Ther. 2001;24(9):569-575 [DOI] [PubMed] [Google Scholar]
- 5. Cann AP, Vandervoort AA, Lindsay DM. Optimizing the benefits versus risks of golf participation by older people. J Geriatr Phys Ther. 2005;28(3):85-92 [DOI] [PubMed] [Google Scholar]
- 6. Cole MH, Grimshaw PN. Electromyography of the trunk and abdominal muscles in golfers with and without low back pain. J Sci Med Sport. 2008;11(2):174-181 [DOI] [PubMed] [Google Scholar]
- 7. Fukuda TY, Rossetto FM, Magalhães E, et al. Short-term effects of hip abductors and lateral rotators strengthening in females with patellofemoral pain syndrome: a randomized controlled clinical trial. J Orthop Sports Phys Ther. 2010;40(11):736-742 [DOI] [PubMed] [Google Scholar]
- 8. Furlan AD, Yazdi F, Tsertsvadze A, et al. A systematic review and meta-analysis of efficacy, cost-effectiveness, and safety of selected complementary and alternative medicine for neck and low-back pain. Evid Based Complement Alternat Med. 2012;2012:953139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gluck GS, Bendo JA, Spivak JM. The lumbar spine and low back pain in golf: a literature review of swing biomechanics and injury prevention. Spine J. 2008;8(5):778-788 [DOI] [PubMed] [Google Scholar]
- 10. Gosheger G, Liem D, Ludwig K, Greshake O, Winkelmann W. Injuries and overuse syndromes in golf. Am J Sports Med. 2003;31(3):438-443 [DOI] [PubMed] [Google Scholar]
- 11. Grimshaw P, Burden AM. Case report: reduction of low back pain in a professional golfer. Med Sci Sports Exerc. 2000;32(10):1667-1673 [DOI] [PubMed] [Google Scholar]
- 12. Grimshaw P, Giles A, Tong R, Grimmer K. Lower back and elbow injuries in golf. Sports Med. 2002;32(10):655-666 [DOI] [PubMed] [Google Scholar]
- 13. Guadagnoli M, Holcomb W, Davis M. The efficacy of video feedback for learning the golf swing. J Sports Sci. 2002;20(8):615-622 [DOI] [PubMed] [Google Scholar]
- 14. Hosea TM, Gatt CJ. Back pain in golf. Clin Sports Med. 1996;15(1):37-53 [PubMed] [Google Scholar]
- 15. IBISWorld Golf courses and country clubs in the US: market research report. http://www.ibisworld.com/industry/default.aspx?indid=1652 Accessed December 12, 2011
- 16. Imai A, Kaneoka K, Okubo Y, et al. Trunk muscle activity during lumbar stabilization exercises on both a stable and unstable surface. J Orthop Sports Phys Ther. 2010;40(6):369-375 [DOI] [PubMed] [Google Scholar]
- 17. Iwamoto J, Takeda T, Sato Y, Wakano K. Short-term outcome of conservative treatment in athletes with symptomatic lumbar disc herniation. Am J Phys Med Rehabil. 2006;85:667-674 [DOI] [PubMed] [Google Scholar]
- 18. Kao JT, Pink M, Jobe FW, Perry J. Electromyographic analysis of the scapular muscles during a golf swing. Am J Sports Med. 1995;23(1):19-23 [DOI] [PubMed] [Google Scholar]
- 19. Kiesel K, Plisky PJ, Voight ML. Can serious injury in professional football be predicted by a preseason functional movement screen? N Am J Sports Phys Ther. 2007;2(3):147-158 [PMC free article] [PubMed] [Google Scholar]
- 20. Kolar P, Sulc J, Kyncl M, et al. Stabilizing function of the diaphragm: dynamic MRI and synchronized spirometric assessment. J Appl Physiol. 2010;109(4):1064-1071 [DOI] [PubMed] [Google Scholar]
- 21. Lindsay D, Horton J. Comparison of spine motion in elite golfers with and without low back pain. J Sports Sci. 2002;20(8):599-605 [DOI] [PubMed] [Google Scholar]
- 22. Malátová R, Pucelík J, Rokytová J, Kolár P. The objectification of therapeutical methods used for improvement of the deep stabilizing spinal system. Neuro Endocrinol Lett. 2007;28(3):315-320 [PubMed] [Google Scholar]
- 23. McHardy A, Pollard H. Muscle activity during the golf swing. Br J Sports Med. 2005;39(11):799-804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McHardy A, Pollard H, Luo K. A comparison of the modern and classic golf swing: a clincian’s perspective. South Afr J Sports Med. 2006;18(3): 80-92 [Google Scholar]
- 25. McHardy A, Pollard H, Luo K. Golf injuries: a review of the literature. Sports Med. 2006;36(2):171-187 [DOI] [PubMed] [Google Scholar]
- 26. McHardy A, Pollard H, Luo K. Golf-related lower back injuries: an epidemiological survey. J Chiropr Med. 2007;6(1):20-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. McHardy A, Pollard H, Luo K. One-year follow-up study on golf injuries in Australian amateur golfers. Am J Sports Med. 2007;35(8):1354-1360 [DOI] [PubMed] [Google Scholar]
- 28.Men’s Handicap Indexes. USGA handicap department. [Accessed January 2012]. http://www.usga.org/handicapping/articles_resources/men-s-USGA-Handicap-Indexes.html
- 29. Micheli LJ. Stress fractures in the spine and sacrum. Clin Sports Med. 2006;25:75-88 [DOI] [PubMed] [Google Scholar]
- 30. Mundt DJ, Kelsey JL, Golden AL, et al. An epidemiologic study of sports and weight lifting as possible risk factors for herniated lumbar and cervical discs: the Northeast Collaborative Group on Low Back Pain. Am J Sports Med. 1993;21(6):854-860 [DOI] [PubMed] [Google Scholar]
- 31. Murray E, Birley E, Twycross-Lewis R, Morrissey D. The relationship between hip rotation range of movement and low back pain prevalence in amateur golfers: an observational study. Phys Ther Sport. 2009;10(4):131-135 [DOI] [PubMed] [Google Scholar]
- 32. Okubo Y, Kaneoka K, Imai A, et al. Electromyographic analysis of transversus abdominis and lumbar multifidus using wire electrodes during lumbar stabilization exercises. J Orthop Sports Phys Ther. 2010;40(11):743-750 [DOI] [PubMed] [Google Scholar]
- 33. Parziale JR. Healthy swing: a golf rehabilitation model. Am J Phys Med Rehabil. 2002;81(7):498-501 [DOI] [PubMed] [Google Scholar]
- 34. Parziale JR, Mallon WJ. Golf injuries and rehabilitation. Phys Med Rehabil Clin N Am. 2006;17(3):589-607 [DOI] [PubMed] [Google Scholar]
- 35. Pink M, Perry J, Jobe FW. Electromyographic analysis of the trunk in golfers. Am J Sports Med. 1993;21(3):385-388 [DOI] [PubMed] [Google Scholar]
- 36. Reed JJ, Wadsworth LT. Lower back pain in golf: a review. Curr Sports Med Rep. 2010;9(1):57-59 [DOI] [PubMed] [Google Scholar]
- 37. Sherman CA, Finch CF. Preventing injuries to competitive and recreational adult golfers: what is the evidence? J Sci Med Sport. 2000;3(1):65-78 [DOI] [PubMed] [Google Scholar]
- 38.SRI International The 2005 golf economy report. http://www.cmaa.org/uploadedFiles/Member/Legislative/2005GolfEconomyReport.pdf Published 2008. Accessed December 12, 2011
- 39. Sutcliffe J, Ly JQ, Kirby A, Beall DP. Magnetic resonance imaging findings of golf-related injuries. Curr Probl Diagn Radiol. 2008;37(5):231-241 [DOI] [PubMed] [Google Scholar]
- 40. Titleist Performance Institute Level 1 Seminar Manual. Oceanside, CA: Titleist Performance Institute; 2011 [Google Scholar]
- 41. Tsai YS, Sell TC, Smoliga JM, Myers JB, Learman KE, Lephart SM. A comparison of physical characteristics and swing mechanics between golfers with and without a history of low back pain. J Orthop Sports Phys Ther. 2010;40(7):430-438 [DOI] [PubMed] [Google Scholar]
- 42. Vad VB, Bhat AL, Basrai D, Gebeh A, Aspergren DD, Andrews JR. Low back pain in professional golfers: the role of associated hip and low back range-of-motion deficits. Am J Sports Med. 2004;32(2):494-497 [DOI] [PubMed] [Google Scholar]
- 43. Wadsworth LT. When golf hurts: musculoskeletal problems common to golfers. Curr Sports Med Rep. 2007;6(6):362-365 [DOI] [PubMed] [Google Scholar]
- 44. Weishaupt P, Obermüller R, Hofmann A. Spine stabilizing muscles in golfers. Sportverletz Sportschaden. 2000;14(2):55-58 [DOI] [PubMed] [Google Scholar]
- 45. Westcott WL, Parziale JR. Golf power. Fitness Management. 1997;13:39-41 [Google Scholar]
- 46. Willson JD, Dougherty CP, Ireland ML, Davis IM. Core stability and its relationship to lower extremity function and injury. J Am Acad Orthop Surg. 2005;13(5):316-325 [DOI] [PubMed] [Google Scholar]
- 47. Women’s handicap indexes. http://www.usga.org/handicapping/articles_resources/women-s-USGA-Handicap-Indexes.html Accessed January 2012



