Abstract
Significance: Numerous studies have reported associations between declining nutrition status and risk for pressure ulcers. Oral eating problems, weight loss, low body weight, undernutrition, and malnutrition are associated with an increased risk for pressure ulcers. Moreover, inadequate nutrient intake and low body weight are associated with slow and nonhealing wounds. However, the biologic significance of deterioration in nutrition status and consistent methodologies to quantify malnutrition and diminished micronutrient stores as predictors of skin breakdown remains controversial.
Recent Advances: The Academy of Nutrition and Dietetics (Academy) and the American Society for Parenteral and Enteral Nutrition (ASPEN) Consensus Statement: Characteristics Recommended for the Identification and Documentation of Adult Malnutrition provide a standardized and measureable set of criterion for all health professionals to use to identify malnutrition. The Agency for Healthcare Research and Quality identified malnutrition as one of the common geriatric syndromes associated with increased risk for institutionalization and mortality that may be impacted by primary and secondary preventions.
Critical Issues: The purpose of this article is to examine the Academy/ASPEN consensus statement on characteristics of adult malnutrition in the context of the National Pressure Ulcer Advisory Panel (NPUAP)/European Pressure Ulcer Advisory Panel (EPUAP) Guidelines on the Prevention and Treatment of Pressure Ulcers.
Future Directions: Moreover, clinicians, and in particular, registered dietitians have the opportunity to integrate the Characteristics of Malnutrition with the NPUAP/EPUAP 2009 Prevention and Treatment Clinical Practice Guidelines, into clinical assessment and documentation using the Nutrition Care Process. Consensus guidelines will provide consistent research criteria yielding more useful data than presently available.

Mary D. Litchford, PhD, RD, LDN
Scope and Significance
Meeting macro- and micronutrient requirements form the cornerstone of good health. The point at which diminished nutrient reserves impacts skin integrity is undetermined. The National Pressure Ulcer Long Term Care Study1 reported that oral eating problems and weight loss were associated with a higher risk of developing pressure ulcers. Moreover, inadequate nutrient intake and low body weight are associated with slow and nonhealing wounds.2–8 Pre-existing malnutrition and/or weight loss was a positive predictive variable for all undesirable surgery-related hospital-acquired conditions (i.e., Centers for Medicare and Medicaid “never” events), including pressure ulcers.9 The prevalence of malnutrition in acute care settings internationally is estimated to be 40%10 and up to 30% in nursing homes.11 In these studies, the criterion for quantifying malnutrition was determined independently by the investigators since a standardized set of diagnostic characteristics was not available in the literature.
Studies addressing the prevalence and incidence of malnutrition have provided a mixture of inconclusive data because there has not been a consensus on the criterion required to quantify a diagnosis of malnutrition.12 Historically, the diagnosis of malnutrition has been loosely defined using a range of criterion, including biochemical test results, anthropometric benchmarks, and physical assessment findings.10,11,13–25 Many studies have not differentiated between undernutrition (nonsevere malnutrition) and severe malnutrition. The Agency for Healthcare Research and Quality identified malnutrition as one of the common syndromes of older adults associated with increased risk for institutionalization and mortality that may be impacted by primary and secondary preventions.26 Utilizing the Academy/American Society for Parenteral and Enteral Nutrition (ASPEN) Characteristics of Adult Malnutrition12 in the context of the National Pressure Ulcer Advisory Panel (NPUAP)/European Pressure Ulcer Advisory Panel (EPUAP) Guidelines for the Prevention and Treatment of Pressure Ulcers27 offers clinicians a standardized approach to quantify changes in nutritional status and risk for skin breakdown.
Translational Relevance
The consensus guidelines defining characteristics of malnutrition are vital new tools for clinicians to use in risk assessment for pressure ulcers and in the systems approach to nutrition assessment. The systematic approach to nutrition assessment includes collecting data from a variety of domains to guide in the diagnosis of a malnutrition syndrome. Important components of the assessment process are indicators of malnutrition and inflammation, including the medical/surgical history and clinical diagnosis, clinical signs and physical examination, anthropometric data, laboratory indicators, dietary assessment, and functional outcomes.28–30
Clinical Relevance
Incorporation of the diagnostic characteristics of malnutrition in adults provides a vital tool for clinicians to identify patients at risk for pressure ulcers. A standardized approach to diagnose malnutrition will facilitate an improved correlation between best practice related to the prevention and healing of pressure ulcers. The Academy and ASPEN are developing a standardized data collection format and protocol to validate additional characteristics of malnutrition. Systems are needed to track comorbid conditions and diseases associated with malnutrition. The collection, analyzing, and dissemination of evidence data supporting malnutrition diagnosis will ensure resources are used efficiently and that the health of individuals is optimized.
Discussion of Findings and Relevant Literature
Nutrition-related evidence-based guidelines for prevention and treatment of pressure ulcers
NPUAP and the EPUAP collaborated and published the NPUAP/EPUAP 2009 Prevention and Treatment Clinical Practice Guidelines.27 These guidelines were developed following a systematic, comprehensive review of peer-reviewed, published research on pressure ulcers from 1998 to January 2008. The Sackett Level of Evidence Rating System for Individual Studies was applied to each published research evaluated and the strength of evidence supporting each recommendation was rated.31 Table 1 summarizes the nutrition guidelines for prevention and treatment of pressure ulcers.27 The revised guidelines, to be published in 2014, will be a combined effort of the NPUAP, EPUAP, and the Pan Pacific Pressure Injury Advisory Panel (PPPIAP), thus extending the international influence.
Table 1.
Nutrition guidelines for prevention and treatment of pressure ulcers
| 1. Screen and assess nutritional status for each individual with a pressure ulcer at admission and with each condition change—and/or when progress toward pressure ulcer closure is not observed. (Strength of Evidence=C) |
| • Refer all individuals with a pressure ulcer to the dietitian for early assessment of and intervention for nutritional problems. (Strength of Evidence=C) |
| • Assess weight status for each individual to determine weight history and significant weight loss from usual body weight (≥5% change in 30 days or≥10% in 180 days). (Strength of Evidence=C) |
| • Assess the individual's ability to eat independently. (Strength of Evidence=C) |
| • Assess the adequacy of total nutrient intake (food, fluid, oral supplements, enteral/parenteral feedings). (Strength of Evidence=C) |
| 2. Provide sufficient calories. (Strength of Evidence=B) |
| • Provide 30–35 kcal/kg body weight for individuals under stress with a pressure ulcer. Adjust formula based on weight loss, weight gain, or level of obesity. Individuals who are underweight or who have had significant unintentional weight loss may need additional kcal to cease weight loss and/or regain lost weight. (Strength of Evidence=C) |
| • Revise and modify (liberalize) dietary restrictions when limitations result in decreased food and fluid intake. These adjustments are to be managed by a dietitian or medical professional. (Strength of Evidence=C) |
| • Provide enhanced foods and/or oral supplements between meals if needed. (Strength of Evidence=B) |
| • Consider nutritional support (enteral or parenteral nutrition) when oral intake is inadequate. This must be consistent with the individual's goals. (Strength of Evidence=C) |
| 3. Provide adequate protein for positive nitrogen balance for an individual with a pressure ulcer. (Strength of Evidence=B) |
| • Offer 1.25–1.5 g protein/kg body weight daily for an individual with a pressure ulcer when compatible with goals of care, and reassess as condition changes. (Strength of Evidence=C) |
| • Assess renal function to ensure that high levels of protein are appropriate for the individual. (Strength of Evidence=C) |
| 4. Provide and encourage adequate daily fluid intake for hydration. (Strength of Evidence=C) |
| • Monitor individuals for signs and symptoms of dehydration: changes in weight, skin turgor, urine output, elevated serum sodium, or calculated serum osmolality. (Strength of Evidence=C) |
| • Provide additional fluid for individuals with dehydration, elevated temperature, vomiting, profuse sweating, diarrhea, or heavily draining wounds. (Strength of Evidence=C) |
| 5. Provide adequate vitamins and minerals. (Strength of Evidence=B) |
| • Encourage consumption of a balanced diet that includes good sources of vitamins and minerals. (Strength of Evidence=B) |
| • Offer vitamin and mineral supplements when dietary intake is poor or deficiencies are confirmed or suspected. (Strength of Evidence=B) |
From National Guideline Clearing House, used with permission.27
In 2010, the Academy appointed a wound care expert work group to formulate research questions addressing the relationship of nutrition for wound healing. The Wound Care Expert Work group adapted the NPUAP/EPUAP evidence-based nutrition guidelines since their methods met both the Academy and Appraisal of Guidelines for Research and Evaluation criteria.32 The Academy Wound Care Expert Workgroup formulated practice questions that were not addressed by the NPUAP/EPUAP Nutrition Guidelines for Pressure Ulcers. Research questions included how to calculate energy and fluid needs to promote healing in obese/nonobese adults with acute surgical wounds, the role of indispensable amino acids for adults with pressure ulcers and renal disease plus questions on the association of inflammation and wound healing. Unfortunately, there was insufficient scientific evidence to support any recommendations, but the demand for research on these topics is significant.
Inflammation-malnutrition connection
Globally, the term malnutrition is associated with famine secondary to natural disasters or political unrest. When malnutrition is related to very low macronutrient intakes and inflammation is not present, the depleted nutrient status can be treated successfully with nutrition supplementation. Yet, in both the developing and developed world, inflammation plays a role in disease progression and concurrent deterioration of nutrition status. Recent evidence suggests that there are varying degrees of acute and chronic inflammation associated with injury, infection, and disease that lead to declining nutrition status and well-being.24,25,28–30
Inflammation is characterized by an acute phase response that triggers a cascade of reactions leading to elevated resting energy expenditure, impaired utilization of protein, and increased nitrogen excretion. Moreover, the acute-phase inflammatory response is associated with increased energy and protein requirements in individuals coupled with anorexia and pathologically altered utilization of nutrients. Yet, nutrition supplementation alone is not sufficient to reverse the mobilization of nutrients and other cytokine-related changes in an organ function. The point at which the severity or persistence of inflammation leads to a decrease in lean body reserves linked to impaired functional status is defined by Jensen as disease-related malnutrition.28,29 Numerous International Classification of Diseases, Ninth Revision, Clinical Modification codes are associated with malnutrition, but there has been a lack of consensus on the use of a standardized set of characteristics to differentiate undernutrition versus malnutrition in adults and the role of inflammation as a comorbid condition.
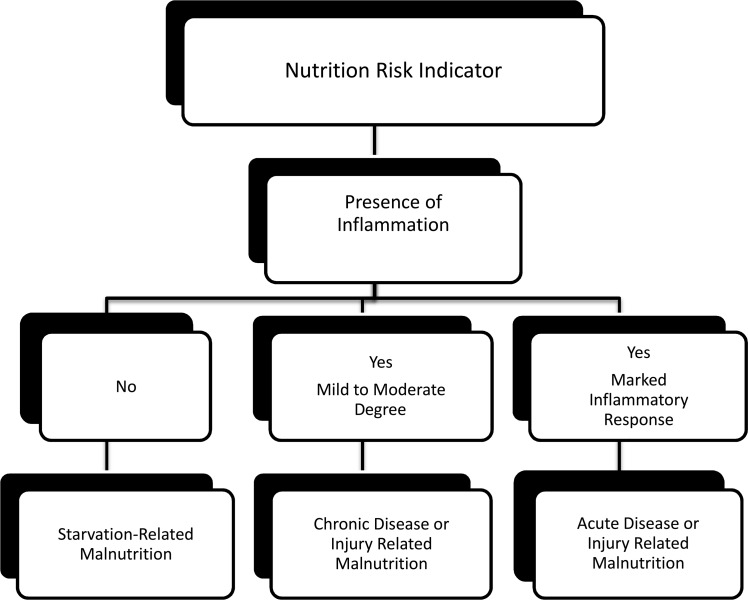
Jensen et al. proposed that malnutrition is a syndrome driven by different etiologies and varying degrees of inflammation.28,29 If inflammation is present, the clinician must determine the degree of severity (mild, moderate, or severe) and whether it is transient or sustained. Figure 1 illustrates the concept of etiology-based malnutrition syndromes.12 For example, an acute illness, such as pneumonia, may result in a moderate to severe malnutrition. Adequate nutrients are required to support vital organ system functions, while acute medical treatment is provided. Resolution of the pneumonia extinguishes the acute inflammatory response and normal utilization of nutrients is resumed to replenish depleted reserves. The successful management of the medical condition hinges on both the degree and resolution of the inflammation and meeting nutrient requirements. Acute illnesses with cytokine-related anorexia, insulin resistance and, prolonged bed rest create an ideal environment for pressure-related skin issues to evolve.
Figure 1.
Etiology-based malnutrition. Adapted with permission from White.12
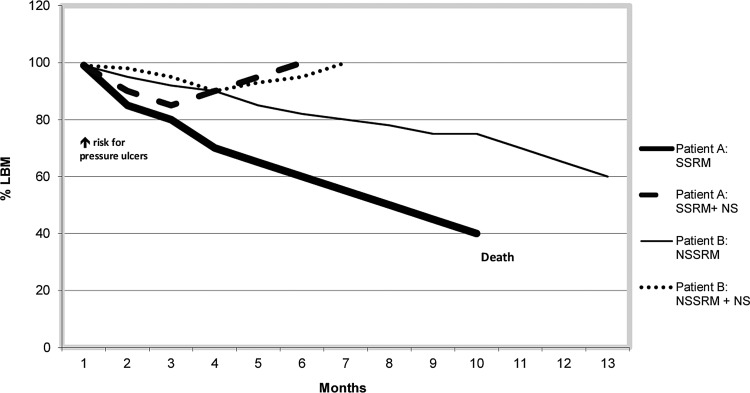
Figures 2 and 3 illustrate the predicted loss of lean body reserves and its relationship with increased risk for skin breakdown29 in four hypothetical patients. The illustrations assume that the patients have no pre-existing loss of lean body mass. In Fig. 2, Patient A has severe starvation-related malnutrition (SSRM). The solid bold line represents the linear progression of loss of lean body mass without nutrition intervention for SSRM. The dashed bold line represents the contribution of nutrition support to counteract the depletion of lean body reserves for SSRM with a nutrition supplement (SSRM+NS). Also, in Fig. 2, Patient B has nonsevere starvation-related malnutrition (NSSRM) or undernutrition. The solid thin line represents the linear progression of loss of lean body mass without nutrition intervention for NSSRM. The dotted line represents the contribution of nutrition support to counteract the depletion of lean body reserves with NS (NSSRM+NS).
Figure 2.
Hypothetical patient with starvation-related malnutrition. LBM, lean body mass; NS, nutrition supplement; NSSRM, nonsevere starvation-related malnutrition (undernutrition); SSRM, severe starvation-related malnutrition. Adapted with permission from Jensen et al.29
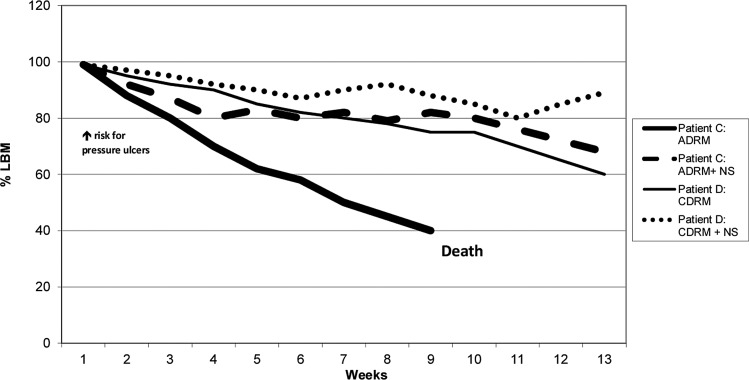
Figure 3.
Hypothetical patients with inflammation-related malnutrition. ADRM, acute disease-related malnutrition; CDRM, chronic disease-related malnutrition (undernutrition). Adapted with permission from Jensen et al.29
Figure 3 illustrates the predicted loss of lean body reserves and its relationship with increased risk for skin breakdown29 in two hypothetical patients with inflammation-related malnutrition. The chart assumes that the patients have no pre-existing loss of lean body mass and the inflammatory condition is relatively constant with changes in lean body reserves. Patient C has malnutrition in the context of an acute disease (acute disease-related malnutrition [ADRM]). For ADRM, the solid bold line represents the linear progression of loss of lean body mass without nutrition intervention. For ADRM+NS, the dashed line represents the contribution of nutrition support to counteract the depletion of lean body reserves in the context of acute illness. Patient D has malnutrition in the context of a chronic disease (chronic disease-related malnutrition [CDRM]). For CDRM, the solid thin line represents the linear progression of loss of lean body mass without nutrition intervention. For CDRM+NS, the dotted line represents the contribution of nutrition support to counteract the depletion of lean body reserves in the context of a chronic medical condition.
In both Figs. 2 and 3, the hypothetical patients experience loss of lean body mass and increased risk of pressure ulcers as the result of malnutrition. Nutrition supplementation replenishes depleted reserves in the patient with undernutrition (nonsevere starvation) and SSRM to baseline. Intervention with NSs supports the nutrient needs of the patient with inflammatory related malnutrition by reducing the rate of lean mass depletion. It is important to note that nutrition supplementation alone does not thwart the cytokine-driven mobilization of lean mass.
Etiology-based malnutrition
Using an etiology-based approach, the International Guideline Committee working with ASPEN and the European Society for Parenteral and Enteral Nutrition Congresses and the Malnutrition Task Force from the Academy have published a standardized set of diagnostic characteristics to be used to identify and document adult malnutrition in routine clinical practice.12 It uses an etiology-based nomenclature that reflects the current understanding of the role of the inflammatory response on the incidence, progression, and resolution of adult malnutrition. Moreover, malnutrition syndromes are defined by patient settings, including acute illness or surgery, chronic disease, and environmental or social circumstances. Additionally, the presence and degree of inflammation further differentiates the types of malnutrition as nonsevere and severe. Nonsevere does not mean not urgent. It is mild to moderate malnutrition or undernutrition.
There is no single parameter that defines malnutrition. The Consensus Guidelines identify six characteristics of malnutrition.12 From these, the clinician must identify a minimum of two characteristics that relate to the context of the concurrent medical condition for a nutrition diagnosis of malnutrition. The characteristics of nonsevere malnutrition are described in Table 2, while those of severe malnutrition are listed in Table 3.12–14,33–39,41,44 Each of the characteristics has a defined criterion to meet either nonsevere or severe malnutrition in the context of acute illness, chronic disease, or environmental circumstances. Characteristics specific to reduced energy intake and weight loss have both time and percentage benchmarks to meet. Please refer to Academy/ASPEN publications for specifics.12
Table 2.
Characteristics of nonsevere malnutrition
| Characteristic | Acute Illness/Injury | Chronic Illness | Social/Environmental |
|---|---|---|---|
| Insufficient energy intake33–35 | <75% for >7 days | <75% for ≥1 month | <75% for ≥3 months |
| Interpretation of weight loss13,14,36,37 | 1–2%/1 week | 5%/1 month | 5%/1 month |
| 5%/1 month | 7.5%/3 months | 7.5%/3 months | |
| 7.5%/3 months | 10%/6 months | 10%/6 months | |
| 20%/1 year | 20%/1 year | ||
| Changes in body composition: loss of body fat13,38 | Mild depletion | Mild depletion | Mild depletion |
| Changes in body composition: loss of muscle mass13,38 | Mild depletion | Mild depletion | Mild depletion |
| Changes in body composition: accumulation of fluid13,38 | Mild | Mild | Mild |
| Grip strength13,39,41,44 | Not applicable | Not applicable | Not applicable |
Adapted from White,12 used with permission.
Table 3.
Characteristics of severe malnutrition
| Characteristic | Acute Illness/Injury | Chronic Illness | Social/Environmental |
|---|---|---|---|
| Insufficient energy intake33–35,40 | ≤50% for >5 days | ≤75% for ≥1 month | ≤50% for 1 month |
| Interpretation of weight loss13,14,36,37 | >1–2%/1 week | >5%/1 month | >5%/1 month |
| >5%/1 month | >7.5%/3 months | >7.5%/3 months | |
| >7.5%/3 months | >10%/6 months | >10%/6 months | |
| >20%/1 year | >20%/1 year | ||
| Changes in body composition: loss of body fat13,38 | Moderate depletion | Severe depletion | Severe depletion |
| Changes in body composition: loss of muscle mass13,38 | Moderate depletion | Severe depletion | Severe depletion |
| Changes in body composition: accumulation of fluid13,38 | Moderate to severe | Severe | Severe |
| Grip strength13,39,41,44 | Markedly reduced | Markedly reduced | Markedly reduced |
Adapted from White,12 used with permission.
It is important to note that laboratory test results for albumin and prealbumin, used for decades as biomarkers of malnutrition, are not included as characteristics of malnutrition due to lack of evidence-based research. Albumin is a negative acute-phase reactant with a long half-life. Cytokine mediators, interleukin 1-beta, interleukin 6, and tumor necrosis factor, redirect the liver to synthesize positive acute-phase reactants rather than negative acute-phase reactants resulting in a lower albumin synthesis. Since the concentration of albumin is far greater in the extravascular compartment than in the plasma, albumin moves from the extravascular compartment to the plasma via osmosis. The literature is inconclusive on the relationship between the changes in albumin and prealbumin as predictors of changes in nutrition status.12–14,25,34,35,45–48 For these reasons, laboratory test results for albumin, prealbumin, and other serum proteins are not considered to be sensitive measures of protein status and were not included as characteristics of malnutrition. In addition, inflammatory biomarkers, C-reactive protein and other positive acute-phase reactants, are excluded because the literature is inconclusive on the relationship between the changes in these biomarkers and changes in nutrition status.12,17–23,45–48
The Academy/ASPEN Characteristics of Malnutrition serve as an evidence-based framework for use in identifying individuals at nutritional risk for pressure ulcers. Individuals with pressure ulcers may also have malnutrition as defined by the new Consensus Guidelines.12 Utilization of the new evidence-based guidelines will help clarify the role of nutrition supplementation in preventing skin breakdown and in promoting healing.
Systems approach to nutrition assessment
The clinician primarily responsible for the nutrition assessment is the registered dietitian (RD) who collects the data with the assistance of the interprofessional team. For example, as the RD gathers historical data and reviews the admission diagnosis, the physician and pharmacist maybe consulted and advised against prescribing medications that promote anorexia. A careful nutrition-focused physical examination should include determining the degree of body fat and muscle mass loss and the evaluation of any fluid accumulation. Weight loss is often masked by the presence of edema. Accurate anthropometric measurements and documentation are an important piece of the assessment process. Since weight loss is the most validated assessment parameter, the interprofessional team should ascertain the individual's historical weights. As noted, laboratory data should be interpreted with caution. The RD relies on the interprofessional team to assist in the collection of current food/fluid consumption. In addition to determining muscle loss, a practical measure of the functional outcome is hand-grip strength using a hand-grip dynamometer. Research indicates that decreased hand-grip strength is linked to premature mortality, declining nutrition status, and increased disability.41–44 Timed gait speeds and chair stands are additional methods of measuring functional outcomes.49,50 Based on the data documented on the nutrition assessment, the interprofessional team and the individual/patient should collaborate and formulate an action plan with the goal of preventing or healing pressure ulcers.
Case Studies
Pressure ulcer prevention
A 65-year-old woman is admitted to acute care with a diagnosis of hip fracture, obesity, rheumatoid arthritis, and diabetes mellitus. She lives alone and her neighbor found her on the floor 12 h after she fell. The duration of time spent in one position causes ischemia as a result of deformation of the tissues leading to hypoxia thus increasing the risk of pressure ulcer development. Her admission weight was 325 pounds (147.7 kg), height 60 inches (152.4 cm), and body mass index (BMI) 63.6 kg/m2. Medications included oral hypoglycemic, diuretic, and non-steroid anti-inflammatory drugs. Following surgery, her intake for the last 6 days was 50% of her estimated energy requirement. She stated that her usual diet was microwave meals, chips, and snack food. She lost 7 pounds (2% unintended weight loss) in a week, which was attributed to edema. Her biochemical data included hemoglobin A1C (Hgb A1C), 9% (<6%); fasting glucose, 195 mg/dL (70–100 mg/dL); serum albumin, 2.6 g/dL (3.5–5.0 g/dL); hemoglobin, 10 g/dL (12–16 g/dL); hematocrit, 32% (37%–42%); C-reactive protein, 18 mg/L (<1 mg/dL). Poor hand-grip strength measurements were documented using the hand-grip dynamometer. She has poor endurance and exhibits great difficulty ambulating during her physical therapy sessions and prefers to spend a major portion of the day in bed, refusing to change positions or elevate her heels because she is not able to see the television when she is repositioned. Her prolonged time spent in one position places her at risk for pressure ulcers.
Clinical malnutrition
Acute injury-associated malnutrition (hip surgery) and chronic disease-associated malnutrition:
• History and clinical diagnosis: Longstanding obesity and chronic inflammation associated with diabetes mellitus and arthritis plus current compromise in food/fluid intake and historical diet of poor quality per interview. Hip surgery associated with acute inflammatory response compounded by comorbidities.
• Anthropometric data: BMI consistent with obesity.
• Laboratory data: Fasting glucose and Hgb A1C consistent with diabetes mellitus and poor control. The elevated C-reactive protein characteristic of inflammation observed with surgery. Low hemoglobin and hematocrit are characteristics of blood loss from surgery, however, may reflect a pre-existing nutritional anemia. Historic data are unavailable.
• Dietary intake: Her current intake and history confirms the poor nutritional quality of her diet. Nutrient analysis of her oral intake suggests that her usual diet is low in high-quality protein, vitamins A, C, B12, and D, calcium, and iron. Intakes of fat, sodium, and carbohydrate exceed recommended levels.
• Functional outcome: An interprofessional assessment of her functional status indicates poor endurance and physical performance during therapy sessions. Grip strength is significantly reduced for age and gender. The loss of muscle mass is difficult to determine, but Dual-energy X-ray Absorptiometry could confirm sarcopenic obesity.
• Nutrition diagnosis: Severe malnutrition in the context of acute injury as evidenced by significantly reduced energy intake for more than 5 days and reduced grip strength for age and gender.
Nutrition intervention
Consultations with the RD to determine a menu plan to achieve estimated energy needs and provide consistent carbohydrates at each meal to improve glucose control. A daily multivitamin with minerals is recommended. Since she is at risk for pressure ulcers, a mixed (protein, carbohydrate, vitamin, and minerals) oral nutritional supplement is recommended in the evening to avoid any reduction in intake at mealtime. Follow up laboratory tests are recommended to assess for potential vitamin mineral deficiencies.
Pressure ulcer treatment
A 75-year-old resident was admitted to a skilled nursing facility 6 months ago following hospitalization for a cerebrovascular accident. Additional diagnoses included hypertension, chronic obstructive pulmonary disease (COPD), and pressure ulcers. Current medications control his hypertension. He has a stage IV pressure ulcer on his coccyx measuring 3.2 cm×1.7 cm and a stage III on his right hip measuring 2.5 cm×3.0 cm. His admission height was 67 inches (170.1 cm) and weight was 155 pounds (70.4 kg) with a BMI of 24.3 kg/m2. His wife stated his appetite has declined in the last few years. His weight 6 months ago, before the cerebrovascular accident, was 176 pounds, BMI of 27.6. This indicates a 12% unintended weight loss. Currently, his intake is <75% of his estimated energy and protein requirements and he has difficulty chewing. A physical examination revealed a moderate loss of subcutaneous fat, a moderate loss of muscle mass, and a generalized decline of physical strength. He was unable to rise from a sitting position without assistance and his handgrip strength was poor. Laboratory test results include fasting glucose, 108 mg/dL (70–100 mg/dL); blood urea nitrogen (BUN), 22 mg/dL (10–20 mg/dL); serum albumin, 4.2 g/dL (3.5–5.0 g/dL); prealbumin, 15 mg/dL (15–36 mg/dL); creatinine, 1.0 mg/dL (0.6–1.2 mg/dL); sodium, 147 mEq/L (136–145 mEq/L); potassium, 4.0 mEq/L (3.5–5.3 mEq/L); C-reactive protein, 19 mg/L (<1 mg/dL). He is on a mechanical soft diet with nectar thick liquids. Water intake from foods and beverages is estimated to be less than 1,000 mL/day.
Clinical malnutrition
Chronic disease-associated malnutrition:
• History and clinical diagnosis: Declining nutrition status based on an intake of less than 75% of estimated energy and protein requirement plus an unintended weight loss of 12% in 6 months. He also has COPD and several pressure ulcers, which are conditions, associated with a chronic inflammatory response of mild to moderate degree. He developed a stage IV pressure ulcer on his coccyx measuring 3.2 cm×1.7 cm and a stage III on his right hip measuring 2.5 cm×3.0 cm since admission.
• Clinical signs/physical examination: A nutrition-focused examination noted a moderate loss of subcutaneous fat, a moderate loss of muscle mass, and poor handgrip strength.
• Anthropometric data: Unintended weight loss of more than 10% in 6 months in the absence of edema.
• Laboratory values: Laboratory test results, including elevated BUN, serum sodium, and albumin, suggest suboptimal water intake. The C-reactive protein level is consistent with inflammation.
• Dietary intake: The suboptimal water intake and diet is inadequate in energy and protein.
• Functional outcomes: Grip strength is significantly reduced for age and gender. Physical performance consistent with functional impairment.
• Nutrition diagnosis: Severe malnutrition in the context of chronic illness as evidenced by intake of <75% of estimated energy and protein requirement for more than 1 month, unintended weight loss of more than 10% in 6 months, and significantly reduced grip strength for age and gender.
Nutrition intervention
Physician orders consultation with the speech language therapist to determine the appropriate diet texture to improve intake. Based on the NPUAP/EPUAP pressure ulcer treatment guidelines,27 the RD assesses energy requirements to be between 2,113 and 2,465 kcal/day (30–35 kcal/kg body weight [bw]) and estimates protein requirements to be between 87.5 and 105 g/protein/day (1.25–1.5 g/kg bw). A high-calorie/protein oral nutritional supplement is recommended twice a day between meals. A multivitamin with minerals is recommended and fluids are encouraged to achieve a goal of 2,000–2,200 mL daily. The interprofessional team will initiate weekly weights and monitor the daily intake to ensure the individual is ingesting the desired calories to meet nutrient needs. The nutrition plan will be reviewed weekly and adjusted to reflect progress toward the outcome of improving nutritional status and healing. Renal function will be assessed to ensure that high levels of protein are appropriate and tolerated.
Summary
The goal for implementation of clinical practice guidelines in all health care settings is to improve clinical outcomes. The NPUAP Clinical Practice Guidelines include nutrition recommendations for individuals at risk for pressure ulcers and with pre-existing pressure ulcers. Recently published Consensus Guidelines for Identification of Malnutrition are a companion tool to assist clinicians in risk assessment using evidence-based criterion.
Malnutrition is a major contributor to decreased functionality, quality of life, and increased morbidity and mortality. Depleted lean body mass is a predictor of adverse events among the elderly and those at risk for pressure ulcers. Clinicians should utilize the standardized approach described to diagnose malnutrition and select diagnostic descriptors to document its presence in individuals. This approach will facilitate better correlation between best practices related to nutrient needs and the prevention and treatment of pressure ulcers. Integrating the recommended diagnostic characteristics for malnutrition into practice centers care on the individual and a nutrition intervention designed to promote positive outcomes. Early nutrition intervention that supports lean body reserves during a period of inflammatory stress can serve to prevent or delay protein and energy deficits and their impact on pressure ulcer risk and healing.
Take-Home Messages.
• Nutrition recommendations for individuals with pre-existing pressure ulcers or at risk for ulcer development can be found in the NPUAP Clinical Practice Guidelines. Risk assessment can be guided by the recently published Consensus Guidelines for Identification of Malnutrition.
• Malnutrition is a major contributor to decreased functionality, quality of life, and increased morbidity and mortality. Depleted lean body mass is a predictor of adverse events among the elderly and those at risk for pressure ulcers.
• Using the described approach to diagnose malnutrition will facilitate better correlation between best practices related to nutrient needs and the prevention and treatment of pressure ulcers.
• Integrating the recommended diagnostic characteristics for malnutrition into practice focuses care on the patient and nutrition intervention to promote positive outcomes.
• Early nutrition intervention supports lean body reserves by preventing or delaying protein and energy deficits and their impact on pressure ulcer risk and healing.
Abbreviations and Acronyms
- ADRM
acute disease-related malnutrition
- ASPEN
American Society for Parenteral and Enteral Nutrition
- BMI
body mass index
- BUN
blood urea nitrogen
- bw
body weight
- CDRM
chronic disease-related malnutrition
- COPD
chronic obstructive pulmonary disease
- EPUAP
European Pressure Ulcer Advisory Panel
- Hgb A1C
hemoglobin A1C
- LBM
lean body mass
- NPUAP
National Pressure Ulcer Advisory Panel
- NS
nutrition supplement
- NSSRM
nonsevere starvation-related malnutrition
- RD
Registered Dietitian
- SSRM
severe starvation-related malnutrition
Author Disclosure and Ghostwriting
No competing financial interests exist. The content of this article was expressly written by the authors listed. No ghostwriters were used to write this article.
About the Authors
Mary Litchford, PhD, RD, LDN, is a speaker, author, medical/legal expert, and healthcare consultant. She received her PhD in nutrition from University of North Carolina–Greensboro and is president of CASE Software & Books. Her professional career has encompassed clinical practice, university teaching, and consulting. She is on the National Pressure Ulcer Advisory Panel (NPUAP) Board of Directors and served on the Academy's Wound Care Expert work group. Becky Dorner, RDN, LD, is President of Becky Dorner & Associates, Inc., and Nutrition Consulting Services, Inc. She is currently on the Academy of Nutrition and Dietetics Board of Directors and is Past Speaker of the House of Delegates; was on Research Committee and Evidence Analysis Library; and is an alumna of the NPUAP Board of Directors. Mary Ellen Posthauer, RD, LD, is past president of NPUAP and chaired the Prevention and Treatment Guidelines nutrition work group. She coauthored chapters in Wound Care Essentials, Wound Care, and Chronic Wound Care. She writes the nutrition blog for Wound Source and is on the Editorial Advisory Board of Advances in Skin and Wound Care. Mary Ellen has spoken nationally and internationally on nutrition.
References
- 1.Horn S: National pressure ulcer LTC study: pressure ulcer development in LTC residents. JAGS 2004; 52:359. [DOI] [PubMed] [Google Scholar]
- 2.Bergstrom N. and Braden B: A prospective study of pressure sore risk among institutionalized elderly. JAGS 1992; 40:747. [DOI] [PubMed] [Google Scholar]
- 3.Berlowitz DR. and Wilking SV: Risk factors for pressure sores. A comparison of cross-sectional and cohort-derived data. JAGS 1989; 37:1043. [DOI] [PubMed] [Google Scholar]
- 4.Breslow RA. and Bergstrom N: Nutritional predication of pressure ulcers. J Am Diet Assoc 1994; 94:1301. [DOI] [PubMed] [Google Scholar]
- 5.Bourdel-Marchasson I. and Barateau M: A multi-center trial of the effects of oral nutritional supplementation in critically ill older inpatients. Nutrition 2000; 16:1. [DOI] [PubMed] [Google Scholar]
- 6.Ek AC, Unosson M, Larsson J, Von Schenck H, and Bjurulf P: The development and healing of pressure sores related to the nutritional state. Clin Nutr 1991; 10:245. [DOI] [PubMed] [Google Scholar]
- 7.Gilmore S, Robinson G, Posthauer ME, and Raymond J: Clinical indicators associated with unintentional weight loss and pressure ulcers in elderly residents of nursing facilities. J Am Diet Assoc 1995; 95:984. [DOI] [PubMed] [Google Scholar]
- 8.Piloian BB: Defining characteristics of the nursing diagnosis ‘high risk for impaired skin integrity’. Decubitus 1992; 5:32. [PubMed] [Google Scholar]
- 9.Fry D. and Pine M: Patient characteristics and the occurrence of never events. Arch Surg 2010; 145:148. [DOI] [PubMed] [Google Scholar]
- 10.Barker L, Gout B, and Crowe T: Hospital malnutrition: prevalence, identification and impact on patients and the healthcare system. Int J Environ Res Public Health 2011; 8:514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Törmä J, Winblad U, Cederholm T, and Saletti A: Does undernutrition still prevail among nursing home residents? Clin Nutr 2013; 32:562. [DOI] [PubMed] [Google Scholar]
- 12.White J: Consensus statement: AND and ASPEN: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet 2012; 112:730. [DOI] [PubMed] [Google Scholar]
- 13.Keys A: Chronic undernutrition and starvation with notes on protein deficiency. JAMA 1948; 138:500. [DOI] [PubMed] [Google Scholar]
- 14.Blackburn GL, Bistrian BR, Maini BS, Schlamm HT, Smith MF: Nutritional and metabolic assessment of the hospitalized patient. JPEN J Parenter Enteral Nutr 1977; 1:11. [DOI] [PubMed] [Google Scholar]
- 15.Martin CT, Kayser-Jones J, Stotts NA, Porter C, and Froelicher ES: Risk for low weight in community-dwelling, older adults. Clin Nurse Spec 2007, 21:203. [DOI] [PubMed] [Google Scholar]
- 16.Ledikwe JH. and Smiciklas-Wright H: Dietary patterns of rural older adults are associated with weight and nutritional status. J Am Geriatr Soc 2004; 52:589. [DOI] [PubMed] [Google Scholar]
- 17.Lee SJ, Lindquist K, Segal MR, and Covinsky KE: Development and validation of a prognostic index for 4-year mortality in older adults. JAMA 2006; 295:801. [DOI] [PubMed] [Google Scholar]
- 18.Doweiko JP. and Nompleggi DJ: Role of albumin in human physiology and pathophysiology. JPEN J Parenter Enteral Nutr 1991; 15:207. [DOI] [PubMed] [Google Scholar]
- 19.Doweiko JP. and Nompleggi DJ: The role of albumin in human physiology and pathophysiology, Part III: albumin and disease states. JPEN J Parenter Enteral Nutr 1991; 15:476. [DOI] [PubMed] [Google Scholar]
- 20.Ferguson M, Capra S, Bauer J, and Banks M: Development of a valid and reliable malnutrition screening tool for adult acute hospital patients. Nutrition 1999; 15:458. [DOI] [PubMed] [Google Scholar]
- 21.Friedman A. and Fadem S: Reassessment of albumin as a nutritional marker in kidney disease. J Am Soc Nephrol 2010; 21:223. [DOI] [PubMed] [Google Scholar]
- 22.Gabay C. and Kushner I: Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 1999; 340:448. [DOI] [PubMed] [Google Scholar]
- 23.Covinsky KE: Malnutrition and bad outcomes. J Gen Intern Med 2002; 17:956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson AM: Low levels of plasma proteins: malnutrition or inflammation? Clin Chem Lab Med 1999; 37:91. [DOI] [PubMed] [Google Scholar]
- 25.Johnson AM. and Merlini G: Clinical indications for plasma protein assays: transthyretin (prealbumin) in inflammation and malnutrition. Clin Chem Lab Med 2007; 45:419. [DOI] [PubMed] [Google Scholar]
- 26.Kane RL, Talley KM, Shamliyan T, and Pacala JT: Common Syndromes in Older Adults Related to Primary and Secondary Prevention. Evidence Report/Technology Assessment No. 87. AHRQ Publication No. 11-05157-EF-1. Rockville, MD: Agency for Healthcare Research and Quality, July2011 [PubMed] [Google Scholar]
- 27.National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel: Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Washington DC: NPUAP, 2009 [Google Scholar]
- 28.Jensen GL, Bistrian B, Roubenoff R, and Heimburger DC: Malnutrition syndromes: a conundrum vs continuum. JPEN J Parenter Enteral Nutr 2009; 33:710. [DOI] [PubMed] [Google Scholar]
- 29.Jensen GL, Mirtallo J, Compher C, Dhaliwal R, Forbes A, Grijalba RF, Hardy G, Kondrup J, Labadarios D, Nyulasi I, Castillo Pineda JC, Waitzberg D; International Consensus Guideline Committee: Adult starvation and disease-related malnutrition: a proposal for etiology-based diagnosis in the clinical practice setting from the International Consensus Guideline Committee. JPEN J Parenter Enteral Nutr 2010; 34:156. [DOI] [PubMed] [Google Scholar]
- 30.Soeters PB. and Schols AM: Advances in understanding and assessing malnutrition. Curr Opin Clin Nutr Metab Care 2009; 12:487. [DOI] [PubMed] [Google Scholar]
- 31.Sackett DL, Rosenberg WM, Gray JA, Haynes RB, and Richardson WS: Evidence based medicine. What it is and what it isn't. BMJ 1996; 312:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Academy of Nutrition and Dietetics: Introduction—Wound Care Evidence Analysis Project http://adaevidencelibrary.com/topic.cfm?cat=4871 (accessed October3, 2012)
- 33.Kondrup J: Can food intake in hospitals be improved? Clin Nutr 2001; 20 (Suppl 10):153 [Google Scholar]
- 34.Bankhead R, Boullata J, Brantley S, Corkins M, Guenter P, Krenitsky J, Lyman B, Metheny NA, Mueller C, Robbins S, Wessel J; A.S.P.E.N. Board of Directors: Enteral nutrition practice recommendations. JPEN J Parenter Enteral Nutr 2009; 33:122. [DOI] [PubMed] [Google Scholar]
- 35.American Dietetic Association Evidence Analysis Library: Critical illness (CI) Evidence-based nutrition practice guideline. Critical illness nutrition practice recommendations. http://adaevidencelibrary.com/topic.cfm?cat=3016 (accessed July12, 2010)
- 36.Rosenbaum K, Wang J, Pierson RN, and Kotler DP: Time-dependent variation in weight and body composition in healthy adults. JPEN J Parenter Enteral Nutr 2000; 24:52. [DOI] [PubMed] [Google Scholar]
- 37.Klein S, Kinney J, Jeejeebhoy K, Alpers D, Hellerstein M, Murray M, and Twomey P: Nutrition support in clinical practice: review of published data and recommendations for future research directions. Summary of a conference sponsored by the National Institutes of Health, American Society for Parenteral and Enteral Nutrition, and American Society for Clinical Nutrition. JPEN J Parenter Enteral Nutr 1997; 21:133. [DOI] [PubMed] [Google Scholar]
- 38.Sacks G, Dearman K, Replogle W, Cora VL, Meeks M, and Canada T: Use of subjective global assesment to identify nutrition-associated complications and death in long term care facility residents. J Am Coll Nutr 2000; 19:570. [DOI] [PubMed] [Google Scholar]
- 39.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinková E, Vandewoude M, Zamboni M; European Working Group on Sarcopenia in Older People: Sarcopenia: consensus on definition and diagnosis (Report of the European Working Group on Sarcopenia in Older People). Age Aging 2010; 39:412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Soeters PB, Reijven PLM, van Bokhorst-de van der Schueren MAE, Schols JM, Halfens RJ, Meijers JM, and van Gemert WG: A rational approach to nutritional assessment. Clin Nutr 2008; 27:706. [DOI] [PubMed] [Google Scholar]
- 41.Matos LC, Tavares MM, and Amaral TF: Handgrip strength as a hospital admission nutritional risk screening methods. Eur J Clin Nutr 2007; 61:1128. [DOI] [PubMed] [Google Scholar]
- 42.Windsor JA. and Hill GL: Grip strength: a measure of the proportion of protein loss in surgical patients. Br J Surg 1988; 75:880. [DOI] [PubMed] [Google Scholar]
- 43.Schlussel MM, dos Anjos LA, de Vasconcellos MTL, and Kac G: Reference values of handgrip dynamometry of healthy adults: a population-based study. Clin Nutr 2008; 27:601. [DOI] [PubMed] [Google Scholar]
- 44.Norman K, Stobaus N, Gonzalez MC, Schulzke J-D, and Pirlich M: Hand grip strength: outcome predictor and marker of nutritional status. Clin Nutr 2011; 30:135. [DOI] [PubMed] [Google Scholar]
- 45.Sullivan DH, Roberson PK, Johnson LE, Mendiratta P, Bopp MM, Bishara O: Association between inflammation-associated cytokines, serum albumin, and mortality in the elderly. JAMDA 2007; 8:458. [DOI] [PubMed] [Google Scholar]
- 46.American Dietetic Association Evidence Analysis Library: Does serum albumin correlate with weight loss in four models of prolonged protein-energy restriction: anorexia nervosa, non-malabsorptive gastric partitioning bariatric surgery, calorie-restricted diets or starvation. http://adaevidencelibrary.com/conclusion.cfm?conclusion_statement_id=251263&highlight=albumin&home=1 (accessed January2, 2012)
- 47.American Dietetic Association Evidence Analysis Library: Does serum prealbumin correlate with weight loss in four models of prolonged protein-energy restriction: anorexia nervosa, non-malabsorptive gastric partitioning bariatric surgery, calorie-restricted diets or starvation. http://adaevidencelibrary.com/conclusion.cfm?conclusion_statement_id=251313&highlight=prealbumin&home=1 (accessed January2, 2012)
- 48.National Alliance for Infusion Therapy and the American Society for Parenteral and Enteral Nutrition Public Policy Committee and Board of Directors: Disease-related malnutrition and enteral nutrition therapy: a significant problem with a cost-effective solution. Nutr Clin Pract 2010; 25:548. [DOI] [PubMed] [Google Scholar]
- 49.Guralnik JM. and Ferrucci L: Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med 1995; 332:556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, and Wallace RB: A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 1994; 49:M85. [DOI] [PubMed] [Google Scholar]