Abstract
Early work suggested that dietary cholesterol increases plasma total cholesterol concentrations in humans. Given the relationship between elevated plasma cholesterol concentrations and cardiovascular disease risk dietary guidelines have consistently recommended limiting food sources of cholesterol. Current intakes are approaching recommended levels. Recently there have been calls to reassess the importance of continuing to recommend limiting dietary cholesterol. Over the past 10 years there have been a limited number of studies addressing this issue. Striking among these studies is the high degree of variability in background diet, subject characteristics and study design. Within the context of current levels of dietary cholesterol intake, the effect on plasma lipids concentrations, with primary interest in LDL-C cholesterol concentrations, is modest and appears to be limited to population subgroups. In these cases, restrictions in dietary cholesterol intake are likely warranted. The biological determinants of inter-individual variability remain a relatively understudied area.
Keywords: Dietary cholesterol, Plasma cholesterol, Low density lipoprotein cholesterol, High density lipoprotein cholesterol, Total cholesterol:high density lipoprotein cholesterol ratio, Eggs, Cardiovascular disease, Cholesterol absorption
Introduction
Cardiovascular disease (CVD) is the leading cause of mortality in developed and developing countries [1]. Dyslipidemia, high low density lipoprotein cholesterol (LDL-C) and triglyceride concentrations, and low high density lipoprotein cholesterol (HDL-C) concentrations, are associated with elevated CVD risk [2]. There are many factors that impact on plasma lipoprotein profiles, including those that are non-modifiable (e.g., age, genetics) and modifiable (e.g., diet, physical activity). One that received considerable attention early in the elucidation phase of the diet/heart disease hypothesis is dietary cholesterol [3].
In humans, there is a linear relationship between dietary cholesterol up to about 1000 mg/day and plasma cholesterol concentrations [4]. Most recommendations to reduce CVD risk include limiting dietary cholesterol to 200 or 300 mg per day [2, 4–6]. Mean intakes in the U.S. are currently estimated to be 224 mg and 333 mg cholesterol per day for females and males, respectively. This review addresses the relationship between dietary cholesterol and plasma lipoprotein profiles, and is limited to randomized controlled trials published within the past 10 years.
Cholesterol
The cholesterol molecule has a steroid structure and hydrocarbon side chain. Technically it is a sterol because it is composed of a steroid and alcohol. Cholesterol has multiple functions in the human body. It is a precursor for steroid hormones (gonadal and adrenal), vitamin D and bile acids, and is a structural component of cell membranes and lipoprotein particles (reviewed, [7]). The substrate for cholesterol synthesis is acetyl CoA, an intermediate of fat, carbohydrate and protein metabolism.
The total body cholesterol pool reflects a balance between de novo synthesis, dietary intake, absorption efficiency, metabolism, enterohepatic recirculation and excretion (either as cholesterol or bile acids). One of the primary tissues responsible for cholesterol homeostasis is the liver. Hepatic cholesterol is determined by a balance between LDL uptake from plasma and intracellular de novo synthesis. Liver cells have LDL receptors that are subject to feedback inhibition. These receptors recognize apoprotein (apo) B100, the protein component of the LDL particle, and apo E, an apoprotein component of chylomicron remnant, very low density lipoprotein and intermediate density lipoprotein particles. After binding apo B100 or E present on the surface of lipoprotein particles, the LDL receptor and the particle are taken up into the cell by endocytosis. The receptor can be recycled, the lipoprotein particle is disassembled into its constituent components. The subsequent release of free cholesterol into the cytosol has three main effects: (1) inhibition of 3-hydroxy-3-methyl-glutaryl-CoA CoA (HMG CoA) reductase activity, the rate limiting enzyme in cholesterol biosynthesis, , slowing the rate of de novo cholesterol synthesis; (2) increase of the activity of acyl CoA cholesterol acyltransferase (ACAT), the enzyme that esterifies intracellular cholesterol, yielding a more non-polar molecule that coalesces into intracellular lipid droplets; and (3) inhibition of LDL receptor synthesis, resulting in a decreased uptake rate of LDL from plasma. These mechanisms allow for a reciprocal relationship between plasma LDL cholesterol concentrations and hepatic de novo cholesterol synthesis (reviewed, [8]).
The intestine plays an important role in whole body cholesterol balance by regulating cholesterol absorption. Intestinal cholesterol is derived from dietary sources, sloughed cells from the intestinal lining, and direct secretion via bile (reviewed [9]). The process by which cholesterol is absorbed is complex, involving a balance between transport into the enterocytes, facilitated by the Niemann-Pick C1 -like 1 (NPC1L1) protein, and transport out of the enterocytes by ATP-binding cassette (ABC) G5/8 and possibly by an alternate pathway termed transintestinal cholesterol efflux. Free cholesterol associated with NPC1L1 is delivered to the endoplasmic reticulum where the majority is esterified by ACAT and incorporation into chylomicron particles for subsequent secretion into the lymphatic system. The portion of intracellular cholesterol that remains unesterified forms a pool for potential resecretion into the intestinal lumen. Plant sterols (phytosterols) are structurally similar to cholesterol. They interfere with cholesterol absorption by displacing cholesterol from intestinal micelles. They are poor substrates for ACAT, hence, a high proportion are resecreted into the intestinal lumen. Plant sterols have a low absorption efficiency, 1% to 3%, compared to 50% to 60% for cholesterol. Another factor mediated by the intestine that impacts on the whole body cholesterol pool is bile acids, a metabolic product of cholesterol. After secretion into the intestine, bile acids are recycled by an extremely efficient process of enterohepatic recirculation facilitated by apical Na-dependent bile acid transporters. Any interference with this cycle will result in a net loss of bile acids in the stool, forcing the body to draw from the cholesterol pool to synthesize bile acids.
Dietary Cholesterol and Plasma Cholesterol
Early work suggested that dietary cholesterol increased plasma total cholesterol concentrations in humans[10]. Subsequent work confirmed this early observation [11–13]. Given the relationship between elevated plasma cholesterol concentrations and CVD risk, dietary guidelines have consistently recommended limiting food sources of cholesterol [2, 5, 14–19]. Recent reviews on the topic have questioned whether the relationship is still relevant within the context of current cholesterol intakes [20–22]. The issue remains unresolved. One issue difficult to factor into dietary cholesterol recommendations is individual responsiveness. It has been clearly shown that individuals vary considerably with respect to their response to dietary cholesterol [23]. Subsequent work has demonstrated that the distinction between hyperresponders or hyporesponders has a genetic basis, dependent on polymorphisms in the cholesterol transporters ABCG5/8 and NPC1L1, among others [24]. However, at this time there is no simple way to determine whether an individual is a hyperresponder or hyporesponder to dietary cholesterol.
Dietary Cholesterol
Potential sources of dietary cholesterol are limited to animal foods; eggs, dairy products and meat. The majority of dietary cholesterol in the U.S. diet comes from eggs and egg mixed dishes (24.6% of total cholesterol intake) [25]. Chicken and chicken mixed dishes (12.5%) and beef, beef mixed dishes and burgers (11.0%) are the two next largest contributors. These are followed by regular cheese (4.2%), sausage, franks, bacon and ribs (3.9%), fish and fish mixed dishes (3.4%), grain-based desserts (3.3%), dairy desserts (3.2%), pasta and pasta dishes (3.1%), pizza (2.9%), Mexican mixed dishes (2.9%), cold cuts (2.7%), reduced fat milk (2.5%), pork and pork mixed dishes (2.3%), and shrimp and shrimp mixed dishes (2.0%). Together, these sources account for 85% of total dietary cholesterol.
Literature Identification
Studies that assessed the effect of dietary cholesterol on plasma lipoprotein profiles in humans were identified by electronic searches of the MEDLINE database using search criteria "cholesterol, dietary"[MeSH Terms] or "cholesterol"[All Fields] and "dietary"[All Fields] or "dietary cholesterol"[All Fields] or "dietary"[All Fields] and "cholesterol"[All Fields] and "eggs"[MeSH Terms] OR "eggs"[All Fields] and “dietary cholesterol”]. Predetermined inclusion criteria were: (1) published between 3/1/2003 and 2/28/2013; (2) published in the English language; (3) conducted using a human subjects; (4) included data for at least three of the following (not necessarily a primary analysis), total cholesterol (TC), LDL-C, HDL-C and triglyceride concentrations, and TC:HDL-C ratio; (5) included an intervention which increased dietary cholesterol by a minimum of 200 mg/day; and (6) held dietary fat type constant. Both cross-over and parallel design studies were included. Reviews, case reports and observational studies were not included.
Results
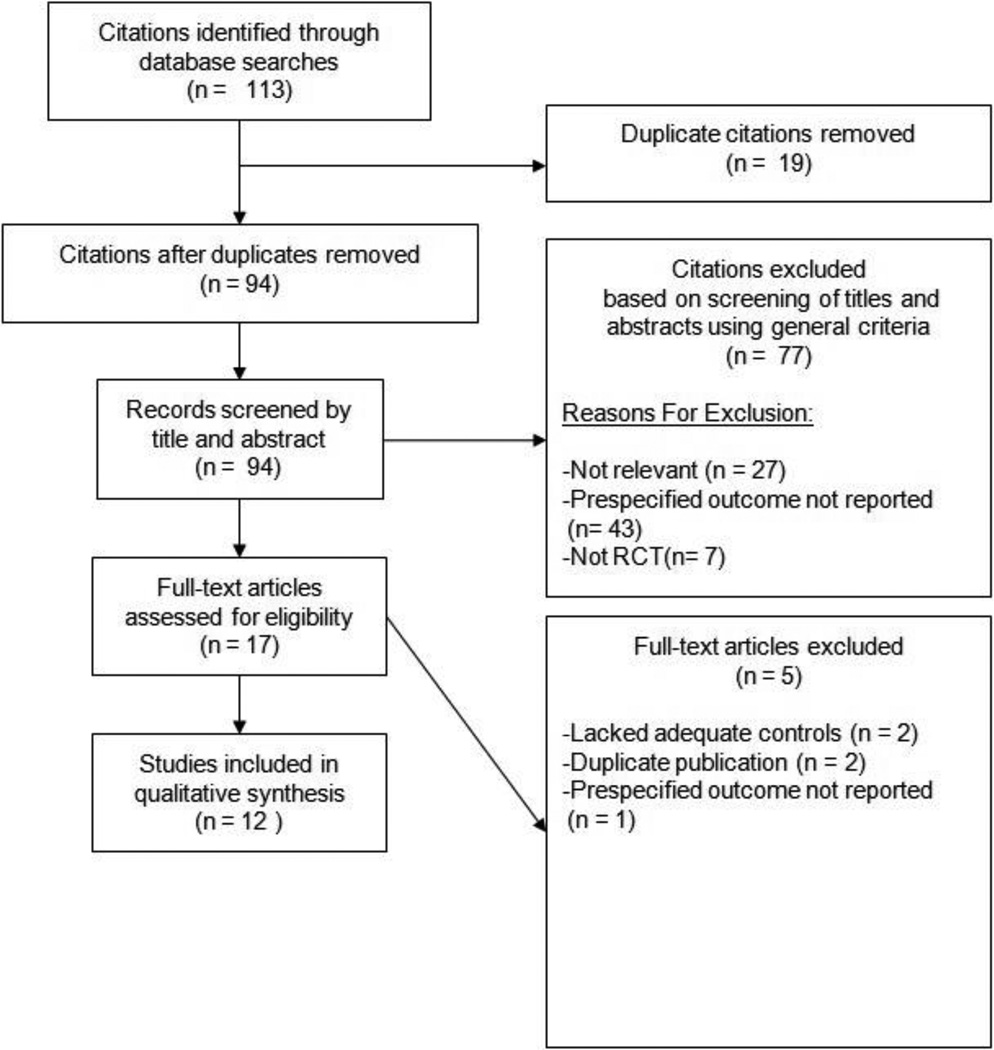
The electronic database searches resulted in 112 citations (Figure). Seventeen studies met the inclusion criteria on the basis of abstract screening and 12 studies remained on the basis of full text screening (Table). Of the 12 studies, 7 controlled for the background diet [26–32] and 5 studies did not control or did not specify whether they controled for background diet [33–37]. In 3 of those 7 studies, subjects were instructed to modify their diets to promote weight loss [26– 28] and 4 studies were specifically designed to maintain body weight [29–32]. In the vast majority of studies, eggs were used as the source of dietary cholesterol.
Figure 1.
Flow diagram showing the assessment of intervention trials involving dietary cholesterol from 2003–2013
Table 1.
Characteristics of studies included in review of dietary cholesterol intervention trials conducted within the past 10 years
| Citation | N(Agerange[y]) | Study Design (durationinter- vention[w]) |
Subject Characteristic(s) |
Background Diet |
Dietary Cholesterol |
Total Cholesterol |
LDL-C | HDL-C | Triglyceride | TC:HDL | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Treatment/ Control |
Source | Baseline/ Final [mmol/L] |
P-value | Baseline/ Final [mmol/L] |
P-value | Baseline/ Final [mmol/L] |
P-value | Baseline/ Final [mmol/L] |
P-value | Baseline/ Final |
P-value | |||||
| Pearce et al., 2011 [26] |
65(20–75) | Parallel(12) | Type 2 diabetics |
Energy restricted, high protein |
590mg/ 213mg |
2eggs 1egg |
C:4.81±0.15/ 4.51±0.15 T:4.66±0.18/ 4.60±0.18 |
NS p=0.09 |
C:2.76±0.13/ 2.71 ±0.13 T:2.66±0.13/ 2.80±0.13 |
NS | C:1.24±0.05/ 1.17±0.01 T:1.21±0.05/ 1.24±0.05 |
0.01 | C:1.80±0.16/ 1.39±0.16 T:1.77±0.16/ 1.36±0.16 |
NS | C:4.04±0.18/ 3.97±0.18 T:4.02±0.23/ 3.88±0.23 |
NS |
| Isherwood et al., 2010 [33] |
23(20–70) | RCT(4) | Normo- lipidemic |
NA | 794mg | Cold water prawns (225g) |
C:5.12±0.92/ 5.09±0.81 T:5.08±1.08/ 5.11±0.83 |
NS | C:2.98±0.69/ 2.98±0.64 T:2.94±0.84/ 3.02±0.65 |
NS | C:1.58±0.44/ 1.55±0.42 T:1.56±0.44/ 1.57±0.39 |
NS | C:1.22±0.57/ 1.23±0.42 T:1.26±0.46/ 1.16±0.43 |
NS | NA | NA |
| Njike et al, 2010 [34] |
40(35–77) | RCT(6) | Hyperlipid- emic |
NA | NA | 2 eggs | C:6.31±0.62/ 5.87±0.70 T:6.31 ±0.62/ 6.18±0.70 |
<0.01 | C:4.34±0.44/ 3.98±0.62 T:4.34±0.44/ 4.27±0.62 |
0.0 1 | C:1.34±0.38/ 1.29±0.34 T:1.34±0.38/ 1.32±0.36 |
NS | C:1.49±0.59/ 1.31±0.56 T:1.49±0.59/ 1.33±0.53 |
NS | C:5.0±1.3/ 4.8±1.3 T:5.0±1.3/ 5.0±1.2 |
NS |
| Mutungi et al., 2008 [27] |
28(40–70) | RCT(12) | BMI between 26–37 kg/m2 |
Carbohydrate restricted diet (10–15% energy) |
640mg above baseline/ 0 mg above baseline |
3 liquide ggs |
C:4.87±0.87/ 4.84±1.02 T:5.13±1.09/ 5.23±1.08 |
NS | C:2.87±0.89/ 3.14±1.09 T:3.30±1.09/ 3.73±1.17 |
NS | C:1.29±0.25/ 1.26±0.23 T:1.23±0.39/ 1.48±0.39 |
<0.01 | C:1.42±0.78/ 0.87±0.37 T:1.29±0.56/ 0.79±0.23 |
NS | NA | NA |
| Harman et al., 2008 [28] |
45(18–55) | RCT(12) | NA | Energy restricted diet 500kcal- 100kcal deficit) |
582mg/ 144mg |
2 eggs | C:5.20±0.99/ 4.98±0.91 T:5.34±1.14/ 4.99±1.24 |
NS | C:2.95±0.66/ 2.85±0.51 T:3.02±0.76/ 2.85±0.78 |
NS | C:1.08±0.36/ 1.10±0.32 T:1.12±0.28/ 0.97±0.30 |
NS | C:1.28±0.59/ 1.21 ±0.72 T:1.20±0.56/ 1.11±0.44 |
NS | NA | NA |
| Vislocky et al., 2009 [29] |
11(18–30) | RCT(8) | Unfit (VO2 <45mL× kg−1 ×min−1 for men;<40mL× kg−1× min−1 for women) |
Endurance training regimen prescribed (4–5 days/week, 60 min, 65% vo2 max). isoenergetic diet |
469mg/159mg | 1egg | NA | NS | NA | NS | NA | NS | NA | NS | NA | NA |
| Herron et al., 2006 [30] |
91(mean=30.8) | RCT(4) | Sub group analysis 1) ABCG5C/ Callele 2) ABCG5C/ GandG/ Gallele |
NCEP Step 1 diet |
+640 mg above baseline/+ 0 above baseline |
3 eggs | 1) C:4.37±0.71 T:4.72±0.85 2) C:4.29±0.72 T:4.39±0.71 |
1)<0.05 2) NS |
1) C:2.43±0.63 T:2.72±0.76 2) C:2.35±0.70 T:2.39±0.65 |
1:<0.052:NS | 1) C:1.40±0.30 T:1.47±0.38 2) C:1.45±0.34 T:1.49±0.40 |
1:NS 2:NS |
NA | NA | NA | NA |
| Greene et al., 2005 [35] |
42(>60) | RCT(4) | Normo- cholestero- lemic |
NA | +640mg above baseline/+ 0 mg above baseline |
3 eggs | Men) C:4.42±0.67 T:4.57±0.78 Women) C:4.75±0.88 T:5.06±1.00 |
Men <0.05 Women <0.05 |
Men) C:2.72±0.84 T:2.78±0.72 Women) C:2.72±0.84 T: 2.98±1.05 |
Men: <0.05 Women: <0.05 |
Men) C:1.22±0.33 T:1.34±0.33 Women) C:1.49±0.31 T: 1.53±0.38 |
Men: <0.05 Women: <0.05 |
Men: C:1.09±0.55 T:0.98±0.39 Women:C:1.18±0.67 T: 1.18 ±0.62 |
Men:NS Women:NS |
NA | NA |
| Katz et al., 2005 [36] |
49(36–73) | RCT(6) | Normo- cholesterol- emic |
NA | NA | 2 eggs | 5.27±0.81/ 5.31±0.92 |
NS | 3.23±0.65/ 3.34±0.83 |
NS | 1.36±0.38/ 1.32±0.39 |
NS | 1.53±0.87/ 1.43±0.82 |
NS | NA | NA |
| Chakrabarty et al., 2004 [31] |
34(mean=25.7) | RCT(8) | Subgroup analysis 1) Hyper- responders (risein LDL-C > 15.4%from baseline) 2) Hypo- responders (LDL-C ≤15.4% from baseline) |
Otherwise egg free lacto- vegetarian diet while avoiding baked goods |
300mg/ day above baseline/0mg /day above baseline |
1 egg | Main) C:4.75±0.72 T:4.96±0.77 1) C:4.46±0.64 T:5.28±0.73 2) C:4.91±0.73 T:4.79±0.74 |
Main: NS 1:p<0.025 2:NS |
Main)C:2.71±0.77 T:2.98±32.47 1) C:90.34±0.84 T:3.31±0.82 2) C:3.83±0.76 T:2.81 ±0.81 |
Main:NS 1:p<0.025 2:NS |
Main) C:1.36±0.32 T:1.29±0.31 1) C:1.40±0.36 T:1.23±0.33 2) C:1.34±0.31 T:1.33±0.29 |
Main:NS 1:NS 2:NS |
Main) C:1.29±0.34 T:1.36±0.40 1) C:1.43±0.47 T:1.45±0.55 2) C:1.22±0.24 T:1.31±0.29 |
Main:NS 1:NS 2:NS |
Main) C :3.73±1.24 T:4.07±1.31 1) C:3.42±1.32 T:4.55±1.40 2) C:3.90±1.20 T:3.80±1.21 |
Main: p<0.05 1:p<0.025 2:NS |
| Ballesteros et al., 2004 [37] |
54(8–12) | RCT(4) | Subgroup analysis 1) Hyper- responders (TC change > 0.06 mmol /L/100mg supplemental cholesterol) 2) Hypo- responders (TCchange <0.06mmol /L/100mg supplemental cholesterol) |
NA | 518mg/ day above baseline/ 0 above baseline |
2 egg | NA | NA | 1) C:1.54±0.38 T:1.93±0.36 2) C:1.83±0.44 T:1.88±0.42 |
1:p<0.05 2:NS |
1) C:1.23±0.26 T:1.35±0.29 2) C:1.22±0.19 T:1.28±0.19 |
1:p<0.05 2:NS |
1) C:1.02±0.37 T:1.00±0.68 2)C:1.10±0.47 T:0.93±0.31 |
1:NS 2:NS |
1) C:2.66±0.52 T:2.85±0.57 2) C:3.00±0.53 T:2.96±0.55 |
1:NS 2:NS |
| Knopp et al., 2003 [32] |
197 group 1)49.4±9.3 2)55.0±11.5 3)54.1±9.1 |
RCT (4) | 1) IS(≤4.2(10−4 min−1 uU/mL insulin sensitivity index) 2) IR(>4.2 (10−4 min−1uU/mL insulin sensitivity index) 3) OIR(>4.2 10−4 min−1 uU/mL insulin sensitivity index and BMI >27.5) |
NCEP Step 1 diet |
0 mg/day, 425m/day, 850mg/day |
2 or 4 “egg preparation” /day (34g egg yolk+ 64g Egg Beaters +10g water or 68g egg yolk +20g Egg Beaters+ 10g water, respectively) |
% change from baseline IS) 2 eggss: C:0.7±11.5 T:2.2±9.1 4 eggs: C:0.7±11.5 T:6.2±8.7 IR) 2 eggs: C: −3.0±1.8 T:1.2±7.2 4 eggs: C: −3.0±8.1 T:3.2±9.9 OIR) 2 eggs: C: −1.6±8.3 T: −1.6±10.0 4 eggs: C: −1.6±8.3 T: 2.3±8.1 |
IS) 2 eggs: p<0.05 4 eggs: p<0.001 IR) 2 eggs: NS 4 eggs:p<0.01 OIR)2 eggs:NS 4 eggs:p<0.05 |
% change from baseline IS) 2 eggs: C:1.2±17.1 T:3.3±13.8 4 eggs: C:1.2±17.1 T:7.8±13.7 IR) 2 eggs: C: −2.2±14.3 T:1.5±10.8 4 eggs: C: −2.2±14.3 T:3.3±13.2 OIR) 2 eggs: C:2.1±19.4 T: −1.9±14.94 eggs: C:2.1±19.4 T:2.4±12.6 |
IS)2 eggs:NS 4 eggs:p<0.001 IR)2 eggs:NS 4 eggs:p<0.05 OIR) 2 eggs:NS 4 eggs:NS |
% change from baseline IS) 2 eggs: C:1.5±10.7 T:5.5±10.3 4 eggs: C:1.5±10.7 T:8.8±10.4 IR) 2 eggs: C:−0.8±10.6 T:2.2±8.8 4 eggs: C:0.8±10.6 T:5.2±10.4 OIR) 2 eggs: C:−2.0±11.8 T: −0.2±8.6 4 eggs: C: −2.0±11.8 T:3.6±9.4 |
IS) 2 eggs: p<0.001 4 eggs:p<0.001 IR) 2 eggs: p<0.05 4 eggs: p<0.001 OIR) 2 eggs: NS 4 eggs:p<0.01 |
% change from baseline IS) 2 eggs: C:9.9±48.1 T: −3.3±39.0 4 eggs: C:9.9±48.1 T: −5.5±36.9 IR) 2 eggs: C:2.6±45.5 T:1.1±29.6 4 eggs: C:2.6±45.5 T:0.3±36.6 OIR) 2 eggs: C:8.1±45.7 T:3.2±33.5 4 eggs: C:8.1±45.7 T:5.5±33.2 |
IS) 2 eggs:NS 4 eggs: p<0.05 IR) 2 eggs:NS 4 eggs:NS OIR) 2 eggs:NS 4 eggs:NS |
NA | NA |
Randomized control trials, RCT; not available, NA; not significant, NS; C, control; T, treatment; TC, total cholesterol; LDL–C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol, IS, insulin sensitive; IR, insulin resistant; OIR, obese and insulin resistant
Dietary Cholesterol Supplementation While Controlling for Background Diet Dietary cholesterol supplementation with weight loss
Mutungi et al assessed the effect of carbohydrate restriction and dietary cholesterol in 28 overweight or obese (BMI of 26–37 kg/m2) male subjects aged 40–70 years using a parallel study design [27]. Subjects were instructed to reduce energy intake by consuming a low carbohydrate (10–15% energy carbohydrate) diet and were randomly assigned to supplement this diet with three eggs per day (640 mg cholesterol) or cholesterol-free egg substitute (0 mg cholesterol) which was provided to them for 12 weeks. The intervention resulted in significant reductions in body weight. Plasma LDL-C and triglyceride concentrations were similar between the two intervention groups, whereas HDL-C concentrations were higher in the egg supplemented group.
Harman et al. randomly assigned 67 healthy volunteers aged 18–55 years to an energy restricted diet (500–100 kcals less than baseline). In a parallel study design for 12 weeks subjects received either two eggs per day (438 mg cholesterol) or no supplemental egg [28]. At the end of the study period, both groups lost a similar amount of body weight. The addition of eggs had no significant effect on plasma lipids.
Pearce et al. randomly assigned 65 individuals with type 2 diabetes aged 20 to 75 years to consume a high protein (30% of total energy) hypoenergetic diet (calories reduced 30% from habitual diet) with either 2 eggs per day (590 mg cholesterol per day) or 100 grams of lean protein (213 mg cholesterol per day) [26]. The hypoenergetic diet resulted in weight loss in both the high cholesterol (6.5kg ± 3.2kg) and low cholesterol (5.3kg ± 3.6kg) groups. At the end of 12 week period, plasma HDL-C concentrations were higher in the egg fed group compared to the lean protein group, whereas there was no significant change in the other plasma lipids.
Dietary cholesterol supplementation without weight loss
Using a parallel study design, Vislocky et al. assessed the effect of either 12 eggs/week (469 mg cholesterol/day) or no supplemental eggs (159 mg cholesterol/day) on plasma lipid and apolipoprotein concentrations in 12 normocholesterolemic physically unfit subjects aged 18 to 30 years (men, VO2 peak <45 mL/kg−1 per min−1, and women, <40 mL/kg−1 per min−1) [29]. All diets were similar with regard to macronutrient content (60% carbohydrate, 30% fat, 10% protein) and designed to maintain body weight. Subjects began the dietary intervention two weeks before starting an endurance training program and continued throughout the 6 week training period. Independent of cholesterol intake, endurance training significantly increased HDL-C and decreased LDL-C and apo-B concentrations, and increased plasma cholesterol ester transfer protein activity. Supplementation with an average of one egg per day had no significant effect on plasma lipids or the enzyme parameters assessed.
Knopp et al. studied three groups of individuals: insulin sensitive (Insulin Sensitivity Index Score < 4.2 × 1.0−4 min−1 µU/mL, n=65) (average age 49.4 years); insulin resistant, normal body weight (Insulin Sensitivity Index Score > 4.2 × 1.0−4 min−1 µU/mL; BMI <27.5, n=75) (average age 55.0 years); and insulin resistant, obese (Insulin Sensitivity Index Score > 4.2 × 1.0−4 min−1 µU/mL; BMI >27.5, n=57) (average age 54.1 years) using a randomized cross-over design [32]. Baseline plasma lipid concentrations (0 egg diet period) were not significantly different among the three groups. The dietary interventions were no supplemental eggs, 2 eggs per day (425 mg cholesterol) and 4 eggs per day (850 mg cholesterol). Each intervention period was 4 weeks followed by a 4 week washout. During the intervention, the background diet was standardized by instructing subjects to adhere to the National Cholesterol Education Program (NCEP) Step 1 guidelines (<30% fat, <10% saturated fat and <300 mg cholesterol per day). In insulin sensitive individuals, increasing dietary cholesterol by feeding the equivalent of 4 eggs per day, but not 2 eggs per day, resulted in significant increased in TC, LDL-C, HDL-C, non-HDL-C and apoB concentrations. This pattern was also observed in the two insulin resistant groups, although the differences, for the most part, did not reach statistical significance. These data suggest the effects of dietary cholesterol were more prominent in insulin sensitive than resistant individuals.
Using a randomized cross-over design, Herron et al. instructed 91 individuals (40 men, average age 32.6 years and 51 women, average age 29.5 years) to consume a NCEP Step 1 diet [30]. The dietary variable was 3 eggs per day or a cholesterol-free, fat-free egg substitute. The intervention period was 4 weeks per phase and there was a 3 week washout period. The data were analyzed based on ABCG5 alleles. During the egg supplemented period, individuals with the C/C ABCG5 allele had a significantly greater increase in plasma TC and LDL-C than either the C/G or G/G alleles. The NCEP Step 1 diet resulted in a significant increase in HDL-C concentrations during both diet periods and this was independent of ABCG5 genotype. These results suggest that the ABCG5 allele may affect an individual’s response to changes in dietary cholesterol.
Chakrabarty et al conducted a cross-over design study involving 34 subjects (average age 25.7 years) who were instructed to consume a lacto-vegetarian diet and avoid baked goods (to minimize sources of dietary cholesterol) [31]. The intervention variable was one egg per day (300 mg cholesterol) or no supplemental food. Each diet phase was 8 weeks and was not separation by a washout period. There were no significant differences at the end of the diet periods for TC, LDL-C, HDL-C or triglyceride concentrations. One egg per day resulted in a higher TC:HDL-C ratio. Considerable variability was noted among study subjects. Differences between the diet phases in LDL-C concentrations ranged from 15% to 73%. A secondary analysis was conducted after dividing subjects into two groups, hyperresponders (n=12) and hyporesponders (n=22), defined as having less than or greater than a 15% change in LDL-C concentrations in response to one egg per day. Compared to the no supplemental egg, hyperresponders, but not hyporesponders, had a significantly higher TC and LDL-C concentrations, and TC:HDL-C ratio.
Dietary Cholesterol Supplementation Without Controlling the Background Diet
Katz et al compared the effect of 2 eggs per day (600 mg cholesterol) or uncooked oatmeal (60 g, 0 mg cholesterol) in 49 normocholesterolemic adult subjects (30 men, average age 54.1 years and 19 women, average age 59.2 years) on plasma cholesterol concentrations and brachial artery flow mediated dilation (FMD) using a randomized controlled crossover design [36]. Each diet phase was 6 weeks and there was a 4 week washout phase. Compared to baseline values, the 2 supplemental eggs per day had no significant effect on TC, LDL-C, HDL-C and triglyceride concentrations, or FMD. In contrast, 60 g of uncooked oats resulted in significant reductions in TC and LDL-C, and no changes in HDL-C and triglyceride concentrations, or FMD compared to baseline values.
Using a randomized crossover design, Ballesteros et al. assigned 54 children (8–12 y) to add either 110 grams of eggs, the equivalent of 2 eggs per day (518 mg cholesterol) or an equivalent amount of cholesterol-free egg white substitute [37]. Each diet phase was 30 days and there was a three week washout period. At the end of the study, the children were divided into hyporesponders and hyperresponders based on change in plasma TC concentrations at the end of the egg diet phase; change in TC concentration from baseline less than or greater than 0.05 mmol/L per 100 mg supplemental dietary cholesterol, respectively. The addition of 2 eggs to the diet of hyperresponders significantly increased LDL-C and HDL-C but not triglyceride and apo B concentrations or TC:HDL-C ratio, compared to baseline. There was no significant effect of supplemental dietary cholesterol in the hyporesponders. At the end of the intervention periods, the difference in LDL-C and HDL-C concentrations between hyperresponders and hyporesponders was significant. Supplemental eggs, but not egg substitute, significantly increased mean LDL peak diameter in both hypo- and hyperresponders, accounted for by a reduction in the smaller LDL subfractions.
Greene et al conducted a randomized crossover trial in 42 normocholesterolemic men and postmenopausal women less than 60 years of age comparing the effects of 3 large eggs per day (640 mg cholesterol) or an equivalent amount of cholesterol-free fat-free egg substitute [35]. At the end of each 4 week intervention periods, separated by a 3 week washout period, there was no significant effect of supplemental eggs on TC, LDL-C and HDL-C concentrations, and no significant change in triglyceride concentration or the LDL:HDL ratio compared to the egg substitute period. As reported in previously [37], the supplemental eggs resulted in a significant increase in LDL peak diameter.
Isherwood et al conducted a randomized crossover trial in 23 normocholesterolemic male subjects (aged range 19–67 years) [33]. Subjects were provided with 225 g of cold water prawns per day (750 mg cholesterol) or 225 g of crab sticks per day (200 mg cholesterol) for 4 weeks each with a 4 week washout period. Neither intervention resulted in a significant change in plasma TC, LDL-C, HDL-C, triglyceride, apo A1 and apo B concentrations, or LDL particle size. The authors suggested the lack of an effect may have been attributed to the characteristics of the study subjects, normocholesterolemic, or the non-cholesterol sterol content of the prawns, which may have interfered with cholesterol absorption.
A study performed by Njike and coworkers randomized 40 subjects aged 35 to 77 years and diagnosed with hyperlipidemia (as defined by serum total cholesterol >240 mg/dL, and/or LDL cholesterol >160 mg/dL, and/or a total cholesterol/HDL ratio >5.7) to receive either 2 eggs (400 mg cholesterol) or an equivalent amount of a cholesterol-free egg substitute daily for 6 weeks [34]. There were no additional dietary instructions. At the end of the intervention period there were no significant differences in plasma lipid concentrations in the egg supplemented group, however, in the cholesterol-free egg substitute group, TC and LDL-C concentrations were significantly lower. Triglyceride concentrations were significantly lower, compared to baseline, in both groups. It is difficult to draw conclusions from this study in the absence on data on how the groups receiving the eggs or egg substitute compensated with respect to the other components of the diet. The potential for no change in the dietary cholesterol intake in the group receiving eggs and an exchange of the egg substitute for habitually consumed eggs in the other group cannot be ruled out.
Summary
Among the studies that met our eligibility criteria, there was a wide range of study types, interventions and participants. The study subjects included normolipidemic and hyperlipidemic; adults and children; normal weight and overweight/obese; and insulin sensitive and insulin insensitive. In some studies the data were stratified on the basis of cholesterol responsiveness and ABCG5 genotypes. Diets were fed in amounts intended to maintained body weight or promoted weight loss. Both parallel and cross-over study designs were used. Intervention periods ranged from 4 to 12 weeks. In one case diets were restricted in meat, in other cases study subjects were instructed to follow NCEP Step 1 diet guidelines. The majority of the studies compared eggs as the source of dietary cholesterol, to cholesterol-free egg substitutes.
Most studies assessed the effect of 1–3 eggs per day. The majority of studies that controlled for background diet reported no significant effect on LDL-C concentrations [26–29], or the effect was only significant after subgroup analysis on the basis of responsiveness or genotype [30, 32]. Data for the studies in which the background diet was not controlled were mixed for LDL-C concentrations, with 2 studies reporting no significant effect [33, 36], 1 study reporting no significant effect in hyporesponders and a significant increase in hyperresponders [37], and 1 study reporting no significant effect in response to 2 eggs per day, but a significant decrease in the group receiving the cholesterol-free egg substitute [34]. There were no trends on the basis of whether the intervention included 2 or 3 eggs per day, which represented the majority of the studies, or the length of the intervention period. Those studies that coupled weight loss with supplemental egg intake were less likely to report an effect on LDL-C concentrations. Effects of supplemental eggs on HDL-C concentrations tended to be small, albeit significant in some cases, and generally resulted in an increase. There was little effect of supplemental cholesterol on plasma triglyceride concentrations.
Conclusions
Over the past 10 years, there has been only a limited number of studies on the effect of dietary cholesterol on plasma cholesterol concentrations. Striking among the available studies is the high degree of variability in background diet, study subject characteristics and study design. Within the context of current levels of dietary cholesterol, the effect on plasma lipids concentrations, with primary interest in LDL-C cholesterol concentrations, is modest and appears to be limited to population subgroups. In these cases, restrictions in dietary cholesterol intake are likely warranted. The biological determinants of inter-individual variability remain a relatively understudied area.
Footnotes
Compliance with Ethics Guidelines
Conflict of Interest
John D. Griffin has received financial support through the National Institutes of Health (NIH) Obesity and Metabolism Training Grant Fellowship. Alice H. Lichtenstein declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Contributor Information
John D. Griffin, Tufts University, JM USDA Human Nutrition Research Center on Aging, 711 Washington Street, Boston, MA 02111, John.Griffin@Tufts.edu
Alice H. Lichtenstein, Tufts University, JM USDA Human Nutrition Research Center on Aging, 711 Washington Street, Boston, MA 02111, phone: 617 556 3127, Alice.Lichtenstein@Tufts.edu
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, et al. Executive summary: heart disease and stroke statistics-2013 update: a report from the American Heart Association. Circulation. 127:143–152. doi: 10.1161/CIR.0b013e318282ab8f. [DOI] [PubMed] [Google Scholar]
- 2.Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Executive summary of the third report of the National Cholesterol Education Program (NCEP) Journal of the American Medical Association. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 3.Finking G, Hanke H. Nikolaj Nikolajewitsch Anitschkow (1885–1964) established the cholesterol-fed rabbit as a model for atherosclerosis research. Atherosclerosis. 1997;135:1–7. doi: 10.1016/s0021-9150(97)00161-5. [DOI] [PubMed] [Google Scholar]
- 4.IOM. National Academy of Sciences. Washington, DC: 2005. Dietary reference intakes. Energy, carbohdyrate, fiber, fat, fatty acids, cholesterol, protein and amino acids; p. 482. [Google Scholar]
- 5.Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, Franklin B, Kris-Etherton P, Harris WS, Howard B, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114:82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]
- 6.Dietary Guidelines for Americans. 2010 http://www.cnpp.usda.gov/DGAs2010-DGACReport.htm.
- 7.Lecerf J-M, de Lorgeril M. Dietary cholesterol: from physiology to cardiovascular risk. British Journal of Nutrition. 106:6–14. doi: 10.1017/S0007114511000237. [DOI] [PubMed] [Google Scholar]
- 8.van der Wulp MY, Verkade HJ, Groen AK. Regulation of cholesterol homeostasis. Mol Cell Endocrinol. 2013;368:1–16. doi: 10.1016/j.mce.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 9.Abumrad NA, Davidson NO. Role of the gut in lipid homeostasis. Physiological Reviews. 2012;92:1061–1085. doi: 10.1152/physrev.00019.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grande F, Anderson J, Chlouverakis C, Proja M, Keys A. Effect of dietary cholesterol on man's serum lipids. Journal of Nutrition. 1965;87:52–62. doi: 10.1093/jn/87.1.52. [DOI] [PubMed] [Google Scholar]
- 11.Clarke R, Frost C, Collins R, Appleby P, Peto R. Dietary lipids and blood cholesterol: quantitative meta-analysis of metabolic ward studies. British Medical Journal. 1997;314(7074):112–117. doi: 10.1136/bmj.314.7074.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howell W, McNamara D, Tosca M, Smith B, Gaines J. Plasma lipid lipoprotein responses to dietary fat and cholesterol: a meta-analysis. American Journal of Clinical Nutrition. 1997;65:1747–1764. doi: 10.1093/ajcn/65.6.1747. [DOI] [PubMed] [Google Scholar]
- 13.Weggemans R, Zock P, Katan M. Dietary cholesterol from eggs increases the ratio of total cholesterol to high-density lipoprotein cholesterol in humans: a meta-analysis. American Journal of Clinical Nutrition. 2001;73:885–891. doi: 10.1093/ajcn/73.5.885. [DOI] [PubMed] [Google Scholar]
- 14.Food and Nutrition Board and American Heart Association. Diet and coronary heart disease. Nutrition Reviews. 1972;30(10):223–225. doi: 10.1111/j.1753-4887.1972.tb03975.x. [DOI] [PubMed] [Google Scholar]
- 15.AHA. Dietary Guidelines for Healthy American Adults. Circulation. 1986;74:1465A–1468A. [PubMed] [Google Scholar]
- 16.Expert Panel on Detection E, and Treatment of High Blood Cholesterol in Adults. Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Archives of Internal Medicine. 1988;148(1):36–69. [PubMed] [Google Scholar]
- 17.Expert Panel on Detection E, and Treatment of High Blood Cholesterol in Adults. Summary of the second report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel II) Journal of the American Medical Association. 1993;269(23):3015–3023. [PubMed] [Google Scholar]
- 18.Krauss RM, Deckelbaum RJ, Ernst N, Fisher E, Howard BV, Knopp RH, Kotchen T, Lichtenstein AH, McGill HC, Pearson TA, et al. Dietary guidelines for healthy American adults. A statement for health professionals from the Nutrition Committee, American Heart Association. Circulation. 1996;94(7):1795–1800. doi: 10.1161/01.cir.94.7.1795. [DOI] [PubMed] [Google Scholar]
- 19.Krauss RM, Eckel RH, Howard B, Appel LJ, Daniels SR, Deckelbaum RJ, Erdman JW, Jr., Kris-Etherton P, Goldberg IJ, Kotchen TA, et al. AHA Dietary Guidelines: revision 2000: A statement for healthcare professionals from the Nutrition Committee of the American Heart Association. Circulation. 2000;102(18):2284–2299. doi: 10.1161/01.cir.102.18.2284. [DOI] [PubMed] [Google Scholar]
- 20.Djousse L, Gaziano J. Egg consumption in relation to cardiovascular disease and mortality: the Physicians' Health Study. American Journal of Clinical Nutrition. 2008;87:964–969. doi: 10.1093/ajcn/87.4.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rong Y, Chen L, Zhu T, Song Y, Yu M, Shan Z, Sands A, Hu F, Liu L. Egg consumption and risk of coronary heart disease and stroke: dose response meta-analysis of prospective cohort studies. British Medical Journal. 2013;346:e8539. doi: 10.1136/bmj.e8539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shin JY, Xun P, Nakamura Y, He K. Egg consumption in relation to risk of cardiovascular disease and diabetes: a systematic review and meta-analysis. American Jounal of Clinical Nutrition. 2013;98:146–159. doi: 10.3945/ajcn.112.051318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Katan MB, Beynen AC, de Vries JH, Nobels A. Existence of consistent hypo- and hyperresponders to dietary cholesterol in man. American Journal of Epidemiology. 1986;123(2):221–234. doi: 10.1093/oxfordjournals.aje.a114231. [DOI] [PubMed] [Google Scholar]
- 24.Rudkowska I, Jones PJH. Polymorphisms in ABCG5/G8 transporters linked to hypercholesterolemia and gallstone disease. Nutrition Reviews. 2008;66:343–348. doi: 10.1111/j.1753-4887.2008.00042.x. [DOI] [PubMed] [Google Scholar]
- 25.Sources of dietary cholesterol. 2013 http://riskfactor.cancer.gov/diet/foodsources/cholesterol/table1.html.
- 26.Pearce K, Clifton P, Noakes M. Egg consumption as part of an energy-restricted high-protein diet improves blood lipid and blood glucose profiles in individuals with type 2 diabetes. British Journal of Nutrition. 2011;105:584–592. doi: 10.1017/S0007114510003983. [DOI] [PubMed] [Google Scholar]
- 27.Mutungi G, Ratliff J, Puglisi M, Torres-Gonzalez M, Vaishnav U, Leite J, Quann E, Volek J, Fernandez M. Dietary cholesterol from eggs increases plasma HDL cholesterol in overweight men consuming a carbohydrate-restricted diet. Journal of Nutrition. 2008;138:272–276. doi: 10.1093/jn/138.2.272. [DOI] [PubMed] [Google Scholar]
- 28.Harman N, Leeds A, Griffin B. Increased dietary cholesterol does not increase plasma low density lipoprotein when accompanied by an energy-restricted diet and weight loss. European Journal of Nutrition. 2008;47:287–293. doi: 10.1007/s00394-008-0730-y. [DOI] [PubMed] [Google Scholar]
- 29.Vislocky L, Pikosky M, Rubin K, Vega-Lopez S, Gaine P, Martin W, Zern T, Lofgren I, Fernandez M, Rodriguez N. Habitual consumption of eggs does not alter the beneficial effects of endurance training on plasma lipids and lipoprotein metabolism in untrained men and women. Journal of Nutritional Biochemistry. 2009;20:26–34. doi: 10.1016/j.jnutbio.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 30.Herron K, McGrane M, Waters D, Lofgren I, Clark R, Ordovas J, Fernandez M. The ABCG5 polymorphism contributes to individual responses to dietary cholesterol and carotenoids in eggs. Journal of Nutrition. 2006;136:1161–1165. doi: 10.1093/jn/136.5.1161. This article assessed the effect of a relatively large cholesterol challenge, 3 eggs per day, on the basis of ABCG5 polymorphisms.
- 31.Chakrabarty G, Bijlani R, Mahapatra S, Mehta N, Lakshmy R, Vashisht S, Manchanda S. The effect of ingestion of egg on serum lipid profile in healthy young free-living subjects. Indian Journal of Physiology and Pharmacology. 2004;46:492–498. This article assessed the effect of a modest cholesterol challenge, 1 egg per day, within the context of hyper and hypo-responder adults.
- 32.Knopp R, Retzlaff B, Fish B, Walden C, Wallick S, Anderson M, Aikawa K, Kahn S. Effects of insulin resistance and obesity on lipoproteins and sensitivity to egg feeding. Arteriosclerosis Thrombosis & Vascular Biology. 2003;23:1437–1443. doi: 10.1161/01.ATV.0000082461.77557.C7. [DOI] [PubMed] [Google Scholar]
- 33.Isherwood C, Wong C, Jones W, Davies I, Griffin B. Lack of effect of cold water prawns on plasma cholesterol and lipoproteins in normo-lipidaemic men. Cellular and Molecular Biology. 2010;56:52–58. [PubMed] [Google Scholar]
- 34.Njike V, Faridi Z, Dutta S, Gonzalez-Simon AL, Katz DL. Daily egg consumption in hyperlipidemic adults-effects on endothelial function and cardiovascular risk. Nutrition Journal. 2010;9:28. doi: 10.1186/1475-2891-9-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Greene C, Zern T, Wood R, Shrestha S, Aggarwal D, Sharman M, Volek J, Fernandez M. Maintenance of the LDL cholesterol: HDL cholesterol ratio in an elderly population given a dietary cholesterol challenge. Journal of Nutrition. 2005;135:2793–2798. doi: 10.1093/jn/135.12.2793. [DOI] [PubMed] [Google Scholar]
- 36.Katz D, Evans M, Nawaz H, Yanchou Njike V, Chan W, Comerford B, Hoxley M. Egg consumption and endothelial function: a randomized controlled crossover trial. International Journal of Cardiology. 2005;99:65–70. doi: 10.1016/j.ijcard.2003.11.028. [DOI] [PubMed] [Google Scholar]
- 37.Ballaesteros M, Cabrera R, del Socorro Saucedo M, Luz Fernandez M. Dietary cholesterol does not increase biomarkers for chronic disease in a pediatric population from northern Mexico. American Journal of Clinical Nutrition. 2004;80:855–861. doi: 10.1093/ajcn/80.4.855. This article assessed the effect of a moderate cholesterol challenge, 2 eggs per day, within the context of hyper and hypo-responder children.