Abstract
In a previous paper, we presented initial findings from a study on the feasibility and challenges of implementing teleretinal screening for diabetic retinopathy in an urban safety net setting facing eyecare specialist shortages. This paper presents some final results from that study, which involved six South Los Angeles safety net clinics. A total of 2,732 unique patients were screened for diabetic retinopathy by three ophthalmologist readers, with 1035 receiving a recommendation for referral to specialty care. Referrals included 48 for proliferative diabetic retinopathy, 115 for severe non-proliferative diabetic retinopathy (NPDR), 247 for moderate NPDR, 246 for mild NPDR, 97 for clinically significant macular edema, and 282 for a non-diabetic condition, such as glaucoma. Image quality was also assessed, with ophthalmologist readers grading 4% to 13% of retinal images taken at the different clinics as being inadequate for any diagnostic interpretation.
Introduction
Diabetic retinopathy is damage to the blood vessels of the retina stemming from diabetes, and it is the leading cause of blindness among US adults between the ages of 20 and 74 years.1, 2 Individuals with diabetes would benefit from timely retinal screening examinations, which help to reduce the incidence of blindness because early detection means that effective treatments such as laser photocoagulation surgery can be provided.3, 4
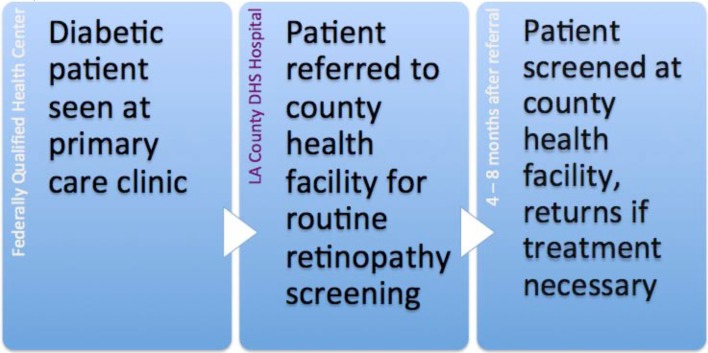
The United States medical safety net includes Federally Qualified Health Centers (FQHCs), State and County Hospitals that provide primary health care services to over 16 million patients nationally, and to roughly 2 million patients in the state of California, regardless of the patients’ ability to pay.5 Although primary care safety net clinics in South Los Angeles offer monitoring and other services for diabetic patients, they usually are not able to provide specialty care services such as retinal screening examinations. Access to specialists who can provide retinal exams can be increased through the use of telemedicine, which has shown great promise as a means of screening for diabetic retinopathy both in the US and internationally.6–13 Figure 1 shows the screening process for diabetic retinopathy for many FQHCs in South Los Angeles in the absence of teleretinal screening, with wait times of frequently more than 6 to 9 months, given the large volume of referrals to County health facilities.
Figure 1.
Screening process for diabetic retinopathy in the absence of telemedicine for some South Los Angeles safety net clinics
A number of studies have demonstrated the benefits of incorporating teleretinal screening for diabetic retinopathy into clinical practice. One such study details implementation in a rural primary care clinic of a randomized trial of point-of-service screening for diabetic retinopathy using nonmydriatic digital cameras and transmission of digital images for review by local ophthalmologists. That study produced a six-fold increase in the rate of retinal examination when compared to the usual referral protocol.14 Although many studies of teleretinal screening focus on its benefits for rural areas or developing countries, where eye care providers are few and patient access to providers is often limited by geographic distance, several studies have demonstrated that inner-city patients with diabetes also have limited access to appropriate eye care and that this is tied to delayed diagnosis and treatment of diabetic retinopathy.15–17 On average, only 60% of diabetic patients in the US receive timely eye examinations.18–22 Available data for the urban safety net setting have shown that annual eye examination rates for inner-city diabetic patients may be lower than 25%.17, 23, 24
In previous work, we presented initial findings from our study on the feasibility and challenges of implementing teleretinal screening for diabetic retinopathy in an urban safety net setting facing eyecare specialist shortages.25–27 For that study, images were uploaded into the EyePACS image viewing system8, 28 developed at UC Berkeley and subsequently graded by Los-Angeles-based ophthalmologist readers. This paper presents final results from that study, which involved six South Los Angeles safety net clinics. Overall study goals included assessing: (a) the proportion of diabetic patients at risk for retinopathy from each primary care clinic who received a retinal screening examination in compliance with current evidence-based guidelines; (b) the proportion of diabetic patients from each primary care clinic that required ophthalmologic referral or treatment and subsequently received it; (c) the proportion and quality of readable images; and, (d) the acceptability of using teleretinal screening to evaluate diabetic retinopathy in inner-city clinics through a qualitative analysis of clinic staff views of its utility, workflow impact, and ease of use, as well as safety net patient perceptions of telemedicine post clinic-visit. While this paper emphasizes final results for the first three study goals, some observations from focus group studies are also presented.
Methods
Agreements between Study Partners
Institutional Review Board (IRB) approval for the study was obtained from Charles Drew University of Medicine and Science. Memoranda of understanding (MOUs) were signed by CDU, the CEOs of all participating clinics, and the director of the clinics’ healthcare collaborative outlining the scope of the study and responsibilities of each party. An additional MOU between CDU and EyePACS was also signed. The CDU Center for Biomedical Informatics agreed to:
provide three board-certified ophthalmologists to review retinal images taken at the clinic sites regardless of the health coverage status of patients,
have the ophthalmologists perform retinal image readings and provide their assessments of patient images to the clinics within 14 days of retinal image upload, and,
provide two new nonmydriatic digital retinal cameras and staff training on the use of the cameras to clinics that had no prior experience with teleretinal screening (two out of the six clinics) and technical support for all the clinics as needed.
The six clinics agreed to:
identify staff to be trained on the use of digital nonmydriatic cameras,
allocate sufficient staff time for implementing the digital retinal screening project, including staff photographers to capture retinal images, and staff to manage electronic referrals to the county,
make all follow up referrals to outside agencies (e.g., county health facilities) for patients with positive findings, and,
provide access to patient medical records for chart review.
The director of the clinics’ healthcare collaborative agreed to:
serve as project liaison between the research team and the participating community health centers,
incorporate work on the study into the South Los Angeles Collaborative for Specialty Care Access work plan, specifically to address the need for intervention and treatment for patients with positive findings, and,
provide participating community health centers with technical assistance to fast-track and prioritize patients with positive findings at a county health facility.
Digital Retinal Image Capture and Evaluation Using Telemedicine
Image takers were provided training and were evaluated on use of the retinal cameras and the purpose of a screening program by EyePACS staff (per MOU with EyePACS). They were also given information on steps to follow for image taking through the EyePACS handbook.29 Photographers captured four retinal images for each eye – one external picture and three internal pictures covering: (1) the optic disc and macula, (2) the optic disc alone, and (3) the macula and retina temporal to the macula.8 They uploaded retinal images to the web-based system for ophthalmologist review.
Ophthalmologists reviewed image quality to determine adequacy for diagnosis. Images of sufficient quality were examined for the presence of mild, moderate, or severe non-proliferative diabetic retinopathy, proliferative diabetic retinopathy, clinically significant macular edema, and other clinically significant conditions that would warrant referral for specialty care.30 The ophthalmologists’ reviews of image quality enabled us to make decisions about retaking retinal images, retraining image takers, evaluating camera equipment, etc.
Results
Two ophthalmologists began screening retinal images for the study on September 8, 2010 and a third began screening retinal images on December 14, 2010.
Between September 8, 2010 and September 25, 2011, a total of 2,876 teleretinal screenings were performed, with 2,732 unique diabetic patients successfully screened for diabetic retinopathy. The ophthalmologists reading images recommended that 1,035 of these patients be referred for specialty care, which was about 38% of the patients screened. Of the patients referred, 48 (1.8%) had proliferative diabetic retinopathy (PDR), 115 (4.2%) had severe non-proliferative diabetic retinopathy (NPDR), 247 (9%) had moderate NPDR, 246 (9%) had mild NPDR, and 97 (3.5%) had only clinically significant macular edema. Table 1 lists the number of diabetic patients identified as having conditions requiring referral for specialty care, including clinically significant macular edema. Additional conditions recommended for referral included cataract, glaucoma, non-diabetic maculopathy, and vascular occlusion. Roughly 144 patients had repeat screenings for various reasons, including poor image quality in their first set of retinal images. This accounts for the difference between the total number of screenings (2,876) and the total number of unique patients screened (2,732).
Table 1:
Number of recommended referrals to specialists from teleretinal screening for diabetic retinopathy at six South Los Angeles clinics
| Total number of diabetic patients at 6 clinics | 9432 | |
|---|---|---|
| Total number of retinal image screenings 9/2010 – 9/2011 | 2876 | |
| Total number of unique patients screened 9/2010 – 9/2011 | 2732 | 100% |
| Percentage of diabetic patients screened across 6 clinics | 29% | |
| Total number of patients recommended for referral to a specialist | 1035 | 37.9% |
| Patients with proliferative diabetic retinopathy (PDR) | 48 | 1.8% |
| Patients with severe NPDR | 115 | 4.2% |
| Patients with moderate NPDR | 247 | 9% |
| Patients with mild NPDR | 246 | 9% |
| Patients with clinically significant macular edema only | 97 | 3.6% |
| Patients with other conditions recommended for referral | 282 | 10.3% |
Table 2 outlines the ophthalmologists’ ratings of image quality across the six clinics. The category of “insufficient for full interpretation” applied to images that had interpretable elements but were deficient in a way that made overall categorization difficult. For example, this would apply in a case where severe disease in need of referral could be clearly ruled out, but image quality was not high enough to discount subtle changes (i.e., a few scattered microaneurysms), or in a case in which image quality of one eye was adequate or better (and therefore sufficient for interpretation) while that of the other eye was not.
Table 2:
Retinal image quality ratings by clinic
| Image Quality | Clinic A | Clinic B | Clinic C/F* | Clinic D | Clinic E |
|---|---|---|---|---|---|
| Insufficient for any Interpretation | 8% | 4% | 5% | 13% | 11% |
| Insufficient for full Interpretation | 20% | 11% | 25% | 36% | 21% |
| Adequate | 39% | 49% | 36% | 35% | 30% |
| Good | 14% | 17% | 14% | 6% | 20% |
| Excellent | 9% | 12% | 7% | 1% | 7% |
| Not rated | 10% | 7% | 13% | 9% | 11% |
Clinics C & F share a camera
Discussion
We expected that by the 12-month mark, the annual screening rate achieved by our study would exceed the typical rate observed for inner-city safety net clinics. While the study achieved a screening rate of 29%, which is above the average screening rate for inner-city clinics of below 25%, it still lags behind the 60% national screening rate. We discovered a number of factors that negatively influenced screening rates in the course of our study:
Lack of integration of image-taking for teleretinal screening into primary care visit. Varying types of workflow, reduced staffing levels and other resource challenges meant that none of the six clinics involved in the study had the resources to fully integrate image-taking for teleretinal screening into a diabetic patient’s primary care visit, even though EyePACS protocol recommended this. In the one clinic with the best resources, medical assistants were available to take pictures for several hours each day (e.g., from noon to three). While this made it possible for some diabetic patients to have retinal images taken every day, it also meant that patients arriving outside those hours on a given day would have to return for image-taking on a different day. For the other five clinics, image-taking was provided two or three times a week. This had a dual negative impact on screening: there were fewer opportunities for patients to get screened in a given week, and, photographers taking pictures only two or three days a week had to continually refresh their skills in ways that photographers taking pictures every day did not.
Patients did not always understand the reasoning for their teleretinal screening visit. Some results from focus group sessions with patients who participated in teleretinal screening showed that many mistook the purpose of the screening as being for assessment of visual acuity, even though photographers were meant to explain the importance of screening for diabetic retinopathy. Patients who were not experiencing any eye problems may have simply decided that there was no need for an assessment. This highlights the important role that patient education plays in this intervention.
Image quality problems. When ophthalmologist readers graded images as being “insufficient for any interpretation,” per Table 2 above, this often meant that patients had to return for image taking, impacting the ability to screen new patients. Some of the locations available within the clinics for teleretinal screening were not optimal to routinely achieve the best images, e.g., a closet with no door and thus a reduced ability to control the amount of light that would be most favorable for image taking. To address problems stemming from human error, photographers were provided with refresher courses and direct suggestions for improvement from ophthalmologists on the project. While in general, we observed that image quality improved over time, with ratings across clinics of images “inadequate for any interpretation” falling from between 4% and 19% as in our first published report to between 4% and 13% by the end of the study, at least one photographer was unable to satisfactorily improve image quality. To address such continual image quality problems, one of the board certified ophthalmologists on the project (LPD) developed an image quality rating cut-off of 15% or fewer images rated ungradable. This cut-off was based on comparison data from other health systems that have successful teleretinal screening programs and deemed suitable for safety net clinic photographers. The cut-off was intended to indicate a level at which the optimization of the benefit of this intervention begins to wane, given the need for staff resource allocation to repeat image taking and use of limited patient resources (transportation, time off work, etc.) to return for imaging appointments. It was presented to the clinics for future use in determining those photographers who were unable to successfully achieve an appropriate quality rating and should be rotated off image-taking duties.
Diversion of staff involved in teleretinal screening to other duties. Although Medical Directors and other staff not directly involved with teleretinal screening were briefed on the importance of teleretinal screening for diabetic retinopathy and the study’s screening goals, sometimes staffing shortages/disruptions meant that Medical Assistants involved in teleretinal screening were asked to assist with other duties during times that they could have been taking images.
We also discovered that the following factors positively influenced screening rates in the course of our study:
Proactive Clinic Personnel. Medical Assistants involved in photography facilitated the teleretinal screening process when they took the time to: a) explain to patients what diabetic retinopathy is and the value of screening, b) follow up with patients, and, c) track patient referrals made to county clinics for further action.
Clinic environment that rewards photographer creativity in troubleshooting. Photographers performed better in clinics that allowed them to take ownership of their role in this intervention – for example, a photographer at one of the clinics came up with an innovative labeling system for tracking retinal images that was adopted at his clinic and later presented to other clinic photographers for adoption.
Acknowledgment of importance of screening by clinic staff not involved in study. Support from high-level administration and leadership within the clinics was instrumental in the most successful clinic implementations. Presence of this factor increased the likelihood of both 1) and 2) above.
Provision of incentives for photographers to improve upon/maintain their skills. Although clinics could not provide monetary incentives for photographers to improve upon their skills, the use of recognition programs and announcement of image quality ratings for individual photographers provided many with incentives to achieve ratings of “Good” or “Excellent.”
Post study, the six clinics involved in our study have continued their teleretinal screening programs, mostly utilizing optometrists in place of board-certified ophthalmologists on cost grounds and on the basis of convenience and previously established relationships. Within the Los Angeles County Department of Health Services, a new referral process using the eConsult system has been rolled out to upwards of 50 safety net clinics. At this time, 440 primary care providers are using eConsult at 68 sites throughout LA County, and rollout at 65 additional sites is planned over the next 5 months. Ophthalmology was one of the 6 initial pilot specialties in the system, allowing for a much more rapid turnaround time for appointments than previously existed with the previous Referral Processing System (RPS). In addition, the FQHCs continue to employ a patient navigator located in the County health facility to help their patients navigate the diabetic retinopathy treatment process.
Future work includes the development of software that uses novel image processing techniques to help improve the triage process for patients with suspected diabetic retinopathy by automatically flagging cases for reader attention.
Acknowledgments
The authors would like to thank Erin Moran for collecting data for the study. This project was supported by the NIH under grant number U54 MD007598-01S2 (formerly U54 RR026138-01S2). Drs. Ogunyemi and George also received support from grant number S21 MD000103.
References
- 1.Klein R, Klein BE. Diabetes in America. 2nd ed. National Diabetes Data Group, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 1995. Vision Disorders in Diabetes. [Google Scholar]
- 2.Zhang X, Saaddine JB, Chou CF, Cotch MF, Cheng YJ, Geiss LS, et al. Prevalence of diabetic retinopathy in the United States, 2005–2008. JAMA. 2010 Aug 11;304(6):649–56. doi: 10.1001/jama.2010.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings, DRS Report Number 8. The Diabetic Retinopathy Study Research Group. Ophthalmology. 1981 Jul;88(7):583–600. [PubMed] [Google Scholar]
- 4.Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Early Treatment Diabetic Retinopathy Study research group. Arch Ophthalmol. 1985 Dec;103(12):1796–806. [PubMed] [Google Scholar]
- 5.Takach M, Osius E. Federally Qualified Health Centers and State Health Policy: A Primer for California. California Healthcare Foundation; 2009. [Google Scholar]
- 6.Chabouis A, Berdugo M, Meas T, Erginay A, Laloi-Michelin M, Jouis V, et al. Benefits of Ophdiat, a telemedical network to screen for diabetic retinopathy: a retrospective study in five reference hospital centres. Diabetes Metab. 2009 Jun;35(3):228–32. doi: 10.1016/j.diabet.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Conlin PR, Fisch BM, Cavallerano AA, Cavallerano JD, Bursell SE, Aiello LM. Nonmydriatic teleretinal imaging improves adherence to annual eye examinations in patients with diabetes. J Rehabil Res Dev. 2006 Sep-Oct;43(6):733–40. doi: 10.1682/jrrd.2005.07.0117. [DOI] [PubMed] [Google Scholar]
- 8.Cuadros J, Bresnick G. EyePACS: an adaptable telemedicine system for diabetic retinopathy screening. J Diabetes Sci Technol. 2009;3(3):509–16. doi: 10.1177/193229680900300315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peters AL, Davidson MB, Ziel FH. Cost-effective screening for diabetic retinopathy using a nonmydriatic retinal camera in a prepaid health-care setting. Diabetes Care. 1993 Aug;16(8):1193–5. doi: 10.2337/diacare.16.8.1193. [DOI] [PubMed] [Google Scholar]
- 10.Romero-Aroca P, Sagarra-Alamo R, Basora-Gallisa J, Basora-Gallisa T, Baget-Bernaldiz M, Bautista-Perez A. Prospective comparison of two methods of screening for diabetic retinopathy by nonmydriatic fundus camera. Clin Ophthalmol. 2010;4:1481–8. doi: 10.2147/OPTH.S14521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wei JC, Valentino DJ, Bell DS, Baker RS. A Web-based telemedicine system for diabetic retinopathy screening using digital fundus photography. Telemed J E Health. 2006 Feb;12(1):50–7. doi: 10.1089/tmj.2006.12.50. [DOI] [PubMed] [Google Scholar]
- 12.Wilson C, Horton M, Cavallerano J, Aiello LM. Addition of primary care-based retinal imaging technology to an existing eye care professional referral program increased the rate of surveillance and treatment of diabetic retinopathy. Diabetes Care. 2005 Feb;28(2):318–22. doi: 10.2337/diacare.28.2.318. [DOI] [PubMed] [Google Scholar]
- 13.Yogesan K, Kumar S, Goldschmidt L, Cuadros J. Teleophthalmology. Berlin: Springer; 2006. [Google Scholar]
- 14.Davis RM, Fowler S, Bellis K, Pockl J, Al Pakalnis V, Woldorf A. Telemedicine improves eye examination rates in individuals with diabetes: a model for eye-care delivery in underserved communities. Diabetes Care. 2003 Aug;26(8):2476. doi: 10.2337/diacare.26.8.2476. [DOI] [PubMed] [Google Scholar]
- 15.Appiah AP, Ganthier R, Jr, Watkins N. Delayed diagnosis of diabetic retinopathy in black and Hispanic patients with diabetes mellitus. Ann Ophthalmol. 1991 Apr;23(4):156–8. [PubMed] [Google Scholar]
- 16.Baker RS, Watkins NL, Wilson MR, Bazargan M, Flowers CW., Jr Demographic and clinical characteristics of patients with diabetes presenting to an urban public hospital ophthalmology clinic. Ophthalmology. 1998 Aug;105(8):1373–9. doi: 10.1016/S0161-6420(98)98015-0. [DOI] [PubMed] [Google Scholar]
- 17.Wylie-Rosett J, Basch C, Walker EA, Zybert P, Shamoon H, Engel S, et al. Ophthalmic referral rates for patients with diabetes in primary-care clinics located in disadvantaged urban communities. J Diabetes Complications. 1995 Jan-Mar;9(1):49–54. doi: 10.1016/1056-8727(94)00005-9. [DOI] [PubMed] [Google Scholar]
- 18.Brechner RJ, Cowie CC, Howie LJ, Herman WH, Will JC, Harris MI. Ophthalmic examination among adults with diagnosed diabetes mellitus. JAMA. 1993 Oct 13;270(14):1714–8. [PubMed] [Google Scholar]
- 19.Cavallerano AA, Conlin PR. Teleretinal imaging to screen for diabetic retinopathy in the Veterans Health Administration. J Diabetes Sci Technol. 2008 Jan;2(1):33–9. doi: 10.1177/193229680800200106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moss SE, Klein R, Klein BE. Factors associated with having eye examinations in persons with diabetes. Arch Fam Med. 1995 Jun;4(6):529–34. doi: 10.1001/archfami.4.6.529. [DOI] [PubMed] [Google Scholar]
- 21.Orr P, Barron Y, Schein OD, Rubin GS, West SK. Eye care utilization by older Americans: the SEE Project. Salisbury Eye Evaluation. Ophthalmology. 1999 May;106(5):904–9. doi: 10.1016/s0161-6420(99)00508-4. [DOI] [PubMed] [Google Scholar]
- 22.Schoenfeld ER, Greene JM, Wu SY, Leske MC. Patterns of adherence to diabetes vision care guidelines: baseline findings from the Diabetic Retinopathy Awareness Program. Ophthalmology. 2001 Mar;108(3):563–71. doi: 10.1016/s0161-6420(00)00600-x. [DOI] [PubMed] [Google Scholar]
- 23.Deeb LC, Pettijohn FP, Shirah JK, Freeman G. Interventions among primary-care practitioners to improve care for preventable complications of diabetes. Diabetes Care. 1988 Mar;11(3):275–80. doi: 10.2337/diacare.11.3.275. [DOI] [PubMed] [Google Scholar]
- 24.Payne TH, Gabella BA, Michael SL, Young WF, Pickard J, Hofeldt FD, et al. Preventive care in diabetes mellitus. Current practice in urban health-care system. Diabetes Care. 1989 Nov-Dec;12(10):745–7. doi: 10.2337/diacare.12.10.745. [DOI] [PubMed] [Google Scholar]
- 25.Fish A, George S, Terrien E, Eccles A, Baker R, Ogunyemi O. Workflow concerns and workarounds of readers in an urban safety net teleretinal screening study. AMIA Annu Symp Proc; 2011; 2011. pp. 417–26. [Research Support, N.I.H., Extramural] [PMC free article] [PubMed] [Google Scholar]
- 26.Ogunyemi O, Moran E, Patty L, George S, Teklehaimanot S, Ilapakurthi R, et al. Autonomy Versus Automation: Perceptions of Nonmydriatic Camera Choice for Teleretinal Screening in an Urban Safety Net Clinic. Telemed J E Health. 2013 doi: 10.1089/tmj.2012.0191. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ogunyemi O, Terrien E, Eccles A, Patty L, George S, Fish A, et al. Teleretinal screening for diabetic retinopathy in six Los Angeles urban safety-net clinics: initial findings. AMIA Annu Symp Proc; 2011; 2011. pp. 1027–35. [Research Support, N.I.H., Extramural] [PMC free article] [PubMed] [Google Scholar]
- 28.The EyePACS Handbook. 2009. [updated 2009; Accessed June 6, 2012]; Available from: http://eyepacs.com/documents/EyePACS_Handbook_FINAL_3_9_09.pdf.
- 29.The EyePACS Handbook. 2009. [updated 2009; Accessed March 2, 2011]; Available from: https://http://www.eyepacs.org/RelatedResources/EyePACS_Handbook_FINAL_3_9_09.pdf.
- 30.Grading diabetic retinopathy from stereoscopic color fundus photographs--an extension of the modified Airlie House classification. ETDRS report number 10. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991 May;98(5 Suppl):786–806. [PubMed] [Google Scholar]