Abstract
Research has shown that “place matters” in health and illness. Climate, pollution and crime are examples of geographically specific social and environmental factors that can substantially impact health. However, health care decision-making and practice do not currently include spatial data on specific patients. Opportunities to incorporate clinically relevant data from the environment into health care practice are numerous, and the implementation issues are virtually unexplored. We use a qualitative study from a natural disaster, the Middle Tennessee Flood of 2010, to examine the possibilities presented by community-sourced spatial data. In our case, linking EHR data with data from rasterized photos of inundated areas could have enabled providers to identify at-risk populations of patients after the flood and conduct supportive outreach for patients with chronic illness. We explore the potential benefits for patients, policy issues and implications for biomedical informatics of expanding the health record to incorporate or link to community-sourced data.
Introduction
Epidemiologists have long recognized the importance of physical location in public health [1–6]. Neighborhood characteristics such as safety, pollution, and availability of fresh foods can have substantial impacts on the health of individuals. The advent of sophisticated geographic information systems (GIS) has made research into this area much easier, enabling scientists to generate data about the surrounding area of a patient’s residence.
The electronic health record (EHR) contains the patient address, which can be rapidly geocoded to produce computational data elements that, when linked to referential data such as crime rates, climate information, pollution/air quality and neighborhood walkability scores, can produce actionable alerts, reminders and other events for clinical decision support, care coordination and outreach.
A possibility for future application of these combined technologies exists in disaster support and recovery for individuals with chronic illnesses such as diabetes, hypertension, and cardiac conditions. This sort of support can be realized through the integration of GIS with the EHR. Such an integration could yield information about patients that may have experienced disruption from a natural disaster, and provide a basis for outreach and support for affected individuals.
Background
Spatial Data in Health Research
In 1854, a London physician by the name of John Snow identified the source of a cholera outbreak by plotting cases of the disease on geographic maps, along with the location of water pumps.[7] His finding led to a new understanding of water as the mode of transmission of the deadly disease during a time when many thought cholera was airborne. Snow convinced public officials to remove the pump handle, an action that is credited with ending the outbreak. Many consider his mapping of the Broad Street pump, an elementary form of Geographic Information System (GIS), to be the starting point for medical geography. The environment is one of the three elements, along with agent and host, of the Epidemiologic Triad, a model of disease causation. To halt the spread of the disease epidemiologists work to understand and disrupt or repair one of these three elements. Researchers have argued that this approach can be applied to other diseases and chronic illnesses, such as diabetes.[8] Traditional medical care has focused on the agent (the disease) and the host (e.g. the individual), but has lacked information about the environment at a patient-specific level. New information infrastructures such as mobile computing and community-sourced public data present opportunities for biomedical informatics to usher in a new era of socially and environmentally personalized health care.
A GIS “integrates hardware, software, and data for capturing, managing, analyzing, and displaying all forms of geographically referenced information.” [9] This spatial information is stored in a data layer, which can be overlaid onto an existing map. Each layer contains information that has been geocoded to a specific geographical location. These layers can contain information such as census data, socioeconomic status (SES), crime data from local police departments, and climate/atmospheric data from weather stations. Examples of spatially measurable variables that can have an impact on health include air pollution levels [10], temperature, crime rate, socioeconomic status, distance to affordable or healthy food and public transportation.
A study by the CDC that examined determinants of physical activity in the United States illustrates the importance of walkable, safe communities in the promotion of increased physical activity.[11] This study revealed that members of lower income communities were more likely to report high crime rates as a barrier to physical activity. The same study also showed that, regardless of income or gender, participants reported a lack of sidewalks as a barrier to physical activity. Crime rates and availability of sidewalks are examples of factors that can be included in geographically specific “walkability scores.”[12] As this is one of the specified activities recommended for many chronically ill patients, health care providers alerted to the low walkability score in a specific patient’s neighborhood can take steps to assist the patient in identifying alternatives for getting exercise.
Researchers have begun testing GIS-enabled applications in clinical settings[13–15], providing customized maps to patients, depicting community health-related resources available near their homes. This work demonstrates the feasibility of GIS for providing “practical and present localized data on demand”[15]. We consider the value of sociospatial analysis in a way that traverses levels of health care activity, from population-based outreach to communication with specific patients.
The case of disasters
Disasters such as heat waves, tornadoes, hurricanes and floods can produce massive, geographically specific loss of life and health. The elderly and chronically ill are known to be vulnerable to morbidity and mortality due to social isolation [16–18], lack of access to routine medical care [19, 20] and physical and cognitive impairments [21]. The research on long-term effects of surviving a disaster has focused primarily on psychological impacts [22, 23]. Other long-term health effects are assumed to exist as a result of the conditions that often characterize the aftermath of a disaster, (e.g. lack of proper shelter, limited access to medical care, lack of nutrition and safe water sources, and destruction of community infrastructure) [24]. It has been suggested that disaster conditions can lead to lower adherence to medications and other therapeutic regimens of chronic disease management, resulting in increased morbidity, mortality and cost [18]. These effects may be amplified in the elderly and chronically ill who are managing very complicated medication regimens, as complexity has been associated with decreased adherence to therapy [25]. However, epidemiological data on the progression of chronic illness among disaster victims has not been widely reported, likely because of the loss of physical records in some disasters and loss to follow up.
In the United States, Hurricane Katrina demonstrated the unique vulnerability and substantial deficiencies in support for the elderly, disabled and chronically ill [26–31]. In the weeks following the storm, the holders of large health data repositories, including the Veterans Administration [32] and retail pharmacies,[33] provided access to patient information in an effort to reconnect evacuated patients with their medical records.
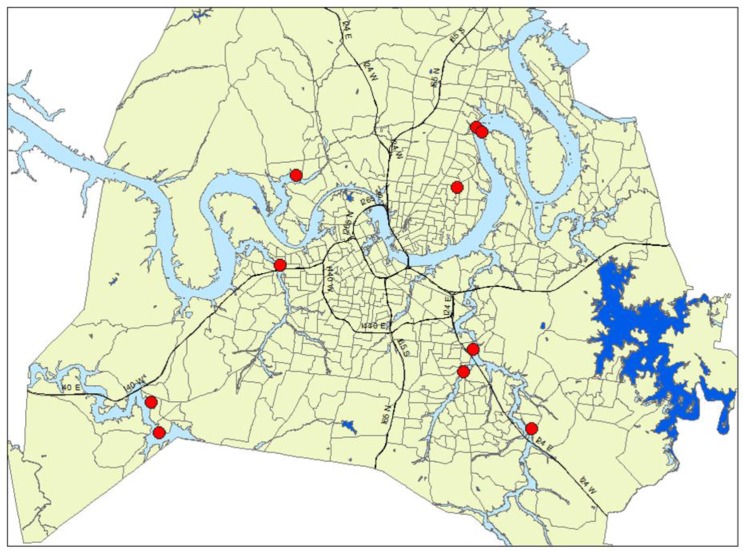
Due to the advent of GIS, analysts can now integrate aerial imagery into map layers, giving them the ability to assess the impacts of natural disasters. Aerial and satellite imagery was indispensable during the relief efforts following Hurricane Katrina and the 2005 Kashmir earthquake in Pakistan [34] Digital aerial photos can be geo-coded to produce maps. Figure 2 below depicts waterways in the Nashville, TN area at their typical levels. Figure 3 is a map generated by data from an aerial photo taken of the flood inundation in the same area in May, 2010. The widespread flood conditions can be seen by comparing the figures.
Figure 2:
Pre-flood GIS map showing the addresses of interview participants.
Figure 3:
Map from Figure 2 with an added layer depicting the inundation from the flood of May 1–2, 2010.
Here we present findings from a qualitative study of chronically ill flood survivors and discuss the opportunities for using existing technology to provide outreach to disaster victims. We explore practical and policy implications of linking external information to EHR data.
Flood event
From late April to early May of 2010, a weather event resulting in rainfall in excess of 17 inches flooded the Middle TN area. The Harpeth and Cumberland Rivers recorded record levels during this time. This devastating event claimed 11 lives and resulted in an estimated $2 billion in private property damage in Nashville alone. The storm system claimed a total of 24 lives across the state of Tennessee, displaced approximately 10,000 people and resulted in the damage of almost 11,000 properties.
Methods
Research question
Our exploratory research focused on the question: How does a major life disruption impact self-care in chronic illness? We were interested in understanding, from the participants’ perspectives, the significance of routines in successful diabetes self-care, and how those routines were disrupted by the disaster.
Participants
Recruitment efforts for this project_took place primarily through fliers, which were distributed to various community centers and social workers. The focus of these recruitment efforts were diabetics who were displaced (i.e. lost access to their homes) by the Middle Tennessee Flood of 2010. We conducted in-depth interviews with thirteen participants, ranging in age from 41–86 years of age, with six females and seven males.
Setting
Eleven of these interviews took place at the participant’s home, with one interview conducted via telephone and one conducted at our facility.
Interviews
We interviewed the participants using a semi-structured interview in the form of an illness narrative. [35] We asked the participants to describe their diabetes-related routines prior to the flood, probing for details on specific events, artifacts and people that were important to maintaining adherence to their prescribed medication and diet regimens. We maintained a neutral, non-judgmental affect and attitude during the interview, developing rapport to encourage participants to give honest, complete answers. We then asked participants to recount the flood event and their evacuation, including sources of assistance. Finally, we asked the participants to discuss their current illness management routines and the effectiveness of those routines, and how they felt the flood impacted their diabetes and general health. We also recorded field notes of other observations during the interview such as body language and the physical environment. We used interview guides in order to provide direction for the interview, as well as to provide cues for further probing on specific subjects.
Analysis
We analyzed the interview data using NVivo 9 software. We used free coding, in which all themes in the text are coded (i.e. tagged), regardless of whether they appear related to the primary research question. This analysis method yielded major domains, as well as sub-domains for further pattern analysis.
Findings
Analysis of the interviews from this project revealed consequences of the flood on the management of diabetes. Many of the participants described difficulties in maintaining established routines around blood glucose testing and taking medication, as well as the interruption of sometimes long-established routines for self-management. The following quotes illustrate some of the difficulties that participants reported:
Patients relied on routines to manage diabetes
The patients reported routines for the self-management of their condition prior to the flood. Most of these routines involved glucose testing, medication administration and physical activity. Some routines were temporally regimented, as in medication-taking, and others were oriented to places, people or artifacts. An example is the exercise routine of a 50 year old male subject:
“…last Christmas we got one of those Nintendo Wii Fit things, you know, my oldest daughter and I, when we get home, we would spend about an hour doing those together because at that time my youngest… was in preschool… and… she and [her mother] would get home about an hour after we did, so we would do that almost every day and I wound up losing probably ten pounds from doing that.”
Another example is this routine described by a 50 year old female subject:
“Well, first thing in the morning I test and then usually depending on what my blood sugars are when I wake up, but usually at 10:00 and then before lunch, then 2:00 or 3:00 and then before dinner and then before I go to bed. “
Routines were disrupted by the flood
All of the participants felt overwhelmed by the disruption and the details of relocation or renovation, negotiating the financial assistance bureaucracy, grief over the loss of precious artifacts, and helping children and others cope. Amid these challenges and distractions, they often forgot aspects of diabetes management. This quote from a 50 year old female subject, who has been a diabetic for over 30 years, provides an example:
“Thursday, I had a friend…who was a diabetes nurse, and she said, “Have you checked your sugar lately?” And I just kind of looked at her.”
This quote from the same subject described her inability to resume her routines until she was back in her home, 8 months after the event:
“…once I got back to the house … I felt was home… I [felt] like, okay, let’s get back into the groove of things.”
A 50 year old male participant described a similar experience. When asked what advice he would give to other people with diabetes going through a major disruption, he responded:
”My suggestion is just the obvious one, is that to remember that it is important to take those medicines and don't allow anything like that to, any kind of event to stop you from taking those medicines when you should. I don't know, I’m just trying to think of what I could have done differently. I just don't know because I’m such a creature of habit. When I went from hotel to hotel to my mother-in-law’s, I could not get myself set up in a routine.”
A 59 year old female participant illustrated another example of how routines centered on illnesses can take a back seat to other concerns during a catastrophic event. When asked if she thought about her diabetes or other medical conditions during the time of the flood, she responded:
“Interviewer: So, during this whole time, were you thinking about your diabetes or your other medical?
Interviewee: Not at all....
Not even room in my head for that thought.”
There were negative consequences for health
In about half of the interviews that we conducted, participants reported that the status of their illness(es) had worsened since the flood. Of those who mentioned that their illness was worse than it had been prior to the flood, most attributed this to non-adherence to medication regimens, weight gain or stress. Some of these difficulties are illustrated by the following quote from a 50 year old male who has been a diabetic for over 10 years:
“I can tell you that being displaced totally threw me way off track when it came to taking my meds. When I went to see my doctor in July, the results of my A1C test were awful. I had to double my medication and agree to 3 month testing intervals instead of the 6 months I had been doing... Since May 1 I have gained 20 pounds because I now live in an apartment. Most of my exercise came from doing yard work and now I don't have a yard.
- 50 year old male
Some participants spoke directly about the impact of stress:
“Probably – I don't know – I think sometimes it feels like it went backwards a little.… And stress can be your worst thing for diabetes, you know.”
- 52 year old male
“I would imagine, being honest, it probably took a couple of years off my life. I would imagine at least. But not as bad as it did some people. But a lot of stress there.”
- 68 year old male
Missing scheduled medication doses during a crisis can present problems for both patients and the medical providers responsible for their care. A 58 year old male participant discusses his missed medications during the flood event, highlighting the impacts for both the patient and the health care system:
“I missed about two days of Coumadin and that was a problem because it took almost two weeks to get it back regulated.“
“So, when I went back to the doctor, he said, you missed – like I said, I didn't have no choice…..
And he went, oh, okay, never mind. We'll figure out how to get it regulated.”
Discussion
An infrastructure for outreach
Our findings suggest that establishing an infrastructure for outreach to people impacted by disruptive events could be valuable to those managing chronic illness. Notably, all of the participants we interviewed evacuated their homes with their cell phones intact. Examples of such an outreach infrastructure include:
Identification of individuals and families impacted by the event
Aerial flood inundation images were rasterized, i.e. translated into polygon-based shapefiles that can be inserted as a layer into a GIS. This layer is tied geospatially to a map. Patient addresses from the affected ZIP codes can then be mapped onto the flood layer, and the GIS can produce a list of addresses in the inundated areas. In this way, the health care provider can pinpoint potentially affected patients during or after a natural disaster. This establishes a link between the environmental factor (flood inundation) and the wealth of information in the EHR, e.g. diagnoses, care plans, and contact information for the affected patient(s) via cell phone and/or e-mail.
Outreach and case finding
Health care organizations already conduct outreach via telephone for appointment reminders and community alerts. These systems provide an infrastructure for messaging or calling potentially affected patients, who can then respond if they would benefit from further assistance from the provider.
Mobile phone alerts and reminders
All of the participants who owned a cell phone were also able to evacuate with it. This suggests that there may be an opportunity for the health care system to support patients in crisis through the use of mobile technologies. Examples of services that may have been useful to the subjects in our study include reminders for glucose testing and taking medications, reminders of clinical appointments, and basic information about obtaining refills and contacting the clinic.
Practical implications
Linking community-sourced data with patient records, while potentially valuable, poses a significant informatics challenge. First, the home address data in the EHR may be incomplete or inaccurate, resulting in missed cases or people inappropriately identified as living in the affected area. Data quality, e.g. typos and transcription errors, can produce these problems as well. Many people may not own mobile phones, or have not yet provided the mobile phone number to the institution. Another confounding factor is the current format of patient addresses in the EHR. The addresses that have been provided may have changed, or may be in the incorrect format for GIS utilization (i.e. P.O. Box instead of a physical address). Finally, numerous potential problems resulting from the ecological fallacy of inferring patient-specific attributes from population-based data will need to be resolved with procedures of confirmation. Data layers that are linked for mapping or decision support purposes may have different levels of geographical scope, thereby determining the granularity of the data. For example, it may be confirmed that a person lives on a particular parcel of land, and that the parcel is within one mile of a pharmacy. However, further inference on less granular data (e.g. at the census tract level, which is a larger spatial division) would be problematic. Therefore it would be erroneous to assume that any specific patient has problems with the cost of medications based on census-derived income data.
The coordination of these data would also require specialized personnel who could understand how to link the GIS data to EHR information for the particular problem at hand, and who may not be readily available to all institutions. Additionally, the outreach effort would need to be coordinated and overseen by people with the appropriate clinical skills. For example, if victims responded to outreach messages with specific clinical questions, those issues would need to be triaged and assigned to appropriate clinical specialists. Investment in infrastructure to support such an endeavor, including the hiring of staff with the necessary skills, would be required.
Policy implications
With the advent of mobile technology and social media, the line between public health and medical care has become blurred. The role of the health care provider in disasters has traditionally been as a first responder. Technology can enable health care systems to reach out to patients to facilitate maintenance of health and illness management routines, and improve long-term health. Institutions may need information on the value of this investment in order to prioritize such interventions. This would constitute a major advancement in preventative care, allowing practitioners to be more proactive in their support of patient health during a disaster.
Giving health care providers access to environmental data associated with specific patients may prove clinically useful, but have negative impacts on the patient-provider relationship if not handled appropriately. For example, if environmental barriers are presented to patients without problem-solving assistance, patients may assume that their therapeutic goals cannot be reached. Having access to data about the environment surrounding a patient’s residence or place of employment may enable the provider to make suggestions that are better suited to the patient.
Further research is needed to determine if spatio-temporal attributes may affect the support needed by various patients. The sample size for this project was limited, so it was not possible to analyze the data with these criteria in mind. Future studies could include details regarding the distance from the affected area(s) and the time elapsed since the event, possibly revealing challenges related to natural disasters that various patients may encounter. Varying needs of the patient population based on these spatial or temporal aspects could lead to differing policy implications. For instance, a patient’s home may not be directly affected by a flood event, but they may be unable to obtain needed medications because the pharmacy that they normally use is closed or damaged.
Imperatives
New emphasis on patient-centered care and research is emerging. [36] Expanding provider and patient access to patient-specific data on the social and environmental determinants of health may prove an essential catalyst for improving patient outcomes. These values are also reflected in the aims of the Affordable Care Act,[37] and the personalized medicine paradigm [38], which to date has focused primarily on genomic personalization rather than social and environmental factors.
Conclusion
Social and environmental data are missing from the EHR. Incorporating GIS can provide sociospatial information that can enrich the EHR, and make it easier for providers to deliver personalized care. The information delivered by spatial analysis adds to the current data set about the patient (i.e. habits, living arrangements, vital signs and test results, insurance information, etc.), and can reveal information relevant to health and illness such as access to public transportation, proximity to medical providers, proximity to healthy food vendors, walkability index, socioeconomic information and climate/air quality data surrounding the patient’s residence.
Geographic information can help to identify patients and families impacted by natural disasters. This information can provide the basis for outreach to patients that may require or benefit from health services (i.e. prescription refills, doctor appointments, glucose testing, medication adherence support, etc.) during a crisis situation. Expansion of this type of outreach could have a positive impact on management of patients with chronic illnesses, possibly reducing the need for emergency interventions and/or readmissions in the long term. The advent of mobile technology, and the fact that most of the victims interviewed were able to make it to safety with their mobile phones, highlights the feasibility of an electronic support system during a time of crisis.
The ability to include various layers of information into a map makes it easier to visualize the impacts that such disasters can have on a patient population. The integration of such information into the EHR could have profound effects on the support of patients after such a disaster.
References
- 1.Schlundt DG, Hargreaves MK, McClellan L. Geographic clustering of obesity, diabetes, and hypertension in Nashville, Tennessee. The Journal of ambulatory care management. 2006;29(2):125–32. doi: 10.1097/00004479-200604000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Schlundt DG, et al. Use of innovative technologies in the evaluation of Nashville's REACH 2010 community action plan: reducing disparities in cardiovascular disease and diabetes in the African American community. The Journal of ambulatory care management. 2001;24(3):51–60. doi: 10.1097/00004479-200107000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Bedimo-Rung AL, Mowen AJ, Cohen DA. The significance of parks to physical activity and public health: a conceptual model. American journal of preventive medicine. 2005;28(2 Suppl 2):159–68. doi: 10.1016/j.amepre.2004.10.024. [DOI] [PubMed] [Google Scholar]
- 4.Koh HK, et al. Using public health data systems to understand and eliminate cancer disparities. Cancer causes & control : CCC. 2005;16(1):15–26. doi: 10.1007/s10552-004-1254-2. [DOI] [PubMed] [Google Scholar]
- 5.Lovasi GS, et al. Using built environment characteristics to predict walking for exercise. International journal of health geographics. 2008;7:10. doi: 10.1186/1476-072X-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rushton G. Public health, GIS, and spatial analytic tools. Annual review of public health. 2003;24:43–56. doi: 10.1146/annurev.publhealth.24.012902.140843. [DOI] [PubMed] [Google Scholar]
- 7.Snow J. On the mode of communication of cholera. John Churchill; 1855. [Google Scholar]
- 8.Egger G, Swinburn B, Rossner S. Dusting off the epidemiological triad: could it work with obesity? Obesity reviews : an official journal of the International Association for the Study of Obesity. 2003;4(2):115–9. doi: 10.1046/j.1467-789x.2003.00100.x. [DOI] [PubMed] [Google Scholar]
- 9.(ESRI), E.S.R.I. 2013. [cited 2013 March 13]; Available from: http://www.esri.com/what-is-gis/overview#overview_panel.
- 10.Koken PJ, et al. Temperature, air pollution, and hospitalization for cardiovascular diseases among elderly people in Denver. Environmental health perspectives. 2003;111(10):1312–7. doi: 10.1289/ehp.5957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brownson RC, et al. Environmental and policy determinants of physical activity in the United States. American journal of public health. 2001;91(12):1995–2003. doi: 10.2105/ajph.91.12.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doyle S, et al. Active Community Environments and Health: The Relationship of Walkable and Safe Communities to Individual Health. Journal of the American Planning Association. 2006;72(1):19–31. [Google Scholar]
- 13.Gravesande K. Using Geographic Information Systems (GIS) to Improve Patient-Clinician Encounters and Patient Care. 2010 [Google Scholar]
- 14.Hawkins R, et al. Extending an Electronic Medical Record Geographic Information System [Google Scholar]
- 15.Jones-Quartey K, et al. Integrating a Geographic Information System with Electronic Medical Records [Google Scholar]
- 16.Friedsam HJ. Older Persons as Disaster Casualties. Journal of Health and Human Behavior. 1960;1(4):269–273. [Google Scholar]
- 17.Ngo EB. When Disasters and Age Collide: Reviewing Vulnerability of the Elderly. Natural Hazards Review. 2001;2(2):80–89. [Google Scholar]
- 18.Li R. In: Meeting Report: Advancing Behavioral and Social Research on the Elderly in Disasters. Academies N, editor. 2009. [Google Scholar]
- 19.Spiegel P, et al. Health programmes and policies associated with decreased mortality in displaced people in postemergency phase camps: a retrospective study. The Lancet. 2002;360(9349):1927–1934. doi: 10.1016/S0140-6736(02)11915-5. [DOI] [PubMed] [Google Scholar]
- 20.Arrieta MI, et al. Insuring continuity of care for chronic disease patients after a disaster: Key preparedness elements. American Journal of the Medical Sciences. 2008;336(2):128–133. doi: 10.1097/MAJ.0b013e318180f209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dyer C, et al. Recommendations for Best Practices in the Management of Elderly Disaster Victims. Baylor College of Medicine; 2006. [Google Scholar]
- 22.Phifer JF, Norris FH. Psychological Symptoms in Older Adults Following Natural Disaster: Nature, Timing, Duration, and Course. Journal of Gerontology. 1989;44(6):S207–S212. doi: 10.1093/geronj/44.6.s207. [DOI] [PubMed] [Google Scholar]
- 23.Rubonis AV, Bickman L. Psychological impairment in the wake of disaster: The disaster–psychopathology relationship. Psychological Bulletin. 1991;109(3):384–399. doi: 10.1037/0033-2909.109.3.384. [DOI] [PubMed] [Google Scholar]
- 24.Aldrich N, Benson WF. Disaster preparedness and the chronic disease needs of vulnerable older adults. Prev Chronic Dis. 2008;5(1):A27. [PMC free article] [PubMed] [Google Scholar]
- 25.Choudhry NK, et al. The implications of therapeutic complexity on adherence to cardiovascular medications. Arch Intern Med. 2011;171(9):814–22. doi: 10.1001/archinternmed.2010.495. [DOI] [PubMed] [Google Scholar]
- 26.Aldrich N, Benson WF. Disaster preparedness and the chronic disease needs of vulnerable older adults. Preventing chronic disease. 2008;5(1):A27. [PMC free article] [PubMed] [Google Scholar]
- 27.Adams V, et al. Aging Disaster: Mortality, Vulnerability, and Long-Term Recovery among Katrina Survivors. Medical Anthropology. 2011;30(3):247–270. doi: 10.1080/01459740.2011.560777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burton CG. Social Vulnerability and Hurricane Impact Modeling. Natural Hazards Review. 2010;11(2):58–68. [Google Scholar]
- 29.Cloyd E, Dyer CB. Catastrophic events and older adults. Crit Care Nurs Clin North Am. 2010;22(4):501–13. doi: 10.1016/j.ccell.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 30.Dobalian A, Claver M, Fickel JJ. Hurricanes Katrina and Rita and the Department of Veterans Affairs: a conceptual model for understanding the evacuation of nursing homes. Gerontology. 2010;56(6):581–8. doi: 10.1159/000302713. [DOI] [PubMed] [Google Scholar]
- 31.Evans J. Mapping the vulnerability of older persons to disasters. Int J Older People Nurs. 2010;5(1):63–70. doi: 10.1111/j.1748-3743.2009.00205.x. [DOI] [PubMed] [Google Scholar]
- 32.Brown SH, et al. Use of electronic health records in disaster response: the experience of Department of Veterans Affairs after Hurricane Katrina. American journal of public health. 2007;97(Supplement_1):136–141. doi: 10.2105/AJPH.2006.104943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Franco C, et al. Systemic collapse: medical care in the aftermath of Hurricane Katrina. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science. 2006;4(2):135–146. doi: 10.1089/bsp.2006.4.135. [DOI] [PubMed] [Google Scholar]
- 34.Nourbakhsh I, et al. Mapping disaster zones. Nature. 2006;439(7078):787–788. doi: 10.1038/439787a. [DOI] [PubMed] [Google Scholar]
- 35.Kleinman A. The Illness Narratives: Suffering, Healing and the Human Condition. USA: Basic Books; 1988. [DOI] [PubMed] [Google Scholar]
- 36.Selby JV, Beal AC, Frank L. The Patient-Centered Outcomes Research Institute (PCORI) national priorities for research and initial research agenda. JAMA: The Journal of the American Medical Association. 2012;307(15):1583–1584. doi: 10.1001/jama.2012.500. [DOI] [PubMed] [Google Scholar]
- 37.Huntington WV, et al. Patient Protection and Affordable Care Act of 2010: Reforming the health care reform for the new decade. Pain Physician. 2011;14:E35–E67. [PubMed] [Google Scholar]
- 38.Ginsburg GS, McCarthy JJ. Personalized medicine: revolutionizing drug discovery and patient care. TRENDS in Biotechnology. 2001;19(12):491–496. doi: 10.1016/s0167-7799(01)01814-5. [DOI] [PubMed] [Google Scholar]