Abstract
Pre-hospital communication is a critical first step towards ensuring efficient management of critically injured patients during trauma resuscitation. Information about incoming patients received from the field and en route serves a critical role in helping emergency medical teams prepare for patient care. Despite many efforts, inefficiencies persist. In this paper, we examine the pre-hospital communications between pre-hospital and hospital providers, including the types of information transferred during en-route calls, as well as the information needs of trauma teams. Our findings show that Emergency Medical Services (EMS) teams report a great deal of information from the field, most of which match the needs of trauma teams. We discuss design implications for a computerized system to support the use and retention of pre-hospital information during trauma resuscitation.
Introduction
Trauma resuscitation is a specialized medical domain in which critically injured patients are treated in a dedicated facility in the emergency department (resuscitation bay) [1]. During resuscitation, an interdisciplinary team of medical specialists (resuscitation team) must provide rapid and focused intervention in an organized manner to identify and manage potentially life-threatening injuries. The timely acquisition and dissemination of information from pre-hospital staff is a critical first step towards achieving this goal. Pre-hospital information is used for trauma team activation as well as for efficient planning and use of resources at the receiving trauma center [2]. Despite its important role in ensuring the continuity and safety of patient care, communication between pre-hospital staff and trauma teams remains inefficient: patients often arrive either unannounced or are described in insufficient detail to allow appropriate preparations [3,4], Emergency Medical Services (EMS) reports during patient handover often lack structure [5,6], and communication breakdowns are common [7,8]. While handoffs have been widely studied in other medical contexts, including clinical shift handovers [9,10,11,12,13,14], fewer studies have looked at information handover between care providers in the field and those in the receiving trauma centers [3,4,5,15,16].
A key factor in efficient pre-hospital information handover is the seamless information exchange between pre-hospital and hospital teams. To date, however, this mostly verbal information exchange has been supported using traditional telecommunication systems such as two-way radio or phone communications. Previous research has focused on developing information and communication technologies (ICT) to better support field data collection and information flow between the accident sites and command and control centers or receiving care centers [2,8,17,18, 19,20,21]. These solutions have been proposed for both disaster response and emergency medical situations. For example, telepresence systems such as RealityFlythrough [20] allow first responders to remotely observe accident scenes through live video feeds. Few studies, however, have examined the ways in which pre-hospital information is presented to receiving medical teams for more efficient acquisition, retention and use [7].
Our long-term goal is to design and develop an information technology system that facilitates the acquisition, retention and use of pre-hospital information during trauma resuscitation. This goal has been shaped based upon our own preliminary work as well as existing literature showing that trauma teams have difficulties in retaining information from pre-hospital calls and EMS reports upon patient arrival [5,6,7,15,16]. In this paper, we focus on pre-hospital communications occurring en route between care providers in the field and those in the trauma centers and emergency departments. More specifically, we examine the structure of pre-hospital communications as well as the information needs of trauma team members to better understand the nature of the pre-hospital communication process. We identify and categorize the types of information relayed during this process and use this insight to discuss implications for an information technology system to facilitate the use of pre-hospital information during trauma resuscitation.
While we extend our own and existing research on handover practices upon patient arrival, we also contribute new knowledge by identifying (1) the structure of en-route, pre-hospital communications; (2) the types of information being communicated; (3) pre-hospital information needs of trauma teams; and (4) system requirements for technologies to support pre-hospital data presentation during trauma resuscitation.
Background
Information exchange between EMS teams (first responders, paramedics and air-ambulance crews) and staff at the receiving trauma center (emergency communication center) occurs en route via radio or cellular link, as the EMS teams transport the patient to the hospital. The information relayed at this time usually includes the estimated time of arrival (ETA), number of incoming patients, demographics, mechanism of injury, and patient status. Upon receiving this initial report, the staff at the hospital’s emergency communication center calls the emergency department (ED), relays the reported information, and together with an emergency medicine attending decides on the trauma level activation. Patient information is then summarized into a brief notification message and sent to trauma team members using pagers and overhead announcements. As the trauma team assembles in the resuscitation bay, the emergency medicine attending relays known information about the patient. The team then uses this information to prepare for the patient arrival.
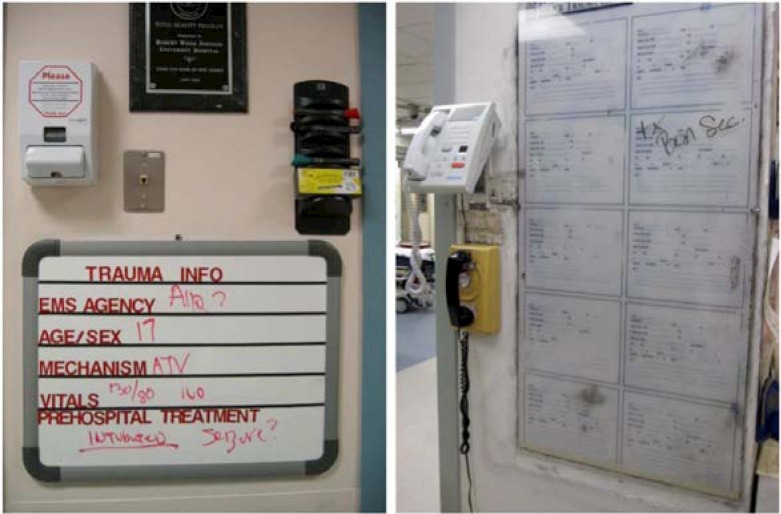
Pre-hospital communication is now mostly verbal. Pager messages are short and lack detail, but this design is intentional given their sole purpose to summon trauma team members. In some trauma centers, basic pre-hospital information is also written down on whiteboards near resuscitation areas, e.g., at the entrance to the resuscitation bay (Figure 1). This presentation, however, offers limited insight into the patient status and is often ignored. Despite these inefficiencies, we believe that coupling a status board with computerized system that interactively displays patient information to trauma teams during transport can better support teams in acquiring and retaining pre-hospital information. Studies of status boards and wall displays in medical settings have already shown their potential in supporting work that is distributed over people, time and space [22,23]. To further explore the ideas related to interactive presentation of the pre-hospital information, we must first understand the information needs of trauma team members and nature of the pre-hospital communication process.
Figure 1:
Current ways of presenting pre-hospital information to trauma teams in US Level 1 trauma centers.
Methods
Study Setting
Our research site was Children’s National Medical Center in Washington DC, an urban, pediatric teaching hospital and a regional Level I trauma center that provides the highest level of trauma expertise and 24-hour trauma care. Children’s Emergency Communication and Information Center (ECIC) is a state-of-the-art facility with a team of communication specialists, all of which are EMT-B (Emergency Medical Technician-Basic) trained. The role of the ECIC staff is to connect primary care physicians with the Children’s emergency department specialists, dispatch and monitor all ground and air teams, and act as liaison with fire, emergency medical services (EMS), and private ambulance services. The study was approved by the hospital’s Institutional Review Board (IRB).
Data Collection
Over the past four years, we have conducted several field studies using multifaceted qualitative methods such as field observations, semi-structured interviews and content analysis of pre-hospital communications. We conducted semi-structured interviews with a total of 16 trauma team members, including five emergency medicine physicians, eight senior surgical residents, one surgical fellow, one respiratory therapist and one nurse practitioner. Participants’ years of experience in these roles ranged from two to 21 years. Interviews lasted from 30 minutes to an hour, depending on providers’ availability. The interview questions focused on participants’ roles and responsibilities, and pre-hospital information needs.
We also audiotaped 68 pre-hospital communications between EMS crews and ECIC teams over a four-month period (June–September, 2009). The length of communications varied from 30 seconds to 4 minutes, and depended on the available information about the patient, number of incoming patients, and the purpose of the call (e.g., consultation vs. patient arrival notification).
Data Analysis
Data from semi-structured interviews was transcribed and analyzed by the authors using Atlas.ti, a program for organizing, storing, and manipulating qualitative data. We used an open coding technique to identify the pre-hospital information needs as well as challenges that trauma teams face in acquiring, retaining and using pre-hospital information. Audio recordings of communications between EMS an ECIC teams were transcribed by trauma resuscitation experts and then analyzed by the authors using Atlas.ti. We again used an open coding technique to uncover common information types, as well as the structure and nature of pre-hospital communications. To maintain confidentiality, we removed all information that could help identify the patient or event from the transcripts.
Results
We report our results in two parts. First, we present our analysis of pre-hospital communications between EMS crews and staff at the hospital’s emergency communication center. Here, we focus on identifying and categorizing information types, and describing the structure of the en-route reports. We then present data from interviews to describe the pre-hospital information needs of trauma team members and challenges that teams face in acquiring, retaining and using this information.
Information Types Reported during Pre-Hospital Communications
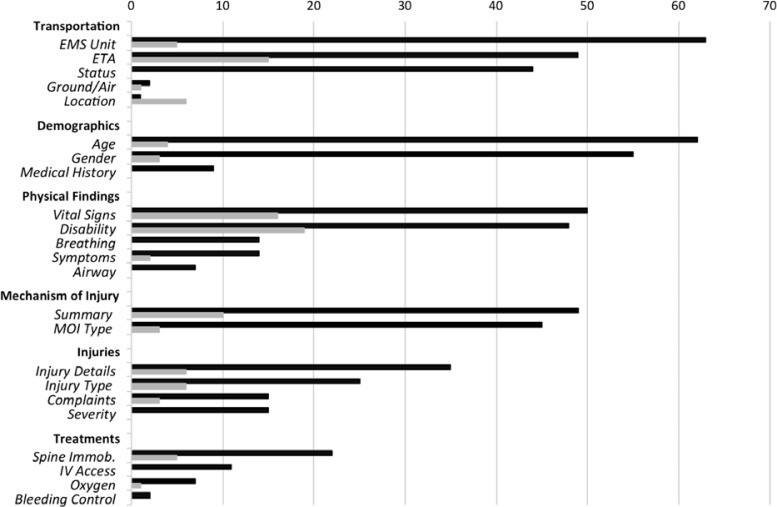
Our analysis of pre-hospital communications showed that EMS crews report a great deal of information during en route calls to the ECIC. The ECIC staff relays this information to ED physicians and trauma teams, who then use the relayed information to prepare for the patient arrival. We identified 17 information types and grouped them into six high-level categories (Figure 2). Below, we discuss each high-level category in greater detail and provide excerpts from different communications to illustrate the ways in which pre-hospital information is communicated.
Figure 2:
Information types identified in EMS-ECIC communications, grouped into six high-level categories. Dark bars indicate the number of communications in which the information was reported by EMS teams. Gray bars indicate the number of communications in which the information was requested by ECIC teams.
Transportation:
A call from the field typically starts with transportation details, including the type (e.g., air, ambulance), status (e.g., still at the scene, leaving the scene), estimated time of arrival (ETA), and sometimes even current location of EMS crews, as shown in the excerpt below:
“This is Medic [unit number], I’m consulting with you, I’m at [location] right now rendezvousing with Trooper 3 who’s going to fly my patient to your facility. Should be there, probably in the next twenty minutes. They haven’t left the ground yet though, could be a little bit.”
[Event #4]
Transportation status, which was reported in 65% of all communications, allows ECIC teams to better estimate patient arrival time. Because the patients are typically transported by ground, transportation type was reported rarely, in only two events. In contrast, ETA is one of the most important information types because it helps medical teams estimate how much time they have to prepare for patient arrival. ETA was reported in 72% of all communications (49 out of 68), and requested by ECIC teams in remaining 23%. In six events, EMS teams could not specify ETA, so ECIC staff inquired about their current location to estimate their arrival.
Demographics:
The transportation information was usually followed by patient demographics, including patient age, gender and medical history:
“Medic [unit number], we’ll be coming to you, in about twenty minutes ET. [Age] year old [gender]… [The patient] has no past medical, no meds, and no allergies.”
[Event #7]
Patient age and gender are important because trauma teams can estimate the impact of injuries and en-route treatments. Patient age was initially reported by EMS crews during 62 communications and subsequently requested by ECIC staff in four events. Similarly, gender was reported during 55 communications and requested three times in a follow-up discussion. The patient’s age was missing in only two cases and was not reported.
The patient’s medical history, including allergies and previous hospitalizations, was included in the verbal report when available. Because our study examined pre-hospital communications in a pediatric trauma center, availability of medical history depended on whether the patients were accompanied by parents or guardians. We observed medical history being reported in 13% of all communications (9 out of 68).
Physical findings:
The most common information reported in this category included vital signs, such as heart rate, blood pressure and respiratory rate (74%), and patient neurological status (71%). The information about patient neurological status, including Glasgow Coma Score (GCS), alertness and orientation (A&O), memory and consciousness, was reported in most cases:
“…[the patient] was very disoriented, uh, extremely diaphoretic, cold and clammy …the patient had a GCS of 15, airway is patent, monitoring of vital signs, blood pressure is 118/69, sats 100% with a nasal cannula.”
[Event #2]
When this information was omitted from the EMS initial report, ECIC staff requested it in a follow-up discussion, which shows the importance of this information:
EMS: “… I have [age] [gender] that fell out of a second story window, um, we believe to be about 20 feet or so. […] No obvious injuries noticed on face and feet. Um, is complaining of little bit of chest and abdomen tenderness. No bruising or anything at the moment. Lungs are clear. No obvious injuries at the moment.”
ECIC: “Medic [unit number], do you advise: patient has scratches to the face and feet, and complained of chest and abdominal tenderness? Did the patient have any LOC?”
EMS: “No, no LOC, alert and oriented times three. Remembers, um, the incident.”
[Event #59]
Mechanism of injury:
An accurate description of the mechanism of injury is critical for patient management during trauma resuscitation. Common mechanisms include falls, motor vehicle accidents, burns, and gunshot and stab wounds. EMS crews were able to explicitly state the mechanism of injury in 66% of all communications. Most communications, however, contained at least some description or summary of the mechanism, such as how the patient got injured, when or where the incident happened. If the exact mechanism was known, the description was short, as in event #27: “…uh, pedestrian struck. [The patient] was hit by a car, uh, less than 20 miles an hour.” If the exact mechanism was not known, the description was longer and somewhat speculative:
“…uh, not really sure of the mechanism but, uh, family members seem to think [the patient] was riding scooter. Not clear whether [the patient] had a helmet on or not. There was a helmet found, uh, laying on the ground. This probably happened over an hour ago, uh, according to the family.”
[Event #42]
Injuries:
The description of injuries included the severity and type of injury, such as swelling, abrasions, fractures, bruises, lacerations and deformities. If patient injuries were not observable, EMS crew reported patient complaints as an indicator of a potential internal injury:
“…[the patient] complains about head pain, left chest wall pain, [patient] has an abrasion to the left bilateral aspect of-or-upper lower quadrant of left side and some generalized abdominal discomfort.”
[Event #7]
We also found that EMS crews provided detailed reports about injuries after assessing the patient. The reports often included location and number of wounds, as well as their description:
“The patient has two wounds both, um, both approximately the same size. Not sure if they’re an entrance exit or two entrance, um, one is midpoint to the right side and by the umbilicus, and the other is midline with the nipple line a little bit over towards the sternum.”
[Event #1]
The type and description of injuries were reported more frequently than the severity of injury, being included in 37% and 51% of all communications respectively.
Pre-Hospital Treatments:
EMS teams regularly reported details about any treatments provided either at the scene or en route. The treatments involved establishing IV access, administering oxygen, and immobilizing spine (e.g., “[the patient] is fully immobilized, has an IV established” [Event #8]). IV access and spine immobilization were the two most common interventions, being reported in 16% and 32% of all communications respectively.
We observed ECIC personnel asking EMS providers if they needed any help or orders at the end of their calls. Although they were not frequent, we observed these inquiries in eight events, all of which involved high-risk and severely injured patients, with either positive loss of consciousness (LOC) or unstable vitals:
EMS: “…[the patient] was unconscious for approximately three minutes on the scene, the bystanders and the motorist said [the patient] was not breathing…”
ECIC: “Copy, medic [unit number]. Do you require orders?
EMS: “No orders at the present time. I’ll give you a chirp back up if [the patient] changes significantly. Uh, expect us in about 25 minutes or so.”
ECIC: “Copy, medic. Was the patient found in the decorticate or the cerebrate position or do you not know?”
EMS: “No, I don’t think we’ve progressed to that point. Um, I think [the patient] was just, uh, flat when they found [the patient].”
[Event #45]
The Structure of Pre-hospital Reports
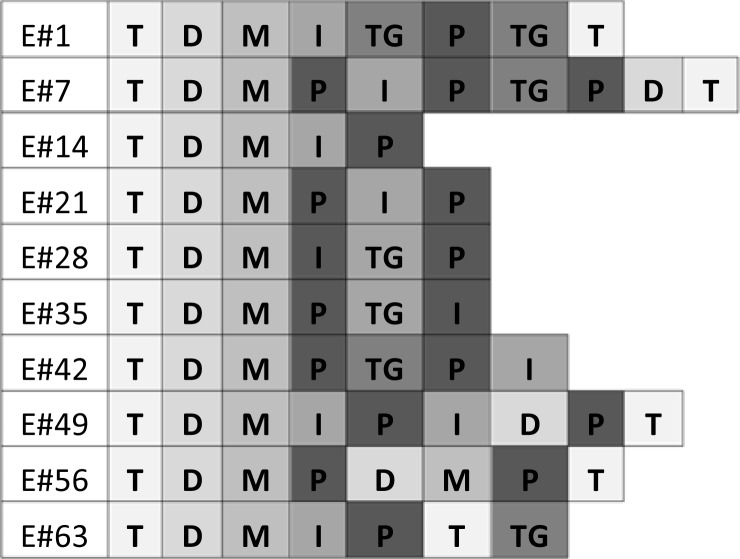
Our initial analysis of pre-hospital communications between EMS and ECIC teams showed that communications are fluid and subject to change, consisting of reports, questions, clarifications, and requests for information. The initial EMS report about the patient status was rarely complete and was typically followed by a discussion to clarify ambiguous issues and add new information. To further examine the nature of the pre-hospital communication process, we analyzed the structure of initial reports provided by EMS teams in all 68 communications. We were interested in the kinds of information that were reported first and what types of information followed. This analysis also helped us uncover patterns in field data presentation, providing the basis for our discussion of system requirements. Each initial EMS report was broken down into a series of text snippets representing different information categories. Due to the space restrictions, we only show a sample of this analysis, containing nine communications randomly selected from the dataset (Figure 3).
Figure 3:
A sample of communications (events) showing their structure. T = Transportation, D = Demographics, M = Mechanism of injury, I = Injuries, TG = Treatments given, P = Physical findings.
The analysis revealed relatively stable structure of the information types reported initially during en-route calls. We found that the information about transportation, patient demographics and mechanism were reported in the same order before any other information in 78% of all communications (53 out of 68). Subsequent information categories included injuries, physical findings and en-route treatments. Although reporting these categories did not follow any specific order, we observed that injuries and physical findings preceded any reports about en-route treatments. We also found that EMS teams used to complete their reports by repeating transportation information, i.e., their estimated time of arrival. Below is an example of a report following this relatively stable structure:
“Paramedic [unit number], hospital assist… Okay, we’re en route to your facility. [Age] [gender] struck by vehicle. Vehicle speed approximately 25 miles per hour. Damage noted to the vehicle’s hood, patient does have a positive loss of consciousness on the scene. Currently [patient] is alert and oriented times three. Complaining of pain in the back. Vitals are as follows: blood pressure 134/88, heart rate 96…02, attempt to start IVs en route. ETA with this Priority Two patient is eight minutes.”
[Event #23]
The remaining 22% of communications did not follow this overall structure. The order in which the information was reported varied and largely depended on the pre-hospital provider or on the information that was available. Some reports provided information about injuries and physical findings, but no mechanism or transportation related information. Other included only demographics, mechanism and transportation information:
“Report of a [age], fell 40 feet. Uh, [unit number] ETA is about 12 minutes and [unit number] will be there in about 25 minutes. I’ll keep you updated with ETA’s.”
[Event #40]
Upon further examination, we also observed that pre-hospital communications with the same macro-level structure differ by the types of information reported at the micro level. For example, events #14 and #59 share the same macro-level structure: Transportation > Demographics > Mechanism of injury > Injuries > Physical findings (Figure 4). However, after zooming in to specific information categories, we found that the content within each differed between the two reports. For example, in event #14, report about injuries (I) included the type of injury as well as injury details, whereas in event #59, injury type was replaced by patient complaints (Figure 4). Similarly, event #14 included detailed information about physical findings (symptoms, vital signs and neurological status), whereas event #59 included airway status only. Two explanations can account for these differences. First, the level of detail was relative to the amount of observable and available information. EMS providers in event #14 were able to identify specific injuries. In contrast, providers in event #59 could not identify specific injuries so they reported patient complaints, information that could still provide enough indications about potential injuries. Second, the level of detail was related to the severity of patient injuries. The more severe the injuries, the more detail the report had.
Figure 4:
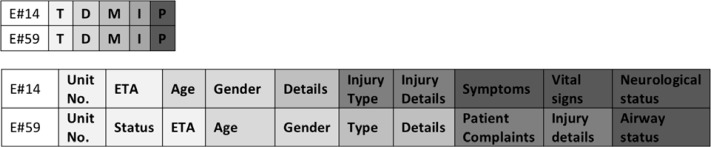
Macro-level vs. micro-level structure of pre-hospital communications. Top rows show the macro-level structure for two events. Bottom rows show the micro-level structure for the same two events.
Pre-Hospital Information Needs of Trauma Teams
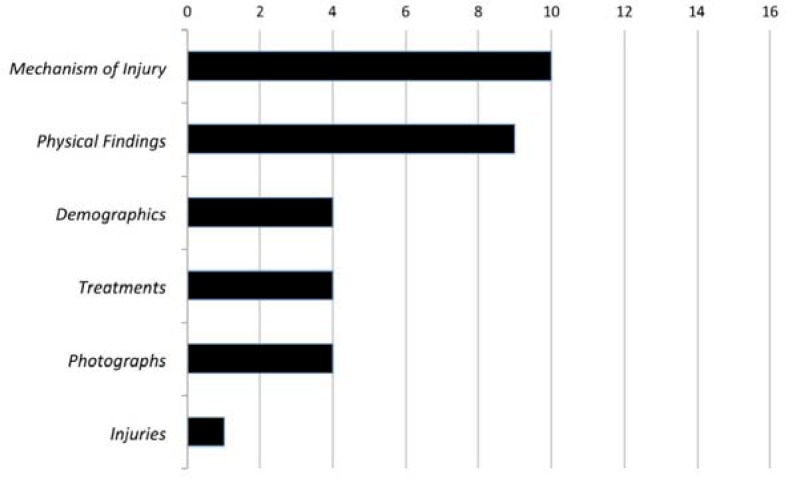
Previous research has shown that trauma teams make their initial decisions about patient management (e.g., equipment, specialists, and treatments) based on pre-hospital information [24]. Our interviews with trauma team members further examined the importance of pre-hospital information and identified information types that are critical during trauma resuscitation (Figure 5).
Figure 5:
Pre-hospital information needs, ranked by the number of participants who expressed the need for a particular information type.
Information types:
Our participants emphasized the importance of two pre-hospital information types in relation to other information: mechanism of injury and physical findings. Mechanism of injury, in particular, was considered important by ten participants because it helped the teams anticipate potential injuries, as described by an emergency medicine physician: “[I need to know] what happened, because it is really important to know… so you can assess the risks, what are potential injuries, and then anticipate impact on airway, breathing and circulation.”
Often times, however, information about the mechanism alone was not sufficient to adequately prepare for the patient arrival. For example, upon hearing mechanisms such as “pedestrian struck” or “kid run over,” team members assumed the worst scenarios until they saw the patient. As the nurse practitioner commented, the extent of injury is never completely known until the patient is before them:
“Some of those kids, they may have an abrasion. They have nothing wrong with them, but then other kids come in with every bone in their body broken. So we never know until they hit the door and even the report we get, sometimes they’re like, loss of consciences, hemodynamically unstable, and then [patients] roll through the door and they’re awake, alert and talking with normal vital signs.”
Information about physical findings, including neurological status (e.g., loss of consciousness) and vital signs, was therefore viewed as critical because it added the necessary detail to the mechanism of injury description. Trauma team leaders wanted to know physical findings in advance to be able to determine if additional specialists or more experienced providers were needed. A surgical fellow explained: “If a patient sounds like a pedestrian was struck and is now having a bad airway and is hypotensive, then I know right away I may have to call the anesthesia attending just so there’s somebody more experienced [in the room].” This information also helped the leader plan and allocate resources, e.g., if the patient needed a computer tomography (CT) scan, as further described by a surgical fellow: “[EMS] told me that the patient had lost consciousness and I immediately thought someone with this kind of mechanism should probably get a CT scan of the brain.”
Patient demographics, treatments en route, and photographs from the scene were also viewed as being important in preparation for the patient arrival. More specifically, trauma team members expressed the need to know patient age, weight, allergies and medical history, and if any fluids or medications were administered during transportation. Often times, however, information about patient medical history is not immediately available. As found through the interviews, the lack of medical history does not affect the care negatively. A nurse practitioner commented:
“[Allergies] are important but if I don’t have the information I don’t stop my primary survey to turn around and get allergies from mom or dad or the shot record. … For the most part, the meds that we’re giving in the trauma bay are emergency meds and it doesn’t matter. We have to give them. … Though [allergies] are [important], like [with] a kid with the big laceration, I am going to turn around to that parent and ask if the shots are up to date because if the shots are up to date then I don’t have to worry about the kid getting a tetanus shot.”
Photographs from the scene are welcome but not critical. Four participants saw photographs as a helpful addition to the summary of injuries because they visually augmented the EMS reports. A surgical resident explained:
“A lot of times, whoever brings [patients] in will bring a picture of the car, and that’s useful. I don’t think it’s vital right away. I think just saying somebody was in a car crash, and the car was going 5 miles an hour, versus 105 miles an hour, that to me is the most important piece of information. The only time a visual is helpful is if they were in a car crash going 20 miles an hour, and they were a restrained driver, and then in the picture of the car, the whole driver’s side is just completely torn apart, so you can see where the force came from.”
Although each information type serves an important role, trauma teams need all of the pre-hospital information combined to formulate initial decisions. For example, a nurse practitioner described a case in which information about injuries and physical findings informed the team’s decision to prepare for the chest tube placement:
“The [pre-hospital] information would change preparation, I mean in most cases, we have everything ready. But if we know someone has a chest stab wound, and the vitals are dropping, then we would prepare for chest tube and it would be more ready, so that would save some time.”
Challenges:
Our analysis of interview data showed several challenges that trauma teams face when receiving pre-hospital information. First, information from the field is not always accurate, as explained by a bedside physician: “I don’t feel it is precise. Many times we get different story. I don’t know if EMS didn’t give enough information to the ED, or ED didn’t deliver the reported information, there are so many people in the link. So lots of times I am not sure if the information got lost on the way, or there was another problem.” Second, some trauma team members arrive late to the trauma bay (e.g., they are held up by other duties) and miss the EMS report. To get up to speed, they ask the leader or the charge nurse to repeat the report, which leads to interruptions and frustrations of those involved in the care. An emergency fellow who often assumes the leadership role commented:
“I wait for enough people get into the room and say ‘ok, everybody, here is what’s going on.’ And then often times, the surgical coordinator runs late, and I have to redo it. Especially if the patient is getting sicker and we need anesthesia to do something, or we need nurse from ICU, so those who are late walk in and start asking questions, that’s going to be interruption.”
Finally, the biggest challenge is not getting enough information about an incoming patient, or not receiving a notification at all, as described by a respiratory therapist: “Trauma alert is warning you about the patient arrival. But you may not know how severe that trauma is; you don’t know who is coming to the ED; and even someone on the transport does not know how badly the patient is injured.”
Discussion
Our study has shown that the pre-hospital communication process is extremely important and involves multiple stakeholders. The efficiency and accuracy of communications between pre-hospital and hospital providers vary based on the available information, time, patient complexity, and EMS providers. Although we found that pre-hospital information needs of trauma team members match what is typically reported during pre-hospital communications, not all information types are available at all times; even when available, information may not necessarily be accurate. Time pressure plays an important role as well. Often times, EMS crews were not able to acquire the needed information, but called the hospital nevertheless to announce their arrival, reporting only a fraction of patient information. The efficiency of communications is also determined by the severity of injury. EMS teams spent more time and effort when announcing the arrival of more severely injured patients; these reports were also less structured and more speculative than those with less severely injured patients.
A computerized system that supports the use and retention of pre-hospital information during trauma resuscitation cannot address all of the challenges we identified in the pre-hospital communication process. Patient information is either available or not, and even the most sophisticated systems could hardly manage the challenge of missing or inaccurately reported information. The system could, however, help translate the pre-hospital narrative into a meaningful, easy-to-absorb data presentation for trauma team members. This data could be available in real time, as EMS providers communicate with emergency communication teams. Below we discuss two main design implications that emerged from our study, focusing primarily on translating existing pre-hospital narratives for efficient use and retention during trauma resuscitation.
Structured data input for efficient translation of pre-hospital narratives
Data acquisition from the field requires structured data input so that pre-hospital narratives can be effectively translated into dynamic data presentation for trauma team members. Structured data input, however, implies standardization of the pre-hospital communication process. Although standardizing handovers can reduce the cost of communication and improve patient safety [25], human factors researchers have increasingly argued against standardization given its many unintended consequences [26,27]. A study of handovers in the emergency department found that structured reports resulted in worse retention by the ED staff than unstructured reports [7].
Our analysis of en-route EMS reports showed that most EMS teams already follow a relatively stable structure when reporting patient data. The structure we identified is similar to that of previously proposed formats, such as MIST (Mechanism, Injuries, Signs, Treatments) or DeMIST (Demographics, Mechanism, Injuries, Signs, Treatments) [7,15]. For example, our P (physical findings) category includes the same types of information as reported under S (signs) in MIST or DeMIST protocols.
Our findings set the framework for developing mechanisms for structured data input for emergency communication teams (e.g., digital checklists or forms). Interviews with trauma team members uncovered information types that are critical not only to their preparation work but also during resuscitations. The importance of information items expressed by team members can help prioritize the items for data input. Results showing the structure of pre-hospital communications also contribute to designing the mechanisms for structured data input. For example, because patient demographics and mechanism of injury were always reported together, these two information items should be positioned in close proximity to allow for rapid data entry. Data input should be digitized so that it can be automatically fed into the display for trauma team members.
The adoption of structured data input in emergency communication can minimize information loss and cognitive load for both EMS and emergency communication teams. We should, however, keep in mind that “no representation of the world is either complete or permanent” [Error! Reference source not found.]. Protocols and other formal constructs will never exhaustively describe the action and will always encounter situations that go beyond precomputed boundaries. Affordances and constraints of structured data input mechanisms should therefore be studied, and our plan is to do so as we continue with this line of work in the future.
Interactive Pre-Hospital Data Presentation for Trauma Teams
We found that EMS teams report a great deal of information, most of which match the needs of trauma teams. Most EMS reports contained the information about injury mechanism, demographics, physical findings and treatments. Despite having most of the information available, trauma teams still faced a number of challenges when receiving pre-hospital data, a finding analogous to other studies of handovers between ambulance crews and ED staff [15]. Report from the field is usually heard once during preparation for patient arrival or upon patient arrival, when teams already start evaluating the patient, so teams rarely pay attention to the report. In addition, current pre-hospital communication system contains several links in the communication chain. Information rarely goes straight from the field to trauma teams; it first passes through the emergency communication center and ED physicians on call, who then provide summarized information to teams as they assemble for the patient arrival. Using a system that interactively displays pre-hospital data and makes it available in real time as emergency communication teams capture information from EMS teams could help facilitate the use and retention of pre-hospital information.
Although technologies exist for providing a direct link between EMS teams in the field and trauma teams in the hospital (e.g., telepresence systems [20]), we believe that the role of emergency communication teams should be preserved as they help acquire, clarify and verify information from the field. Even so, we can imagine information from the field being fed into the system through different sources, and not only through structured data capture provided by emergency communication teams. For example, patient vital sings and photographs from the field could be sent directly via sensors or video links. The key challenges in designing interactive displays for pre-hospital data presentation include grouping and visualizing high priority information, as well as integrating data from different sources. For efficient and sustained use, displays need to be positioned in the resuscitation rooms to allow for easy visual access (e.g., quick glance).
Study Limitations:
We focused our inquiry on one aspect of the entire pre-hospital communication process: pre-hospital communications between EMS teams and staff at the emergency communication center to understand the kinds of information that are available from the field. We did not examine summaries provided by ED physicians to trauma teams based on calls from the emergency communication center. Over the course of our fieldwork, we observed many such summaries, but we have not yet analyzed the data. This is part of our future work. Finally, we have not analyzed handovers occurring upon patient arrival, but we have observed and reported on these in our prior work, which this papers extends [5].
Conclusion and Future Work
We studied pre-hospital communications between pre-hospital and hospital staff, focusing on information types relayed during calls, the structure and nature of these communications, and the pre-hospital needs of trauma teams. However, our understanding of how pre-hospital communication affects subsequent patient care and how best to support the pre-hospital communication process is still limited. Our future work will focus on the work of emergency communication teams to better understand their work practices to support the design of mechanisms for structured data input. We also plan to conduct participatory design workshops with trauma team members to elicit design requirements for interactive pre-hospital data displays.
Acknowledgments
This material is based upon work supported by the National Science Foundation under Grant No. 0915871.
References
- 1.Barach P, Weinger MB. Trauma team performance. In: Wilson WC, Grande CM, Hoyt DB, editors. Trauma: Emergency resuscitation, perioperative anesthesia, surgical management. New York, NY: Informa Healthcare USA, Inc; 2007. [Google Scholar]
- 2.Xiao Y, Kim YJ, Gardner SD, Faraj S, MacKenzie CF. Communication technology in trauma centers: a national survey. J Emerg Med. 2006 Jan;30(1):21–8. doi: 10.1016/j.jemermed.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 3.Rowlands A. An evaluation of pre-hospital communication between ambulances and an accident and emergency department. J Telemed Telecare. 2003;9(Suppl 1):S35–7. doi: 10.1258/135763303322196277. [DOI] [PubMed] [Google Scholar]
- 4.Harrison JF, Cooke MW. Study of early warning of accident and emergency departments by ambulance services. J Accid Emerg Med. 1999 Sep;16(5):339–41. doi: 10.1136/emj.16.5.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sarcevic A, Burd RS. Information handover in time-critical work. ACM Conf Supporting Group Work Proc; 2009. pp. 301–310. [Google Scholar]
- 6.Thakore S, Morrison W. A survey of the perceived quality of patient handover by ambulance staff in the resuscitation room. Emerg Med J. 2001 Jul;18(4):293–6. doi: 10.1136/emj.18.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Talbot R, Bleetman A. Retention of information by emergency department staff at ambulance handover: do standardised approaches work? Emerg Med J. 2007 Aug;24(8):539–42. doi: 10.1136/emj.2006.045906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reddy MC, Paul SA, Abraham J, McNeese M, DeFlitch C, Yen J. Challenges to effective crisis management: using information and communication technologies to coordinate emergency medical services and emergency department teams. Int J Med Inform. 2009 Apr;78(4):259–69. doi: 10.1016/j.ijmedinf.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 9.Cheung DS, et al. Improving handoffs in the emergency department. Ann Emerg Med. 2010 Feb;55(2):171–80. doi: 10.1016/j.annemergmed.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 10.Currie J. Improving the efficiency of patient handover. Emerg Nurse. 2002 Jun;10(3):24–7. doi: 10.7748/en2002.06.10.3.24.c1064. [DOI] [PubMed] [Google Scholar]
- 11.Horn J, Bell MD, Moss E. Handover of responsibility for the anaesthetised patient - opinion and practice. Anaesthesia. 2004 Jul;59(7):658–63. doi: 10.1111/j.1365-2044.2004.03760.x. [DOI] [PubMed] [Google Scholar]
- 12.Abraham J, Nguyen V, Almoosa KF, Patel B, Patel VL. Falling through the cracks: information breakdowns in critical care handoff communication. AMIA Annu Symp Proc. 2011;2011:28–37. [PMC free article] [PubMed] [Google Scholar]
- 13.Abraham J, Kannampallil TG, Patel VL. Bridging gaps in handoffs: a continuity of care based approach. J Biomed Inform. 2012 Apr;45(2):240–54. doi: 10.1016/j.jbi.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 14.Cohen MD, Hilligoss PB. The published literature on handoffs in hospitals: deficiencies identified in an extensive review. Qual Saf Health Care. 2010 Dec;19(6):493–7. doi: 10.1136/qshc.2009.033480. [DOI] [PubMed] [Google Scholar]
- 15.Bost N, Crilly J, Wallis M, et al. Clinical handover of patients arriving by ambulance to the emergency department - a literature review. Int Emerg Nurs. 2010 Oct;18(4):210–20. doi: 10.1016/j.ienj.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 16.Brown R, Warwick J. Blue calls-time for a change? Emerg Med J. 2001 Jul;18(4):289–92. doi: 10.1136/emj.18.4.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.http://www.emscharts.com/
- 18.http://www.safepatientsystems.com/products/safe-triage-pro.ashx
- 19.Chan TC, Killeen J, Griswold W, Lenert L. Information technology and emergency medical care during disasters. Acad Emerg Med. 2004 Nov;11(11):1229–36. doi: 10.1197/j.aem.2004.08.018. [DOI] [PubMed] [Google Scholar]
- 20.McCurdy NJ, Griswold WG, Lenert LA. RealityFlythrough: enhancing situational awareness for medical response to disasters using ubiquitous video. AMIA Annu Symp Proc. 2005:510–4. [PMC free article] [PubMed] [Google Scholar]
- 21.Pavlopoulos S, Kyriacou E, Berler A, Dembeyiotis S, Koutsouris D. A novel emergency telemedicine system based on wireless communication technology—AMBULANCE. IEEE Trans Inf Technol Biomed. 1998 Dec;2(4):261–7. doi: 10.1109/4233.737581. [DOI] [PubMed] [Google Scholar]
- 22.Wong HJ, Caesar M, Bandali S, Agnew J, Abrams H. Electronic inpatient whiteboards: improving multidisciplinary communication and coordination of care. Int J Med Inform. 2009 Apr;78(4):239–47. doi: 10.1016/j.ijmedinf.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 23.Xiao Y, Lasome C, Moss J, Mackenzie CF, Faraj S. Cognitive properties of a whiteboard: A case study in a trauma centre. European Conf. on Computer-Supported Cooperative Work Proc; 2001. pp. 259–278. [Google Scholar]
- 24.Sarcevic A, Zhang Z, Kusunoki D. Decision making tasks in time-critical medical settings. ACM Conf Supporting Group Work Proc; 2012. pp. 99–102. [Google Scholar]
- 25.Owen C, Hemmings L, Brown T. Lost in translation: maximizing handover effectiveness between paramedics and receiving staff in the emergency department. Emerg Med Australas. 2009 Apr;21(2):102–7. doi: 10.1111/j.1742-6723.2009.01168.x. [DOI] [PubMed] [Google Scholar]
- 26.Patterson ES. Structuring flexibility: the potential good, bad and ugly in standardisation of handovers. Qual Saf Health Care. 2008 Feb;17(1):4–5. doi: 10.1136/qshc.2007.022772. [DOI] [PubMed] [Google Scholar]
- 27.Perry SJ, Wears RL, Patterson ES. High-hanging fruit: improving transitions in health care. In: Henriksen K, Battles JB, Keyes MA, Grady ML, editors. Advances in Patient Safety: New Directions and Alternative Approaches. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008. Aug, [PubMed] [Google Scholar]
- 28.Gerson EM, Star SL. Analyzing due process in the workplace. ACM Trans Info Syst. 1986 Jul;4(3):257–70. [Google Scholar]