Abstract
Cutaneous leishmaniasis and HIV coinfection has been reported in Brazil since the initial description of AIDS in the country. We report an HIV-positive patient under antiretroviral treatment who presented with cutaneous leishmaniasis which was successfully treated with meglumine antimoniate.
Keywords: Acquired immunodeficiency syndrome; HIV; Leishmaniasis, cutaneous
Abstract
A coinfecção leishmaniose cutânea e HIV tem sido descrita no Brasil desde o início da endemia de Aids no país. É relatado caso de paciente masculino, HIV positivo, em uso de terapia antirretroviral, que apresentou quadro de leishmaniose cutânea, tratada com antimoniato de meglumina.
A 33-year-old male HIV-positive patient presented with a three-month history of an assymptomatic lesion on the face. He had been taking biovir and efavirenz for the past six months. HIs T-CD4+ cell count was 380 cells/mm3 and viral load was below detection level. The patient lived in Manaus, capital of Amazonas State, but reported hunting on side roads off the interstate highway. Physical examination showed an ulcerated lesion, 4-cm in diameter, with irregular and infiltratated borders, granulous center on the right malar region. Smaller ulcers were also apparent, some with crusting around the central lesion (Figure 1). There were no submandibular, cervical or retro-auricular lymph nodes. Direct examination revealed Leishmania amastigotes, which were also revealed on histopathological examination (Figures 2 and 3). The patient was given meglumine antimoniate, 15 mg/kg/day endovenously, for 20 days and after a three-month follow-up, a complete reepitelization of the lesion was seen (Figure 4).
FIGURE 1.

An ulcerated lesion, about 4 cm in diameter, presenting with infiltrated borders on the left malar region
FIGURE 2.
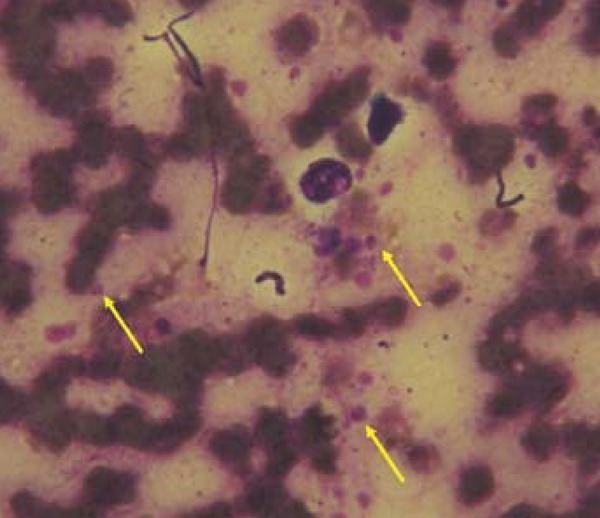
The arrows show Leishmania amastigotes
FIGURE 3.
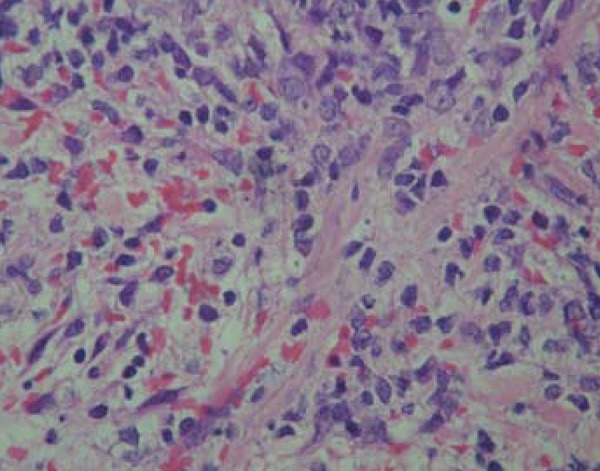
Histopatholo gical examination reveals inflammatory infiltrate consisting of histiocytes and plasmocytes. Leishmania amastigotes were revealed within the histiocytes
FIGURE 4.

Lesion reepitelization 3 months after first treatment
Mucocutaneous leishmaniasis and HIV/AIDS coinfection has been reported in Brazil since 1987.1 Recently, in a study conducted in the Amazon region, 7 of 15 coinfected patients presented with an atypical clinical picture or therapeutic failure, as has been observed in the rest of the country.2,3 According to the Brazilian Ministry of Health, any ulcerated or mucosal lesion in patients with HIV/AIDS exposed to leishmaniasis endemic areas should be investigated. Although the treatment of choice for mucocutaneous leishmaniasis and HIV/AIDS is amphotericin B, meglumine antimoniate is also an alternative drug for coinfection, approved by the Brazilian Ministry of Health.4,5
Footnotes
Work performed at the Amazonas Tropical Medicine Foundation (FMTAM) - Manaus (AM), Brazil.
Financial Support: None
Conflict of Interests: None.
REFERENCES
- 1.Coura JR, Castro GB, Grimaldi G., Jr Disseminated American Cutaneous Leishmaniasis in a Patient with AIDS. Mem Inst Oswaldo Cruz. 1987;82:581–582. doi: 10.1590/s0074-02761987000400019. [DOI] [PubMed] [Google Scholar]
- 2.Guerra JA, Coelho LI, Pereira FR, Siqueira AM, Ribeiro RL, Almeida TM, et al. American tegumentary leishmaniasis and HIV-AIDS association in a tertiary care center in the Brazilian Amazon. Am J Trop Med Hyg. 2011;85:524–527. doi: 10.4269/ajtmh.2011.11-0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rabello A, Orsini M, Disch J. Leishmania/HIV co-infection in Brazil: an appraisal. Ann Trop Med Parasitol. 2003;97:17–28. doi: 10.1179/000349803225002507. [DOI] [PubMed] [Google Scholar]
- 4.Lima EB, Porto C, Motta JOC, Sampaio RNR. Treatment of American cutaneous leishmaniasis. An Bras Dermatol. 2007;82:111–124. [Google Scholar]
- 5.Brasil; Ministério da Saúde do Brasil. Manual de Vigilância da Leishmaniose Tegumentar Americana. 2. ed. atual. Brasília: Ministério da Saúde; 2007. 180 p. (Série A. Normas e Manuais Técnicos). [Google Scholar]


