Abstract
Berardinelli-Seip syndrome is a rare autosomal recessive disease characterized by inadequate metabolism and inefficient storing of lipids in fat cells, generating accumulation of fat in organs such as the liver, spleen, pancreas, heart, arterial endothelium and skin. Classically, patients manifest generalized lipoatrophy at birth or until 2 years of age, and in adolescence usually develop marked insulin resistance with rapid progression to diabetes and dyslipidemia. We report the case of a 17-year-old Berardinelli-Seip syndrome patient with eruptive xanthoma associated with severe hypertriglyceridemia. It is worth noting Eruptive xanthoma as a dermatological manifestation that is not generally highlighted in the reports of cases of this genetic metabolic disorder.
Keywords: Acanthosis nigricans; Diabetes mellitus; Dyslipidemias; Lipodystrophy, congenital generalized; Xanthomatosis
Abstract
Síndrome de Berardinelli-Seip é doença genética autossômica recessiva rara, caracterizada por ineficiência em metabolizar e estocar material lipídico adequadamente nos adipócitos, gerando acúmulo de gordura em órgãos não habituais, como fígado, baço, pâncreas, coração, endotélio arterial e pele. Classicamente, os portadores nascem ou manifestam lipoatrofia generalizada até os 2 anos e, geralmente na adolescência, desenvolvem marcada resistência insulínica com rápida progressão para diabetes e dislipidemia. Relatamos um caso de portadora da síndrome de Berardinelli-Seip, de 17 anos, com xantoma eruptivo associado à hipertrigliceridemia grave. Ressalta-se o xantoma eruptivo como manifestação dermatológica não enfatizada nos casos relatados sobre esse distúrbio metabólico genético.
CASE REPORT
A 17-year-old female patient was referred from the Endocrinology Department with yellowish papules on her arms and legs for about a year.
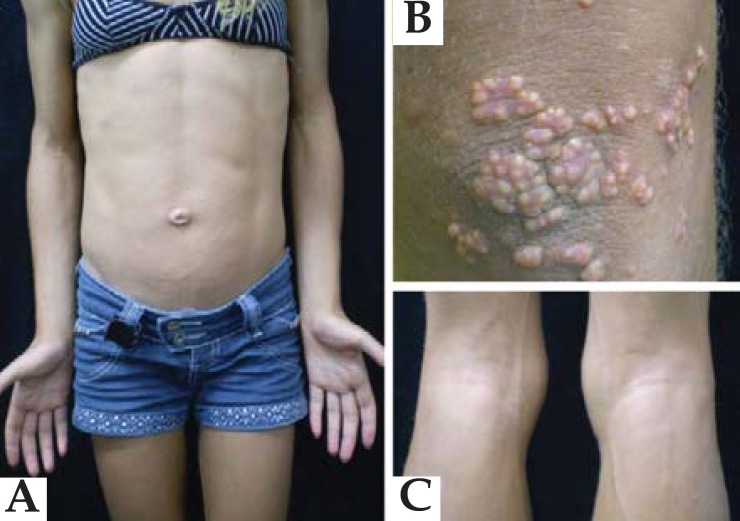
On examination, the patient presented acromegaloid fascies, generalized lipoatrophy, phlebomegaly, hepatomegaly, axillary acanthosis nigricans, clitoromegaly, and yellowish coalescing and isolated papules with an erythematous halo in the upper and lower limbs (Figure 1).
FIGURE 1.
A: Generalized lipoatrophy leading to an athletic appearance. B: Right elbow showing coalescing and isolated yellow papules with erythematous halo. C: Phlebomegaly in the lower limbs
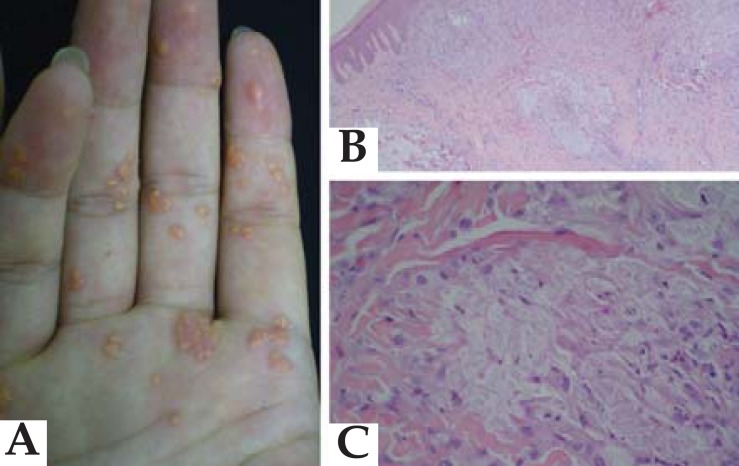
From birth, she presented a total absence of subcutaneous fat. At age 10, she had impaired glucose tolerance which, because unchecked, had developed into diabetic ketoacidosis in under one year. Subsequently, she presented type 2 diabetes mellitus (DM) associated with dyslipidemia and hepatic steatosis. These disorders were not responsive to the usual pharmacological doses, and required the administration of high doses of exogenous insulin, oral hypoglycemic and hypolipidemic agents. Despite therapy, tests showed fasting glucose level of 284 mg/dl; postprandial glucose, 423 mg/dl; total cholesterol, 579 mg/dl; and triglycerides, 3.194 mg/dl. Histopathological examination confirmed clinical hypothesis of eruptive xanthoma (Figure 2).
FIGURE 2.
A: Palmar region showing yellowish papules with erythematous halo. B: Rectified and epidermal inflammatory infiltrate composed of lymphocytes and xanthomized histiocytes in upper and middle dermis. (Hematoxylin–eosin; 40× magnification). C: Detail of xanthomized histiocytes (hematoxylin–eosin; 400× magnification)
DISCUSSION
Berardinelli-Seip syndrome (BSS) or Berardinelli-Seip congenital lipoatrophy, is a rare autosomal recessive genetic disease, with only up to 200 reported cases to date.1,2 The first case was reported in Brazil in 1954 by Berardinelli.3 Four years later in Norway, Seip described the cases of 3 patients. Since then, this disease has been referred to as the Seip-Berardinelli syndrome.4,5
BSS is diagnosed in cases where 3 major criteria or 2 major criteria and 2 or more minor criteria are met (Chart 1).6
CHART 1.
Diagnostic criteria of BSCL
| Major Criteria | Minor Criteria |
| • Lipoatrophy affecting the trunk, limbs, and face | • Hypertrophic cardio- myopathy |
| • Acromegalic appearance (gigantism, prog- nathism, muscle hypertrophy leading to an athletic appearance, advanced bone age, increased size of hands and feet, clitorome- galy or increased size of external genitalia in men | • Mild (IQ, 50-70) to moderate psychomo- tor retardation (IQ*, 35-50) |
| • Hepatomegaly | • Hirsutism |
| • Increased serum triglycerides (sometimes associated with hypercholesterolemia) | • Early puberty in girls |
| • Insulin resistance (increase in serum C- peptide and insulin levels)\acanthosis nigricans | • Bone cysts |
| • Phlebomegaly |
Source: Khandpur S, et al. 6
IQ: intelligence quotient.
The pathogenic mechanism of SBS is related to inefficiency in metabolizing and storing lipid material and is represented by generalized lipoatrophy, hirsutism and acanthosis nigricans.7
Classically these patients develop progressive peripheral insulin resistance, with rapid evolution for diabetes type 2, as in our patient, whose Diabetic Ketoacidosis was manifested at 10 years old. Early development of atherosclerosis can be observed as well as non-alcoholic fatty liver disease (often progressing to liver cirrhosis), and type V dyslipidemia (Fredrickson classification), which is represented by increased serum chylomicrons, very low-density lipoproteins (VLDL), and triglyceride levels.8
Our patient showed 5 major diagnostic criteria and one minor criterion (Chart 1).
Eruptive xanthoma is characterized by the appearance of yellowish papules with erythematous halo arising from the deposition of increased blood triglycerides in the skin. The papulae are generally observed around the buttocks and extensor surfaces of the extremities. These papulae occur in BSS patients with chylomicronemia and hypertriglyceridemia, and these could be caused by either lipase deficiency or hyperlipidemia type V.8 Furthermore, this could lead to eruptive xanthomas, as previously shown in the case of a Brazilian BSS patient.9 Despite this condition being an expected cutaneous manifestation in patients with severe and resistant type of dyslipidemia, the medical literature has not highlighted this aspect of cutaneous syndrome. This may indicate that the majority of studies have been conducted in the fields of metabolism and genetics. However, we consider these cutaneous manifestations important and assume that xanthomas are predictors of lipid dysregulation.
The therapy that we administered restricted lipid intake and increased the intake of polyunsaturated fats. We also employed medical management of dyslipidemia associated with insulin resistance or diabetes and closely monitored the liver and cardiovascular system to prevent fatal liver and cardiological complications.1
Footnotes
Work performed at the Pedro Ernesto University Hospital - Rio de Janeiro State University, Rio de Janeiro (RJ), Brazil.
Financial Support: None.
Conflict of Interests: None.
REFERENCES
- 1.Garg A. Acquired and inhereited lipodysthrofies. N Engl J Med. 2004;350:1220–1234. doi: 10.1056/NEJMra025261. [DOI] [PubMed] [Google Scholar]
- 2.Agarwal AK, Garg A. Genetic disorders of adipose tissue development, differentiation, and death. Annu Rev Genomics Hum Genet. 2006;7:175–199. doi: 10.1146/annurev.genom.7.080505.115715. [DOI] [PubMed] [Google Scholar]
- 3.Berardinelli W. An undiagnosed endocrinometabolic syndrome: report of 2 cases. J Clin Endocrinol Metab. 1954;14:193–204. doi: 10.1210/jcem-14-2-193. [DOI] [PubMed] [Google Scholar]
- 4.Seip M. Lipodystrophy and gigantismo with associated endocrinone manifestation: a new diencephalic syndrome? . Acta Paediatr. 1959;48:555–574. [PubMed] [Google Scholar]
- 5.Seip M, Trygstad O. Generalized lipodystrophy. Arch Dis Child. 1963;38:447–453. doi: 10.1136/adc.38.201.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khandpur S, Kumar A, Khadgawat R. Congenital generalized lipodystrophy of Berardinelli-Seip type: A rare case. Indian J Dermatol Venereol Leprol. 2011;77:402–402. doi: 10.4103/0378-6323.79740. [DOI] [PubMed] [Google Scholar]
- 7.Haque W, Garg A, Agarwal AK. Enzimatic activity of naturally occurring 1-acylglycerol- 3-phosphate-0-acyltransferase 2 Mutants Associated with Generalized Lipodysthrophy. Biochem Biophys Res Commun. 2005;327:446–453. doi: 10.1016/j.bbrc.2004.12.024. [DOI] [PubMed] [Google Scholar]
- 8.Naik S N. Eruptive xanthomas. Dermatol Online J. 2001;7:11–11. [PubMed] [Google Scholar]
- 9.Sousa JB, Carvalho SP, Pereira LB, Vale ES. Você conhece esta síndrome? An Bras Dermatol. 2006;81:87–90. [Google Scholar]