Abstract
Background
No gold standard exists for identifying successful outcomes 1 and 2 years after operative and non-operative management of anterior cruciate ligament (ACL) injury. This limits the ability of researcher and clinicians to compare and contrast results of interventions.
Purpose
to establish a consensus based on expert consensus of measures that define successful outcomes 1 and 2 years after ACL injury or reconstruction.
Methods
Members of international sports medicine associations, including the American Orthopaedic Society for Sports Medicine (AOSSM), the European Society for Sports Traumatology, Surgery, and Knee Arthroscopy (ESSKA), and the American Physical Therapy Association (APTA), were sent a survey via e-mail. Blinded responses were analyzed for trends with frequency counts. A summed importance percentage (SIP) was calculated and 80% SIP operationally indicated consensus.
Results
1779 responses were obtained. Consensus was achieved for six measures in operative and non-operative management: the absence of giving way, patient return to sports, quadriceps and hamstrings strength greater than 90% of the uninvolved limb, the patient having no more than a mild knee joint effusion, and using patient reported outcomes (PRO). No single PRO achieved consensus, but threshold scores between 85 and 90 were established for PROs concerning patient performance.
Conclusion
The consensus identified six measures important for successful outcome after ACL injury or reconstruction. These represent all levels of the International Classification of Functioning; effusion, giving way, muscle strength (body structure and function), PRO (activity and participation), and return to sport (participation) and should be included to allow for comparison between interventions.
Keywords: anterior cruciate ligament (ACL), successful outcome, patient reported outcomes (PRO), survey research
INTRODUCTION
Criteria used to assess outcomes after anterior cruciate ligament injury address the physical and personal domains of the World Health Organization’s International Classification of Functioning, Disability, and Health (WHO-ICF): impairments in body structure and function, activity limitations and participation restrictions. Joint effusion, joint laxity, muscle strength, functional performance tests, and patient reported outcomes (PROs) are used to determine the severity of the injury and track progress over time.[1-5] The breadth of outcomes allows for researchers to identify whether or not their intervention was successful for the target measure (e.g. quadriceps strength increased after strength training; anterior tibiofemoral laxity minimized with surgical reconstruction).
PROs specific to the knee joint and ACL injury with established validity, reliability and responsiveness abound.[2,6,7] PROs measure patient perspective on how the knee joint affects daily life and sports activities[1,8], which has a greater influence on patient satisfaction than standard clinical measures.[9] PROs are especially effective in comparing the results of interventions on patient perspective after injury, in both clinical practice and research.[9,10] PROs fall into two major categories – self-reported patient performance scales which measure function and symptoms; and activity level measures of frequency of participation. Clinical performance based outcomes such as quadriceps strength and functional hop testing capture different aspects of function than self-reported function.[11] Therefore, a combination of outcome measures is likely necessary to provide a comprehensive evaluation of functional success.[11,12]
The research and clinical communities lack a gold standard definition of success. Each of the commonly used outcomes has its place in the continuum of care, although some outcome measures are not feasible in every practice or clinic, limiting their generalizability. Additionally, most of the outcomes do not have validated thresholds or normative data for defining success. An ideal outcome to identify success after injury should be easy to administer, generalizable to all clinical settings, and target all realms of the health condition – body structure and function, activity and participation.[1] Additionally, clearly defined scores for differentiating successful management from unsuccessful management should be established for each measure used.
Establishing a professional consensus definition of success is an important step forward in choosing outcome measures after ACL injury. This investigation sought expert consensus on a minimum set of outcomes to identify successful outcome one and two years after ACL injury or reconstruction through an online survey. We also sought to similarly identify consensus expert consensus for threshold scores for those patient reported outcomes that were considered important for identifying a successful outcome after ACL injury or reconstruction. We hypothesized that return to sport, absence of giving way, patient reported measures of function, functional tests, and quadriceps strength would be identified by a majority of respondents as important measures of successful outcome after ACL injury or reconstruction. We also hypothesized that measures of hamstrings strength, passive laxity, effusion and arthritis would not be identified as important measures of successful outcome 1 or 2 years after ACL injury or reconstruction because these variables do not have as significant an impact on function in the 1 to 2 year time frame. In the discussion section, the empirical evidence in support of the measures will also be discussed.
METHODS
Survey Development and Content
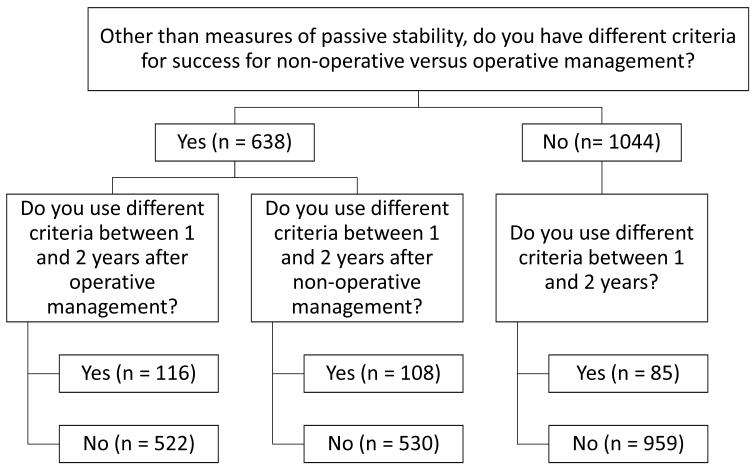
The Delaware-Oslo ACL Cohort Research Group developed a preliminary paper and pencil survey to identify important measures of successful outcomes 1 and 2 years after ACL injury or reconstruction based on a literature review and the recommendation of experts in orthopedic surgery (two surgeons with over 20 years of experience each) and physical therapy (two established principal investigators in the field of rehabilitation after ACL injury and reconstruction and four graduate students with a track record of publication and presentation in the same area). This survey was provided to attendees of the 2010 Congress of the European Society for Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA). Based on 40 preliminary responses from orthopedic surgeons and physical therapists at ESSKA 2010, the original survey was modified and a final online version of the survey was created complete with survey logic to minimize the response burden (See Appendix). Two screening questions were asked (1) “do you use different criteria to identify successful outcome between those patients undergoing operative management and non-operative management?” and (2) “do you use different criteria to identify successful outcome at 1 and 2 years post intervention?” If respondents used different criteria for operative and non-operative management, they were asked about each individually. If respondents used different criteria at 1 and 2 years post-intervention, they were asked about each individually. The questions and the responses to them are illustrated in the flow chart in Figure 1. Preliminary responses from ESSKA 2010 were not included in these results; however these respondents were invited to participate in the final version.
FIGURE 1. RESPONSES TO SCREENING QUESTIONS FOR OPERATIVE VS. NON-OPERATIVE MANAGEMENT AND CRITERIA BETWEEN FOLLOW-UPS.
97 Respondents indicated that they did not allow patients to return to sports with non-operative management.
All domains of the WHO-ICF were represented in the proposed criteria. The items chosen for inclusion in the survey are frequently used as outcome measures in clinical practice and research. Return to play is used as a measure of participation restrictions. Functional tests mimic the demands of play in controlled settings to identify activity limitations. Impairments in body structure and function are quantified with effusion measurements (a surrogate of inflammation), measures of laxity (arthrometry and the pivot-shift test) and instability (giving way of the knee), radiographic degeneration, and muscle strength. Persistent effusion, excessive laxity, a positive pivot-shift, and arthritis are all associated with poor self-reported outcomes and satisfaction after ACL injury. [9,13-15] Patient reported outcomes measure patient perception on how their knee affects their participation, activity, and body structure and function, as well as contextual factors.[1,7]
The proposed criteria are further defined in the online supplemental materials (Appendix) and summarized in Table 1 (with abbreviations used in Figures and Tables), per their role in the WHO-ICF guidelines. A rating scale was used to allow respondents to identify the relative importance of each criterion (Table 2). The answer choices for each item were explicitly defined without the ability for the respondent to respond with a narrative. A free text general comment box was provided at the end of the survey.
Table 1.
Criteria Proposed in the Survey
| Realm of Function |
To consider management successful, one (two) year(s) after surgery (injury), the athlete must: |
Abbreviations |
|---|---|---|
| Participation | Have played one (two) season(s) in the sport of injury at the same level as prior to injury. |
RTS |
| Activity | Achieve symmetrical performance on a functional test | Functional Test |
| Body Structure and Function |
Not have more than a mild, persistent effusion | Effusion |
| Not have any episodes of giving way | Give Way | |
| Not have radiographic progression of osteoarthritis | OA | |
| Have a laxity difference < 3mm on instrumented testing | Laxity | |
| Have a pivot shift grade of normal | Pivot-shift | |
| Achieve symmetrical quadriceps strength (>90% of the uninvolved limb) |
Quads | |
| Achieve symmetrical hamstrings strength (>90% of the uninvolved limb) |
Hams | |
| Patient Reported Outcome Measure |
Achieve >90% on an outcome tool | PRO |
| Knee Outcome Survey –Activities of Daily Living Scale | KOS-ADLS | |
| Knee Outcome Survey –Sports Activities Scale | KOS-SAS | |
| Global rating of perceived function | GRS | |
| Tegner Activity Scale | Tegner | |
| Lysholm Score | Lysholm | |
| International Knee Documentation Committee 2000 Subjective Knee Form |
IKDC2000 | |
| Cincinnati Knee Score | Cincinnati | |
| Knee Injury and Osteoarthritis Outcome Score | KOOS | |
| Marx Activity Rating Scale | Marx |
Table 2. Rating Scale for Survey Questions.
| Rating | Description |
|---|---|
| Primary Importance | This criterion should be measured in all cases, as it is truly important for success. |
| Secondary Importance | Indicates good progress, but is not necessary for success. |
| Not Important/Do Not Use | Does not affect the outcome or does not matter, or I do not use it. |
| Indifferent | No opinion on the value of this measure. |
| Unfamiliar with measure |
Analysis of Patient Reported Outcome Measures
Respondents who indicated that PROs were of primary or secondary importance as a measure of successful outcome after ACL injury or reconstruction were asked to identify which of nine common PROs used after ACL injury were important measures of successful outcome. Respondents who indicated that a PRO was an important measure of successful outcome were asked a final follow-up free text question to identify threshold scores that indicate successful outcome after ACL injury or reconstruction. Several PROs demonstrate exceptional performance in reliability, validity, and responsiveness and are available for the knee joint and ACL injuries.[2,7,16] The individual PROs proposed were the Knee Outcome Survey –Activities of Daily Living Scale (KOS-ADLS), Knee Outcome Survey –Sports Activities Scale (KOS-SAS), Global rating of perceived function (GRS), Lysholm Score, International Knee Documentation Committee 2000 Subjective Knee Form (IKDC2000), Cincinnati Knee Score, Knee Injury and Osteoarthritis Outcome Score (KOOS), (Patient Performance Measures); and the Tegner Activity Scale and Marx Activity Rating Scale (Activity Level Measures).
Populations
The survey was administered through a survey generating website (qualtrics.com; Qualtrics, Inc.). The memberships of international sports medicine organizations were targeted: the American Orthopedic Society for Sports Medicine (AOSSM), the Sports Physical Therapy Section of the American Physical Therapy Association (SPTS) and ESSKA. Each organization was polled through direct e-mail contact twice. Additionally, member organizations of the International Federation of Sports Physical Therapists and subscribers to the Journal of Orthopedic & Sports Physical Therapy were provided with the survey. Organizations who confirmed distribution to their membership are identified in Table 3. It is not possible to determine true response rates for the smaller organizations due to unconfirmed distribution sizes. The data presented in Table 3 is for reference of the scope of the distribution. Safeguards preventing the completion of the survey multiple times from the same internet location were used to limit the number of responses from the same individual.
Table 3. Sports Medicine Organizations with Confirmed Participation.
| American Orthopedic Society for Sports Medicine |
Sports Physical Therapy Section of the American Physical Therapy Association |
European Society for Sports Traumatology, Knee Surgery and Arthroscopy |
| Italian Manual Therapy Group |
Portuguese Sports Physiotherapy Group |
Irish Society of Chartered Physiotherapists |
| Association of Turkish Sports Physiotherapists |
Swiss Sports Physiotherapy Association |
Italian Sport Specialist Group |
| Association of Chartered Physiotherapists in Sports Medicine (UK) |
Norwegian Manual Therapy Association |
Demographic data were collected including clinical discipline, country/continent of practice, and years of experience. All respondents answered questions concerning successful outcome after operative management. Respondents were asked whether they allow patients with ACL deficiency to return to sports without reconstruction. If respondents indicated that they allowed non-operative return to sports, they answered questions concerning successful outcome after non-operative management. Surveys completed by individuals identifying themselves as orthopedic surgeons, rehabilitation specialists (physical therapists and athletic trainers), researchers or other pertinent professions were included for analysis. Surveys from those deemed inappropriate to respond were excluded from the analysis (students, personal trainers, fitness professionals). To obtain a broad representation of the state of clinical practice, respondents who were in clinical practice were included regardless of years of clinical experience. We included these respondents as experts as they have received extensive training and are responsible for determining the outcomes of their patients, and thus are considered experts by their patients.
Survey Analysis
Frequency counts for each question were analyzed for trends. Criteria identified as having “Primary Importance” and “Secondary Importance” were operationally defined as positive. Criteria identified as “Not Important/Do Not Use” were operationally defined as negative. Criteria identified as “Indifferent” were operationally defined as having no impact on the overall value of a measure. Respondents who were unfamiliar with the measure were not used in the determination of importance. Overall importance of each criterion was based on a summed importance percentage considering perspectives on each measure:
An operational definition of 80% was used to identify consensus. An 80% threshold has been used previously to identify consensus in surveys of orthopedic surgeons with a different rating scale.[17] This study was approved by the Human Subjects Review Board at The University of Delaware.
RESULTS
Respondents
Responses for the final online survey were obtained from 553 orthopedic surgeons, 1132 rehabilitation specialists, and 94 responding “other” (researchers, sports medicine physicians), for a total of 1779 respondents. Responses were obtained from every continent (Table 4). The average practice time of respondents was 14 years (1 – 45 years). Respondents belonged to over 125 professional organizations, with large representative samples from the targeted organizations: SPTS (6097 distributed, 665 returned, 11% response rate), AOSSM (2615 distributed, 338 returned, 13% response rate), and ESSKA (1378 distributed, 263 returned, 19%; Table 5). Response rates for other organizations were not available as the number of surveys distributed was not available.
Table 4. Demographics of Survey Respondents.
| Profession | n | Years Practicing |
Africa | Asia | Australasia | Europe | North Americ a |
South Americ a |
|---|---|---|---|---|---|---|---|---|
| MD | 553 | 15.7 (±10.1) | 5 | 18 | 4 | 240 | 276 | 7 |
| Rehab | 1132 | 13.6 (±10.2) | 0 | 11 | 16 | 384 | 698 | 3 |
| Other | 94 | 14.1 (±8.6) | 0 | 1 | 0 | 13 | 9 | 0 |
| Total | 1779 | 14.5 (±10.2) | 5 | 30 | 20 | 637 | 983 | 10 |
93 respondents did not provide enough information for identification of location.
1 rehabilitation specialist from Antarctica responded
Other included researchers and non-surgeon sports medicine physicians
Abbreviations: MD: Orthopedic Surgeons
Rehab: Rehabilitation Specialists
Table 5. Sports Medicine Organizations with at least 10 respondents.
| Organization | # of Respondents |
|---|---|
| American Physical Therapy Association | 665 |
| American Orthopaedic Society for Sports Medicine | 338 |
| American Academy of Orthopaedic Surgeons | 319 |
| European Society of Sports Traumatology Knee Surgery and Arthroscopy | 263 |
| International Society of Arthroscopy Knee Surgery and OrthopaedicSports Medicine |
190 |
| American College of Sports Medicine | 124 |
| National Athletic Trainers Association | 98 |
| Arthroscopy Association of North America | 76 |
| Norwegian Sport Physiotherapy Group (NSPG) of the Norwegian Physiotherapist Association |
66 |
| Irish Society of Chartered Physiotherapists (ISCP) | 66 |
| Portuguese Sports Physiotherapy Group (PSPG) | 51 |
| National Strength and Conditioning Association | 42 |
| Orthopaedic Research Society | 40 |
| Chartered Physiotherapists in Sports and Exercise Medicine (CPSEM) (Ireland) |
40 |
| Gruppo Di TerapiaManuale, a special interest group of AssociazioneItalianaFisioterapisti (AIFI) |
33 |
| Association of Chartered Physiotherapists in Sports Medicine (United Kingdom) |
33 |
| Swiss Sports Physiotherapy Association (SSPA) | 26 |
| Chartered Physiotherapists in Manipulative Therapy (CPMT) | 20 |
| Canadian Physiotherapy Association | 18 |
| American Academy of Orthopaedic Manual Physical Therapists | 16 |
| Swedish Society of Sports Medicine | 15 |
| Canadian Orthopaedic Division | 14 |
| Norwegian Manual Therapy Association | 13 |
| International Cartilage Repair Society | 10 |
| Association of Turkish Sports Physiotherapists (ATSP) | 10 |
Outcome Criteria
The vast majority of orthopedic surgeons (89.2%) and rehabilitation specialists (97.0%) responded that they allow patients to return to sports without ACL reconstruction. Consensus was achieved for the same six measures in for both one and two years after operative and non-operative management encompassing the domains of the WHO-ICF: the absence of giving way, quadriceps and hamstrings strength greater than 90% of the uninvolved limb, the patient having no more than a mild knee joint effusion (body structure and function), patient return to sports (participation), and using patient reported outcomes (participation and activity) (Table 6). Laxity measures, functional testing and measures of osteoarthritis did not achieve consensus. The majority of patients indicated that they used the same criteria for both operative and non-operative management (n = 1044, 58.7%) and for one and two years post-intervention (n = 1481, 83%), therefore, the results for operative and non-operative management and for one and two years are very similar (Figure 1).
Table 6. Summed Importance Percentages for Outcome Criteria After ACL Injury.
| Operative Management | Non-operative Management |
|||
|---|---|---|---|---|
| 1 year | 2 year | 1 year | 2 year | |
| Absence of Giving Way* |
96.6 | 96.4 | 96.2 | 96.5 |
| Return to Sports* | 91.7 | 92.4 | 91.7 | 92.7 |
| Quadriceps Strength Symmetry* |
90.5 | 90.3 | 90.7 | 90.7 |
| Absence of Joint Effusion* |
84.1 | 84.1 | 85.0 | 85.0 |
| Hamstrings Strength Symmetry* |
83.7 | 83.1 | 85.7 | 85.6 |
| Patient Reported Outcomes* |
83.2 | 83.2 | 83.2 | 83.5 |
| Functional Test | 75.4 | 75.6 | 73.3 | 73.5 |
| Negative Pivot-shift | 77.8 | 77.9 | 66.4 | 66.4 |
| Laxity < 3mm | 72.9 | 72.5 | 67.2 | 67.1 |
| Absence of Radiographic Osteoarthritis |
36.5 | 37.4 | 40.3 | 41.3 |
indicates measures for which the operational definition of consensus was reached (80%)
No PRO had a summed importance percentage that met the consensus criteria of 80% for any of the four time points in consideration. Of the survey respondents who indicated that PROs were an important measure of successful outcome after ACL injury or reconstruction, over 40% indicated that the GRS, KOS-ADLS, and KOS-SAS were important (Table 7). Over 40% of respondents identified the Cincinnati Knee Score and the Marx Activity Rating Scale as being unimportant measures of successful outcome after ACL injury and reconstruction. 40% were unfamiliar with the Marx Activity Rating Scale.
Table 7. Importance and Threshold Scores Identified for PROs.
| N1 | Important | Not Important |
Unfamiliar | N2 | Operative | Non- operative |
|
|---|---|---|---|---|---|---|---|
| PRO | Operative Non-operative |
Operative Non-operative |
Median [1Q, 3Q] |
Median [1Q, 3Q] |
|||
| GRS | 1374 1261 |
45% | 32% | 17% | 123 107 |
90 [90, 90] |
90 [85, 90] |
| KOS-SAS | 1386 1267 |
42% | 35% | 18% | 87 75 |
90 [80, 90] |
90 [80, 90] |
| KOS- ADLS |
1382 1266 |
41% | 36% | 17% | 95 84 |
90 [80, 90] |
90 [80, 90] |
| IKDC2000 | 1377 1262 |
38% | 33% | 24% | 87 70 |
90 [85, 90] |
90 [85, 90] |
| KOOS | 1379 1263 |
37% | 38% | 18% | 56 48 |
85 [80, 90] |
85 [80, 90] |
| Lysholm | 1382 1269 |
36% | 36% | 22% | 94 76 |
90 [85, 90] |
85 [82.5, 90] |
| Cincinnati | 1363 1253 |
29% | 42% | 22% | 33 25 |
90 [80, 90] |
90 [80, 90] |
| Tegner | 1379 1268 |
29% | 38% | 28% | 38 32 |
7 [6, 8] | 7 [5,8] |
| Marx | 1354 1247 |
13% | 42% | 40% | 10 7 |
12 [8.5, 12] |
12 [10, 12] |
Abbreviations: PRO – patient reported outcome; N1 – the number of respondents concerning the importance of each PRO (maximum 1490 operative, 1326 non-operative) ; N2 – the number of respondents who provided a valid threshold score for defining success on each measure; 1Q – the first quartile representing the 25th percentile; 3Q – the third quartile representing the 25th percentile; GRS – global rating scale; KOS-SAS – Knee Outcome Score – Sports Activities Scale; KOS-ADLS - Knee Outcome Score – Activities of Daily Living Scale; IKDC2000 – International Knee Documentation Committee 2000 Subjective Knee Form; Lysholm – Lysholm Knee Score; Cincinnati – Cincinnati Knee Score; Tegner – Tegner Activity Scale; Marx – Marx Activity Rating Scale
For PROs of patient performance, median threshold scores for measuring a successful outcome one and two years after operative or non-operative management were between 85 and 90 with threshold scores skewed toward the higher end of the scale as indicated by the small interquartile ranges (Table 7). For the Tegner Activity Scale and Marx Activity Rating Scale (activity level measures), median threshold scores were identified as 7 (Competitive sports- tennis, running, motorcars speedway, handball; Recreational sports- soccer, football, rugby, ice hockey, basketball, squash, racquetball, running) and 12 (at least one time in a week for running, cutting, decelerating and pivoting on average) respectively.
DISCUSSION
The purpose of this study was to establish a consensus based on expert consensus about measures to determine successful outcome one and two years after ACL injury or reconstruction. Our hypotheses were largely supported. The absence of symptomatic knee joint instability, patient return to sports, quadriceps and hamstrings strength symmetry, the presence of no more than a mild knee joint effusion, and patient reported outcomes were identified as important measures of successful outcome one and two years after ACL injury or reconstruction. Functional tests, laxity measures, and arthritis were not identified as important measures of successful outcome one or two years after ACL injury or reconstruction. Although consensus was achieved that PROs are an important measure of successful outcome after ACL injury or reconstruction, consensus was not achieved for any individual PRO as being an indicator of successful outcome one or two years after ACL injury or reconstruction. However, respondents identified median threshold scores between 85% and 90% for patient performance measures, and threshold scores that identified weekly participation at high levels for activity level measures.
Outcome Criteria Achieving Consensus
Symptomatic instability is failure of both the passive ligamentous restraint and the active neuromuscular restraints to knee stability. Giving way is an inability to actively stabilize the ACL deficient knee and a re-injury to the reconstructed knee. This instability potentially puts other structures in the knee at risk for injury, including the meniscus and collateral ligaments.[18,19] A knee joint with multiple injuries leads to poorer outcomes in the long term, including poor self-report and increased arthritic changes.[20-22] Therefore, recurrent instability is indicated as a primary reason to perform reconstruction and giving way serves as an important measure of successful outcome after both ACL injury and reconstruction.[17]
As the majority of ACL injuries occur during sport, it is likely that the patient’s ultimate goal is to return to that sport.[23-25] Therefore, patient return to sport status is a measure of the success of the surgical procedure and/or rehabilitation protocol, as well as a measure of patient satisfaction, and was identified as such. However, patient return to sport is influenced by contextual factors personal to the athlete and from the competitive environment, more so than the other measures in consideration in this study.[24] Sport participation at pre-injury levels may not be available due to life situations (graduation beyond the level at which skill level allows participation, time constraints due to work/school/family), personal choices and perspectives (fear of re-injury, changing sport), or environmental factors (no snow to downhill ski, too much snow to play soccer). Contextual factors may impact the participation of the patient, regardless of the functional performance capabilities of their knee joint. Additionally, patients may return to their sport of injury, but may not have the same ability as pre-injury for any number of reasons including confidence and functional performance[23], which may indicate an unsuccessful management for the patient or medical team. Regardless of motivation, the simplicity of patient self-reporting the ability to return to sport can be an extremely valuable measure of success one and two years after ACL injury or reconstruction.
Our hypothesis that PROs would be identified as important measures of successful outcome one and two years after ACL injury and reconstruction was supported by our data. PROs are frequently used to report outcomes in large scale studies of knee injury, including registries and multicenter trials, due to well established validity, reliability, and responsiveness for these outcomes, as well as ease of application and standardization.[26-28] PROs measure various aspects of function and can be directly compared without clinician bias. Patient perception is a key element in determining whether or not an intervention was successful. The variation in PROs allows clinicians and researchers flexibility in choosing a measure for their population, however, the many PROs available make it difficult to compare across trials. Identifying the best measure available and encouraging its use would improve our ability to compare results. However, to truly measure global function, it is likely that a more comprehensive and representative measure is needed.
The GRS [also called the single assessment numeric evaluation (SANE)] was most frequently identified as an important measure of successful outcome one and two years after ACL injury or reconstruction likely due to its simplicity of application and direct patient relevance. When dealing with an injured patient, returning to the pre-injury functional level should be the goal. Using a single assessment numeric evaluation (SANE) of current function relative to prior function quickly summarizes patient functional status and correlates with other established PROs.[29] The GRS can be framed to include activities of daily living and/or sports activities, encompassing multiple aspects of function. The two subscales of the KOS were most commonly identified as important measures of successful outcome one and two years after ACL injury or reconstruction, representing a global appreciation for patient function. Using the GRS and both subscales of the KOS analyzes function comprehensively from the patient perspective, supporting our hypothesis that PROs encompassing multiple aspects of function would be identified as important measures of successful outcome after ACL injury and reconstruction.
The IKDC2000 is similar to the two KOS subscales. It was developed with consideration of these measures and asks questions concerning activities of daily living and sport function.[30] The IKDC2000 also has a question that asks the patient to rate knee function currently and prior to knee injury, similar to the GRS. The IKDC2000 is a valid and reliable measure of symptoms, daily function and sports activities, making it a robust measure of multiple aspects of function for comparison,[30] addressing many of the symptoms and patient-reported responses identified by Kocher as being predictive of poor satisfaction, including pain, stiffness, swelling, instability, sport and ADL function, and overall rating of knee joint function.[9] This measure was not as frequently identified as being an important measure of successful outcome one and two years after ACL injury or reconstruction, and a relatively high percentage of respondents were unfamiliar with it. Regardless, the IKDC2000 combines the aspects of the three PROs most commonly identified as important into one questionnaire, simplifying the process.
As an alternative to the IKDC2000, the Knee Injury and Osteoarthritis Outcome Score (KOOS) also addresses daily function, symptoms, pain, and sports participation. The KOOS has a quality of life subscale, which adds more information to the assessment of the patient’s perspective. The KOOS is used in knee ligament registries and was the primary outcome measure in a randomized controlled trial of operative and non-operative management of ACL injuries.[27,31]
A median score of 90% was identified as a threshold to identify successful outcome after both ACL injury and reconstruction for the GRS, two subscales of the KOS and the IKDC2000. A median score of 85% was identified as the threshold to identify success for the KOOS. The IKDC2000 has the added benefit of having a normative data set to which patients can be compared.[32] This is an important distinction because most of the rating scales that are currently used have no well-defined score to identify success from failure or to stratify results. The comprehensive yet concise nature of the IKDC2000 with a normative database to compare patients lead the authors to promote the use of the IKDC2000 to measure function after ACL injury or reconstruction.
The Tegner Activity Scale and Marx Activity Rating Scale provide different analyses of patient function after injury or reconstruction than the other PROs in this analysis. The Tegner Activity Scale and Marx Activity Rating Scale both classify patients according to their sport or leisure time participation, as opposed to the patient’s self-reported perception of knee function. The Tegner Activity Scale provides an arbitrary ranking based on the level of sport and leisure time activities and/or competition at which the individual is currently participating.[33] The Marx Activity Rating Scale quantifies the frequency of activities that challenge the dynamic stability of the knee over the past year.[33] Both of these measures were frequently identified as an unimportant measure of successful outcome one and two years after ACL injury or reconstruction, and many respondents were unfamiliar with them. No other PRO included in this analysis adequately measures activity level, which was identified as an important measure of successful outcome after ACL injury or reconstruction.
Quadriceps strength was identified as an important measure of successful outcome one and two years after ACL injury or reconstruction, likely due to its relationship with future self-reported function and significant for long term outcome.[13,15,34] Many factors contribute to quadriceps strength deficits after ACL injury or reconstruction. Arthrogenic muscle inhibition, where joint changes result in an inability to volitionally activate the quadriceps, reduces functional strength.[35,36] Inadequate rehabilitation of the quadriceps before surgery compounds the deficits seen after reconstruction.[13] Pre-operative strength deficits can be compounded by the choice of a patellar tendon graft source. This graft harvest can result in anterior knee pain and decreased quadriceps strength, especially in the short-term follow-up in consideration. Because strength deficits can persist after injury [37-39] and do not resolve without significant intervention[40], the measurement of quadriceps strength is an important measure of successful outcome one and two years after ACL injury or reconstruction.
Hamstrings strength was also identified as an important measure of successful outcome one and two years after ACL injury or reconstruction. While quadriceps strength is predictive of future function, hamstring strength does not seem to be predictive of future function. Even when the hamstrings are used as a graft source for reconstruction, hamstrings strength recovers by 1 year [41,42] although deficits are seen in some populations.[43] Contrary to reports of no statistically significant relationship between hamstrings strength and function, this was identified as an important measure of successful outcome one and two years after ACL injury and reconstruction.
Measures of joint effusion are used as clinical surrogate measurements for joint inflammation.[5,44] Effusion measured by clinicians may not be considered important in determining success, as a measure of effusion validated against the gold standard of joint aspiration has not been established. However, measures of effusion that have acceptable face validity and good interrater reliability are available.[5] If the demand placed on the knee joint is too great for the joint to handle, inflammation and effusion may increase, indicating a joint incapable of current functional demands.[45] Effusion may be expected for a few months after injury or reconstruction, but at the one and two year time frames, an effused joint is considered a negative outcome. Increased effusion, like poor quadriceps strength, can affect knee joint kinematics affecting participation in sports[46,47] and can indirectly contribute to joint degeneration.
Outcome Criteria Not Achieving Consensus
Functional performance tests did not reach consensus levels as important measures of successful outcome one and two years after ACL injury or reconstruction. Functional tests are designed to test balance or mimic the demands of on field performance such as jumping, cutting, pivoting, landing, and running and are typically used to identify poor performance which would preclude patients from returning to sport.[48-50]. The tests give the clinician a standardized method of evaluating performance of each athlete and benchmarking against normative data or their own clinical experiences, and are recommended as criteria that should be used for returning patients to sport.[51] Quality and symmetry of movement and measureable performance between injured and uninjured limbs allow for consistent comparisons. Various methods have been described in the literature and used to test patients after an array of injuries. These tests are typically quick, and require little extra equipment to perform, making them ideally suited for clinical evaluation Even though these tests allow for quantification of performance in the clinic, their utility is not supported by a consensus rating.
Measures of passive knee laxity were not identified as being important measure of successful outcome one and two years after ACL injury or reconstruction. Laxity measures confirm the integrity of the graft and the amount of rotational laxity within the reconstructed knee joint. A positive pivot-shift test after reconstruction may be indicative of future joint degeneration.[9,14] However, the amount of laxity does not relate to functional performance after injury [14,52,53], bringing into question why these measures are still used in the literature and clinical practice as important measures of successful outcome after ACL injury. After reconstruction, these tests can be used to determine the patency of the graft and the extent to which the graft is able to control motion, however these results do not relate to function.
Measures of osteoarthritis were not identified as important measures of successful outcome one or two years after ACL injury or reconstruction. Degeneration is not likely seen at one and two years post injury as these changes take longer to develop. Between 0% and 13% of isolated ACL injured subjects have shown knee osteoarthritis more than 10 years after injury[54], indicating that the number of patients with measurable joint degeneration by conventional radiograph at one or two years after injury is likely very small. The prevention of osteoarthritis is a key factor in many interventions after ACL injury, however it is not an important determinant of a successful outcome one or two years after injury or reconstruction.
The Influence of Evidence on Practice
These results indicate that the available evidence does not impact clinical opinion in all cases. Despite a lack of published evidence linking hamstrings strength to functional performance after ACL injury and reconstruction, it was still identified as an important measure of successful outcome one and two years after ACL injury and reconstruction by more than 80% of respondents. Similarly, the well-established, valid, and reliable patient reported outcomes that are used to measure function in the literature that is meant to shape practice were frequently identified as not important or were unfamiliar to the respondents. These gaps need to be continually addressed in the educational programs and continued training of clinicians.
Limitations
Calculation of true response rates is not possible due to distribution methods. However, over 10% of members of AOSSM, ESSKA, and SPTS responded. Each organization distributed a link to the survey to their own membership, not allowing for the investigators to track how many surveys were distributed and how many were returned. The large, well distributed sample (over 1700 responses) of different professions provides a representative sample for this analysis. A representative composite score was calculated to account for all respondents who had an opinion on the value of a measure, including those who did not find a measure to be important. The outcomes in this survey are frequently reported in the literature concerning ACL injury and reconstruction, thus they are mostly familiar to the clinicians polled. For this reason, the respondents who had a negative opinion of a measure were included in the calculation to mitigate the familiarity of the measures. Similarly, the authors removed the bias of those individuals unfamiliar with each measure from influencing the final composite score.
CONCLUSION
The respondents met consensus definitions for six measures of knee function important for successful outcome one and two years after ACL injury or reconstruction, representing all levels of the International Classification of Functioning: absence of knee joint effusion, absence of knee joint giving way, symmetrical quadriceps and hamstrings muscle strength (body structure and function), patient reported outcomes with clearly defined thresholds for success (activity and participation), and return to sport (participation). Each of these, with the exception of hamstrings strength, is strongly supported by evidence. No individual patient reported outcome was identified by a consensus, although measures which take into account function in sports and activities of daily living were most frequently nominated. The Marx Activity Rating Scale clearly represents the participation level of patients in activities which challenge the ACL, but the results of this study do not clearly indicate that more clinicians use the Marx compared to the Tegner Activity Scale to measure activity level. These comprehensive measures should be included in clinical practice and research to allow for comparison between patients and interventions and across countries.
Supplementary Material
What are the new findings?
Five measures supported by empirical evidence were identified as important to identify successful outcomes one and two years after ACL injury or reconstruction: the absence of giving way, patient return to sport status, the absence of knee joint effusion, quadriceps muscle strength symmetry, and patient reported outcomes. Hamstrings muscle strength symmetry was also identified as an important measure of successful outcome one and two years after ACL injury or reconstruction despite a lack of empirical evidence relating hamstrings strength with functional outcome.
Despite being identified as an important measure of successful outcome by a consensus of respondents, no individual patient reported outcome was identified as important by a consensus of respondents.
Measures of ligament laxity and osteoarthritis were not identified as important measures of successful outcome one or two years after ACL injury or reconstruction.
How might it impact on clinical practice in the near future?
A standard set of criteria identified by a consensus of clinicians and experts in the field were established as a possible reference standard for comparing results.
Cutoff scores for functional patient reported outcomes were established between 85 and 90%, providing a goal for clinical practice.
Less attention should be placed on standard measurements of laxity in determining the outcome of an anterior cruciate ligament rupture.
Acknowledgments
We would like to thank the organizations that facilitated our data collection by distributing the survey to their membership: the Sports Physical Therapy Section of the American Physical Therapy Association, the European Society for Sports Traumatology, Surgery and Knee Arthroscopy, the American Orthopaedic Society for Sports Medicine, the Italian Manual Therapy Group, the Portuguese Sports Physiotherapy Group, the Irish Society of Chartered Physiotherapists, the Association of Turkish Sports Physiotherapists, the Swiss Sports Physiotherapy Association, the Italian Sport Specialist Group, the Association of Chartered Physiotherapists in Sports Medicine, the Norwegian Manual Therapy Association, and the Journal of Orthopaedic & Sports Physical Therapy.
Funding
This work was funded by a grant from the United States National Institutes of Health (NIH R01 HD37985).
This work was funded by a grant from the United States National Institutes of Health (HD R01 37985). The USNIH had no role in any aspect of this study.
Footnotes
Competing Interests
The authors declare no competing interests which influenced the performance of this research.
The authors declare no competing interests in the completion or publication of this work
Contributor Information
Andrew D. Lynch, University of Pittsburgh, School of Medicine, Department of Orthopaedic Surgery, Division of Sports Medicine; and UPMC Center for Sports Medicine; Pittsburgh, PA, USA.
David S. Logerstedt, Department of Physical Therapy, University of Delaware; Newark, DE, USA.
Hege Grindem, Norwegian Research Center for Active Rehabilitation and Norwegian School of Sports Sciences; Oslo, Norway.
Ingrid Eitzen, Norwegian Research Center for Active Rehabilitation; Oslo, Norway.
Gregory E. Hicks, Department of Physical Therapy, University of Delaware; Newark, DE, USA.
Michael J. Axe, First State Orthopaedics; Newark, DE, USA.
Lars Engebretsen, Oslo University Hospital; Oslo, Norway.
May Arna Risberg, Norwegian Research Center for Active Rehabilitation; Oslo, Norway.
Lynn Snyder-Mackler, Department of Physical Therapy, University of Delaware; Newark, DE, USA.
REFERENCES
- 1.Irrgang JJ, Snyder-Mackler L, Wainner RS, et al. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80(8):1132–45. doi: 10.2106/00004623-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Logerstedt DS, Snyder-Mackler L, Ritter RC, et al. Knee stability and movement coordination impairments: knee ligament sprain. J Orthop Sports Phys Ther. 40(4):A1–A37. doi: 10.2519/jospt.2010.0303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katz JW, Fingeroth RJ. The diagnostic accuracy of ruptures of the anterior cruciate ligament comparing the Lachman test, the anterior drawer sign, and the pivot shift test in acute and chronic knee injuries. Am J Sports Med. 1986;14(1):88–91. doi: 10.1177/036354658601400115. [DOI] [PubMed] [Google Scholar]
- 4.Benjaminse A, Gokeler A, van der Schans CP. Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis. J Orthop Sports Phys Ther. 2006;36(5):267–88. doi: 10.2519/jospt.2006.2011. [DOI] [PubMed] [Google Scholar]
- 5.Sturgill LP, Snyder-Mackler L, Manal TJ, et al. Interrater reliability of a clinical scale to assess knee joint effusion. J Orthop Sports Phys Ther. 2009;39(12):845–9. doi: 10.2519/jospt.2009.3143. [DOI] [PubMed] [Google Scholar]
- 6.Lysholm J, Tegner Y. Knee injury rating scales. Acta Orthop. 2007;78(4):445–53. doi: 10.1080/17453670710014068. [DOI] [PubMed] [Google Scholar]
- 7.Marx RG. Knee rating scales. Arthroscopy. 2003;19(10):1103–8. doi: 10.1016/j.arthro.2003.10.029. [DOI] [PubMed] [Google Scholar]
- 8.Pantano KJ, Irrgang JJ, Burdett R, et al. A pilot study on the relationship between physical impairment and activity restriction in persons with anterior cruciate ligament reconstruction at long-term follow-up. Knee Surg Sports Traumatol Arthrosc. 2001;9(6):369–78. doi: 10.1007/s001670100239. [DOI] [PubMed] [Google Scholar]
- 9.Kocher MS, Steadman JR, Briggs K, et al. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2002;84-A(9):1560–72. doi: 10.2106/00004623-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Marx RG, Jones EC, Allen AA, et al. Reliability, validity, and responsiveness of four knee outcome scales for athletic patients. J Bone Joint Surg Am. 2001;83-A(10):1459–69. doi: 10.2106/00004623-200110000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Eitzen I, Moksnes H, Snyder-Mackler L, et al. Functional tests should be accentuated more in the decision for ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1517–25. doi: 10.1007/s00167-010-1113-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Branch TP, Siebold R, Freedberg HI, et al. Double-bundle ACL reconstruction demonstrated superior clinical stability to single-bundle ACL reconstruction: a matched-pairs analysis of instrumented tests of tibial anterior translation and internal rotation laxity. Knee Surg Sports Traumatol Arthrosc. 2011;19(3):432–40. doi: 10.1007/s00167-010-1247-5. [DOI] [PubMed] [Google Scholar]
- 13.Eitzen I, Holm I, Risberg MA. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med. 2009;43(5):371–6. doi: 10.1136/bjsm.2008.057059. [DOI] [PubMed] [Google Scholar]
- 14.Kocher MS, Steadman JR, Briggs KK, et al. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(3):629–34. doi: 10.1177/0363546503261722. [DOI] [PubMed] [Google Scholar]
- 15.Logerstedt D, Lynch A, Axe MJ, et al. Pre-operative quadriceps strength predicts IKDC2000 scores 6months after anterior cruciate ligament reconstruction. Knee. 2012 doi: 10.1016/j.knee.2012.07.011. doi: S0968-0160(12)00135-4 [pii] 10.1016/j.knee.2012.07.011[published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weitzel PP, Richmond JC, Altman GH, et al. Future direction of the treatment of ACL ruptures. Orthop Clin North Am. 2002;33(4):653–61. doi: 10.1016/s0030-5898(02)00017-2. [DOI] [PubMed] [Google Scholar]
- 17.Marx RG, Jones EC, Angel M, et al. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy. 2003;19(7):762–70. doi: 10.1016/s0749-8063(03)00398-0. [DOI] [PubMed] [Google Scholar]
- 18.Finsterbush A, Frankl U, Matan Y, et al. Secondary damage to the knee after isolated injury of the anterior cruciate ligament. Am J Sports Med. 1990;18(5):475–9. doi: 10.1177/036354659001800505. [DOI] [PubMed] [Google Scholar]
- 19.Hawkins RJ, Misamore GW, Merritt TR. Followup of the acute nonoperated isolated anterior cruciate ligament tear. Am J Sports Med. 1986;14(3):205–10. doi: 10.1177/036354658601400305. [DOI] [PubMed] [Google Scholar]
- 20.Lohmander LS, Englund PM, Dahl LL, et al. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35(10):1756–69. doi: 10.1177/0363546507307396. [DOI] [PubMed] [Google Scholar]
- 21.Swirtun LR, Renstrom P. Factors affecting outcome after anterior cruciate ligament injury: a prospective study with a six-year follow-up. Scand J Med Sci Sports. 2008;18(3):318–24. doi: 10.1111/j.1600-0838.2007.00696.x. [DOI] [PubMed] [Google Scholar]
- 22.Jonsson H, Riklund-Ahlstrom K, Lind J. Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5-9 years after surgery. Acta Orthop Scand. 2004;75(5):594–9. doi: 10.1080/00016470410001484. [DOI] [PubMed] [Google Scholar]
- 23.Ardern CL, Taylor NF, Feller JA, et al. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40(1):41–48. doi: 10.1177/0363546511422999. [DOI] [PubMed] [Google Scholar]
- 24.Ardern CL, Webster KE, Taylor NF, et al. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606. doi: 10.1136/bjsm.2010.076364. [DOI] [PubMed] [Google Scholar]
- 25.Ardern CL, Webster KE, Taylor NF, et al. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011;39(3):538–43. doi: 10.1177/0363546510384798. [DOI] [PubMed] [Google Scholar]
- 26.Spindler KP, Huston LJ, Wright RW, et al. The prognosis and predictors of sports function and activity at minimum 6 years after anterior cruciate ligament reconstruction: a population cohort study. Am J Sports Med. 2011;39(2):348–59. doi: 10.1177/0363546510383481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Granan LP, Bahr R, Steindal K, et al. Development of a national cruciate ligament surgery registry: the Norwegian National Knee Ligament Registry. Am J Sports Med. 2008;36(2):308–15. doi: 10.1177/0363546507308939. [DOI] [PubMed] [Google Scholar]
- 28.Dunn WR, Spindler KP. Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010;38(10):2040–50. doi: 10.1177/0363546510370280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shelbourne KD, Barnes AF, Gray T. Correlation of a Single Assessment Numeric Evaluation (SANE) Rating With Modified Cincinnati Knee Rating System and IKDC Subjective Total Scores for Patients After ACL Reconstruction or Knee Arthroscopy. Am J Sports Med. 2012;40(11):2487–91. doi: 10.1177/0363546512458576. doi: 10.1177/0363546512458576 0363546512458576 [pii][published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 30.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29(5):600–13. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 31.Frobell RB, Roos EM, Roos HP, et al. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363(4):331–42. doi: 10.1056/NEJMoa0907797. doi: 363/4/331 [pii] 10.1056/NEJMoa0907797[published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 32.Anderson AF, Irrgang JJ, Kocher MS, et al. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med. 2006;34(1):128–35. doi: 10.1177/0363546505280214. [DOI] [PubMed] [Google Scholar]
- 33.Marx RG, Stump TJ, Jones EC, et al. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213–8. doi: 10.1177/03635465010290021601. [DOI] [PubMed] [Google Scholar]
- 34.Snyder-Mackler L, Delitto A, Bailey SL, et al. Strength of the quadriceps femoris muscle and functional recovery after reconstruction of the anterior cruciate ligament. A prospective, randomized clinical trial of electrical stimulation. J Bone Joint Surg Am. 1995;77(8):1166–73. doi: 10.2106/00004623-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Snyder-Mackler L, Delitto A, Stralka SW, et al. Use of electrical stimulation to enhance recovery of quadriceps femoris muscle force production in patients following anterior cruciate ligament reconstruction. Phys Ther. 1994;74(10):901–7. doi: 10.1093/ptj/74.10.901. [DOI] [PubMed] [Google Scholar]
- 36.Rice DA, McNair PJ. Quadriceps arthrogenic muscle inhibition: neural mechanisms and treatment perspectives. Semin Arthritis Rheum. 2010;40(3):250–66. doi: 10.1016/j.semarthrit.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 37.Risberg MA, Holm I, Tjomsland O, et al. Prospective study of changes in impairments and disabilities after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1999;29(7):400–12. doi: 10.2519/jospt.1999.29.7.400. [DOI] [PubMed] [Google Scholar]
- 38.Ageberg E, Roos HP, Silbernagel KG, et al. Knee extension and flexion muscle power after anterior cruciate ligament reconstruction with patellar tendon graft or hamstring tendons graft: a cross-sectional comparison 3 years post surgery. Knee Surg Sports Traumatol Arthrosc. 2009;17(2):162–9. doi: 10.1007/s00167-008-0645-4. [DOI] [PubMed] [Google Scholar]
- 39.Ageberg E, Thomee R, Neeter C, et al. Muscle strength and functional performance in patients with anterior cruciate ligament injury treated with training and surgical reconstruction or training only: a two to five-year followup. Arthritis Rheum. 2008;59(12):1773–9. doi: 10.1002/art.24066. [DOI] [PubMed] [Google Scholar]
- 40.Logerstedt D, Lynch A, Axe MJ, et al. Symmetry restoration and functional recovery before and after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012 doi: 10.1007/s00167-012-1929-2. doi: 10.1007/s00167-012-1929-2[published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ardern CL, Webster KE. Knee flexor strength recovery following hamstring tendon harvest for anterior cruciate ligament reconstruction: a systematic review. Orthop Rev (Pavia) 2009;1(2):e12. doi: 10.4081/or.2009.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ardern CL, Webster KE, Taylor NF, et al. Hamstring strength recovery after hamstring tendon harvest for anterior cruciate ligament reconstruction: a comparison between graft types. Arthroscopy. 26(4):462–9. doi: 10.1016/j.arthro.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 43.Heijne A, Werner S. A 2-year follow-up of rehabilitation after ACL reconstruction using patellar tendon or hamstring tendon grafts: a prospective randomised outcome study. Knee Surg Sports Traumatol Arthrosc. 2010;18(6):805–13. doi: 10.1007/s00167-009-0961-3. [DOI] [PubMed] [Google Scholar]
- 44.Trees AH, Howe TE, Dixon J, et al. Exercise for treating isolated anterior cruciate ligament injuries in adults. Cochrane Database Syst Rev. 2005;(4):CD005316. doi: 10.1002/14651858.CD005316.pub2. [DOI] [PubMed] [Google Scholar]
- 45.Dye SF, Wojtys EM, Fu FH, et al. Factors contributing to function of the knee joint after injury or reconstruction of the anterior cruciate ligament. Instr Course Lect. 1999;48:185–98. [PubMed] [Google Scholar]
- 46.Coughlan GF, McLoughlin R, McCarthy Persson U, et al. An investigation into the effects of a simulated effusion in healthy subjects on knee kinematics during jogging and running. Clin Biomech (Bristol, Avon) 2008;23(8):1038–43. doi: 10.1016/j.clinbiomech.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 47.Palmieri-Smith RM, Kreinbrink J, Ashton-Miller JA, et al. Quadriceps inhibition induced by an experimental knee joint effusion affects knee joint mechanics during a single-legged drop landing. Am J Sports Med. 2007;35(8):1269–75. doi: 10.1177/0363546506296417. [DOI] [PubMed] [Google Scholar]
- 48.Risberg MA, Ekeland A. Assessment of functional tests after anterior cruciate ligament surgery. J Orthop Sports Phys Ther. 1994;19(4):212–7. doi: 10.2519/jospt.1994.19.4.212. [DOI] [PubMed] [Google Scholar]
- 49.Grindem H, Logerstedt D, Eitzen I, et al. Single-legged hop tests as predictors of self-reported knee function in nonoperatively treated individuals with anterior cruciate ligament injury. Am J Sports Med. 2011;39(11):2347–54. doi: 10.1177/0363546511417085. doi: 0363546511417085 [pii] 10.1177/0363546511417085[published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Logerstedt D, Grindem H, Lynch A, et al. Single-Legged Hop Tests as Predictors of Self-Reported Knee Function After Anterior Cruciate Ligament Reconstruction: The Delaware-Oslo ACL Cohort Study. Am J Sports Med. 2012;40(10):2348–56. doi: 10.1177/0363546512457551. doi: 0363546512457551 [pii] 10.1177/0363546512457551[published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Thomee R, Kaplan Y, Kvist J, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(11):1798–805. doi: 10.1007/s00167-011-1669-8. doi: 10.1007/s00167-011-1669-8[published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 52.Snyder-Mackler L, Fitzgerald GK, Bartolozzi AR, 3rd, et al. The relationship between passive joint laxity and functional outcome after anterior cruciate ligament injury. Am J Sports Med. 1997;25(2):191–5. doi: 10.1177/036354659702500209. [DOI] [PubMed] [Google Scholar]
- 53.Hurd WJ, Axe MJ, Snyder-Mackler L. A 10-year prospective trial of a patient management algorithm and screening examination for highly active individuals with anterior cruciate ligament injury: Part 2, determinants of dynamic knee stability. Am J Sports Med. 2008;36(1):48–56. doi: 10.1177/0363546507308191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Oiestad BE, Engebretsen L, Storheim K, et al. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37(7):1434–43. doi: 10.1177/0363546509338827. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.