Abstract
Study Objectives:
Many cognitive factors contribute to unintentional pedestrian injury, including reaction time, impulsivity, risk-taking, attention, and decision-making. These same factors are negatively influenced by excessive daytime sleepiness (EDS), which may place children with EDS at greater risk for pedestrian injury.
Design, Participants, and Methods:
Using a case-control design, 33 children age 8 to 16 y with EDS from an established diagnosis of narcolepsy or idiopathic hypersomnia (IHS) engaged in a virtual reality pedestrian environment while unmedicated. Thirty-three healthy children matched by age, race, sex, and household income served as controls.
Results:
Children with EDS were riskier pedestrians than healthy children. They were twice as likely to be struck by a virtual vehicle in the virtual pedestrian environment than healthy controls. Attentional skills of looking at oncoming traffic were not impaired among children with EDS, but decision-making for when to cross the street safely was significantly impaired.
Conclusions:
Results suggest excessive daytime sleepiness (EDS) from the clinical sleep disorders known as the hypersomnias of central origin may have significant consequences on children's daytime functioning in a critical domain of personal safety, pedestrian skills. Cognitive processes involved in safe pedestrian crossings may be impaired in children with EDS. In the pedestrian simulation, children with EDS appeared to show a pattern consistent with inattentional blindness, in that they “looked but did not process” information in their pedestrian environment. Results highlight the need for heightened awareness of potentially irreversible consequences of untreated sleep disorders and identify a possible target for pediatric injury prevention.
Citation:
Avis KT; Gamble KL; Schwebel DC. Does excessive daytime sleepiness affect children's pedestrian safety? SLEEP 2014;37(2):283-287.
Keywords: Children, daytime sleepiness, hypersomnia, injury risk, narcolepsy, pedestrian safety
INTRODUCTION
Annually, 5,300 American pedestrians are killed and 85,000 others are injured; more than one-third of injured pedestrians are children.1 In middle childhood, approximately 60% of pedestrian injuries and mortalities occur when the child is crossing a road at or between intersections, typically within a half-mile of the child's home.2–4 Several studies suggest young children regularly negotiate dangerous street environments alone when going to and from school.2,5–7 Not surprisingly, prevention of pediatric pedestrian injury has been targeted as a national public health priority.8
Many factors contribute to unintentional pedestrian injury. Among them are cognitive and temperamental traits of the pedestrian, including reaction time, impulsivity, risk-taking, attention, and decision-making.9–12 These same characteristics that influence pedestrian safety are negatively influenced by excessive daytime sleepiness (EDS). Although EDS can result from sleep deprivation among healthy children, it is the hallmark symptom of a category of sleep disorders known as hypersomnias of central origin. Hypersomnias include narcolepsy and idiopathic hypersomnia (IHS), both of which are characterized by pathologic levels of EDS despite obtaining sufficient amounts of sleep of good quality. Patients with hypersomnia have a primary, chronic complaint of EDS, defined as the inability to stay awake and alert during the day, with unintended lapses into sleep that are not due to disturbed nocturnal sleep, insufficient sleep time, or misaligned circadian rhythms.13 Because this article focused on EDS as a result of narcolepsy or IHS, EDS refers to sleepiness from those disorders for the remainder of this article.
Among adult populations, the presence of EDS puts individuals at high risk for human error, mental inefficiency, and significant injury.14–19 Individuals with EDS are likely to behave impulsively and inattentively, make poor decisions, have slow reaction times, and take risks.16 Adults with untreated narcolepsy are more likely to have daytime sleepiness resulting in motor vehicle crashes.20
Most pediatric research has focused on the daytime consequences of sleep deprivation from insufficient sleep time in healthy children or in children with obstructive sleep apnea syndrome.21–23 A few studies document impaired attentional and learning skills, poor quality of life, and impaired social skills in children with EDS.24–26 However, the daytime consequences of pathologic EDS in children are poorly understood, especially in relation to the effects on applied outcomes such as injury risk.
This study examined whether children with EDS take greater risks in pedestrian settings compared to matched agemates without EDS. We hypothesized that children with EDS would have a greater number of hits or close calls with vehicles while crossing the street in a virtual pedestrian environment. We further hypothesized that these dangerous pedestrian situations would be explained by the facts that children with EDS would have (1) lower average attention to traffic while crossing a virtual road and (2) greater temporal delays before entering a safe traffic gap to cross within. We tested these hypotheses using a case-control research design. Children with EDS were tested while off wake-promoting medications and were matched to controls by age, race, sex, and household income.
METHODS
Participants and Recruitment
Sixty-six children participated in the study (see Table 1 for demographic characteristics). In 33 children, EDS was diagnosed. Diagnosis and recruitment occurred at the Pediatric Sleep Disorders Center at Children's of Alabama. Children met International Classification of Sleep Disorders, Second Edition (ICSD-2) diagnostic criteria for a hypersomnia of central origin (narcolepsy with or without cataplexy, or idiopathic hypersomnia) based on diagnostic assessments that included overnight polysomnography followed by multiple sleep latency tests the following day, drug screening, and thorough clinical evaluation from two attending board-certified sleep specialists. In all children with EDS, the diagnosis was made within 3 y of the study date and wake-promoting medication (modafinil) was prescribed. Exclusion criteria were minimal and included cognitive or physical disabilities that prevented full participation in the experimental protocol (e.g., mental retardation, blindness, use of a wheelchair); comorbid medical or neurologic conditions; or antipsychotic medication use. Only one child was excluded, based on recent diagnosis of traumatic brain injury. To verify diagnosis of sleepiness, we sampled level of sleepiness as measured by Epworth Sleepiness Scale-modified for children.21 Children with EDS were clinically sleepy (mean = 12.33, standard deviation [SD] = 5.65).
Table 1.
Demographic characteristics of children with EDS and controls
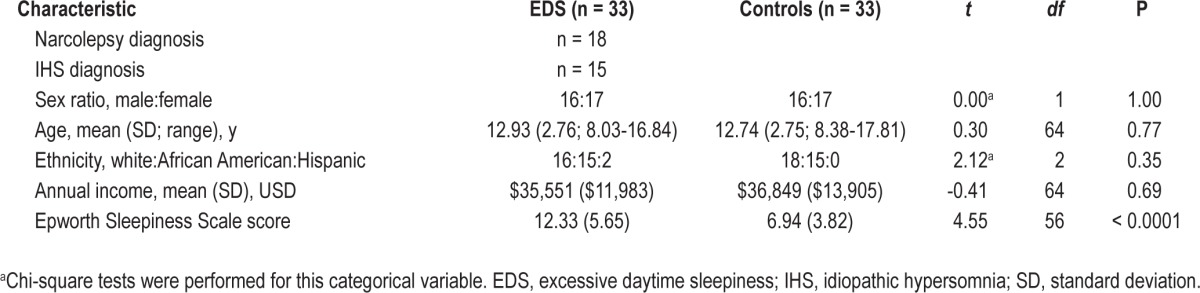
Thirty-three healthy children were recruited from the community using a laboratory database of community residents interested in participating in research. The same exclusion criteria used in the case sample were applied; no children were excluded. The samples were matched by age, sex, race, and average income in the ZIP code of residence. Thus, demographic characteristics of this control sample of healthy children were quite similar to those in the sample of children with EDS (Table 1). The control sample was adequately alert with a mean Epworth Sleepiness Scale score of 6.94 (SD = 3.82).
The study protocol was approved by the Institutional Review Board at the University of Alabama at Birmingham. Informed consent was obtained from participants' parents or legal guardians, and informed assent from participants. Families were compensated for their time.
Protocol
Prior to the visit, caregivers of children with EDS refrained from giving children their prescribed wake-promoting medication (modafinil) for 3 days prior to the research appointment and for the morning of the appointment. This timeline was based on the half-life of the medication. Caregivers were asked to continue administering medication for cataplexy if prescribed. Caregivers of children in both samples prohibited caffeine intake for children the morning of the research appointment and were instructed to keep children awake after their routine wake time and during the drive to the appointment. All sessions were conducted within a 3-h time weekday morning time window.
Once the family arrived at for the appointment and consent processes were completed, children participated in the virtual reality pedestrian environment while the parent completed demographic questionnaires. The research session lasted approximately 1 h.
Virtual Reality Pedestrian Environment
Details of the virtual reality pedestrian environment (VRPE), including validation data demonstrating behavior in the virtual world that corresponds with behavior in real pedestrian environments, are available elsewhere.10 Briefly, children stand on a wooden simulated curb while viewing the virtual pedestrian environment on three consecutive monitors arranged in a semicircle in front of the child (Figure 1). The child is immersed in the virtual environment as they watch vehicles pass bidirectionally on the screen and hear environmental and traffic noise through speakers in the room. After deciding it is safe to cross, the child steps off of the curb onto a pressure plate connected to the computer and a sex-matched avatar is then activated to cross the street. The avatar's walking speed in the VRPE is matched to the child's walking speed, which is evaluated prior to the VRPE task in a separate location. If the avatar safely reaches the other side, the child hears one of two positive messages such as “Yes! Great job!” If the child makes it across safely but was close to being hit by a car, the child hears, “Whoa! That was close!” If the child is struck by one of the cars, they hear, “Uh oh, you should try that again!” Thus, the child is immersed into a virtual world while deciding when it is safe to cross. After choosing to cross, the world becomes third-person, and the child witnesses the safety (or danger) of the crossing.
Figure 1.

Screenshot of virtual reality pedestrian environment.
During the experimental visit, children performed 10 practice trials to reduce learning effects and then engaged in 12 virtual street crossings. Behavior in the 12 crossings was used for analysis.
Pedestrian Safety Measures
We considered three outcome measures based on behavior in the VRPE. First, we looked at simulated injury, assessed via hits or close calls while crossing. We also considered three risk factors involved in street crossings that may be influenced by fatigue, attention to traffic, and decision-making. (1) Simulated injury (collisions/near-collisions with virtual vehicles): The sum of hits and close calls assessed pedestrian injury risk. Hits were any direct collisions between the virtual pedestrian and a vehicle. Close calls were instances when the pedestrian was within 1 sec of being struck by a virtual vehicle. (2) Attention to traffic: To evaluate attention to traffic, looks toward traffic were tallied by head-tracking equipment (Trackir4:Pro, NaturalPoint Inc, Corvallis, OR) that monitored participants' visual attention to traffic from the left and right, a critical aspect of safe pedestrian behavior. We summed the number of times participants looked left plus the number of times they looked right while waiting to cross, divided by the average wait time in sec. (3) Decision-making: To assess the cognitive decision-making aspects of pedestrian safety, we considered average latency to start crossing. This value was computed as the time, in millisec, between the traffic gap the child chose to cross within emerging and the child initiating movement into that gap. Prior research suggests this measure may represent the pedestrian's skill and speed of cognitive processing and decision-making before initiating street-crossing.27,28
RESULTS
Descriptive statistics were considered first (Table 1). As expected based on recruitment of matched samples, the two groups were very similar in terms of age, race, sex, and household income.
The primary hypothesis was that children with EDS would have higher risk of pedestrian injury than the matched group of healthy control children. A Poisson regression analysis, with hits/close calls as the dependent variable and group as the independent variable, was statistically significant, Wald χ2 = 6.45 (P < 0.05). The number of hits/close calls for children with EDS (mean = 1.22, SD = 1.26) was twice that of controls (mean = 0.61, SD = 0.79); odds ratio = 2.01, 95% confidence interval = 1.17-3.45. In addition, 60.6% of children with EDS were hit by a virtual vehicle compared to 39.4% of children in the control group. Thus, as seen in Figure 2, children with EDS were not only at higher risk of getting hit by a car, but also had greater percentages of multiple hits during the assessment in the VRPE.
Figure 2.
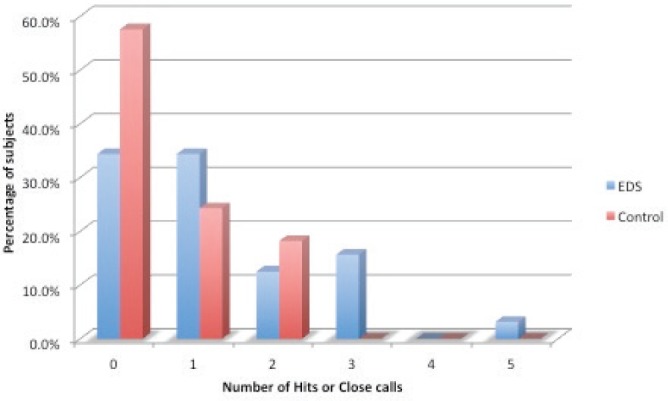
Percent of total sample with hits/close calls in virtual reality pedestrian environment. EDS, excessive daytime sleepiness.
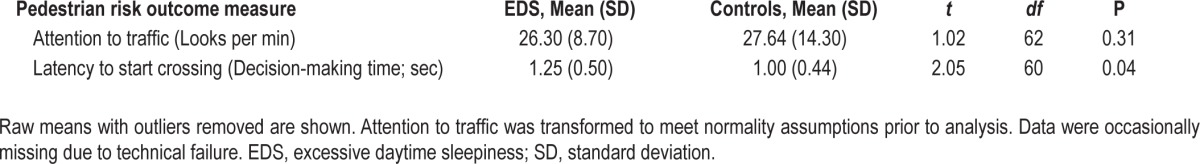
We next considered whether attention to traffic or slow decision-making might explain the increased incidence of virtual pedestrian injuries among children with EDS compared to the control group. Shapiro-Wilk tests suggested both the attention to traffic and the decision-making constructs were non-normal. Outliers were removed ± 2 SD from the mean, correcting the normality of decision-making after removing three outliers. For attention to traffic, one outlier was removed but the variable remained non-normal and was transformed using the square root of absolute value transformation. As detailed in Table 2, independent samples t-tests comparing the EDS versus control groups yielded significant differences on decision-making (EDS raw mean = 1.25, SD = 0.50; control mean = 1.00, SD = 0.44; t(60) = 2.05, P < 0.05; Cohen d = 0.53) but not attention to traffic (EDS raw mean = 26.30, SD = 8.70; control mean = 27.64; SD = 14.30; t(62) = 1.02, not significant; Cohen d = 0.11).
Table 2.
Independent samples t-tests between children with EDS and controls
DISCUSSION
Children with EDS were more likely to get hit or nearly hit by a virtual vehicle than a group of children matched by age, sex, race, and household income. This finding extends previous reports documenting the harmful effect of sleep deprivation on transportation safety of adults and adolescents.15–19 In particular, this study provides initial evidence to suggest that untreated EDS may be associated with increased injury risk to children in pedestrian settings, as children with EDS experienced collisions and near-collisions on over 10% of crossings in the virtual street environment, and at a rate twice that of matched controls.
When we investigated whether inattention to traffic, delayed decision-making, or both, might explain the higher rate of collisions with vehicles in the virtual pedestrian environment among children with EDS, we found decision-making time varied across groups but attention to traffic did not. Crossing streets safely requires simultaneous processing of several pieces of information, and previous research suggests young children are slower and less skilled at perceiving and processing those stimuli, and then deciding how to act compared to older children.29,30 Latency to enter a safe traffic gap is considered a proxy for ability and speed in perceiving, processing, and deciding how to act based on pedestrian environment stimuli.27,28 Children tend to make decisions more quickly when tasks are well within their ability, and require more time to determine the safety of tasks that are more ambiguous and just beyond their ability.30–32 Our results suggest that, as hypothesized, children with EDS might take longer to determine the safety of crossing ambiguous traffic gaps than children without EDS. Longer delays in determining whether to cross could jeopardize children's safety because they enter a safe traffic gap at a later time, thus creating a smaller traffic gap and less time before oncoming vehicles reach the crosswalk.
Future research should investigate exactly what factors may lead children with EDS to make slower and riskier decisions to enter traffic gaps while crossing a street. Decision-making is a complex, higher-order cognitive task that involves several subcomponents. It may be that just one primary subcomponent, such as reaction time, was deficient in the sample and led to slower decision-making processes. Reaction time is delayed in adults with sleep disorders such as narcolepsy.33,34 It may also be that other or multiple subcomponents of street-crossing are affected by side effects of EDS.
We did not find that attention to traffic was impaired among children with EDS. A possible explanation for this finding is that when sleepy, children are able to follow simple and rote rules such as looking both ways before crossing, but they may not fully process cognitively the complex environment they perceive. This possibility is consistent with the adult driving literature. In simulated adult driving research, drivers distracted with a cell phone scan the driving environment in front of them appropriately, but appear not to process the information they see fully or accurately, resulting in what is sometimes called inattentional blindness.35,36 For example, in one study drivers distracted by cell phone conversations processed up to 50% less information in their environment than nondistracted drivers. They were more likely to overlook traffic signals, took longer to react to detected traffic signals, and drove through red lights and stop signs at a higher rate.34 Distracted and sleepy drivers show similar behavior patterns.20,36
The current findings may have implications for both injury prevention and sleep medicine practice. Unintentional injuries are the leading cause of death in children younger than 18 y. Identifying risk factors for injury, such as sleep disorders, is an important early step to move toward development of prevention programs. In this particular case, we might consider two broad solutions: counseling about pedestrian injury risk by sleep professionals and increased community awareness to highlight the effect of sleepiness on children's pedestrian injury risk.
Frequent screenings for symptoms of sleep disorders and heightened awareness of the daytime consequences of sleepiness are needed. Hypersomnias of central origin often persist up to 10 y before proper diagnoses.37,38 Although up to half of patients retrospectively recall symptoms well before age 15 y, diagnosis is rarely made prior to this age.38 However, it appears that sleepy children may be at risk of injury—including pedestrian injury—well before they reach the age of driving. Injury risks from sleepiness should be discussed with any pediatric patient complaining of sleep problems. Community interventions may also reduce risk. Such interventions include road and traffic engineering to improve safety of children, including sleepy children, in street-crossing environments. Two possible interventions include safer walking zones near schools and increased supervision of children in pedestrian settings by parents and school officials.39,40
This study had limitations. First, pedestrian behavior is multifaceted. The virtual reality environment evaluates pedestrian behavior at a bidirectional midblock crossing. We did not investigate pedestrian behavior at signalized or one-way crossings, patterns of route selections when more than one crossing option is available, or perception of acceleration/deceleration in vehicles, for example. We also did not investigate lower-level underlying cognitive processes involved in pedestrian safety-making such as reaction time or visual perceptual skills. Pedestrian safety is a highly complex and multifaceted cognitive-perceptual task. Future research might continue to break down the larger process of crossing streets safely into subcomponents, evaluating how each subcomponent is influenced by disorders such as EDS. Further, because EDS diagnoses are rather rare, findings may be limited due to small sample size. Findings are limited to pedestrian injury, as we did not evaluate other injury risk situations. For example, the effect of EDS on playground behavior, sports injuries, and other potentially risky situations has not been tested carefully. Future research might also consider whether treatments aiming to attenuate or remedy sleepiness (such as wake-promoting medication) successfully reduce injury risk.
DISCLOSURE STATEMENT
This was not an industry supported study. The project described was supported in part by Award Number R01HD058573 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health & Human Development or the National Institutes of Health. This project was also supported by an award from the Kaul Pediatric Research Institute at the Children's of Alabama Foundation. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Anna Johnston, research coordinator for the UAB Safety Lab, for all of her of time and help in recruitment and carrying out the study. We would also like to acknowledge the students of the UAB Youth Safety Lab for their hours of data entry and participation. We would also like to thank Joan Severson and Digital Artefacts for creating and supporting the virtual reality pedestrian environment.
REFERENCES
- 1.National Center for Injury Prevention and Control [NCIPC] WISQARS™ (Web-based Injury Statistics Query and Reporting System) 2010. [Accessed July 19, 2013]. http://www.cdc.gov/ncipc/wisqars/
- 2.Agran PF, Winn DG, Anderson CL. Differences in child pedestrian injury events by location. Pediatrics. 1994;93:284–8. [PubMed] [Google Scholar]
- 3.DiMaggio C, Durkin M. Child pedestrian injury in an urban setting: descriptive epidemiology. Acad Emerg Med. 2002;9:54–62. doi: 10.1111/j.1553-2712.2002.tb01168.x. [DOI] [PubMed] [Google Scholar]
- 4.Lightstone AS, Dhillon PK, Peek-Asa C, Kraus JF. A geographic analysis of motor vehicle collisions with child pedestrians in Long Beach, California: comparing intersection and midblock incident locations. Inj Prev. 2001;7:155–60. doi: 10.1136/ip.7.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Macpherson A, Roberts I, Pless IB. Children's exposure to traffic and pedestrian injuries. Am J Public Health. 1998;88:1840–3. doi: 10.2105/ajph.88.12.1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martin SL, Lee SM, Lowry R. National prevalence and correlates of walking and bicycling to school. Am J Prev Med. 2007;33:98–105. doi: 10.1016/j.amepre.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 7.Rivara FP, Bergman AB, Drake C. Parental attitudes and practices toward children as pedestrians. Pediatrics. 1989;84:1017–21. [PubMed] [Google Scholar]
- 8.National Center for Injury Prevention and Control [NCIPC] WISQARS™ (Web-based Injury Statistics Query and Reporting System) 2002. [Accessed July 19, 2013]. http://www.cdc.gov/ncipc/wisqars/
- 9.Schwebel DC, Davis AL, O'Neal EE. Child pedestrian injury: A review of behavioral risks and preventive strategies. Am J Lifestyle Med. 2012;6:292–302. doi: 10.1177/0885066611404876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schwebel DC, Gaines J, Severson J. Validation of virtual reality as a tool to understand and prevent child pedestrian injury. Accid Anal Prev. 2008;40:1394–400. doi: 10.1016/j.aap.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 11.Schwebel DC, Barton BB. Contributions of multiple risk factors to child injury. J Pediatr Psychol. 2005;30:553–61. doi: 10.1093/jpepsy/jsi042. [DOI] [PubMed] [Google Scholar]
- 12.Thompson JA, Tolmie AK, Foot HC, Sarvary PA, Morrison S. Influence of virtual reality training on the roadside crossing judgements of child pedestrians. J Exp Psychol Appl. 2005;11:175–86. doi: 10.1037/1076-898X.11.3.175. [DOI] [PubMed] [Google Scholar]
- 13.American Academy of Sleep Medicine. International classification of sleep disorders. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005. Diagnostic and coding manual. [Google Scholar]
- 14.Dinges DF. Sleep deprivation and vigilant attention. Ann N Y Acad Sci. 2008;1129:305–22. doi: 10.1196/annals.1417.002. [DOI] [PubMed] [Google Scholar]
- 15.Pack A, Schwab R. Characteristics of crashes attributed to the driver having fallen asleep. Accid Anal Prev. 2005;27:769–75. doi: 10.1016/0001-4575(95)00034-8. [DOI] [PubMed] [Google Scholar]
- 16.Dinges DF. An overview of sleepiness and accidents. J Sleep Res. 1995;4:4–14. doi: 10.1111/j.1365-2869.1995.tb00220.x. [DOI] [PubMed] [Google Scholar]
- 17.National Transportation Safety Board. Annual Report to Congress. 2009. [Accessed September 1, 2013]. http://www.ntsb.gov/Publictn/2010/SPC1001.htm.
- 18.Swaen GMH, Van Amelsvoort LGPM, Bultmann U, Kant IJ. Fatigue as a risk factor for being injured in an occupational accident: Results from the Maastricht Cohort Study. J Occup Environ Med. 2003;60:88–92. doi: 10.1136/oem.60.suppl_1.i88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Connor J, Norton R, Ameratunga S, et al. Driver sleepiness and risk of serious injury to car occupants: population based case control study. BMJ. 2002;324:1125. doi: 10.1136/bmj.324.7346.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Findley L. Vigilance and automobile accidents in patients with sleep apnea or narcolepsy. Chest. 1995;108:619–24. doi: 10.1378/chest.108.3.619. [DOI] [PubMed] [Google Scholar]
- 21.Melendres MC, Lutz JM, Rubin ED, Marcus CL. Daytime sleepiness and hyperactivity in children suspected with sleep-disordered breathing. Pediatrics. 2004;114:768–75. doi: 10.1542/peds.2004-0730. [DOI] [PubMed] [Google Scholar]
- 22.Beebe DW, Groesz L, Wells C, et al. The neuropsychological effects of obstructive sleep apnea: a meta-analysis of norm referenced and case controlled data. Sleep. 2003;26:298–307. doi: 10.1093/sleep/26.3.298. [DOI] [PubMed] [Google Scholar]
- 23.Carskadon M. Patterns of sleep and sleepiness in adolescents. Pediatrics. 1990;17:5–12. [PubMed] [Google Scholar]
- 24.Stores G, Montgomery P, Wiggs L. The psychosocial problems of children with narcolepsy and those with excessive daytime sleepiness of uncertain origin. Pediatrics. 2006;118:1116–23. doi: 10.1542/peds.2006-0647. [DOI] [PubMed] [Google Scholar]
- 25.Dorris L, Zuberi SM, Scott N, Moffat C, McArthur I. Psychosocial and intellectual functioning in childhood narcolepsy. Dev Neurorehabil. 2008;11:187–94. doi: 10.1080/17518420802011493. [DOI] [PubMed] [Google Scholar]
- 26.Dahl R, Holttum J, Trubnick L. A clinical picture of child and adolescent narcolepsy. J Am Acad Child Adolesc Psychiatry. 1994;33:834–41. doi: 10.1097/00004583-199407000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Barton BK, Schwebel DC. The roles of age, gender, inhibitory control, and parental supervision in children's pedestrian safety. J Pediatr Psychol. 2007;32:517–26. doi: 10.1093/jpepsy/jsm014. [DOI] [PubMed] [Google Scholar]
- 28.Plumert JM, Kearney JK, Cremer JF. Children's perception of gap affordances: Bicycling across traffic-filled intersections in an immersive virtual environment. Child Dev. 2004;75:1243–53. doi: 10.1111/j.1467-8624.2004.00736.x. [DOI] [PubMed] [Google Scholar]
- 29.Barton BK, Schwebel DC. The roles of age, gender, inhibitory control, and parental supervision in children's pedestrian safety. J Pediatr Psychol. 2007;32:517–26. doi: 10.1093/jpepsy/jsm014. [DOI] [PubMed] [Google Scholar]
- 30.Plumert JM. Relations between children's overestimation of their physical abilities and accident proneness. Dev Psychol. 1995;31:866–76. [Google Scholar]
- 31.Plumert JM, Schwebel DC. Societal and temperamental influences on children's overestimation of their physical abilities: Links to accidental injuries. J Exp Child Psychol. 1997;67:317–37. doi: 10.1006/jecp.1997.2411. [DOI] [PubMed] [Google Scholar]
- 32.Schwebel D, Plumert J. Longitudinal and concurrent relations among temperament, ability estimation, and injury proneness. Child Dev. 1999;70:222–30. doi: 10.1111/1467-8624.00050. [DOI] [PubMed] [Google Scholar]
- 33.Findley LJ, Suratt PM, Dinges DF. Time on task decrements in “steer clear” performance of patients with sleep apnea and narcolepsy. Sleep. 1999;22:804–9. doi: 10.1093/sleep/22.6.804. [DOI] [PubMed] [Google Scholar]
- 34.Ha KS, Yoo HK, Lyoo IK, Jeong DU. Computerized assessment of cognitive impairment in narcoleptic patients. Acta Neurol Scand. 2007;116:312–6. doi: 10.1111/j.1600-0404.2007.00891.x. [DOI] [PubMed] [Google Scholar]
- 35.Strayer DL, Drews FA. Cell-phone-induced driver distraction. Curr Dir Psych Sci. 2007;16:128–31. [Google Scholar]
- 36.Strayer DL, Drews FA, Johnston WA. Cell phone induced failures of visual attention during simulated driving. J Exp Psychol Appl. 2003;9:23–52. doi: 10.1037/1076-898x.9.1.23. [DOI] [PubMed] [Google Scholar]
- 37.American Thoracic Society. Sleep apnea, sleepiness, and driving risk. Am J Respir Crit Care Med. 1994;50:1463–73. doi: 10.1164/ajrccm.150.5.7952578. [DOI] [PubMed] [Google Scholar]
- 38.Navelet Y, Anders TF, Guilleminault C. Narcolepsy in children. In: Guilleminault C, Dement W, Passount P, editors. Narcolepsy. New York: Spectrum; 1976. [Google Scholar]
- 39.Bartolomeos K, Croft P, Job S, et al. Pedestrian safety: A road safety manual for decision-makers and practitioners. Geneva: World Health Organization; 2013. [Google Scholar]
- 40.Schwebel DC, Davis AL, O'Neal EE. Child pedestrian injury: A review of behavioral risks and preventive strategies. Am J Lifestyle Med. 2012;6:292–302. doi: 10.1177/0885066611404876. [DOI] [PMC free article] [PubMed] [Google Scholar]


