Abstract
Hepatocellular carcinoma (HCC) is the seventh-most common malignancy in males and ninth in females with incidence of one million new cases every year. Situs inversus totalis (SIT) is a rare congenital condition, in which there is a mirror-image transposition of both the abdominal and thoracic viscera. There are very few reported cases of HCC developing in people with SIT. In this review, we present a new case of HCC with SIT, and a review of literatures published between 1983 and 2011 on it. The literatures in English were searched through PubMed and Google Scholar, while those in Japanese language were accessed through J-EAST and translated in English with the help of Google translator on 22 April 2012. There are 6 English and 6 Japanese literatures showing 12 published cases, of which 10 cases were from Japan, 1 from Taiwan and 1 from China. Our case is probably the first case in the world beyond these regions. The articles containing adequate information, such as patient age and sex, investigations, diagnosis, type of congenital anomalies and methods of surgery, were reviewed. On reviewing the literature, we observed that clinical manifestations, laboratory findings and etiology correlate well with HCC, while anomalous hepatic vascularity correlates well with SIT. The reason for high incidence of HCC with SIT in Japan is not well correlated, but may be explained by higher incidence of SIT. All varieties of hepatic resection were feasible in cases of SIT.
Keywords: Situs inversus totalis, Hepatocellular carcinoma (HCC), Hepatectomy, Liver cancer
Introduction
Hepatocellular carcinoma (HCC) is one of the most common internal malignancies worldwide, especially in Eastern Asia, with poor prognosis and first leading cause of cancer-related deaths in southeast of China [1]. HCC is the seventh-most common malignancy in males and ninth in females. At least one million new cases of HCC occur annually and mortality from the disease remains high despite treatment. Cirrhosis has the most common association with HCC, being the underlying disease in 80 %–90 % of patients in most of the countries [2].
Situs inversus totalis (SIT) is a rare congenital condition, occurring with an incidence of 1:5,000 to 1:10,000, in which there is mirror-image transposition of both the abdominal and thoracic viscera [3]. The etiology of transposition of viscera is obscured and the condition does not influence normal health or life expectancy, but it has important surgical implications [4].
Case Report
A 49-year-old woman presented with a history of constant left-upper-quadrant dull aching pain, with no aggravating or relieving factors, for 1 month duration without other significant past medical or surgical history. Clinical examination revealed palpable lump up to 4 cm below left costal margin without jaundice and ascites. X-ray chest showed dextrocardia. Abdominal ultrasonography revealed situs inversus with left-sided liver showing a heterogeneous mass of about 12 × 11 × 7 cm in size in the postero-superior region.
CT scan of abdomen showed stomach and spleen on the right side whereas liver on the left side (Fig. 1). Liver showed 12 × 11 × 9 cm sized HCC involving segment VII and VIII as per Couinaud’s classification without any metastasis and vascular anomalies (Figs. 1 and 2). There were no extrahepatic lymphnode involvement, cirrhosis and ascites. The liver function test with coagulation profile was normal. Viral markers for hepatitis B virus (HBV) and hepatitis C virus (HCV) were negative. The serum α-fetoprotein (AFP) level was 16 ng/ml. The patient was planned for right hepatectomy, as she was clinically fit and CT scan did not show any vascular anomalies, liver metastasis and extrahepatic spread. The patient was operated under general anesthesia with inverted Y bilateral subcostal incision. On exploration of abdomen, liver was found in the left side while stomach and spleen were found in the right side. There were no ascites, extra hepatic lymph nodes and secondaries in the liver. Anatomy of extrahepatic structures was mirror image of normal. Intraglissonian dissection and clamping of vascular pedicles were done. Right hepatectomy was completed with the help of electrocautery (Fig. 3). The right hepatic vein was torn while ligation, requiring temporary vena caval occlusion for repair. The surgery was uneventful except right hepatic vein tear, with blood loss of about 1,000 ml and operating time of 6 hrs. Microscopically, the tumor diagnosed as a moderately differentiated HCC, with histological pattern of solid, nesting and trabecular types combined without vascular invasion and inactive cirrhosis with moderate fatty changes. The postoperative course was uneventful, except the patient had rising titer of serum bilirubin and serum alkaline phospatase for 10 days with maximum serum bilirubin (7.1 mg%) and serum alkaline phospatase (296 IU/l), which were returned to normal by twentieth day. Follow-up of the patient showed minimal regeneration of the liver on ultrasonography at 6 months and ascites with small tumor in the left lobe. The patient died after 9 months of surgery.
Fig. 1.
Transverse section view: liver in left side and stomach and spleen in right side
Fig. 2.
Left sagittal view: HCC involving VII and VIII segment of liver
Fig. 3.
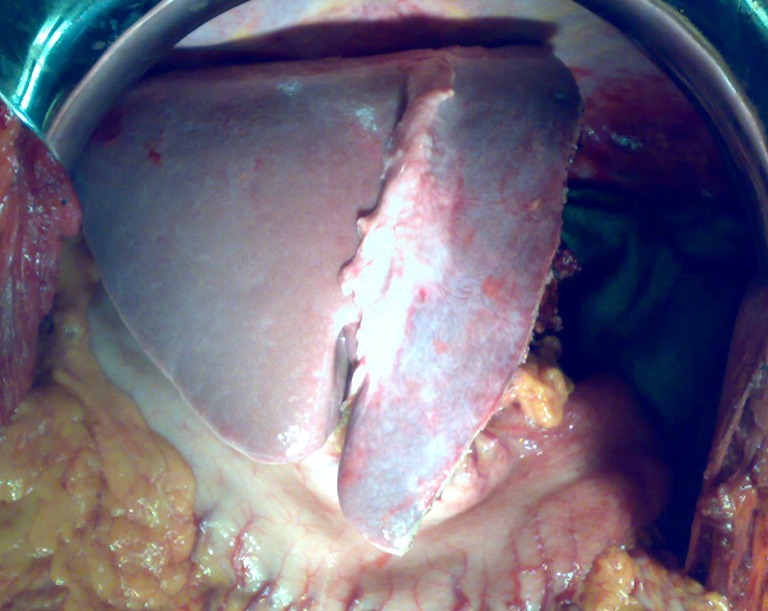
Photograph of liver after right hepatectomy
Discussion
HCC is thought to be rare compared with other organ cancers in SIT [5].
Situs Inversus Totalis (SIT)
In all vertebrates including humans have anatomical left-right asymmetry during embryogenesis. Normal arrangement is situs solitus and the variations results in heterotaxy, expressed either as randomization (situs ambiguous) or complete reversal (situs inversus) of normal organ position [6]. In SIT, a right/left mirror image transposition of the abdominal and thoracic viscera occurs. In heterotaxy, abdominal viscera may be inverted, whereas the thoracic contents may be normal, or vice versa. In isomerism, the body appears symmetric with bilateral left or right features. Situs inversus is rare in human beings and the incidence ranges between 1:1,000 and 1:10,000, depending on the population surveyed [7]. In Japan, prevalence of SIT was 1:4,100 population, which is about two times than that reported among Caucasians [8]. Japan has intermediate incidence of HCC, but most of the cases of SIT with HCC were reported from Japan may be because of high incidence of SIT.
In SIT, anomalies of the organs include: the liver may be bilobed or symmetric, the spleen may be absent or multiple, the gut may exhibit malrotation with abnormal mesentery and the lungs may have reversed pulmonary lobulation. Cardiac defects are common and vascular abnormalities may involve the inferior vena cava, portal vein and hepatic artery [7]. Such anomalies were also reported with HCC, which are shown in Table 1.
Table 1.
Summary of all 13 cases Hepatocellular Carcinoma (HCC) with Situs Inversus Totalis (SIT)
| NO. | Year | Author/(Language) | Country | Age/Sex | Presentation | Tumour location | Size | LFT | AFP ng/ml | Viral markers | Angiography | TAE/TACE | Treatment | Other notes |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1983 | Kanematsu (English) [4] | Japan | 37/M | Convulsion 10 cm hepatomegaly & cirrhosis | Rt. lobe | Multifocal | N | 1,400,000 | HbsAg + | N | TACE+ | Rt. Lobectomy** | Palliative surgery |
| 2 | 1983 | Wada [22] (Japanese) | Japan | 85/M | Abdominal pain, 8 cm hepatomegaly, 15 kg wt loss | Lt. lobe | 10*8*7 cm | N | 200 | – | Tumour thrombous in PV and IVC | TACE+ | Autopsy findings | Metastasis in GB and DU, + synchronous, stomach and Prostatic CA |
| 3 | 1989 | Kim [10] (English) | Japan | 66/F | Pain 3 weeks, 6 cm hepatomegaly | Rt. lobe | 14*12 cm | N | 4,000 | HbsAg + | Anomalous left hepatic vessels. | – | Rt. Lobectomy** & B-I Gastrectomy | Synchronous Gastric malignancy |
| 4 | 1990 | Kanchira[25] (Japanese) | Japan | 59/M | – | Seg. VIII | 3 cm | N | 2,388 | Negative | Anomalous common hepatic artery | – | – | – |
| 5 | 1996 | Kamike [3] (English) | Japan | 69/F | Cirrhosis | Seg. VII | 3*2 cm | N | 291 | – | Anomalous left hepatic vessels. | TAE + | Rt. Segmentectomy | Hepatocellular & Cholengio-cellular CA component |
| 6 | 1996 | Iwakura [5] (Japanese) | Japan | 63/M | Cirrhosis | Seg. VI | 1.5*1.3 cm | N | N | HCV + | N | TAE + | Lower posterior segmentectomy | Recurrence in caudate lobe 6 months |
| 7 | 1999 | Seshimo [25] (Japanese) | Japan | 70/M | Cirrhosis | Seg. II | 2.3*2.3 cm | N | 160 | HCV + | Anomalous common hepatic artery | – | Seg II partial hepatectomy | – |
| 8 | 2003 | Cheng [13] (English) | Taiwan | 43/M | Kartagener’s syndrome | Seg. II, III, IV | 10*9*7 cm | N | 27,910 | HbsAg +, HCV + | N | TAE + | Lt. Lobectomy | GB stone, AFP 30 ng/ml after 12 months |
| 9 | 2004 | Kakinuma[20] (Japanese) | Japan | 70/F | Asymptomatic | Seg. V, VI,VIII | 2.5*2.0 cm | N | N | HCV + | N | TAE + | Seg VII partial hepatectomy | – |
| 10 | 2004 | Niki [23] (English) | Japan | 66/M | Abdominal pain 1 week | Seg. II, V | 6 cm | N | N | Negative | N | TAE + | – | Well after 12 months |
| 11 | 2006 | Swada [24] (Japanese) | Japan | 76/M | Abdominal fullness | Rt. lobe | T2 | N | 803 | Negative | N | TAE + | Hepatic trisegmentectomy | Tumour size as per TNM classification |
| 12 | 2007 | Li [21] (English) | China | 53/M | Asymptomatic | Rt. lobe | 10 cm | Abnormal | 49 | Negative | IVC continuous as Hemiazygos | TACE+ | – | Schistomiasis, well at 12 months |
| 13 | 2011 | Present case | India | 49/F | Abdominal pain | Seg. VII, VIII | 12*11*10 cm | N | N | Negative | N | Not done | Rt lobectomy | Died after 9 months |
N Normal; M Male; F Female; Rt. Right; Lt. Left; GB Gallbladder; DU Duodenum; PV Portal vein; IVC Inferior vena cava; CA Carcinoma; wk week; LFT Liver Function test; AFP Alpha fetoprotein; TAE Trans arterial embolization; TACE trans arterial Chemo embolization; Seg. = segment; HCV Hepatitis C Virus; HbsAg Hepatitis B surface antigen
**original article had mention “lt. lobectomy”
Although most cases of situs inversus are sporadic, inheritance patterns including X-linked, autosomal recessive and autosomal dominant were found [9] with homologous region in humans located on the long arm of chromosome 12 [10]. Yost suggested that left-right axial information is contained in the extracellular matrix early in development and is independently transmitted to the cardiac and visceral primordia [11]. Recently, a theory model of bulk transport of extracellular morphogens by rotating primary cilia during gastrulation is appealing because it ‘bootstraps’ morphological asymmetry of the embryo from the intrinsic structural (molecular) chirality of motile cilia [12]. About 50 % of patients with primary ciliary dyskinesia (Kartagener’s syndrome) have situs inversus [13].
There is no evidence that situs inversus increases risk of malignancy, so association of cancer with this congenital anomaly is rare [14].
Hepatocellular Carcinoma (HCC)
The incidence of HCC has marked variation worldwide, South-east Asian countries (Taiwan, Korea, Thailand, Hong Kong, Singapore, Malaysia, Southern China) and tropical Africa show the high incidence, in the range of 10–20 per 100,000 population with highest being 150 and 28 per 100,000 in Taiwan and Singapore. Intermediate rates in Japan, Middle East and Mediterranean countries, and the lowest rates of 1–3 per 100,000 population for HCC are found in western countries, Australia, South America and India [2].
HCC is 4 to 8 times more common in males. Chronic hepatitis due to infection with HBV and HCV leads to cirrhosis, which is major premalignant condition and increases the risk of HCC about 100-fold higher than non-infected [15]. Rarely, liver cancer occurs in association with conditions that have a genetic, congenital or metabolic origin. HCC has been rarely documented in association with familial polyposis coli, ataxia telangiectasia, familial cholestatic cirrhosis, congenital hepatic fibrosis, neurofibromatosis, situs inversus and the fetal alcohol syndrome [2].
The primary marker for HCC is AFP, a single polypeptide chain glycoprotein. Serum AFP is elevated in chronic hepatic diseases and HCC. Even elevated levels have marked variation in HbsAg + ve and HbsAg –ve patients. HbsAg + ve patients have more elevated levels of AFP, so specificity and positive predictive value are low, especially when AFP is between the range of 25 and 200 ng/ml. Specificity and positive predictive value of AFP for diagnosis of HCC at 200 ng/ml are 80 % and at 3,200 ng/ml are 95 % in HbsAg + ve, whereas in HbsAg –ve patients at 200 ng/ml they are 100 % [16]. AFP may be normal in as many as 40 % of patients with early HCC. The sensitivity of tumor detection using AFP is 68.2 %, which increased to 88.6 % when combined with α-L-fucosidase and 95.5 % when combined with vascular endothelial growth factors (VEGF). The combination of the three markers yielded 100 % detection sensitivity [17].
The nomenclature of hepatectomy depends upon the number of hepatic segments resected as per Couinaud’s classification: extended hepatectomy (five segments), right hepatectomy or lobectomy (four segments), left hepatectomy or lobectomy (three segments), central hepatectomy (three segments), left lateral segmentectomy and right anterior or posterior segmentectomy (two segments). A segmental resection was defined as any sublobar resection [18]. Initial publication on SIT with HCC had documented left lobe liver involvement, which was the right lobe in normal patients. Mirror location of the right lobe of the liver was considered to be left, so they were mentioned as left lobectomy [4, 10]. Subsequent articles had not considered the mirror location of the lobes and had given normal nomenclature as right or left.
Liver grafts with SIT were traditionally considered to be an absolute contraindication for transplant because of anatomical concerns, but now literature is available where liver transplantation is done using SIT donor and normal recipient [19].
HCC with SIT
There are very few reported cases of HCC developing in people with SIT. In 1983, Kanematsu described the first case of HCC with SIT [4]. In this review, we have searched literature published in form of case reports, case series, letters to the editor, original articles and literature reviews relating to HCC with SIT between 1983 and 2012. In addition, reference lists of the articles obtained were also examined. The literature in English was searched via PubMed and Google Scholar, while the literature in Japanese language was accessed via J-EAST, which were translated in English with the help of Google translator on 22 April 2012. There were 12 published cases, 6 were in English and 6 in Japanese and the article types include 7 case reports, 2 case reports with review of previous cases and 2 letters to the editor. The geographic distribution was: 10 from Japan, 1 from Taiwan and 1 from China. Our case is probably the first case in the world beyond these regions. We have analyzed the information, such as patient age and sex, brief clinical presentation, investigations, pathology, diagnosis, type of congenital anomalies, methods of surgery, etc., of all available 12 cases and summarized it along with our case report for future review (Table 1).
The patients were aged from 37 to 85 years, which include 9 males and 4 females. The variety of presentations in these patients include asymptomatic [20, 21], abdominal pain [10, 22–24], abdominal lump [4, 10, 13, 22], cirrhosis with ascites [25], hypoglycaemia with convulsion [4] and azospermia with bronchiectasis [13].
Most of the patients were having normal sr. bilirubin and other liver function tests at the time of presentation, except one where very high bilirubin (44.5 nmol/L) [21]. The diagnostic serum marker for HCC, AFP was higher in 9 cases and normal in 4 patients including our patient. The viral marker for HBV was positive in 3 cases [4, 10, 13] and HCV in 4 cases [13, 20, 25], one had both viral markers positive [13].
Conventional or CT angiography was done in all the cases, 7 patients have normal mirror image presentation, but others have anomalous left hepatic vessels [3, 10], common hepatic artery [25] and IVC continuous as hemiazygos vein [21].
Nine patients had hepatic artery catheterization for transarterial chemoembolization (TAE) of the tumor to reduce tumor burden and vascularity before hepatectomy. TAE had led remarkable reduction in AFP in patients having higher value before the procedure. Variation of hepatectomy included 4 hepatic lobectomy, 2 partial hepatectomy and 3 hepatic segmentectomy.
Conclusion
In patients of HCC with SIT clinical manifestations, laboratory findings and etiology correlates well with HCC, while anomalous hepatic vascularity correlates well with SIT. TAE was performed in almost all cases, either as sole treatment or preoperative procedure. The reason for high incidence of HCC with SIT in Japan is not well correlated, but may be explained by higher incidence SIT. All varieties of hepatic resection were feasible to perform in cases of SIT. The nomenclature of hepatic surgery should not be altered in case of SIT.
Acknowledgment
We acknowledge Dr. Pankaj Patel, Dean, Smt. NHL Municipal Medical College, Dr. K. D. Chavda, Professor and Head, Department of surgery, for their guidance and moral support.
References
- 1.Xu LB, Wang J, Liu C, Pang HW, Chen YJ, Ou QJ, Chen JS. Staging systems for predicting survival of patients with hepatocellular carcinoma after surgery. World J Gastroenterol. 2010;16(41):5257–5262. doi: 10.3748/wjg.v16.i41.5257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leong TY, Leong AS. Epidemiology and carcinogenesis of hepatocellular carcinoma. HPB (Oxford) 2005;7(1):5–15. doi: 10.1080/13651820410024021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kamiike W, Itakura T, Tanaka H, Hatanaka N, Nakamuro M, Miyata M, Izumi H. Hepatic segmentectomy on primary liver cancer with situs inversus totalis. HPB Surg. 1996;9(3):169–172. doi: 10.1155/1996/29894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kanematsu T, Matsumata T, Kohno H, Sugimachi K, Inokuchi K. Hepatocellular carcinoma with situs inversus. Cancer. 1983;51(3):549–552. doi: 10.1002/1097-0142(19830201)51:3<549::AID-CNCR2820510331>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 5.Iwakura Shinji NT, Fumitoshi H. Hepatocellular carcinoma with situs inversus totalis. A case report. J Jpn Surg Assoc. 1998;59(12):3100–3103. doi: 10.3919/jjsa.59.3100. [DOI] [Google Scholar]
- 6.Casey B. Two rights make a wrong: human left-right malformations. Hum Mol Genet. 1998;7(10):1565–1571. doi: 10.1093/hmg/7.10.1565. [DOI] [PubMed] [Google Scholar]
- 7.Fishman LN, Lavine JE. What’s Wrong when it isn’t right: situs inversus and genetic control of organ position. Hepatology. 1994;19(1):257–258. doi: 10.1002/hep.1840190138. [DOI] [PubMed] [Google Scholar]
- 8.Katsuhara K, Kawamoto S, Wakabayashi T, Belsky JL. Situs inversus totalis and Kartagener’s syndrome in a Japanese population. Chest. 1972;61(1):56–61. doi: 10.1378/chest.61.1.56. [DOI] [PubMed] [Google Scholar]
- 9.Mathias RS, Lacro RV, Jones KL. X-linked laterality sequence: situs inversus, complex cardiac defects, splenic defects. Am J Med Genet. 1987;28(1):111–116. doi: 10.1002/ajmg.1320280116. [DOI] [PubMed] [Google Scholar]
- 10.Kim YI, Tada I, Kuwabara A, Kobayashi M. Double cancer of the liver and stomach with situs inversus totalis—a case report. Jpn J Surg. 1989;19(6):756–759. doi: 10.1007/BF02471729. [DOI] [PubMed] [Google Scholar]
- 11.Yost HJ. Regulation of vertebrate left-right asymmetries by extracellular matrix. Nature. 1992;357(6374):158–161. doi: 10.1038/357158a0. [DOI] [PubMed] [Google Scholar]
- 12.Levin M. The embryonic origins of left-right asymmetry. Crit Rev Oral Biol Med. 2004;15(4):197–206. doi: 10.1177/154411130401500403. [DOI] [PubMed] [Google Scholar]
- 13.Cheng-Chung Chen J-HL, Chen D-R. Hepatocellular carcinoma and cholelithiasis in situs inversus totalis associated with primary ciliary dyskinesia (Kartagener’s syndrome) Mid Taiwan J Med. 2003;8:42–47. [Google Scholar]
- 14.Adler HL, Lerner SP. Renal cell carcinoma and situs inversus viscerum. J Urol. 1998;160(6 Pt 1):2141–2142. doi: 10.1097/00005392-199812010-00052. [DOI] [PubMed] [Google Scholar]
- 15.Dienstag JL. Chronic hepatitis. In: Fauci B, Kasper, Hauser, Longo, Jameson, Loscalzo, editors. Harrison’s principles of internal medicine, vol 2. 17. New York: McGraw-Hill Medical; 2008. p. 1955. [Google Scholar]
- 16.Lee HS, Chung YH, Kim CY. Specificities of serum alpha-fetoprotein in HBsAg + and HBsAg- patients in the diagnosis of hepatocellular carcinoma. Hepatology. 1991;14(1):68–72. doi: 10.1002/hep.1840140112. [DOI] [PubMed] [Google Scholar]
- 17.el-Houseini ME, Mohammed MS, Elshemey WM, Hussein TD, Desouky OS, Elsayed AA. Enhanced detection of hepatocellular carcinoma. Cancer Control. 2005;12(4):248–253. doi: 10.1177/107327480501200407. [DOI] [PubMed] [Google Scholar]
- 18.Huang ZQ, Xu LN, Yang T, Zhang WZ, Huang XQ, Cai SW, Zhang AQ, Feng YQ, Zhou NX, Dong JH. Hepatic resection: an analysis of the impact of operative and perioperative factors on morbidity and mortality rates in 2008 consecutive hepatectomy cases. Chin Med J (Engl) 2009;122(19):2268–2277. [PubMed] [Google Scholar]
- 19.Dou J, Yang T, Cao JL, Gao QJ, Su YL, Zhu ZJ (2010) Classical orthotopic liver transplantation from a donor with situs inversus totalis using slight rotation of the liver graft. Chin Med J (Engl) 123(10):1353–1355 [PubMed]
- 20.Kakinuma D, Tajiri T, Yoshida H, Mamada Y, Taniai N, Kawano Y, Mizuguchi Y, Shimizu T, Takahashi T, Akimaru K, Aramaki T, Takano T. A case of hepatocellular carcinoma with situs inversus totalis. J Nippon Med Sch. 2004;71(3):209–212. doi: 10.1272/jnms.71.209. [DOI] [PubMed] [Google Scholar]
- 21.Li T, Wang L, Chen RX, Ye QH, Sun HC, Qin LX, Tang ZY. Hepatocellular carcinoma with situs inversus totalis and polysplenia syndrome. Liver Int. 2007;27(10):1430–1431. doi: 10.1111/j.1478-3231.2007.01597.x. [DOI] [PubMed] [Google Scholar]
- 22.Wada I, Nambu M, Sakita R, Ueyama H, Imai Y, Ueda H, Maeda S. Metastasis of hepatocellular carcinoma to the duodenum—an autopsy case with triple primary carcinoma on heterotaxia (situs inversus transversus viscerum totalis) Nippon Shokakibyo Gakkai Zasshi. 1983;80(2):228–231. [PubMed] [Google Scholar]
- 23.Niki Y, Shiraki K, Enokimura N, Okano H, Yamanaka T, Takase K, Nakano T. Hepatocellular carcinoma associated with situs inversus totalis. J Clin Gastroenterol. 2004;38(4):382–383. doi: 10.1097/00004836-200404000-00019. [DOI] [PubMed] [Google Scholar]
- 24.Sawada Ryugo ST, Tamuratasuro, Kiyotaka K, Kazutsugu S, Yamashitatakafumi Hepatocellular carcinoma with situs inversus totalis, developed in non-cirrhotic liver—a case report. J Jpn Surg Assoc. 2006;67(10):2433–2437. doi: 10.3919/jjsa.67.2433. [DOI] [Google Scholar]
- 25.Seshimo Tatsuyuki IM, Kazunobu M, Tomoo M. A case of hepatocellular carcinoma with situs inversus totalis. Jpn J Gastroenterol Surg. 1999;32(11):2573–2576. doi: 10.5833/jjgs.32.2573. [DOI] [Google Scholar]




