Abstract
There are not many injuries that rival the injured hand in complexity. A better understanding of biologic, behavioral, and socioeconomic risk factors potentially associated with hand injuries can help identify those individuals most at risk and define potential preventative measures to help reduce the incidence. We present a prospective study of 436 consecutive patients of hand and forearm injury treated over a period of 2 years. A serial recording of the demographic profile of the patient along with the type & cause of injury sustained, hand dominance, duration of hospital stay, time lag between injury and admission, type surgery preformed with intra-operative findings and the cost analysis was done. An expected male dominance in economically viable individuals of 21 to 30 years formed 50 % of the patients of which 22.9 % were labourers and students each. The malady was altercation (27.5 %) followed by industrial & road accidents. Post prandial period was most notorious with multiple neuro (27.05 %) vasculo (39.34 %) tendinous (60.66 %) injury common with even simple lacerations. Dominant hand injury was commonest. It is challenging to assess and treat an injured hand. This study defines the demography and the etiology behind the various cases of hand and forearm injury with the detailed trauma profile. The limitation of the study was absence of functional outcome. The necessity of hand trauma registry is a pre-requisite to quantify the burden of hand injuries and formulate a prevention strategy.
Keywords: Hand injuries, Incidence, Demography, Tendon injury, Neuro-vascular injury, Hand dominance
Introduction
There are not many injuries that rival the injured hand in complexity and intricacy. A better understanding of biologic, behavioral, and socioeconomic risk factors potentially associated with hand injuries can help identify those individuals most at risk and define potential preventive measures to help reduce the incidence. Approaching the injured hand with a logical and systematic diagnostic plan allows surgeons to recognize the location and severity of the injury portfolio and direct comprehensive treatment.
An organized experience in the care of hand injuries was not available until World War II, when military hand centers were established with Dr. Sterling Bunnell designated as a special civilian consultant to the Secretary of War in the United States [1].
Accidental injuries to the hand are unfortunately common. These injuries account for major financial loss from time away from work and medical expenses, in addition to permanent deformities and dysfunction of the hand, if not attended to in a manner of trepidation.
Material and Methods
A prospective study of 436 consecutive patients of hand and forearm injury over a period of 2 years was undertaken in a tertiary care institute, situated in the heart of the city known as the Manchester of India. The aim of the study was to build a demographic profile with the extent of injury in the at-risk population and to assess the type and cause of injury in various age groups.
All patients who had upper limb trauma (distal to elbow), with or without bony injury, within the age group of 1–80 years and the duration of injury of less than 2 days, requiring admission were included in the study. Patients with only bon injury, thermal injury, and chronic wounds and patients treated on outpatient basis were excluded from the study.
Data pertaining to the demographic profile of the patient, along with the type and cause of injury sustained, dominance of hand, time of injury, time lag between injury and admission, geographical distribution of referral, spatial distribution over the year, duration of hospital stay, extent of injury, and the cost of treatment were obtained.
The photographic record of the injury and the repair undertaken was maintained.
Results
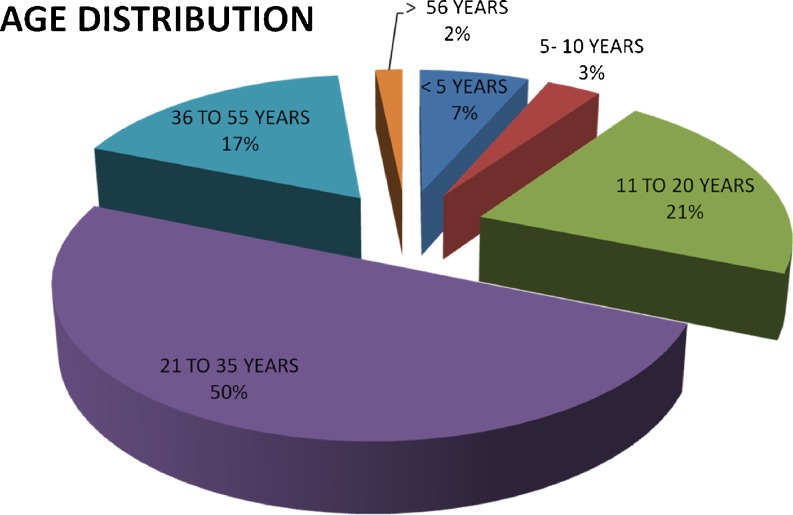
An expected male dominance among the injured, with male–female ratio of 6.18:1, was present. The economically productive age group of 21–55 years formed the major chunk (67 %) (Fig. 1). Closed fractures followed by soft tissue injury were the commonest injuries (Table 1) with associated injury of the proximal arm or the contra-lateral limb (Table 2).
Fig. 1.
Age distribution chart
Table 1.
Breakdown of the type of injuries beyond the elbow
| Type of injury | No. of patients |
|---|---|
| Closed fractures of distal forearm & small bones of hand | 186 |
| Compound fractures | 56 |
| Soft tissue injury | 122 |
| Day care (24 h admissions) | 72 |
| Total | 436 |
Table 2.
Associated injury profile
| Type of injury | Number of patients |
|---|---|
| Head injury | 51 |
| Spinal cord trauma | 23 |
| Blunt trauma chest | 46 |
| Blunt trauma abdomen | 62 |
| Proximal upper limb and/contralateral limb | 76 |
| Lower limb | 20 |
| No associated injury | 158 |
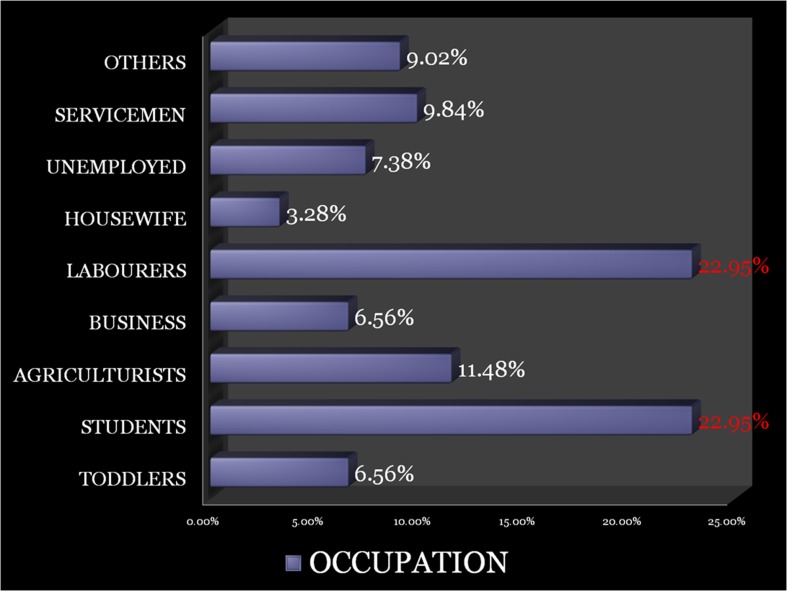
The college-going students (22.95 %) formulated the major patient population being more prone to altercation and road traffic accidents and followed by laborers drawn in industrial accidents (Fig. 2).
Fig. 2.
Occupational profile of the patients with hand injury
Even though the economic profile of the city would make us venture into believing that work-related injuries are the commonest (26.23 %), altercations were alarmingly commoner (27.05 %) (Table 3). Accidental injuries were the commonest (70.5 %), but a large subset of 27.1 % were homicidal and 2.45 % were suicidal commonest in the age group of 16–30 years.
Table 3.
Etiology of injury and the environmental factors responsible
| Cause of injury | Place of injury |
|---|---|
| Factory accidents (22.13 %) | |
| Shop/garage (4.1 %) | |
| Home (13.12 %) | Door/drawer crush |
| Home appliances | |
| Assault (27.05 %) | Roadside |
| Home | |
| Market place | |
| Grounds | |
| Sports injury (3.28 %) | Playground |
| Kite flying | |
| Road traffic accident (13.12 %) | |
| Road rage (0.81 %) | |
| Alcoholic rage (4.1 %) | Home (Glass cut) |
| Suicidal (2.46 %) | Under influence of alcohol |
| Depression | |
| Accidental fall on glass (8.2 %) | Home |
| College | |
| Under influence of alcohol | |
| Religious ceremony (BAKRID) (0.81 %) | |
| Police firing (0.81 %) | |
| Cattle gore (0.81 %) | |
| Train window crush (1.64 %) | |
The triage catered to patients from all over the state of Punjab with the majority referral (51 %) from within the city. Even still only 17 % patients reached the emergency within 1 h of the injury, 61 % within 1–5 h, 18 % within 6–12 h, and 4 % after 12 h of injury. The second quarter of the day witnessed the majority of accidents, with 3 pm to 6 pm forming prime period for the major injuries (24 %) and closely followed by the overtime working hours in the night from 9 pm to 12 am (16 %) and morning hours of 9 am to 12 pm (15 %).
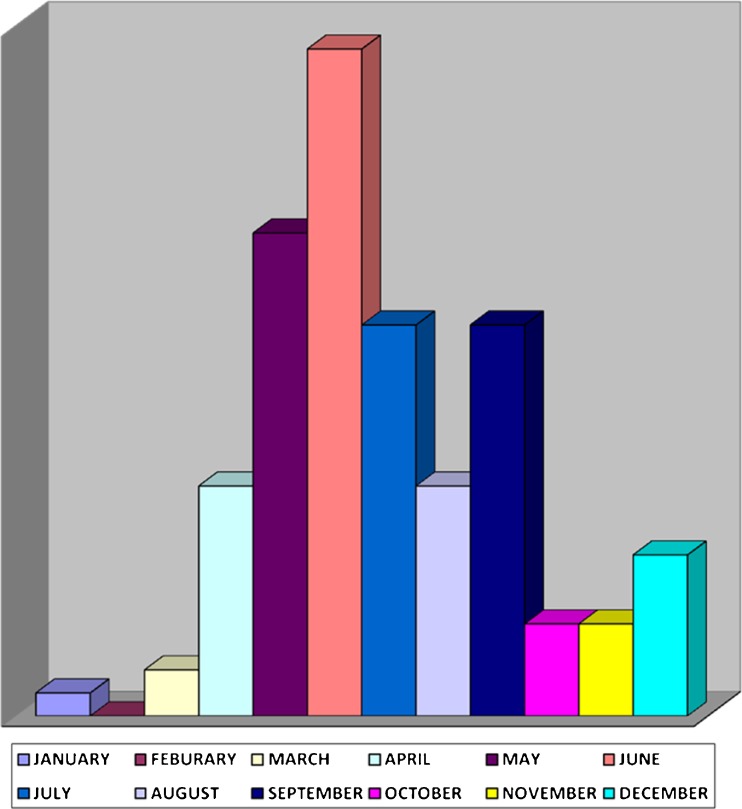
The distribution of various injuries was skewed over the months, with the month of June forming the most injurious month of the year apart from being the hottest followed by May (Fig. 3).
Fig. 3.
Distribution of hand injury over the year
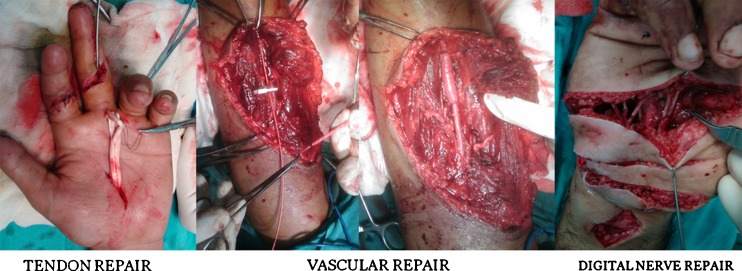
Of the 67.21 % laceration and incised wounds, 74.4 % patients had associated tendon injury and 25.61 % had fractures of the small bones of the hand. Crush injury (majorly industrial accidents) constituted 22.95 % with bony injury in 57.14 % and tendon injury in 35.7 % patients. The global incidence of tendon injury was 60.66 %, with associate vascular injury in 39.34 % patients. Injury to the median, ulnar, and digital nerves was to a tune of 27.05 %, making the simple-looking incised wound grievous in nature. The incidence of isolated vascular injury was 6.56 % with ulnar artery being the commonest injured vessel (Fig. 4).
Fig. 4.
Soft tissue repair of vital structures of the hand
There were 5 patients of re-implantation which included 2 thumbs, 1 hand, and 2 forearms apart from 7 complete revascularization procedures (Fig. 5).
Fig. 5.

Reimplantation of hand in a 65-year-old woman, victim of assault
Hand dominance depicted the common trend with 83.6 % of the patients being right handed and 12.3 % left handed. About 0.80 % patients were ambidextrous and 3.3 % did not have developed hand dominance. Although the injury of either hand was equivalent, the dominant hand was more commonly injured than the nondominant hand (Table 4).
Table 4.
Hand dominance and the injured extremity
| Dominant hand | Total % | Injured hand | ||
|---|---|---|---|---|
| Left hand | Right hand | B/L | ||
| Left | 12.3 % | 60 % | 33.33 % | 6.66 % |
| Right | 83.6 % | 45.1 % | 50 % | 4.9 % |
| Dominance not developed | 3.3 % | 20 % | 80 % | – |
| Ambiextrous | 0.80 % | 58 % | 41 % | 1 % |
Majority of the incised wounds with neurovascular injury were operated within 4 h of presentation, but patients with crush injuries, polytrauma, and nonconsenting attendants were the cause of delayed surgery in 9.83 %.
The median duration of stay in the hospital was 6 days and the cost of treatment ranged from Rs9,000 to [COMP: Rupee symbol]Rs1,48,422.
Discussion
Trauma to the hand presents with multiple soft tissue and osseous manifestations that often appear unrelated, leading to underrecognition and potential undertreatment of the complex injuries. Approaching the injured hand with a logical and systematic diagnostic plan allows surgeons to recognize the location and severity of the injury portfolio and primary comprehensive treatment. Understanding the trauma mechanism and patterns of injury in the injured hand will maximize awareness and guide surgical reconstruction, rehabilitation, and prevention [2].
It is challenging to assess and treat the crushed hand. These are multisystem, combined injuries that can lead to suboptimal functional recovery based on the severity of the tissue trauma alone [3–5]. Aggressive initial management affords the best chance to optimize results. The cornerstone of care is the identification of the pathoanatomy, assessment of the magnitude of the injuries, and focused treatment in the context of the complete injury.
The spectrum of injuries ranges from mild lacerations that can be repaired in the emergency department to multiple finger amputations and exploded hand, which requires extensive, and often multiple, reconstructive procedures [6]. The time and loss of work and wages, as well as the medical expenses, increase dramatically for severe injuries. In addition, there is tremendous physical and emotional pain.
Hand injuries demonstrated a peak in the age group of 21–35 years influenced primarily by industrial accidents and altercations. In our study, the number of hand injury cases in 1–5 years age group was 6.8 % of all cases, which is high when compared to 4.2 % in a study done in North Ireland [7]. The incidence of young Swedish children with hand injuries referred for treatment is 27/10,000 children/year.
In our study, of the eight children less than 5 years of age, 75 % were injured when their hands came in the door (of the house and/car) and 25 % were injured by glass at home. The female child was injured 1.6 times more commonly than the male child of less than 5 years of age.
Understanding the environmental etiology is the first step for formulating preventive measures. As most injuries occur in the home environment, efforts should be directed at reducing childhood injuries at the home. Child-friendly homes and parental supervision are the keystones. The success of “kids can’t fly” campaign developed by New York Health Department highlights the effectiveness of simple accident prevention programs in the peridomestic environment [8].
The at-risk behavior for sustaining hand injury was highest in the age group of 16–30 years, with 37.71 % patients had accidental injury and 16.39 % patients had homicidal injuries. The alarming discovery was that 8.19 % patients in the age groups of 31–50 years and 2.46 % patients of more than 51 years of age were victims of homicidal injury. All the patients with suicidal injuries had associated tendon injury with arterial injury, and all were males. It was their first attempt and were under treatment for depression.
The male–female ratio of 6.2:1 is high in comparison to the ratio of 2.2:1 in the British Isles [9] and 1.6:1 in Denmark [10]. The variation reflects cultural and employment differences.
The social structure of the city and surrounding catchment area is categorized into the laborers (23 %), the service class (9.84 %), the students’ community (23 %), and the agriculturists including the unemployed and others (27.86 %). The latter group forms the major chunk of the assault and road traffic accidents whereas the industrial accidents are the bread snatchers of the labor class.
The epidemiology of violence in India is least understood. The problem, pattern, and causes of violence vary significantly across rural and urban areas, between ages, gender, and in different socioeconomic groups. According to National Crime Records Bureau (2001), the annual injury rate is 87/1,00,000, with the cities accounting for only 10 % of violence-related death and injury [11].
In India, occupational injuries contributed to 2 % of total deaths, 1.8 % of total life years lost due to disabilities, and 2 % of disability-adjusted life years (DALYs) in 1990 [12]. It is estimated that 19 fatal and 1,930 (1:100) nonfatal accidents occur annually per 1,00,000 workers [13]. The incidence of industrial injuries among employed workers was 9/1,000, with a frequency of 2.6 per 1,00,000 man-days work [14]. Across studies, the highest number of injuries occurs among men and in the economically productive age group of 21–49 years. In India, 25–30 % of injuries occur in patients of 16–20 years of age, 30–45 % in 21–35 years of age, and about 30 % in 36–49 years of age, which was similar to our study.
No definite information is available on agricultural injuries in India. In our study of 436 patients, which included 11.48 % farmers, unpredictably none sustained injuries from farm instruments or appliances, but from assault and road traffic accidents. In a longitudinal study of 12,189 agricultural workers by Tiwari et al. (2002) in Madhya Pradesh during 1995–1999, the incidence rate was 1.25/1,000 workers/year. About 78 % of all injuries were due to farm machinery, 12 % due to hand tools, and 11 % due to other causes [15].
Our study was in contrast to the study by Niemines et al’ [7] which showed 70 % of adult hand injuries occurring at home, 28 % at work, and 3 % in road accidents, which in our study was 13.6 % at home, 26.2 % at work, 27.1 % assault, and 13.9 % road accidents.
About 41.8 % of the geographical referral to our institute was from the district of Ludhiana with an estimated population of approximately 14 lakh. The small number of patients is in contrast of the major industrial outlay of the city and can be explained on the factors of high cost of treatment (average Rs20,000–35,000), lack of government funding, and the lack of personal insurance with the daily wage earner. The exploded hands and/or injuries with neurovascular component usually percolate to the tertiary care hospital. The majority of households reported a decline in earnings after injury; further, many had to borrow money from external sources for survival and only 5 % received compensation from insurance agencies or their employers. The poor spent Rs6,000–25,000 (average Rs18,000), while the nonpoor spent Rs32,000 (average Rs27,000) on medical costs [11].
The average cost per patient amounted to Rs32,456 (US$706/€531), which is enormous considering the daily wager earns Rs180 per day (€2.95/US$3.92). Even though the per capita income for an Indian is US$1,030, the 42 % of the population living below the poverty line earns US$1.25 per day.
An injured person has to spend resources for care at different levels—before reaching the hospital and after discharge for transport, drugs, admission, investigation, and interventions, depending on the place of care. The rehabilitation costs can be huge in certain types of injuries such as road traffic accidents, violence, and work-related injuries. Loans taken or savings spent put a strain on the resources of the family [11].
About 17.21 % of patients were able to reach the hospital within 1 h of sustaining injury and 60.66 % within 1–5 h of injury. The excellent road network in the state of Punjab and robust public transport can be credited for connectivity of remote villages to major cities.
The majority of the population is either agriculturists or migrant laborers, and hot months of May, June, and July, when there is no work in the fields and due to frequent power cuts, the industry has to run overtime to meet its production deadlines, form the most devastating months for hand trauma. During the cool months of January and February, the number of injuries is at minimum. The environmental factors play a significant role in the incidence of hand trauma. A study conducted in Southern Sweden documented that there was reduced risk of injury during the months of July, November, and December even though there was not much difference in the type, mechanism, and/or severity of injury between years [16].
There was no statistically significant difference in the days on which the hand injuries occurred more commonly, but the last two quarters of the day from 12 pm to 6 pm and to 12 am constituted 69 % of the injury profile. The postprandial period and the evening overtime fatigue were the common denominators in the industrial accidents whereas alcohol consumption and personal grudges were the factors for late night homicidal injuries. Even though this study does not amount to an epidemiological study, it does predict the high incidence of industrial accidents in fatigued and unskilled laborers. There are a very few epidemiological studies on hand trauma in an urban environment of a developing country [17–19]. The incidence rate of hand injuries in seven manufacturing environments around the world ranges from 4 to 11 per 100 workers per year [20]. Workers aged less than 24 years had the highest risk of hand injury, which was consistent in our study too. It is documented that men have higher rates of severe hand injury than women. More analytic epidemiological research is needed to identify potentially modifiable risk or protective factors for acute hand injuries.
There is no centralized agency in India to examine occupational injuries. These injuries are listed under general surgical conditions, and the underlying causes are not documented and reported; hence, the precise extent of occupational injury is difficult to establish. Even minor injuries, however, may create significant psychosocial and legal issues, which in turn, affect the length and degree of disability. Many of our patients developed neuropsychiatric disorders, ranging from posttraumatic stress disorder to chronic pain syndrome [21].
Lacerations and incised wounds were presenting injuries in 67.21 %, with tendon injury in 74.4 % patients and fractures in 25.61 %. The incidence of crush injury, dominant in the industrial accidents, was 22.95 % with underlying tendon and bony injury in 35.7 % and 57.14 %, respectively. Of the deep structure injuries, tendon injury constituted 60.66 %, vascular injury 39.34 %, nerve injury 27.05 %, and 35.25 % had compound fractures. The pattern of injury was different compared to injuries presenting to emergency services in the west [22] where human bites account for almost 5.2 % for presenting complaints which were prominent in our study by its absence. Incidence of tendon injury with crush injury was high. In general, the normal tendons of the hand do not rupture unless an external trauma or a weakness, due to a pathologic condition, occurs [23]. Blast injuries can cause severe internal damage in the absence of significant surface injury [24].
The highlight of the study was that even though the patient presented with minor lacerations over the wrist and/hand, there was a high incidence of associated injury to the underlying vital structures, whose repair was vital to the final function of the hand. A simple-appearing laceration with underlying occult visual structure injury amounts to grievous injury. Neuro-vasculo-tendinous injury combined was present in 27.86 % of the patients out of which 25 % were complete revascularizations and replantations. Although missed tendon injuries have received an ample interest in the literature, with reported incidences up to 20 %, there is little information about missed nerve and vascular injuries [25]. Further, it is very interesting that Angermann and Lohmann, in a retrospective evaluation of 50,272 hand injuries, have not reported even a single vascular injury. Therefore, it is obvious that it is very easy to overlook an arterial injury.
The right and the left hands were injured with similar frequency, concurrent with the findings of other reports [26]. Studies in ergonomics suggest that the nondominant hand primarily functions in terms of stabilization and positioning whereas the dominant hand has a more active role. It might be thought that the nondominant hand or the passive hand would be more prone to laceration and the active dominant hand to cutting injuries, but both dominant and non-dominant hands are at equal risk whatever the mechanism [27]. Our study demonstrated that left-hand dominant patients were more prone to injuring their dominant hands (60 %) compared to right-hand dominant patients (50 %), which is concurrent with the study conducted in the Philadelphia Hand Center, Philadelphia [28]. The presented data suggested that left-handed individuals had a relative risk of sustaining an amputating injury 4.9 times greater than the right-handed individuals, while minor hand trauma occurred at rates proportional to the distribution of left handedness within the population.
Injuries to the hand are a common cause of presentation in emergency departments. Patients who require transfer to a plastic surgical unit [29] for specialist surgery can be easily identified by a careful history examination and plain X-rays. Criteria for transfer include injury to nerves, tendons or joints, skin loss or complex fractures, injuries requiring skin grafting or reconstruction, and burns [30].
Conclusion
The limitations of the study were the small cohort. As the institute is not the only tertiary care center in the region, and patients presenting after 24 h were not included, the study cannot be considered an epidemiological study in the true sense, but extrapolations can be generated as it encompasses all the strata of the society with all age groups inclusive with the absence of a hand injury registry in the state of Punjab. A major chunk of the patients were migrant laborers who could not be followed up for assessment of postoperative functional valuation.
Epidemiological studies in the urban Indian cities require maintenance of a hand injury registry which can present the broader picture of hand injury and its outcome as has been the endeavor in the current study. The diverse nature of health stratification and erratic referral criteria form a gigantic roadblock in any and all such efforts, which may resolve with the concerted efforts of the hospital administrators, district surgeons, and the surgical community together.
Acknowledgments
Conflict of Interest
None
Source of Funding
None
References
- 1.George EO. Development of hand surgery: education of hand surgeons. J Hand Surg. 2000;25(4):616–628. doi: 10.1053/jhsu.2000.9752. [DOI] [PubMed] [Google Scholar]
- 2.Graham TJ. The exploded hand syndrome: logical evaluation and comprehensive treatment of severely crushed hand. J Hand Surg. 2006;31A:1012–1023. doi: 10.1016/j.jhsa.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 3.Sandzen SC., Jr Crush injuries of the hand and fingers. I. Med Trial Tech Q. 1972;19:144–151. [PubMed] [Google Scholar]
- 4.Sandzen SC., Jr Crush injuries of the hand and fingers. III. Med Trial Tech Q. 1973;19:418–431. [PubMed] [Google Scholar]
- 5.Sandzen SC., Jr Crush injuries of the hand and fingers. II. Med Trial Tech Q. 1973;19:282–289. [PubMed] [Google Scholar]
- 6.Samuel CH, Jason AC, David GD, Alexander YS. The economical impact of electrical saw injuries to the hand. J Hand Surg. 2009;34A:886–889. [Google Scholar]
- 7.Hill C. A regional audit of hand and wrist injuries. J Hand Surg. 1998;23B(2):196–200. doi: 10.1016/S0266-7681(98)80174-5. [DOI] [PubMed] [Google Scholar]
- 8.Spiegel CN, Lindaman FC. Children can’t fly: a program to prevent childhood morbidity and mortality from window falls. Am J Public Health. 1977;67:1143–1147. doi: 10.2105/AJPH.67.12.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilson P. A spectrum of hand injuries. Br J Accid Emerg Med. 1986;1:25–27. [Google Scholar]
- 10.Angermann P, Lohmann M. Injuries to the hand and the wrist. A study of 50272 injuries. J Hand Surg. 1993;18B:642–644. doi: 10.1016/0266-7681(93)90024-A. [DOI] [PubMed] [Google Scholar]
- 11.Gururaj G (2005) Injuries in India: a national perspective. WHO India, NCMH background papers—Burden of disease in india (New Delhi, India), September 2005:325–347
- 12.Sudhir D. Occupational health services for agricultural workers. Ind J Occup Environ Med. 1998;2:96–111. [Google Scholar]
- 13.Nag PK, Patel VG. Work accidents among shift workers in industry. Int J Ind Ergonom. 1998;21:275–281. doi: 10.1016/S0169-8141(97)00050-4. [DOI] [Google Scholar]
- 14.Select socioeconomic statistics of India, 2002. New Delhi: Ministry of Statistics & Programme Implementation, Government of India; 2004. [Google Scholar]
- 15.Tiwari SP, Gite PS, Dubey AK, Kot LS (2002) Agricultural injuries in central india: Nature, magnitude, and economic impact. J Agric Saf Health 8(1):95–111 [DOI] [PubMed]
- 16.Roseberg HE, Dahlin LB. Epidemiology of hand injuries in a middle sized city in southern Sweden: a retrospective comparison of 1989 and 1997. Scand J Plast Reconstr Surg Hand Surg. 2004;38(6):347–355. doi: 10.1080/02844310410022117. [DOI] [PubMed] [Google Scholar]
- 17.Iqbal QM. Long bone fractures among children in Malaysia. Int Surg. 1974;59:410–415. [PubMed] [Google Scholar]
- 18.Mann DC, Rajmaria S. Distribution of physeal and non physeal fractures in 2650 long bone fractures in children aged 0–16 years. J Pediatr Orthop. 1990;10:713–716. doi: 10.1097/01241398-199011000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Wong PC. A comparative epidemiologic study of fractures among Indian, malay and Swedish children. Med J Malaya. 1965;20:132–143. [PubMed] [Google Scholar]
- 20.Sorock GS, Lombardi DA, Courtney TK, Cotnam JP, et al. Epidemiology of occupational acute hand injuries: a literature review. Safety Sci. 2001;38(3):241–256. doi: 10.1016/S0925-7535(01)00004-2. [DOI] [Google Scholar]
- 21.William HF, Miller M, Fox SR, Brand D, Finseth F. Hand injuries: indicence and epidemiology in an emergency service. J Am Colg Emerg Physicians. 1978;7(7):265–268. doi: 10.1016/S0361-1124(78)80336-0. [DOI] [PubMed] [Google Scholar]
- 22.Hultman CS, Erfanian K, Fraser J, Thornton SJ, Calvert CS, Cairns BA. Comprehensive management of hot-press hand injuries: long-term outcomes following reconstruction and rehabilitation. Ann Plast Surg. 2010;64:553–558. doi: 10.1097/SAP.0b013e3181bffc7f. [DOI] [PubMed] [Google Scholar]
- 23.Naohito H, Masato A, Rui A, et al. Closed tendon rupture of both flexor digitorum profundus and superficialis tendons of the small finger in zone II: case report. J Hand Surg Am. 2011;36:121–124. doi: 10.1016/j.jhsa.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 24.Moreno OC, González-Escalada RM, García FJL (2012) Multiple closed avulsions of flexor tendons of the hand caused by a firecracker blast. Ann Plast Surg 68:158–160 [DOI] [PubMed]
- 25.Tuncali D, Yavuz N, Terzioglu A, Aslan G. The rate of upper-extremity deep-structure injuries through small penetrating lacerations. Ann Plast Surg. 2005;55:146–148. doi: 10.1097/01.sap.0000168884.88016.e1. [DOI] [PubMed] [Google Scholar]
- 26.Edward DH. The spectrum of hand injuries. Hand. 1975;7:46–50. doi: 10.1016/0072-968X(75)90038-8. [DOI] [PubMed] [Google Scholar]
- 27.Hollies LJ. The relationship between handedness, mechanism of injury and which hand injured. J Hand Surg. 1993;18B:394. doi: 10.1016/0266-7681(93)90071-M. [DOI] [PubMed] [Google Scholar]
- 28.Taras JS, Beherman MJ, Degnan GG. Left hand dominance and hand trauma. J Hand Surg. 1995;20A:1043–1046. doi: 10.1016/S0363-5023(05)80157-1. [DOI] [PubMed] [Google Scholar]
- 29.Rea S, Jones D, Eadie PA. Establishing a plastic surgery trauma clinic. Ir Med J. 2004;97(4):106–107. [PubMed] [Google Scholar]
- 30.Murphy SM, Whately K, Eadie PA, Orr DJ. Unnecessary inter-hospital referral of minor hand injuries: a continuing problem. Ir J Med Sci. 2010;179:123–125. doi: 10.1007/s11845-009-0416-3. [DOI] [PubMed] [Google Scholar]