Abstract
Background and Purpose
Acute ischemic stroke (IS) patients benefit from rapid evaluation and treatment, and timely brain imaging is a necessary component. We determined the effect of a targeted behavioral intervention on door-to-imaging-time (DIT) among IS patients treated with tissue plasminogen activator (tPA). Secondarily, we examined the variation in DIT accounted for by patient- and hospital-level factors.
Methods
The INSTINCT trial was a cluster-randomized, controlled trial involving 24 Michigan hospitals. The intervention aimed to increase tPA utilization. Detailed chart abstractions collected data for 557 IS patients. We used a series of hierarchical linear mixed-effects models to evaluate the effect of the intervention on DIT (difference-in-differences analysis) and used patient and hospital-level explanatory variables to decompose variation in DIT.
Results
DIT improved over time, without a difference between intervention and control hospitals (intervention: 23.7 to 19.3 minutes, control: 28.9 to 19.2 minutes, p=0.56). Adjusted DIT was faster in patients who arrived by ambulance (7.2 minutes; 95%CI 4.1–10.2), had severe strokes (1.0 minute per +5 point NIHSS; 95%CI 0.1–2.0), and presented in the post-intervention period (4.9 minutes; 95%CI 2.3–7.4). After accounting for these factors, 13.8% of variation in DIT was attributable to hospital. Neither hospital stroke volume nor stroke center status was associated with DIT.
Conclusions
Performance on DIT improved similarly in intervention and control hospitals suggesting that non-intervention factors explain the improvement. Hospital-level factors explain a modest proportion of variation in DIT but further research is needed to identify the hospital-level factors responsible.
Keywords: acute stroke, brain imaging, hospital variation
INTRODUCTION
Tissue plasminogen activator (tPA) remains underutilized in the emergent care of acute ischemic stroke (IS).1 Prolonged door-to-imaging time (DIT) may delay or prevent thrombolysis. Guidelines recommend DIT of 25 minutes,2 yet nationally DITs are sub-optimal.3 This may represent an intervention target to improve thrombolytic delivery. The Increasing Stroke Treatment through Interventional behavioral Change Tactics (INSTINCT) was a cluster-randomized, controlled trial aimed to increase appropriate tPA use with multi-level targeted educational interventions.4
In this analysis, we determined the effect of the INSTINCT intervention on DIT among tPA-treated, acute IS patients. We hypothesized that the standardized, barrier assessment, multi-component educational intervention developed to increase tPA use in community hospitals would improve DIT as part of the overall improvement in local stroke systems. Secondarily, we examined the variation in DIT accounted for by patient- and hospital-level factors.
METHODS
This is a secondary analysis of INSTINCT trial data,4 a cluster-randomized, controlled trial, matching 12 intervention with 12 control non-specialty, acute-care community hospitals in Michigan. A multi-level barrier assessment and interactive educational program based on behavior change theory was delivered to intervention hospitals from January-December 2007. Design and intervention are further detailed in supplemental material.
Study Population
Detailed chart abstractions were conducted only for tPA-treated patients. We excluded patients with in-hospital stroke onset, and patients with missing DIT (3.6% of sample, n=19). Excluded patients were similar in demographics, co-morbidities, risk factors, and stroke severity, but more often from control hospitals pre-intervention.
Analysis
The primary outcome, DIT, was derived from medical records as the difference between Emergency Department (ED) arrival time and initial brain imaging time (CT in all cases).
Data were analyzed using STATA 12.1 (STATA Corp, College Station, TX). Baseline characteristics were compared by treatment group using chi-square or ANOVA as appropriate.
Hierarchical linear models examined the association between DIT and randomization group, accounting for observation time (before versus after intervention), before and after adjustment for patient and hospital factors, with a random hospital-level intercept. The parameter estimate for the randomization group-by-time interaction assessed the significance of the intervention effect (see supplement).
A two-level linear mixed-effect regression model examined the proportion of variation in DIT explained by patient- and hospital-level factors. An empty model decomposed the unadjusted variation. Then patient-level variables were added. Finally, hospital-level variables (stroke volume and stroke center status) were added. We made posterior predictions of the average marginal effects of ambulance arrival and stroke severity on predicted DIT, holding other variables constant (see supplement).
RESULTS
Of the 511 tPA-treated patients, mean age was 69.9 years, 52.5% were male, and 75.9% non-Hispanic white. Mean NIHSS score was 12.2 points (standard deviation, SD, 5.9). Most arrived by ambulance (83.2%) and received tPA within 180 minutes of onset (84.7%) (Supplemental Table 1).
Mean DIT was 20.3 minutes (SD 13.5 min). Baseline DIT and improvement in DIT from pre- to post-intervention was similar between intervention (23.7 to 19.3 minutes) and control hospitals (28.9 to 19.2 minutes, p=0.30 for difference in baseline, p=0.56 for difference in improvement).
Of the unadjusted variation in DIT, 13.4% was attributable to hospitals (intraclass correlation coefficient, ICC, 0.134). After including patient-level factors, the variation attributable to hospitals changed minimally (ICC 0.138). Adding hospital stroke center status and stroke volume did not predict DIT, but did explain 18.4% of the between-hospital variance (ICC 0.116). (Figure 1)
Figure 1.
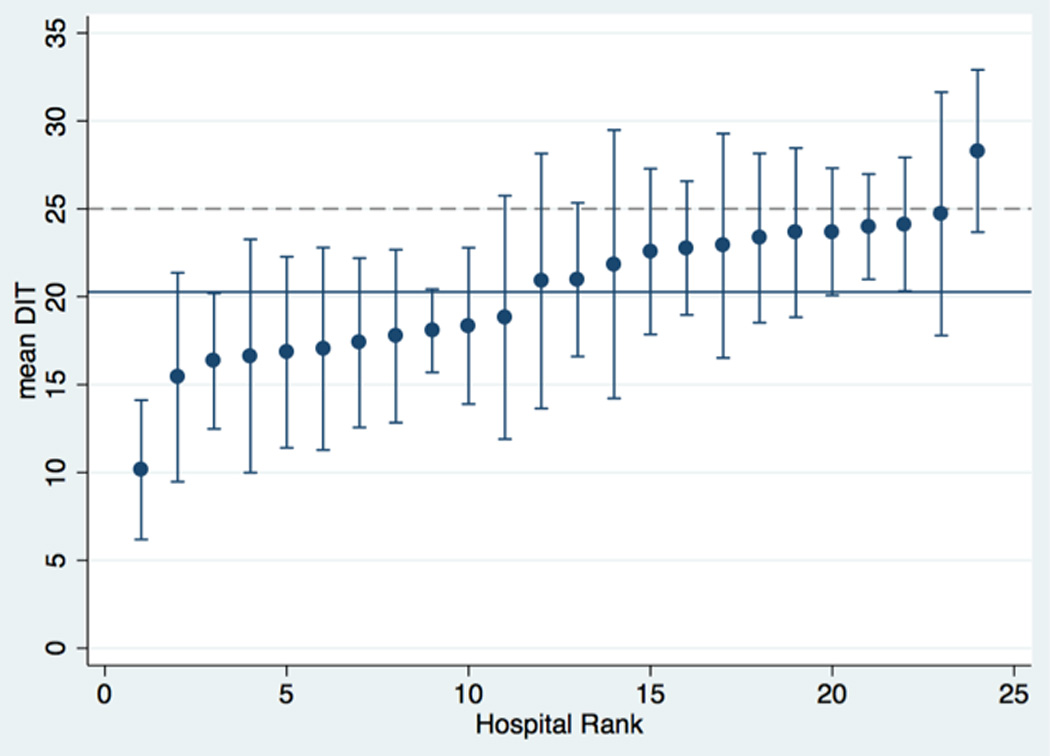
Ranking of Hospitals’ Adjusted Door-to-Imaging time (DIT)
*Hospitals ranked by mean predicted DIT, adjusted for age, race, sex, diabetes, valvular disease, onset location, onset-to-arrival time, stroke severity (NIHSS), ambulance arrival, weekend presentation, elevated blood pressure on arrival, presentation to intervention versus control hospital, and pre-versus post-intervention.
Bars: 95%CI around predicted values
Blue line: overall mean (20.3 minutes)
Dashed line: 25-minute benchmark
In multivariable analysis, predictors of faster DIT were stroke severity (1 minute per 5 point increase in NIHSS; 95%CI 0.1–2.0 min), ambulance arrival (7.2 minutes; 95%CI 4.1–10.2 min), and presentation post-intervention (2009–2010 vs. 2005–2006, 4.9 min; 95%CI 2.3–7.4 min) (Table 1). Ambulance arrival and stroke severity operated independently to effect DIT (Figure 2).
Table 1.
Predictors of Door-to-Imaging time (DIT) in Multivariable Analysis
| Change in DIT (minutes) |
95% CI | |
|---|---|---|
| Other/unknown race (reference: white) | −3.39 | −6.63 – −0.15 |
| Ambulance arrival | −7.2 | −10.2 – −4.1 |
| NIHSS (per +5 points) | −1.00 | −2.0 – −0.1 |
| Post-intervention treatment time | −5.38 | −8.02 – −2.74 |
Significant predictors shown; other covariates included: age, sex, race, diabetes, valvular disease, onset location, onset-to-arrival time, elevated blood pressure on presentation, weekend presentation; hospital: intervention/control, stroke center status, stroke volume.
Figure 2.
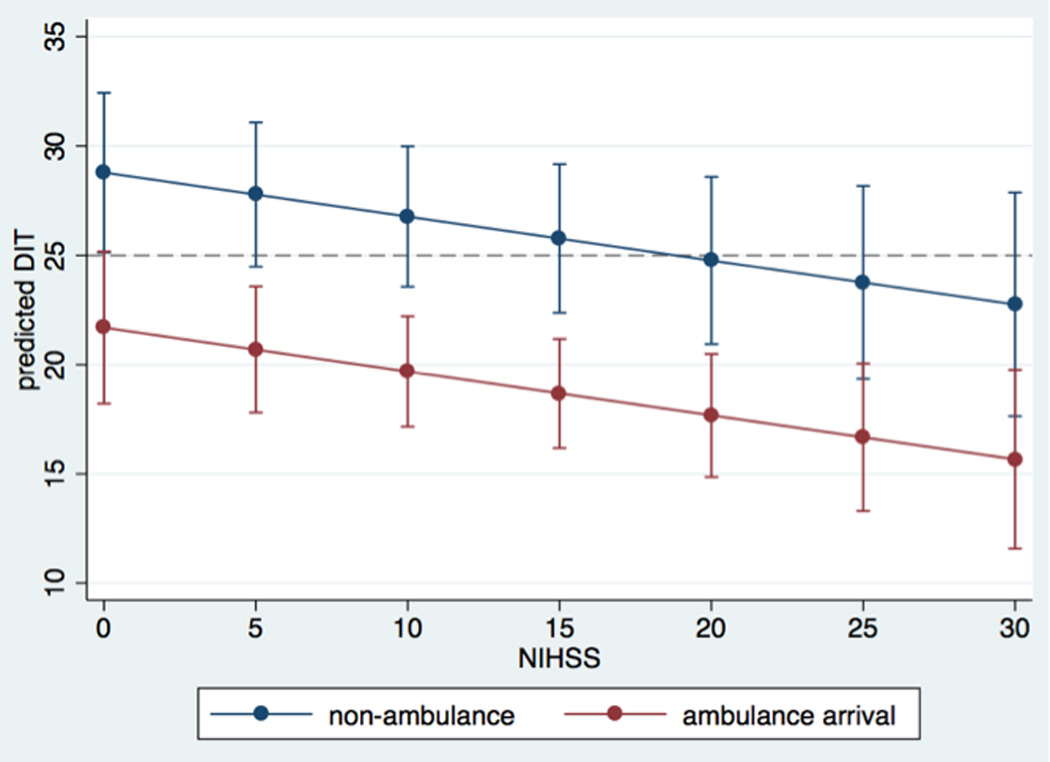
Predicted Door-to-imaging time (DIT) by Stroke Severity and Ambulance Arrival
*Predicted values based on model with all other predictors constant.
Bars: 95%CI around predicted values
DISCUSSION
We found that a targeted educational intervention aimed to improve acute stroke care and emergent tPA delivery had no effect on hospitals’ DIT performance. While we found no difference between control and intervention hospitals’ change over time, both groups showed similar significant improvements. This finding, in a sample deliberately selected for broader generalizability,4 signals strongly for the effect of secular trends. This may be due to increasing awareness and better stroke recognition in the pre-hospital or ED settings, improvements in CT availability, increasing primary stroke center hospitals, the American Heart Association’s Get-with-the-Guidelines program, and national quality reporting incentives.5–7
We found a modest proportion of DIT variation attributable to hospital differences, yet this was not explained by stroke center status or stroke volume. As Figure 1 highlights, differences between hospitals are small and difficult to differentiate. Examination of a larger sample of hospitals and hospital characteristics may better identify actionable targets for DIT.
Consistent with previous reports, stroke severity and ambulance arrival were strong predictors of DIT.3,8 The magnitude of the relationship between ambulance arrival and DIT reaffirms the importance of the pre-hospital and triage settings as targets for improving quality and reducing delays.
Our focus on DIT only among tPA-treated patients was an inherent limitation of the original study design, but may have created bias by excluding untreated patients. We also excluded patients with missing DIT, but this small group of patients was similar to included patients. Finally, we could not assess several potential predictors of DIT, including background quality improvement initiatives, stroke registry participation, EMS pre-notification, or temporal changes in telemedicine or imaging capabilities.
CONCLUSION
Although the targeted educational intervention of the INSTINCT trial did not appear to improve DIT, we found that DIT performance is improving over time. Better understanding of the trends in DIT and reasons for DIT variation across hospitals will have important quality improvement and policy implications.
Supplementary Material
Acknowledgments
Funding Sources: Parent study funded by the NIH National Institute of Neurologic Disorders and Stroke grant R01-NS-050372.
Dr. Levine is funded by NIH K23 AG040278 and received support from NIH P30DK092926.
Footnotes
Disclosures: None
REFERENCES
- 1.Schumacher HC, Bateman BT, Boden-Albala B, Berman MF, Mohr JP, Sacco RL, et al. Use of thrombolysis in acute ischemic stroke: Analysis of the nationwide inpatient sample 1999 to 2004. Annals of emergency medicine. 2007;50:99–107. doi: 10.1016/j.annemergmed.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 2.Kelly AG, Hellkamp AS, Olson D, Smith EE, Schwamm LH. Predictors of rapid brain imaging in acute stroke: Analysis of the get with the guidelines-stroke program. Stroke; a journal of cerebral circulation. 2012;43:1279–1284. doi: 10.1161/STROKEAHA.111.626374. [DOI] [PubMed] [Google Scholar]
- 3.Jauch EC, Saver JL, Adams HP, Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the american heart association/american stroke association. Stroke; a journal of cerebral circulation. 2013;44:870–947. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- 4.Scott PA, Meurer WJ, Frederiksen SM, Kalbfleisch JD, Xu Z, Haan MN, et al. A multilevel intervention to increase community hospital use of alteplase for acute stroke (instinct): A cluster-randomised controlled trial. Lancet neurology. 2013;12:139–148. doi: 10.1016/S1474-4422(12)70311-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prabhakaran S, McNulty M, O'Neill K, Ouyang B. Intravenous thrombolysis for stroke increases over time at primary stroke centers. Stroke; a journal of cerebral circulation. 2012;43:875–877. doi: 10.1161/STROKEAHA.111.640060. [DOI] [PubMed] [Google Scholar]
- 6.Schwamm LH, Fonarow GC, Reeves MJ, Pan W, Frankel MR, Smith EE, et al. Get with the guidelines-stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation. 2009;119:107–115. doi: 10.1161/CIRCULATIONAHA.108.783688. [DOI] [PubMed] [Google Scholar]
- 7.Hospital outpatient quality reporting specifications manual, v6.0b. Quality Net. 2013 http://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FSpecsManualTemplate&cid=1228772438492.
- 8.Abdullah AR, Smith EE, Biddinger PD, Kalenderian D, Schwamm LH. Advance hospital notification by ems in acute stroke is associated with shorter door-to-computed tomography time and increased likelihood of administration of tissue-plasminogen activator. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2008;12:426–431. doi: 10.1080/10903120802290828. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


