Recent trends show that a concerning number of individuals are using prescription opioids for non-medical reasons, but there is a lack of research addressing treatment response (e.g., engagement, retention, and substance use during treatment) for these individuals. The number of individuals who misuse prescription opioids is much greater than the number of heroin users. National estimates for 2006 – 2008 showed approximately 460,000 people over 12 years old using heroin in the past year, but over 12 million non-medical users of pain relievers (Office of Applied Studies, 2010). Estimates for Florida for 2006 – 2008 showed a greater misuse of prescription opioids: about 10,000 people using heroin vs. more than 600,000 non-medical users of pain relievers (Office of Applied Studies, 2010).
With this sizeable number of individuals misusing prescription opioids the number of prescription opioid users in treatment has increased more than four-fold in a fourteen-year period in the U.S. (Substance Abuse and Mental Health Services Administration [SAMHSA], 2010). In one study of treatment for opioid dependence (Brands, Blake, Sproule, Gourlay, & Busto, 2004), less than a fifth of participants (17%) were users of heroin only, almost a quarter (24%) only prescription opioids, and more than half (57%) were users of both. In Florida, 1,413 individuals were admitted to substance abuse treatment for primary heroin use in 2007, but 4,400 were admitted for primary use of other opioids (SAMHSA, 2010). By 2010, the change in these numbers was striking. Although the number of primary heroin users did not change much, with 1,645 reporting primary heroin use, the number of primary users of other opioids more than doubled to 11,950 (SAMHSA, 2010). Highlighting the extent of prescription opioid misuse, these substances now account for 16% of treatment admissions for substance use disorders in Florida, surpassed by only alcohol and marijuana (SAMHSA, 2010).
Given the levels of prescription opioid misuse, the frequency of combined heroin and prescription opioid misuse, and the increases in prescription opioid users being admitted to treatment, an evaluation of treatment response of patients misusing, abusing, or dependent on prescription opioids is paramount. Treatments, e.g., methadone maintenance, have been shown to be effective for heroin users in large naturalistic studies across a number of locales (Gossop, Marsden, Stewart, Edwards, Lehmann, Wilson, & Segar, 1997; Hubbard, Craddock, Flynn, Andeson, & Etheridge, 1997; Teeson, Ross, Darke, Lynskey, Ali, Ritter, & Cooke, 2006). One recent randomized trial (Weiss et al., 2011) showed that prescription opioid users had reduced opioid use while on buprenorphine-naloxone treatment, although use increased after tapering off the medication. However, few studies have examined whether prescription opioid users engage in methadone maintenance or other treatments at similar rates to heroin users, or whether prescription opioid users have comparable retention or reductions in opioid use to heroin users (Magura, 2009).
There are several reasons to believe that individuals who misuse prescription opioids may have equivalent, or better, treatment response than primary heroin users. Studies have shown that prescription opioid users are more likely to report higher levels of formal education and income than heroin users (e.g., Rosenblum et al., 2007). These characteristics have been associated with better outcomes in treatment outcome studies (e.g., Trafton, Oliva, Horst, Minkel, & Humphreys, 2004). One study showed that prescription type opioid users had similar rates of retention in methadone maintenance programs as primary heroin users (Banta-Green, Maynard, Koepsell, Wells, & Donovan, 2009). Similar rates of retention is one indicator of a similar response to treatment, but to our knowledge no studies have examined whether there are differences in other indicators of treatment response, e.g., engagement or abstinence, in addition to retention for prescription opioid users. Although Banta-Green and colleagues (2009) examined retention of prescription opioid users in methadone maintenance treatment, to our knowledge no studies have examined their relationship to engagement or abstinence with prescription opioid users. As noted above, many characteristics of prescription opioid users may differ from heroin users. Banta-Green and colleagues (2009) controlled for differences in several factors, including mental and physical health, baseline severity of substance use, family/social factors, and recent arrests, when examining differences in retention. Statistically controlling for these factors allowed the authors to draw stronger inferences about the relationship between prescription opioid use and retention.
The purpose of this study was to add to the knowledge base about service utilization of opioid users in ATR, as well as comparing the treatment response of prescription opioid users to heroin users. Three primary research questions about treatment response were examined and three indicators of treatment response were used. First, did prescription opioid users have different rates of engagement into treatment as heroin users? Second, did prescription opioid users have different treatment retention? Third, did prescription opioid users have different rates of opioid abstinence? We also examined whether any differences in engagement, retention, or opioid abstinence were associated with the type of opioid use or other variables, such as demographics and mental and physical health, baseline severity of substance use, family/social factors, and recent arrests.
Methods
Setting and Participants
The data for this study were collected as part of an evaluation of the Access to Recovery (ATR) program in Florida. ATR was a federal initiative from SAMHSA targeting underserved populations by providing vouchers to pay for an array of treatment and recovery support services selected by participants (e.g., Washington State; Krupski, Campbell, Joesch, Lucenko, & Roy-Byrne, 2009). In Florida, ATR was implemented from 2004 to 2007 in 20 counties that were selected to represent the diversity of the overall population of the state. Efforts were made to target individuals involved with the criminal justice system, child welfare system, and with co-occurring disorders. A total of 274 provider agencies participated in ATR; 14 of these provided methadone and/or buprenorphine maintenance treatment. Of the 11,955 ATR participants identified as part of an evaluation study (Author, 2008), 1,648 (14%) reported use of opioids in the thirty days before intake. Unlike controlled trials, participants in this study could have different lengths of treatment that corresponded to different amounts of service vouchers. Specifically, participants would receive vouchers for 30 days of service, then have a clinical review, and then could receive vouchers for an additional 30 days of services, followed by a second clinical review, and so on. Available service voucher data indicated that 1,114 (68%) received vouchers for services through 30 days into treatment, 644 (39%) through 60 days, and 301 (27%) more than 60 days. The proportion of users of different types of opioids who were assessed at the three clinical review points was equivalent to the overall proportions in the larger sample, which suggested the data could be combined.
Procedures
Initial assessments determined participant eligibility and the kinds of services needed. Eligibility was determined by assessors who were independent of the provider and administration agencies. The assessors conducted a comprehensive evaluation of service needs using the Addiction Severity Index and then determined level of care using the American Society of Addiction Medicine (ASAM) Patient Placement Criteria (Florida Department of Children and Families, 2006). The client reviewed multiple provider profiles for the recommended services. Assessors explained the information contained in the profiles to ensure an educated choice, and the client chose service providers. Each of the providers selected by the client was alerted via a web-based data system to the range of approved services on a voucher. Providers were able to request changes to the voucher on the clients’ behalf at any point during the episode of care. Informed consent from participants was obtained by service providers following the guidelines of the Florida Department of Children and families. The consent included a description of the data to be collected and how the data will be kept private. To ensure responses were kept private and confidential, data was directly routed from providers to the evaluation team through a protected server and no identifying information was tracked by the evaluation team. Data for the current study were collected during the initial assessment, and then through reviews of clinical progress conducted 30 days after intake, 60 days after intake, and every subsequent 60-day interval through the point of discharge. Data on abstinence was taken from the latest review available for each participant; the differing lengths of review periods by individual participants were controlled statistically in analyses. It should be noted that the differing endpoints where assessments occurred was because participants were assessed only if they continued to receive services within the ATR program. Participants may have received services outside the ATR program, but information on such services was not captured. Data were collected at the time services were completed (at a clinical review), but there was no subsequent follow-up data collection. This differed from clinical trials follow-up assessment strategies, in which researchers would attempt to collect data at the same timepoints for all participants. ATR was designed as a brief, time-limited program, so it was expected that the numbers of participants who received vouchers for a longer period of time and provided data at later timepoints would be significantly smaller. Assessors collected baseline information via the intake process; subsequent reviews were done by vouchered service providers.
Measures
Opioid Use Type
Participants were assigned to one of three groups based on self-reported opioid use in the 30 days before intake: prescription opioids only (PO), heroin only (HO), or both heroin and prescription opioids (H&P). We use the term “prescription” to refer to the type of opioid, which may not necessarily have been obtained with a prescription. These opioid type groups are similar to empirically identified opioid users described in past studies of methadone maintenance (Brands et al., 2004; Wu, Woody, Yang, & Blazer, 2011). Although Brands and colleagues (2004) described four groups the current data did not allow us to determine the temporal precedence of heroin or prescription opioid misuse, so a single mixed use category was used. Opioid use type were taken from the Addiction Severity Index (ASI; McLellan, Luborsky, Woody, & O’Brien, 1980) which was only administered at baseline by trained assessors. It is important to note that the experience of drug users regardless of substance used, manner of use, pattern of use, meanings attributed to substance use are best described as heterogeneous group. The types of use used in this study are a single dimension of interest, and is not meant to imply that these are homogenous groups in other ways.
Engagement into Treatment
Engagement into treatment was defined as a participant receiving at least two units of any service. This definition of engagement is consistent with past intervention engagement research (Prado, Szapocznik, Mitrani, Mauer, Smith, & Feaster, 2002; Author, 2011; Mitrani, Prado, Feaster, Robinson-Batista, & Szapocznik, 2003; Author, 1996; Author, 2001). Note that even though treatment alliance may be related to engagement, the alliance was not directly measured in this study. Treatment services were derived from ATR service vouchers that were redeemed. Vouchers included the date of service, number of units of a service (e.g., methadone doses), and U.S. dollar-cost of services received. As the current study focused on methadone maintenance treatment, the analyses reported here coded services as either methadone maintenance, buprenorphine maintenance, or other non-mainteance treatment (clinical treatment and/or recovery support). Clinical treatment services were services that addressed specific treatment needs and were provided by credentialed professionals. Recovery support services were community services provided by non-credentialed staff. Providers were certified by DCF-ATR staff following on-site reviews. In the current study, receiving at least two units of methadone was defined as engaging in methadone maintenance; receiving at least two units of other non-maintenance services and fewer than two of methadone maintenance was defined as engaging in other services; receiving at least two units of buprenorphine and fewer than two units of methadone or other services was defined as engaging in buprenorphine; and not engaged was defined as receiving fewer than two units of any service.
Retention
Retention in treatment was defined as participation in a scheduled review of clinical progress after the initial intake. Reviews of clinical progress were conducted by service providers 30 days after intake, 60 days after intake, and every subsequent 60-day interval through the point of discharge. Thus, to be retained, a participant had to remain in the ATR program for at least 30 days and participate in clinical review, regardless of the amount of treatment services that were actually received. Participants who were retained were coded as 1, and those not retained were coded as 0.
Opioid Abstinence
Abstinence from opioids the past 30 days in the current study was taken from the self-reported drug use section in on the Government Performance and Results Act (GPRA) instrument administered during the clinical review periods at 30 days post-intake, 60 days post-intake, and every 60 days thereafter. GPRA was initially adopted by the U.S. Congress in 1993 to ensure accountability of program outcome grants. Since then, many programs have adopted a GPRA instrument to collect client outcomes. Although this instrument was not designed for research, it is similar to clinical assessments in many treatment programs. Participants who reported any use of opioids (heroin or non-medical use of prescription opioids) during a 30-day period at the last clinical review point available were coded as not abstinent (1); participants who reported no use of opioids were coded as abstinent (0).
Control Variables
These variables were selected to parallel Banta-Green and colleagues (2009). Control variables were taken from several sections (psychiatric, medical, family/social, and employment, and some items from the alcohol and drug section) of the ASI administered at intake. For the current study, dichotomous items were used to assess current employment (full-time vs. not full-time), relationship status (married/cohabitating vs. not), any psychiatric treatment in the last 30 days (vs. none), any chronic medical problems (vs. none), living with a user of alcohol or drugs (vs. not), and housing status (homeless vs. not homeless). All of these variables were coded as 0 = no/absent, 1 = yes/present. Injection drug use was assessed, but not used for analyses because injecting almost completely overlapped with only heroin use. Gender (male vs. female), education, minority ethnicity (vs. White), self-reported intake level of opioid use in the past 30 days, and age were taken from the GPRA instrument administered at the initial assessment.
Analysis Plan
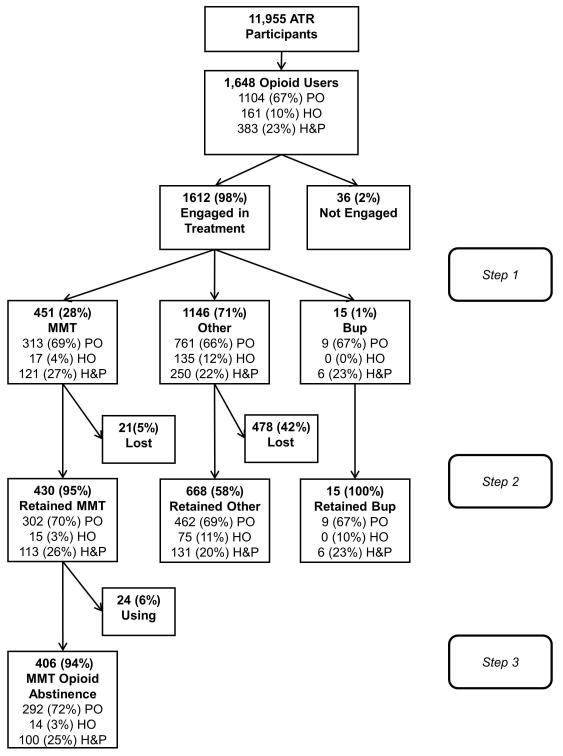
Preliminary ANOVA and chi-square analyses in SPSS 18 were used to determine whether there were significant differences in a number of characteristics (e.g., demographics, baseline level of opiate use) between the types of opioid users (HO vs. PO vs. H&P). Analysis of the research questions was divided into three steps: 1) multinomial regression analyses for engagement into treatment, 2) logistic regression for retention, and 3) logistic regression for opioid abstinence. Multinomial regression analyses are used with a dependent variable that is polytonomous, i.e., for variables that have multiple categories. In comparison, logistic regressions are used with a dichotomous dependent variable. A significant predictor in multinomial analyses may be interpreted in a similar way to a logistic regression predictor: 1) there is a relationship between the predictor and dependent variable and 2) odds of being in a particular level of the dependent variable increase (or decrease) in comparison to one other level of the dependent variable (the reference group). The figure shows participants that were included in each analysis step.
Figure.
Number of participants in each analysis step. MMT = Methadone maintenance treatment. Bup = Buprenorphine maintenance treatment. Other = Treatment other than maintenance medication. PO = Prescription opioid. HO = Heroin only. H&P = Heroin and prescription opioids. Participants chose their treatment and received vouchers to remunerate service providers.
In the first step, engagement into treatment was entered as the dependent variable, and opioid use type (PO vs. HO vs. H&P) as the independent variable. Engagement into treatment had four levels that reflected the three treatment modalities: methadone maintenance (comparison group), buprenorphine maintenance, and other treatment; and not engaged (i.e., only one session or no sessions attended). A separate analysis examined the effect of controlling for characteristics that were significantly different in the initial analyses by entering the control variables in a first block followed by opioid use type in a second block. In the second step, retention was entered as the dependent variable, and opioid use type as the independent variable. Only participants that engaged into treatment were included in this step. A separate analysis examined the effect of controlling for characteristics that were significantly different in the initial analyses by entering these variables and engagement into treatment in a first block followed by opioid use type in a second block. In the third step, opioid abstinence was entered as the dependent variable, and opioid use type as the independent variable. Only participants in methadone maintenance were included in this step due to the low n in buprenorphine maintenance and the low retention in other treatment. A separate analysis examined the effect of controlling for characteristics that were significantly different in the initial analyses by entering the control variables, amount of services and dosage, and review period in a first block followed by opioid use type in a second block. The number of methadone doses received, amount of other services received, and the timing of the clinical review were also entered in the first block to control for differing amounts of treatment received and differing time frames that participants spent in treatment until the clinical review.
Results
Preliminary Analyses
Participants were divided into three groups based on the reported type of opioid use 30 days before intake. The three groups were only heroin users (HO; n = 161, 10%), only prescription opioid users (PO; n = 1104, 67%), and users of both heroin and prescription opioids (H&P; n = 383, 23%). As shown in Table 1, there were significant differences in age, baseline opioid use, gender, ethnicity, psychiatric treatment, chronic medical conditions, and homelessness between the three groups. Post-hoc Bonferroni tests showed that H&P had a significantly greater level of baseline opioid use of than either PO or HO.
Table 1. Characteristics of Participants based on Opioid Use Type on Intake (N = 1648).
| Characteristic | PO (n = 1104) | HO (n = 161) | H&P (n = 383) | p | |||
|---|---|---|---|---|---|---|---|
| Baseline opioid use (days), M, SD | 14.92 | 11.13 | 12.71 | 10.54 | 17.08 | 9.54 | <.001 |
| Age, years, M, SD | 34.65 | 10.04 | 34.59 | 9.28 | 32.87 | 9.35 | .009 |
| Education, years, M, SD | 11.83 | 2.14 | 11.78 | 2.51 | 11.73 | 2.12 | .705 |
| Gender (Male), n, % | 664 | 60% | 126 | 78% | 252 | 66% | <.001 |
| Minority Ethnicity, n, % | 109 | 10% | 53 | 33% | 62 | 16% | <.001 |
| Employed (full-time) , n, % | 128 | 12% | 11 | 7% | 43 | 11% | .195 |
| Married/cohabitating, n, % | 419 | 38% | 69 | 43% | 143 | 37% | .444 |
| Psychiatric treatment (last 30 days) , n, % | 679 | 62% | 76 | 47% | 210 | 55% | < .001 |
| Chronic medical problems, n, % | 507 | 46% | 57 | 35% | 136 | 36% | <.001 |
| Homeless, n, % | 361 | 33% | 79 | 49% | 135 | 35% | <.001 |
| Has children, n, % | 576 | 52% | 84 | 52% | 174 | 45% | .069 |
| Lives with user (alcohol or drugs) , n, % | 193 | 17% | 26 | 16% | 65 | 17% | .905 |
Note: n is number of positive responses.
Engagement
For the multinomial regression analysis the outcome variable was engagement with four levels: 1) those engaged into other (non-maintenance) services, 2) those not engaged, and 3) those engaged in buprenorphine maintenance; and participants engaged into methadone maintenance as the comparison group. This comparison group was chosen to allow a comparison of predictors of engagement into methadone maintenance to other kinds of treatment. Across all services the majority of each of the three groups engaged in treatment: 1083 (98%) in PO, 152 (94%) in HO and 377 (98%) in H&P. There were no significant differences in engagement between PO and H&P. However, compared to PO, HO were significantly less likely to engage in methadone maintenance treatment, B = 2.07, SE = 0.47, p < .001, OR = 7.89, and more likely to engage into other non-maintenance services, B = 1.18, SE = 0.27, p < .001, OR = 3.27. No HO engaged in buprenorphine maintenance. As shown in Table 2, after controlling for age, baseline opioid use, gender, ethnicity, psychiatric treatment, chronic medical conditions, and homelessness, HO remained significantly less likely to engage in methadone maintenance treatment, than PO, and more likely to engage in other non-maintenance treatment. Those with greater baseline opioid use, recent psychiatric treatment, a chronic medical condition, and that were homeless were more likely to engage in in methadone maintenance than other services.
Table 2. Multinomial Predictors of Engagement into Treatment of Opioid Users (N = 1648).
| Other Treatment (n = 1146) | Buprenorphine (n = 15) | Not Engaged (n = 36) | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Variable | B | SE | p | B | SE | p | B | SE | p |
| Intercept | 1.92 | 0.28 | <.001 | −5.02 | 1.58 | <.001 | −2.43 | 0.78 | .002 |
| Baseline opioid use | −0.07 | 0.01 | <.001 | 0.08 | 0.04 | .076 | −0.03 | 0.02 | .047 |
| Age, years | −0.01 | 0.01 | .100 | −0.03 | 0.03 | .371 | 0.02 | 0.02 | .252 |
| Male | 0.16 | 0.13 | .225 | 0.28 | 0.56 | .611 | 0.16 | 0.39 | .683 |
| Minority | 0.01 | 0.20 | .957 | --b | -- | -- | −0.59 | 0.58 | .313 |
| Psychiatric Treatment | 0.32 | 0.13 | .013 | 0.55 | 0.57 | .333 | −0.18 | 0.36 | .629 |
| Chronic Medical Problems | −0.30 | 0.13 | .023 | 0.38 | 0.55 | .489 | −1.06 | 0.42 | .011 |
| Homeless | 1.60 | 0.16 | <.001 | --b | -- | -- | 0.57 | 0.44 | .196 |
| HO (vs. PO) | 0.97 | 0.29 | <.001 | --b | -- | -- | 2.00 | 0.50 | <.001 |
| H&P (vs. PO) | −0.17 | 0.15 | .244 | 0.68 | 0.56 | .225 | −0.37 | 0.48 | .443 |
Note: Too few cases to estimate. Negative B coefficient indicates more likely to engage in methadone maintenance than comparison. 451 participants engaged in methadone maintenance.
Retention
Of the 1,612 participants that were identified as opioid users at intake and who engaged in some form of treatment, 1,113 (69%) were retained. Without controlling for other variables, PO were significantly more likely to be retained than HO, B = −0.54, SE = 0.18, p = .002, OR = 0.58, but not than H&P, B = −0.24, SE = 0.13, p = .067, OR = 0.79. Participants engaged in maintenance treatments had much better retention rates, specifically 430 (95%) of participants who engaged into methadone maintenance, and all 15 (100%) participants who engaged into buprenorphine maintenance, were retained. In comparison, 668 (58%) participants who engaged into non-maintenance treatments were retained. Due to lack of variability among cases engaged in buprenorphine maintenance, these cases were not included in the subsequent analysis with control variables. As shown in Table 3, after controlling for baseline opioid use, age, gender, ethnicity, psychiatric treatment, chronic medical conditions, homelessness, as well as engagement, there was no significant difference in retention between HO and PO, B = −0.23, SE = 0.19, p = .231. Engagement into other services (vs. methadone maintenance) was significantly related to retention, B = −2.82, SE = 0.24, p < .001, OR = 0.06, and no other controls were significant, suggesting that this explained the difference in retention between HO and PO. It should also be noted that after including the other control variables into the regression equation, H&P were significantly less likely to be retained than PO, B = −0.29, SE = 0.15, p = .042, OR = 0.75.
Table 3. Logistic Regression Predicting Retention for Participants Engaged in Methadone Maintenance Treatment and Other Treatments (N = 1597).
| Variable | B | SE | p |
|---|---|---|---|
| Baseline opioid use | −0.01 | 0.01 | .054 |
| Age, years | 0.01 | 0.01 | .071 |
| Male | −0.05 | 0.13 | .668 |
| Minority | −0.12 | 0.17 | .472 |
| Psychiatric Treatment | 0.08 | 0.12 | .501 |
| Chronic Medical Problems | 0.02 | 0.13 | .866 |
| Homeless | 0.14 | 0.12 | .273 |
| Engaged in other treatments (vs methadone) | −2.80 | 0.24 | <.001 |
| HO (vs. PO) | −0.23 | 0.19 | .231 |
| H&P(vs. PO) | −0.29 | 0.15 | .042 |
| Constant | 2.95 | 0.34 | <.001 |
Note: Negative B coefficient indicates less likely to be retained in treatment.
Abstinence
Due to the small number of cases in buprenorphine maintenance and the large proportion of cases in other treatments with missing abstinence data at the clinical review, only data from individuals engaged in methadone maintenance were used in the following analyses. Most (406, 94%) participants who were retained in methadone maintenance treatment reported abstinence from opioids during the 30 days before their clinical review. Of the participants who were retained in methadone maintenance, 292 (72%) were PO, 14 (3%) were HO, and 100 (25%) were H&P. For participants retained in methadone maintenance, there was no significant difference in the number of methadone doses between PO (M = 102.63, SD = 46.49), HO (M = 85.13, SD = 48.51), and H&P(M = 96.44, SD = 49.12), F (2, 429) = 1.52, p = .221, or the number of other services between PO (M = 6.88, SD = 8.86), HO (M = 14.10, SD = 18.27), and H&P (M = 6.92, SD = 9.76), F (2, 429) = 2.83, p = .060. (The number of other services was log-transformed for the ANOVA to account for positive skew, but the actual means are shown). Despite the absence of significant differences, methadone dosage, amount of other services received, and the timing of the clinical review were included as controls in the logistic regression analysis to ensure that these variables did not account for the differences between groups. Although tests did not reach statistical significance, these variables were included as controls because dosage is a well-known predictor of treatment response.
H&P had significantly lower odds of opioid abstinence than PO, B = −1.33, SE = 0.44, p = .002, OR = .26. This translates to over three times the odds of abstinence for PO compared to H&P. HO, B = −0.74, SE = 1.08, p = .498, OR = .48, did not have statistically significantly different odds from PO, but had about half the odds of abstinence of PO. As shown in Table 4, after controlling for baseline opioid use, gender, ethnicity, psychiatric treatment, chronic medical conditions, homelessness, as well as review point and dosage of methadone and other services, opioid use type remained significantly related to abstinence, with H&P having lower odds of abstinence than PO.
Table 4. Logistic Regression Predicting Opioid Abstinence at Post-intake Review for Participants Engaged in Methadone Maintenance Treatment (N = 451).
| Variable | B | SE | p |
|---|---|---|---|
| Baseline opioid use | 0.02 | 0.02 | .441 |
| Age, years | 0.02 | 0.03 | .574 |
| Male | 0.05 | 0.50 | .913 |
| Minority | 0.39 | 0.72 | .583 |
| Psychiatric Treatment | 0.74 | 0.50 | .135 |
| Chronic Medical Problems | −0.25 | 0.52 | .626 |
| Homeless | −0.72 | 0.60 | .225 |
| Review 2 (vs. Review 1) | 0.91 | 1.05 | .386 |
| Review 3 (vs. Review 1) | 1.57 | 1.37 | .253 |
| Methadone doses | 0.01 | 0.01 | .177 |
| Other Services | −0.01 | 0.02 | .552 |
| HO (vs. PO) | −0.32 | 1.24 | .797 |
| H&P(vs. PO) | −1.25 | 0.49 | .011 |
| Constant | 0.27 | 1.37 | .841 |
Note: Negative B coefficient indicates less likely to report abstinence from opioids. Review 1 was 30 days post-intake. Review 2 was 60 days post-intake. Review 3 refers to reviews 120 days or more post-intake.
Discussion
This study compared treatment response of three groups of opioid users: prescription only users (PO), heroin only users (HO), and users of both heroin and prescription opioids (H&P). Although the number of prescription opioid users has been growing rapidly, particularly in Florida, very few studies have examined whether prescription opioid users have equivalent responses to treatment as heroin users. Three indicators of treatment response (engagement into treatment, retention, and abstinence from opioids during treatment) were used. Most (98%) Access to Recovery (ATR) participants who reported opioid use engaged into some type of treatment. A possible explanation for the strong positive engagement response is that individuals who entered the ATR program were initially more highly motivated to participate in treatment. Consistent with the objectives of the ATR program, higher motivation may have been related to increased client choice in treatment, as well as a structured and systematic process for linking clients to services. Another possibility is that the process of seeking approval and maintaining funding for treatment necessarily excluded most individuals who were ambivalent about treatment and would not have engaged in treatment services.
It is important to note that engagement, retention, and outcome are influenced by therapist qualities, program or treatment quality, and significant others in the participant’s social networks and communities. None of these meaningful factors were considered in this study, but should be accounted for in future studies. Further, there are many evidence-based interventions for opiate use and current best practices suggest that a comprehensive drug abuse treatment will have therapeutic activities that focus on treating the substance use disorder including therapy, case management, assessment and treatment planning, pharmacotherapy, self-help groups, substance use monitoring, and continuing care, and ancillary services to address family problems, child care, vocational, mental health, medical, educational, HIV/AIDS, legal, financial, housing/transportation (National Institute of Drug Abuse, 2009). The specific mix of therapeutic activities and other services should be tailored to meet the needs of individuals. Examining the match between individual needs to the therapeutic and other services offered and/or received by each individual, was beyond the scope of the current investigation.
HO were slightly less likely to engage in methadone maintenance treatment or more likely to engage in other non-maintenance treatments compared to PO. The current study was not able to determine why HO were less likely to engage in methadone maintenance treatment. Just over half (56%) of HO who engaged into other treatments were retained, but a large majority (88%) of HO who engaged into methadone maintenance were retained. Most (93%) H&P were retained in methadone maintenance, all (100%) in buprenorphine, and about half (52%) in other treatments were retained. Although the difference in retention was a non-significant trend in the initial analysis, the difference was statistically significant after control variables were included in the regression model. This effect is known as a “suppression” (MacKinnon, Krull, & Lockwood, 2000) and can occur in some cases when a “third” variable is added into a regression equation. We interpreted these results to mean that the worse retention of H&P compared to PO was only apparent after we considered engagement into treatment. In other words, we would not have been able to detect this difference if we had not controlled for engagement into treatment.
Given the poor retention in other treatments, it was not possible to make definitive conclusions about abstinence rates for participants who engaged in treatments besides methadone maintenance. The other treatment category was quite heterogeneous. The reasons for the low retention are not clear, but understanding how to better meet participants’ needs across many kinds of treatment is an important question for future treatment development. The high retention rates in methadone maintenance allowed us to make stronger conclusions about abstinence of participants this group. Of participants in methadone maintenance, H&P were less likely to be abstinent from opioids, than PO. This difference remained statistically significant after controlling for several variables. Although the level of opioid use before intake was included as a proxy for severity, we cannot rule out the possibility that H&P also had more intractable problems or severe dependence. Examining the combined effect of maintenance medication and psychosocial services was beyond the scope of this study, but future studies should examine additional characteristics that might mediate or moderate abstinence and that can inform treatment enhancement and/or motivation/engagement efforts. Previous research has identified several variables related to treatment outcome for opioid users that are possible mediators, but were not included in this study. Among these variables are the level of use of non-opioid illicit drugs or alcohol, craving, severity of psychiatric or withdrawal symptoms, and marital satisfaction (e.g., Homish, Leonard, & Cornelius, 2010). Qualitative studies about reasons for using particular types of opioids, as well as experiences in treatment, might suggest other possible mediators.
Taken together, the results of this study indicate that PO had a better response to treatment than either HO or H&P. That is, PO were more likely to engage in methadone maintenance than HO, which led to better retention in treatment, and likely better abstinence. Although H&P did not have significantly lower engagement into methadone maintenance, there was evidence for lower retention in treatment and less abstinence during treatment. These data suggest that treatment development/enhancement efforts (Rounsaville, Carroll, & Onken, 2001) may be needed to address polydrug use. First, it may be beneficial identify ways to increase engagement of HO into maintenance treatment and/or to improve retention in other treatments. Second, efforts to improve outcomes for individuals struggling with both heroin and prescription opioid use are needed. One possibility is to enhance maintenance treatments for the subgroup of patients that use prescription opioids and heroin.
This study identified several factors that might be examined in future studies of avenues for treatment enhancement efforts. Individuals with recent history of psychiatric treatment or who were homeless were more likely to engage in other services than in methadone maintenance. It is likely that these individuals with positive psychiatric history received vouchers for psychotherapy and/or psychiatric medication and those who were homeless received vouchers for housing assistance. Based on clinical impressions of ATR staff, the psychiatric services that were offered may have been more important to clients because they provided a quick sense of stability and comfort. Given the evidence of treatment effectiveness for those who engaged in methadone maintenance, it may be beneficial to combine psychiatric or housing services with methadone maintenance programs to meet the needs of patients with multiple needs characteristics. Future studies should address the feasibility of such combinations. Participants with chronic medical conditions were more likely to engage in methadone maintenance than with other services. Chronic medical conditions, specifically those conditions with chronic pain that require longer-term administration of analgesics, have been linked to abuse of opioids (e.g., Compton & Volkow, 2006). It is possible that individuals with chronic medical conditions were attracted to methadone maintenance to reduce pain, as has been reported in previous studies (e.g., Rosenblum et al., 2007). This link reinforces the notion that individuals with chronic medical problems are a clinically important subgroup of opioid abusers, whose particular needs warrant further study.
Some limitations of this study should be noted when interpreting these results. Although the ATR program was designed to reflect individuals in treatment in Florida, the project did not sample randomly and only assessed a 30-day window before treatment intake. Proportions of the types of users in this report differed from previous research reports, which may limit generalizability of the results and recommendations of this study. In the current sample, 67% were PO, 10% were HO, and 23% were H&P. These numbers are consistent with the much greater numbers of people in Florida who use prescription opioids compared to heroin (SAMHSA, 2010), but the relative proportions of types of opioid users may differ widely in other locations. As a comparison, in a sample of opioid-dependent patients admitted to methadone maintenance treatment in Ontario, Canada, 24% were PO, 17% were HO, and 48% were H&P (Brands et al., 2004). This study used a broad definition of use that likely allowed more participants to be categorized as “users” than would a dependence diagnosis, which was not in this dataset. However, the results of this study were generally consistent with the results another study (Banta-Green, et al., 2009) that examined a sample with very different proportions of opioid users (12% PO, 88% heroin users) in methadone maintenance.
A complete analysis of the relationship between client choice and outcomes is needed, but beyond the scope of this study due to the absence of a comparison group that did not receive vouchers. Engagement into treatment was defined as two sessions or more of either clinical treatment or recovery support services. Although consistent with past research, other definitions of engagement could have been used. It is also important to note that this study was limited by the relatively short (i.e., less than a year) clinical review periods in the ATR program. Results from a longer period may have shown a worse retention or greater report of opioid use by participants. The GPRA was not designed to collect research data, and self-reports collected by service providers may have underestimated the prevalence of opioid use (U.S. General Accounting Office, 1998). Future studies should include additional measures, including laboratory assessments of opioid use, longer treatment durations, and processes for reviewing client progress post-discharge from treatment.
The data collection procedure in ATR collected only a small amount of information, which left many areas that may be relevant to treatment engagement, retention, and sustained positive outcomes unmeasured. Some additional information about the participant’s resources (strengths and limitations) for daily adaptation and functioning in a range of roles (including the patient role), networks, contexts, situations, and environments, their perceptions, judgments, and decisions, etc. Any of these could be assessed in future studies. Further, qualitative studies could provide more information about how people that misuse prescription opioid drugs view their lives and their experiences.
In conclusion, PO can be treated, particularly in methadone and buprenorphine maintenance programs, and have outcomes that are at least as good as, and likely better than, those of HO or H&P. Future clinical research may benefit from identifying the unique needs of subgroups of clients, e.g., those who misuse both prescription opioids and heroin, with chronic pain, with psychiatric symptoms, or who are homeless, to inform treatment improvement efforts. Information about the positive treatment response of PO, compared to the more-studied HO, is particularly important given the recent trends showing increasing numbers individuals who misuse prescription opioids in the general population and in treatment.
Acknowledgments
This research was funded by the Florida Department of Children and Families and the Substance Abuse and Mental Health Services Administration through the Access to Recovery. grant program (contract LD610). Support for this research was also received from the Center of Excellence for Health Disparities Research: El Centro, National Center on Minority Health and Health Disparities grant P60MD002266 (N. Peragallo, PI)and from the National Institute on Drug Abuse grant R01DA027920 (D. Santisteban, PI). The authors are solely responsible for this article’s content and do not necessarily represent the official views of any grantor agencies.
Contributor Information
Brian E. McCabe, Center of Excellence for Health Disparities Research: El Centro, School of Nursing and Health Studies, University of Miami, Coral Gables, FL, USA 33143.
Daniel A. Santisteban, Center of Excellence for Health Disparities Research: El Centro, School of Nursing and Health Studies, University of Miami, Coral Gables, FL, USA 33143.
Maite P. Mena, Center of Excellence for Health Disparities Research: El Centro, School of Nursing and Health Studies, University of Miami, Coral Gables, FL, USA 33143.
Darran M. Duchene, Access to Recovery Program; Florida Department of Children and Families, Substance Abuse and Mental Health Program Office, Tallahassee, FL, USA 32399.
Carali McLean, Central Florida Behavioral Health Network, Inc., Tampa, FL, USA 33619.
Marcia Monroe, Central Florida Behavioral Health Network, Inc., Tampa, FL, USA 33619.
References
- Banta-Green CJ, Maynard C, Koepsell TD, Wells EA, Donovan DM. Retention in methadone maintenance drug treatment for prescription-type opioid primary users compared to heroin users. Addiction. 2009;104:775–783. doi: 10.1111/j.1360-0443.2009.02538.x. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Brands B, Blake J, Sproule B, Gourlay D, Busto U. Prescription opioid abuse in patients presenting for methadone maintenance treatment. Drug and Alcohol Dependence. 2004;73:199–207. doi: 10.1016/j.drugalcdep.2003.10.012. [DOI] [PubMed] [Google Scholar]
- Compton WM, Volkov ND. Major increases in opioid analgesic abuse in the United States: concerns and strategies. Drug and Alcohol Dependence. 2006;81:103–107. doi: 10.1016/j.drugalcdep.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Florida Department of Children and Families . Florida Supplement to the American Society of Addiction Medicine Patient Placement Criteria for the Treatment of Substance-related Disorders. 2nd ed. Florida Department of Children and Families; Tallahassee, FL: p. 2006. [Google Scholar]
- Gossop M, Marsden J, Stewart D, Edwards C, Lehmann P, Wilson A,&, Segar G. The National Treatment Outcome Research Study in the United Kingdom: six-month follow-up outcomes. Psychology of Addictive Behaviors. 1997;11:324–337. [Google Scholar]
- Homish GG, Leonard KE, Cornelius JR. Individual, partner and relationship factors associated with non-medical use of prescription drugs. Addiction. 2010;105:1457–1465. doi: 10.1111/j.1360-0443.2010.02986.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubbard RL, Craddock SG, Flynn PM, Anderson J, Etheridge RM. Overview of 1-year follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS) Psychology of Addictive Behaviors. 1997;11:261–278. [Google Scholar]
- Krupski A, Campbell K, Joesch JM, Lucenko BA, Roy-Byrne P. Impact of Access to Recovery services on alcohol/drug treatment outcomes. Journal of Substance Abuse Treatment. 2009;37:435–442. doi: 10.1016/j.jsat.2009.05.007. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Krull JL, Lockwood CH. Equivalence of the mediation, confounding, and suppression effect. Prevention Science. 2000;1:173–186. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magura S. What more do we need to know about medication-assisted treatment for prescription-type opioid abusers? Addiction. 2009;104:784–785. doi: 10.1111/j.1360-0443.2009.02581.x. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O’Brien CP. An improved diagnostic evaluation instrument for substance abuse patients: The Addiction Severity Index. Journal of Nervous and Mental Disorders. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- Mitrani VB, Prado G, Feaster DJ, Robinson-Batista C, Szapocznik J. Relational factors and family treatment engagement among low-income, HIV+ African American mothers. Family Process. 2003;42:31–45. doi: 10.1111/j.1545-5300.2003.00031.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monga N, Rehm J, Fischer B, Brissette S, Bruneau J, El-Guebaly N, et al. Using latent class analysis LCA to analyze patterns of drug use in a population of illegal opioid users. Drug and Alcohol Dependence. 2007;881:1–8. doi: 10.1016/j.drugalcdep.2006.08.029. [DOI] [PubMed] [Google Scholar]
- National Institute of Drug Abuse . Principles of drug addiction treatment: a research-based guide. 2nd edition. U.S. Government Printing Office; Washington, DC: 2009. NIH publication NO.09-4180. [Google Scholar]
- Office of Applied Studies . Special Tabulations from the 2006-2008 National Surveys on Drug Use and Health. Substance Abuse and Mental Health Services Administration; 2010. [Google Scholar]
- Prado G, Szapocznik J, Mitrani VB, Mauer MH, Smith L, Feaster DJ. Factors influencing engagement into interventions for adaptation to HIV in African American women. AIDS and Behavior. 2002;6:141–51. doi: 10.1023/a:1015497115009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblum A, Parrino M, Schnoll SH, Fong C, Maxwell C, Haddox JD. Prescription-type opioid abuse among enrollees into methadone maintenance treatment. Drug and Alcohol Dependence. 2007;901:64–71. doi: 10.1016/j.drugalcdep.2007.02.012. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: Getting started and moving on from Stage I. Clinical Psychology: Science & Practice. 2001;8:133–142. [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Office of Applied Studies . The TEDS Report: Substance Abuse Treatment Admissions Involving Abuse of Pain Relievers: 1998 and 2008. Rockville, MD: 2010. [Google Scholar]
- Teeson M, Ross J, Darke S, Lynskey M, Ali R, Ritter A, Cooke R. One year outcomes for heroin dependence: findings from the Australian Treatment Outcome Study (ATOS) Drug and Alcohol Dependence. 2006;83:174–180. doi: 10.1016/j.drugalcdep.2005.11.009. [DOI] [PubMed] [Google Scholar]
- Trafton JA, Oliva EM, Horst DA, Minkel JD, Humphreys K. Treatment needs associated with pain in substance use disorder patients: implications for concurrent treatment. Drug and Alcohol Dependence. 2004;731:23–31. doi: 10.1016/j.drugalcdep.2003.08.007. [DOI] [PubMed] [Google Scholar]
- U.S. General Accounting Office . Drug abuse treatment: Data limitations affect the accuracy of national and state estimates of need. U.S. General Accounting Office; Washington, DC: 1998. [Google Scholar]
- Wu L, Woody GE, Yang C, Blazer DG. How do prescription opioid users differ from users of heroin or other drugs in psychopathology: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Addiction Medicine. 2011;5:28–385. doi: 10.1097/ADM.0b013e3181e0364e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss RD, Potter JS, Fiellin DA, Byrne M, Connery HS, Dickinson W, Ling W. Adjunctive counseling during brief and extended buprenorphine-naloxone treatment for prescription opioid dependence. Archives of General Psychiatry. 2001;68:1238–1246. doi: 10.1001/archgenpsychiatry.2011.121. doi:10.1001/archgenpsychiatry.2011.121. [DOI] [PMC free article] [PubMed] [Google Scholar]