Abstract
The objective of this systematic review was to investigate the effectiveness of interventions to improve medication adherence in ethnic minority populations. A literature search from January 2000 to August 2012 was conducted through PubMed/Medline, Web of Science, The Cochrane Library, and Google Scholar. Search terms used included: medication (MeSH), adherence, medication adherence (MeSH), compliance (MeSH), persistence, race, ethnicity, ethnic groups (MeSH), minority, African-American, Hispanic, Latino, Asian, Pacific Islander, and intervention. Studies which did not have ≥75% of the sample population comprised of individuals of any one ethnic background were excluded, unless the authors performed sub-group analyses by race/ethnicity. Of the 36 studies identified, 20 studies showed significant post-intervention differences. Sample population sizes ranged from 10 to 520, with a median of 126.5. The studies in this review were conducted with patients of mainly African-American and Latino descent. No studies were identified which focused on Asians, Pacific Islanders, or Native Americans. Interventions demonstrating mixed results included motivational interviewing, reminder devices, community health worker (CHW) delivered interventions, and pharmacist-delivered interventions. Directly observed therapy (DOT) was a successful intervention in two studies. Interventions which did not involve human contact with patients were ineffective. In this literature review, studies varied significantly in their methods and design as well as the populations studied. There was a lack of congruence among studies in the way adherence was measured and reported. No single intervention has been seen to be universally successful, particularly for patients from ethnic minority backgrounds.
Keyword: Medication adherence, compliance, intervention, ethnic minority
Introduction
In 2010, prescription drugs accounted for 10% of the $2.6 trillion spent on national health care. From 2009 to 2010, there was a 1.2% increase in prescription drug expenditures.1 Despite increases in prescription drug use, medication non-adherence presents a significant barrier to delivering appropriate health care. The definition of adherence is “the degree to which use of medication by the patient corresponds with the prescribed regimen.”2
The rate of non-adherence to prescription medication averages 50%, and has been estimated to range between 40% and 60%.2–4 As the patient's drug regimen becomes more complex, non-adherence increases. Patients on multiple medications are less likely to adhere to their regimen.3,5 Adherence to regimens in asymptomatic chronic conditions is especially important and difficult for patients.5
Medication non-adherence has many implications, including preventable disease progression, disease complications, reduced functional ability and quality of life, and death; in contrast, proper medication adherence is associated with lower mortality.2,6
Persons of racial and ethnic minority backgrounds face barriers to health care parity due to social, behavioral, and psychological issues not addressed by the Western biomedical model.7 Consequently these populations are disproportionately affected by health care disparities. While a 2003 Institute of Medicine report highlighted the needs of racial and ethnic minorities, a subsequent 2008 National Healthcare Disparities report revealed that gaps in health status persist.6 Medication adherence represents one of the barriers minority groups face in achieving optimal health care; additionally, there are a disproportionately small number of studies investigating methods to improve medication adherence for these groups.
There is a common misconception that medication adherence is the sole responsibility of the patient; however, medication adherence has multiple contributing and causative factors. The World Health Organization outlines five interacting dimensions affecting medication non-adherence: social/economic factors, therapy-related factors, patient-related factors, condition-related factors, and health system/health care team-related factors.2 Interventions should address such issues in order to positively impact medication adherence and thereby improve patient outcomes.
Interventions to improve medication adherence in these groups could contribute greatly to closing the health care gap that minorities face. The purpose of this study is to provide a systematic review of interventions to increase medication adherence in racial and ethnic minority populations.
Methodology
Search Strategy
A literature search was conducted for articles published between January 2000 and August 2012. Databases searched included PubMed/Medline, Web of Science, and The Cochrane Library. Search terms used included: medication, adherence, medication adherence, compliance, persistence, race, ethnicity, ethnic groups, minority, African-American, Hispanic, Latino, Asian, Pacific Islander, and intervention. Abstracts were reviewed and, when necessary, articles were read in full to assess their relevance. References cited in included articles were reviewed for additional articles relevant to this review. For the purpose of this review the term “Latino” is used to describe individuals who were identified as Hispanic, Latino, Mexican, or Puerto Rican.
Inclusion and Exclusion Criteria
Articles were selected for inclusion if they evaluated the impact of at least one intervention on medication adherence. An article was excluded if it was not written in English, was not conducted in the United States, did not test an intervention to improve adherence, did not report adherence outcomes, did not include patients with a chronic disease state, did not have ≥75% of the sample population was comprised of any one ethnic sub-group (eg, African-American, Hispanic, or Asian), failed to report the ethnic make-up of the sample population, or failed to address racial or ethnic disparities (ie, failed to address the needs of ethnic minorities or failed to compare results across races). Articles that did not have ≥75% of the sample population comprised of any one ethnic sub-group were included only if the authors performed sub-group analyses by race. One study was excluded because it was an interim report describing study for which the full report was given later.8,9
Results
Studies and Sample Characteristics
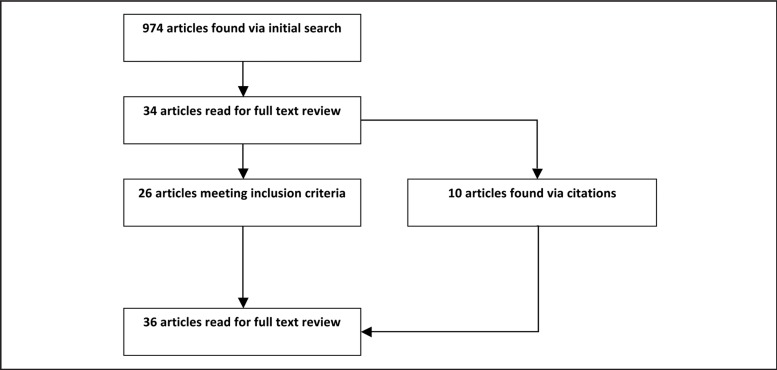
The initial search resulted in 974 articles of which 940 were discarded after reviewing titles and abstract. An additional 8 articles were discarded after reviewing the articles in their entirety, resulting in 26 articles. In the process of reviewing articles identified through the initial searches, 10 additional articles were identified through cited references, bringing the total to 36 articles for this review.
Of the 36 studies identified, 20 studies showed significant post-intervention differences, 10–15,17,19,22–23,26–28,30–32,35,37–38,41 of which 18 interventions10–11,13–15,17,19,22–23,26–28,30,32,35,37–38,41 resulted in a significant increase in medication adherence and two interventions12,31 prevented a decline in medication adherence (Table 1). Twenty-four studies were randomized controlled trials,11–12,14–18,20–26,29–33,35,39–40,42–43 eight used a quasi-experimental design,19,27,34,36–38,44 three used a pre-experimental design,10,13,28 and one was an observational cohort study.41 Sample population sizes ranged from N = 10 to N = 520, with a median of N = 126.5.
Table 1.
Research on Interventions to Improve Medication Adherence in African-Americans and Latinos.
| Authors (year, N) | Type of study | Condition | Population (main ethnicity) | Intervention | Results | Adherence measurement |
| Ailinger, et al, (2010, N=217) | Pre-experimental | Tuber-culosis | Latino immigrants at 9 clinical sites | Cultural intervention delivered by 2 Spanish-speaking nurses | Based on self-report, mean number of medications taken at 9 months was significantly higher in intervention vs. the control group (157 vs 129 doses). | Self-report |
| Andrade, et al, (2005, N=58) | RCT | HIV | African-Americans receiving care at HIV Clinic | Disease Management Assistance System reminder device plus monthly adherence counseling. | Based on electronic drug exposure monitoring caps, mean adherence rates at 24 weeks were significantly higher in the intervention group vs the control group (80% vs 65%). | Electronic caps and self-report |
| Barbamoto, et al, (2009, N=189) | RCT | Diabetes | Recently diagnosed Hispanic/Latino patients | Community health worker (CHW) cultural educational intervention & case management by culturally competent nurses | Based on self-report, medication-taking behavior remained unchanged in the CHW group but worsened in the case management and standard provider care groups after 10 weeks. | Self-report |
| Bartlett, et al, (2002, N=10) | Pre-experimental | Asthma | Inner-city African-American children | Nurse intervention with families via home visits weekly. | Based on electronic monitors, the number of children appropriately using medication was significantly improved after five weeks as compared to baseline (54% vs 29%). | Electronic monitors |
| Bogner, et al, (2010, N=58) | RCT | Diabetes, depression | Elderly African-American patients | Integrated care and education for depression and diabetes. | Based on Medication Event Monitoring System (MEMS), adherence was significantly greater in intervention vs control group at 6 weeks for oral hypoglycemic agents (62% vs 24%) and antidepressants (62% vs 10%). | Medication Event Monitoring System(MEMS) |
| Chaisson, et al, (2001, N=300) | RCT | Tuber-culosis | African-Americans history of drug abuse | Directly observed therapy & peer counseling and education | Supervised patients were more likely than peers (80 vs 51) and controls (80 vs 77) to take 100% of doses after six months. | Dose supervision,self-report, electronic caps |
| Dilorio, et al, (2003, N=17) | RCT, pilot study | HIV | African-American patients | Motivational interviews with nurse counselor | Based on the Antiretroviral General Adherence Scale, mean adherence was not significantly greater in intervention vs. controls (27 vs 23) at 8 weeks | Self-report |
| Dilorio, et al, (2008, N=213) | RCT | HIV | African-American patients at HIV clinic | Motivational interviews with nurse counselor | Based on MEMs, intervention patients had significantly greater adherence than controls (65% vs 55%) at 12 months. | MEMS |
| Feaster, et al, (2010, N=156) | RCT (mixed design) | HIV | African-American women | Structural Ecosystems Therapy (SET) to promote healthy family relationships & Person-Centered Approach (PCA) improving therapist and client relationships | Individuals in the PCA (67%) had significantly lower levels of medication adherence than CC (75%) or SET (89%) at 18 months as measured by self-report | Self-report |
| Fernandez, et al, (2008, N=65) | Quasi-experimental (pre-post controlled intervention) | Hypertension | Elderly African-American and Latino patients | Six group behavioral counseling sessions, with two monthly maintenance sessions | At 14 weeks there were significant increases in adherence in intervention (52% vs 24%) but not controls (58% vs 59%), based on self-report. | Self-report |
| Golin, et al, (2006, N=155) | RCT | HIV | African-Americans at infectious diseases clinic | Motivational interviews and booster letters | Change in adherence level at 12 weeks was not significantly better in intervention vs. control group (+4.5% vs −3.8%). | Pill counts, self-report, and electronic caps |
| Holstad, et al, (2011, N=207) | RCT | HIV | African-American women | Motivational interviewing in groups | Adherence significantly decreased in both groups at 9 months in both % of doses taken and doses taken on schedule measured by MEMS. | MEMS |
| Hovell, et al, (2003, N=286) | RCT | Tuber-culosis | Adolescent Latino patients | Adherence coaching: five 30-minute in person sessions and seven 15-minute phone calls. Self-esteem counseling. | Adherence was measured at 9 months by self-report and urine assays. Coaching resulted in significant increases in adherence compared with attention and usual care groups (180 vs 155 vs 151). | Self-report, urine assays |
| Ingersoll, et al, (2011, N=54) | RCT, pilot | HIV | African-American patients with a history of crack cocaine use | Six sessions of motivational interviewing plus feedback and skills building & Video information | At second follow-up, adherence improved in both intervention and control groups, but there were no significant between-group differences. | Self-report |
| Joseph, et al, (2007, N=314) | RCT | Asthma | African-Americans from six Detroit public high schools | Four web-based educational computer sessions | Changes in adherence were not significant. | Self-report |
| Kopelowicz, et al, (2003, N=92) | RCT | Schizophrenia | Outpatient Latinos and relatives | Training in medication management, 90-minute sessions 4 times/week during 3 months | Adherence as measured by pill counts, family reports, and monthly interviews was not significantly better for intervention vs. control group at 6 months (85% vs 78%). | Pill counts, patient reports, familyreports, monthly interviews |
| Kopelowicz et al. (2012, N=196) | RCT (3-armed) | Schizophrenia | Outpatient Latinos and relatives | Multifamily group-standard (MFG-S), 3 initial sessions, a 1-day educational workshop,andgroupsessionsMultifamily group-adherence (MFG-A), 3 initial sessions, a 1-day educational workshop | At 24 months, adherence in the MFG-A group was significantly better than the control group but not the MFG-S group (MFG-S: 23%, MFG-A: 33%, Control: 11%) as measured by self-report, interviewing relatives, physician interview, and pharmacy data. | Self-report, interviewing relatives, physician interview, pharmacy data |
| Lai, et al, (2007, N=53) | Quasi-experimental (time series) | Hypertension | Latino patients | Consultation on lifestyle and therapy delivered by Hispanic pharmacists and health team interventions | At 9 months, % of patients refilling their medications on time was significantly increased (96% vs 71%) measured by medication refills. | Medication refills |
| Ma, et al, (2008, N=31) | Pre-experimental | HIV | African-American substance users in the South | Modified directly observed therapy (MDOT), 3 month intensive phase and 3 month transition phase | At 6 months the proportion of patients who self-reported at least 80% adherence was significantly increased (67% vs 0%). | Self-report |
| Migneault, et al, (2012, N=337) | RCT | Hypertension | Urban primary care African-American patients | Thirty-two weekly automated, computer-based, interactive, culturally adapted telephone calls | At 12 months, no significant difference in Medication Adherence Score between intervention and control groups as measured by self-report (0.45 vs 0.26). | Self-report |
| Nyamathi, et al, (2011, N=520) | RCT | Tuberculosis | Homeless African-American and Latino patients | Eight educational/skills training modules for 6 months in small groups | Among African-Americans, intervention group had better adherence than controls measured by DOT (OR = 2.6). | Direct observation |
| Ogedegbe, et al, (2008, N=190) | RCT | Hypertension | African-Americans from 2 community-based primary care practices in New York City | 30-minute motivational interviews at 3, 6, 9, and 12 months | At 12 months there was a non-significant 1.1% within-group increase in adherence rates for the intervention group from baseline vs a significant −12.9% decrease in the control group, as measured by MEMS. | MEMS |
| Ogedegbe, et al, (2012, N=256) | RCT | Hypertension | African-American patients in 2 primary care practices | Positive-affect induction and self-affirmation, culturally tailored workbook, bimonthly phone calls | At 12 months, mean adherence as measured by electronic pill monitor (Medic e-Cap) was significantly higher in intervention vs control group (42% vs 36%). | Electronic pill monitor (Medic-eCap) |
| Otsuki, et al, (2009, N=250) | RCT, 3 arm parallel group | Asthma | Inner-city African-American children | Home-based asthma education combined with medication adherence feedback & asthma education alone | After 18 months, no significant differences were found between groups in medication refills or self-reported adherence | Caregiver report, medication refill records |
| Powell-Cope, et al, (2003, N=24) | Quasi-experimental (uncontrolled, pre-post evaluation) | HIV | African-American substance abusing women | Random assignment to 3 types of reminder devices and monthly nurse visits | After 2 months, number of patients missing doses in past two weeks was not significantly improved over baseline based on self-report (30% vs 33%). | Self-reports |
| Remien, et al, (2005, N=215) | RCT | HIV | Heterosexual and homosexual African-American and Latino couples | Four 45–60 minute sessions by nurse practitioner over 5 weeks, with a $20 reimbursement per session | After 8 weeks, intervention group showed higher adherence vs. control (76% vs. 60%) as measured by MEMS caps, effect diminished at 3 and 6 month follow-up. | Self-report |
| Resnick, et al, (2009, N=22) | Quasi-experimental (pre-post intervention, single group) | HTN, hyperlipidemia | Elderly African-American patients | 60 minute motivational, educational, and exercise sessions held 3 times weekly for 12 weeks | After 4 months, medication self-efficacy sum scores were not significantly different from baseline, based on self-report (20.9 vs 23.8). | Self-report |
| Riekert, et al, (2011, N=37) | Quasi-experimental (uncontrolled pilot study, pre-post evaluation) | Asthma | Adolescent African-Americans at an inner-city emergency department | Five sessions at participants' homes at 1, 2, 3, 4 and 8 weeks, motivational interviews and education, monetary compensation | After 8 weeks, caregiver report of adherence was significantly higher as compared to baseline (62% vs 46%), while adolescent report was not (27% vs 32%). | Self-report (caregivers and patients) |
| Robbins, et al, (2004, N=109) | Quasi-experimental (pre-post intervention) | Osteoporosis | African-American, White, and Hispanic women participating in a clinical osteoporosis trial | Educational intervention. White women used pillboxes, minority women used pillboxes for 6 months followed by electronic monitoring bottles for 6 months | After 12 months, Black and Hispanic women showed significant improvements in adherence rates over baseline (88.4 vs 79.2; 85.8 vs 83) while White women did not (96 vs 95.4) as measured by pill counts and MEMS for minority women. | Pill counts, MEMSfor minority groups |
| Rosenzweig, et al, (2011, N=24) | RCT | Breast cancer | African-American women | 45-minute one-on-one Attitudes, Communication, Treatment, and Support (ACTS) intervention | Overall adherence to therapy was not significantly different in intervention vs control groups (92% vs 73%). | NA |
| Rothschild, et al, (2012, N=144) | RCT | Diabetes | Mexican-Americans | Culturally tailored community diabetes self-management training by community health workers | After 24 months, adherence was not significantly better in intervention vs control group based on self-report or MEMS caps. | Self-report, MEMS |
| Tesoriero, et al, (2003, N=435) | Observational cohort (prospective cohort) | HIV | Black, White, and Latinos | Adherence support programs | At follow-up, a significantly smaller % of patients were non-adherent patients compared to baseline according to self-report (27% vs 35%). | Self-report |
| van Servellen, et al, (2005, N=85) | Quasi-experimental, repeated measures | HIV | Spanish-speaking Latinos at two clinics in Los Angeles | 5-week instructional support modular program with a 6-month follow-up nurse case management | After 6 months the increase in % of patients who were >95% adherent over the last four days was not significantly different in intervention vs control group or in 90% adherence over last four days. | Self-report |
| Vivian, et al, (2002, N=56) | RCT | Hypertension | African-American, Caucasian, and Other patients at Veterans Affairs Medical Center in Philadelphia | Six monthly appointments with clinical pharmacist case management | After 6 months, % of patients forgetting to take their medications at least once a week & % of patients getting medications refilled within two weeks of the scheduled date were not significantly different in intervention vs control groups as measured by self-report and pharmacy refills | Self-report, refill records |
| Walker, et al, (2000, N=83) | RCT | Hypertension | Elderly African-American patients | Spiritual and hypertension-related messages via programmed telephone calls, printed material on hypertension, home visits from a health educator | After 6 weeks, mean adherence was not significantly improved over baseline in the intervention group or in the control group based on home visits to conduct pill counts. | Pill counts |
| Wells, et al, (2011, N=85) | Quasi-experimental (3-group descriptive research study) | End Stage Renal Disease | African-American patients | Group 1: One-time, 30-minute, one-on one educational intervention, handout of content taught Group 2: No educational intervention, handout of educational content | After 1 month, there were no significant differences in adherence as measured by Medical Outcomes Study (MOS). General Measures of Patient Adherence. | Medical OutcomesStudy (MOS)General Measures of Patient Adherence |
The majority of the studies included in this review focused on African-American and Latino populations, although five studies performed sub-group analyses on their results to control for ethnicity.20,30,35,38,41 Twenty-five studies used sample populations which were comprised of ≥75% African-Americans11,13–19,21,23–24,28–34,36–37,39–40,42–44 Of those 25 studies, 13 found significant post-intervention improvements in medication adherence.11,13–17,19,23,28,30–32,37 Eight studies used sample populations which were comprised of ≥75% Latino individuals.8,10,12,22,25–27,40 Five of those studies found significant post-intervention improvements in medication adherence.10,12,22,26–27 Five studies performed sub-group analyses by race to determine the effect of interventions on medication adherence.20,30,35,38,41
Twenty studies included in this review had sample populations comprised entirely of individuals from a single ethnic minority background, while the rest recruited individuals of mixed ethnic backgrounds.8,10,12–14,18,22,25–29,31–32,36–37,39–40,43–44 Of those 20 studies, 12 were conducted with African-Americans13–14,18,28–29,31–32,36–37,39,43–44 and eight with Latinos.8,10,12,22,25,27,40 We originally set out to investigate interventions to improve adherence in minority populations including African-Americans, Latinos, Native Americans, Asians, and Pacific Islanders (including Native Hawaiians); however no studies meeting our criteria with sample populations representing Native Americans, Asians, or Pacific Islanders were found.
Patients' chronic conditions included HIV/AIDS (n = 13), hypertension (n = 8), asthma (n =v4), tuberculosis (n = 3), diabetes (n = 3), schizophrenia (n = 2), dyslipidemia (n = 1), osteoporosis (n = 1), breast cancer (n = 1), and end-stage renal disease (ESRD; n = 1).
Interventions and Methods
Types of interventions used included education, counseling, motivational interviews (MI), cognitive-behavioral counseling, medication therapy management (MTM), peer counseling single and group sessions, peer support and counseling, home visits, handouts, telephone calls, and reminder devices (Table 1). The interventions were administered by community health workers (CHWs), pharmacists, trained nurses, and peer counselors in a variety of settings. The studies in this review often used multiple methods to deliver the interventions. Some researchers used multiple interventions in their studies.
Methods of adherence measurement used in the studies in this review included electronic pill caps, direct observation, self-report, and pharmacy reports (Table 1). The majority of studies used the patients' self-reports as a method of assessing adherence. Twenty-four studies8,10–12,15–16,18–20,22–26,28–29,33–34,36–37,40–41,42,44 used self-report either (from patient or caregiver) alone or in combination with other assessment methods while 12 studies11,13–15,17,20–21,31–32,35,38,40 used electronic monitoring devices to measure adherence, either alone or in combination with other assessment methods. Four studies used both self-report and electronic monitoring to assess adherence. One study neglected to report their method(s) of assessing adherence.39
Duration
Two studies used one-time educational interventions lasting 30 minutes.39,44 One study did not report the period of time over which their intervention was delivered.18 In the other 33 studies, the period of time over which the interventions were delivered ranged from one month to 24 months, with a median duration of 6 months. Of the studies with a period of intervention delivery under 6 months (including the two studies using one-time educational interventions), 39% demonstrated benefit in adherence due to the intervention, while 71% of the studies delivering interventions over at least 6 months demonstrated benefit in adherence (although the studies by Nyamathi, et al, (2008) and Robbins et al (2004) only showed improvements with African-American patients and not Hispanic patients).
Effectiveness of Interventions
Due to the wide variation in methodology and design, the studies included in this review often had little in common with one another; however some of the studies overlapped in their methods, and some general themes and similarities emerged regarding the effectiveness of certain interventions. Motivational interviewing appeared to be an effective intervention for some African-American populations. Seven studies used motivational interviewing techniques with African-American populations,16–17,20–21,23,31,37 including five studies performed using patients who had HIV, one with hypertensive patients,31 and one with patients who had asthma.37 Two of the studies conducted with HIV positive patients found motivational interviewing improved adherence, as did the studies done with hypertensive patients and patients with asthma.31,37
Reminder devices were explored as interventions by two studies.11,34 The devices were programmable, portable electronic devices that emitted sounds or vibrations at specific times. Both studies were conducted with African-American patients diagnosed with HIV. While Andrade, et al (2005), found success with a portable device which played pre-recorded voice reminders; Powell-Cope, et al (2003), found no improvements in adherence after they provided patients with reminder devices. It should be noted that the adherence outcomes are reported differently between the two studies; Andrade, et al (2005), report mean adherence scores while Powell-Cope, et al (2003), report the proportion of women missing at least one dose in the past two weeks.
The two studies which focused on using (CHWs) to provide interventions for Latino patients with diabetes had conflicting results. Barbamoto, et al (2009), found that an educational intervention delivered to patients and their families by CHWs prevented a significant decline in adherence after six months. Rothschild, et al (2012), sent CHWs to patients' homes for two years to conduct educational sessions. Contrasting the improvement in adherence found by Barbamoto, et al (2009), Rothschild, et al (2012), did not find any benefit in adherence. Directly observed therapy (DOT) was employed as an intervention by two studies. Ma, et al (2008), used a modified directly observed therapy (MDOT) to monitor HIV seropositive African-American patients in a tapered schedule which decreased the number of observed medication administrations from five days per week to a once-weekly observation. After six months, patients had improved adherence. Chaisson, et al (2001), compared two interventions (DOT and peer counseling) against routine care. The DOT intervention group was significantly more likely to take 100% of their doses as compared to the peer counseling and routine care groups, and significantly more likely to take 90% of their doses as compared to the peer counseling group after six months.
Two studies focused on using pharmacists to deliver education and case management to patients with hypertension. Lai, et al (2007), found that the Latino population in their study improved in the ability to refill medications on time post-intervention. In contrast, Vivian, et al (2002), did not demonstrate differences between control and intervention groups in forgetting to take doses at least once a week or in refilling medications within two weeks of the scheduled date with an African-American population.
Three studies implemented interventions which involved little to no human interaction. Two studies relied on automated phone calls to deliver messages to hypertensive African-American patients,9,43 and neither reported any significant post-intervention improvements in medication adherence after employing telemedicine as an intervention. A web-based program designed by Joseph, et al (2007), to educate African-American teenagers with asthma was likewise ineffective.
Discussion
The studies included in this review varied widely in many aspects, including the types of interventions used, the ethnicities and conditions of the sample populations, the methods used to measure adherence, and types of analyses performed with their results. Although the types of interventions varied, the majority of studies targeted patient knowledge and sought to educate and counsel patients in order to improve their medication adherence. Education and counseling that is provided only once or very briefly may be insufficient to influence a patient's values and behaviors.45 Evidence has shown that despite being recognized as an important component of interventions, education has only a minor and nondurable impact on adherence when used alone.5,47 As demonstrated by two of the studies included in this review, one-time educational sessions did not stimulate improvement in medication-taking behavior.
There appears to be no clear consensus on a “gold standard” for the measurement of medication adherence47,49 despite the assertions of recent studies stating that electronic pill monitors provide such a benchmark.32,48 Objective methods of assessing adherence are an important component of adherence studies, as self-reporting is known to overestimate patient adherence.37 In the absence of a universally accepted gold standard, it is recommended that multiple methods of measuring medication adherence be used to provide the best results.47 Most of the studies in this review used either self-report or electronic monitors alone or in combination with other methods to assess adherence, such as dose supervision, refill data from pharmacies, and pill counts. However, most studies used only a single method of adherence assessment.
The fact that the studies included in our review varied in their definitions of adherence as an outcome is a further hindrance in the comparison of interventions. The authors presented their results in such measurement terms as adherence rates, percent completion, the number of doses missed, percent of doses taken on schedule, and percent of patients who were non-adherent. An example may be found in the presentation of adherence results by Andrade, et al (2005), and Powell-Cope, et al (2003), in testing reminder devices. Where Andrade, et al (2005), reported the mean adherence scores of patients, Powell-Cope, et al (2003), chose to report adherence outcomes in terms of the proportion of women missing at least one dose in the past two weeks. While both studies investigated reminder devices as an intervention, they lack a similar method of assessing and reporting adherence outcomes, thus making it difficult to compare and contrast the two studies.
Most of the studies included in this review ended their patient assessments when the intervention period ended, thus long-term impacts of most of the interventions used are not available in the existing literature. For patients with chronic diseases, the likelihood of adherence diminishes as the duration of treatment increases.50 Migneault, et al (2012), noted previous literature as well as their study demonstrated post-intervention benefits in medication adherence tend to decay toward baseline. Thus, studies should pursue follow-up data beyond the duration of the intervention in order to assess the durability of the intervention.4 No studies meeting our criteria with sample populations representing Native Americans, Asians, or Pacific Islanders were found. Thus these minority populations stand to benefit from future domestic research conducted with samples comprised of individuals from these groups. However, this study only considered published literature written in English and conducted in the United States. Potentially there may have been studies focusing on these groups that did not meet our inclusion criteria.
Conclusion
Interventions directed at patients from racial and ethnic minority backgrounds should take into consideration the patients' cultural beliefs and values. Many patients come from cultural backgrounds whose perspectives on medicine differ from the Western bio-medical model. The impact of a patient's health beliefs, values, communication style, native language, lifestyle, social structure and support, and socioeconomic status must be taken into consideration when applying an intervention to improve adherence.46–47 An intervention that works for individuals of one ethnicity may not be as effective for individuals of a different background. Culturally sensitive interventions can more effectively address patient beliefs regarding their conditions, therapy, and values while appropriately encouraging better compliance. Further studies which address the cultural needs of minority populations may lead to improvements in the health care of minority groups and contribute significantly to closing the health care gap.
In this literature review, the studies varied significantly in their methods and design as well as the populations studied. While some types of interventions (eg, motivational interviewing, reminder devices, one-time educational session) have been effective, no one intervention was proven to be universally successful. A consensus on a “gold standard” for measuring medication adherence would further contribute to facilitating the comparison of different interventions. For patients taking multiple medications, there exists a need for such research in the development of interventions to improve adherence.
Figure 1.
Process Used To Identify Included Articles
Conflict of Interest
None of the authors identify a conflict of interest.
Disclosure Statement
Dr. Juarez's time was supported in part by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number P20MD000173. This project was supported in part by an appointment to the ORISE Research Participation Program at the FDA Office of Minority Health and Center for Drug Evaluation and Research (CDER) administered by the Oak Ridge Institute for Science and Education through an agreement between the US Department of Energy and CDER. None of the authors reported any conflicts of interest.
References
- 1.Centers for Disease Control, author. Health, United States 2012: With Special Feature on Emergency Care. [July 28, 2013]. Available at: http://www.cdc.gov/nchs/data/hus/hus12.pdf.
- 2.World Health Organization, author. Adherence to long-term therapies: Evidence for action, 2003. [September 25, 2012]. Available at: http://www.who.int/topics/patient_adherence/en/
- 3.Schedlbauer A, Davies P, Fahey T. Interventions to improve adherence to lipid lowering medication. Cochrane Database of Systematic Reviews. 2010;(3) doi: 10.1002/14651858.CD004371.pub3. Art. No.: CD004371. [DOI] [PubMed] [Google Scholar]
- 4.Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database of Systematic Reviews. 2008;(2) doi: 10.1002/14651858.CD000011.pub3. Art. No.: CD000011. [DOI] [PubMed] [Google Scholar]
- 5.Lee JK, Grace KA, Taylor AJ. Effect of a Pharmacy Care Program on Medication Adherence and Persistence, Blood Pressure, and Low-Density Lipoprotein Cholesterol: A Randomized Controlled Trial. JAMA. 2006;296:2563–2571. doi: 10.1001/jama.296.21.joc60162. [DOI] [PubMed] [Google Scholar]
- 6.Advisory Committee on Minority Health (ACMH), author A Federal Health Equity Commission Will Promote the Public's Health and Ensure Health Equity in Health Care Reform: A Statement of Principles and Recommendations. [March 2010]. Available at: http://minorityhealth.hhs.gov/Assets/pdf/Checked/1/ACMH_Report_March2010.pdf.
- 7.Russell CN. Culturally responsive interventions to enhance immunosuppressive medication adherence in older African American kidney transplant recipients. Prog Transplant. 2006;16(3):187–196. doi: 10.1177/152692480601600302. [DOI] [PubMed] [Google Scholar]
- 8.Ailinger RL, Martyn D, Lasus H, Garcia NL. The Effect of a Cultural Intervention on Adherence to Latent Tuberculosis Infection Therapy in Latino Immigrants. Public Health Nurs. 2010;27(2):115–120. doi: 10.1111/j.1525-1446.2010.00834.x. [DOI] [PubMed] [Google Scholar]
- 9.van Servelle G, Nyamathi A, Carpio F, et al. Effects of a Treatment Adherence Enhancement Program on Health Literacy, Patient-Provider Relationships, and Adherence to HAART among Low-Income HIV-Positive Spanish-Speaking Latinos. AIDS Patient Care STDs. 2005;19(11):745–759. doi: 10.1089/apc.2005.19.745. [DOI] [PubMed] [Google Scholar]
- 10.van Sevellen GV, Carpio F, Lopez M, et al. Program to Enhance Health Literacy and Treatment Adherence in Low-Income HIV-Infected Latino Men and Women. AIDS Patient Care STDs. 2003;17(11):581–594. doi: 10.1089/108729103322555971. [DOI] [PubMed] [Google Scholar]
- 11.Andrade ASA, McGruder HF, Wu AW, et al. A Programmable Prompting Device Improves Adherence to Highly Active Antiretroviral Therapyin HIV-Infected Subjects with Memory Impairment. Clin Infect Dis. 2005;41:875–882. doi: 10.1086/432877. [DOI] [PubMed] [Google Scholar]
- 12.Barbamoto KS, Sey KA, Camilleri AJ, et al. Improving diabetes care and health measures among Hispanics using community health workers: results from a randomized controlled trial. Health Educ Behav. 2009;36:113–126. doi: 10.1177/1090198108325911. [DOI] [PubMed] [Google Scholar]
- 13.Bartlett SJ, Lukk P, Butz A, Lampros-Klein F, Rand CS. Enhancing Medication Adherence Among Inner-City Children with Asthma: Results from Pilot Studies. J Asthma. 2002;39(1):47–54. doi: 10.1081/jas-120000806. [DOI] [PubMed] [Google Scholar]
- 14.Bogner HR, de Vries HF. Integrating Type 2 Diabetes Mellitus and Depression Treatment among African-Americans: A Randomized Controlled Pilot Trial. Diabetes Educ. 2010;36(2):284–292. doi: 10.1177/0145721709356115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chaisson RE, Barnes GL, Hackman J, et al. A Randomized, Controlled Trial of Interventions to Improve Adherence to Isoniazid Therapy to Prevent Tuberculosis in Injection Drug Users. Am J Med. 2001;110:611–615. doi: 10.1016/s0002-9343(01)00695-7. [DOI] [PubMed] [Google Scholar]
- 16.DiIorio C, Resnicow K, McDonnell M, et al. Using motivational interviewing to promote adherence to antiretroviral medications: a pilot study. J Assoc Nurses AIDS Care. 2003;14:52–62. doi: 10.1177/1055329002250996. [DOI] [PubMed] [Google Scholar]
- 17.DiIorio C, McCarty F, Resnicow K, et al. Using motivational interviewing to promote adherence to antiretroviral medications: A randomized controlled study. AIDS Care. 2008;20(3):273–283. doi: 10.1080/09540120701593489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feaster DJ, Brincks AM, Mitrani VB, Prado G, Schwartz SJ, Szapocznik J. The Efficacy of Structural Ecosystems Therapy for HIV Medication Adherence with African American Women. J Fam Psychol. 2010;24(1):51–59. doi: 10.1037/a0017954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fernandez S, Scales KL, Pineiro JM, Schoenthaler AM, Ogedegbe G. A senior center-based pilot trial of the effect of lifestyle intervention on blood pressure in minority elderly people with hypertension. J Am Geriatr Soc. 2008;56:1860–1866. doi: 10.1111/j.1532-5415.2008.01863.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Golin CE, EArp J, Tien H-C, Stewart P, Porter C, Howie L. A 2-Arm, Randomized, Controlled Trial of a Motivational Interviewing-Based Intervention to Improve Adherence to Antiretroviral Therapy (ART) Among Patients Failing or Initiating ART. J Acquir Immune Defic Syndr. 2006;42:42, 51. doi: 10.1097/01.qai.0000219771.97303.0a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holstad MM, Kelly ME, Resnicow K, Sharma S. Group Motivational Interviewing to Promote Adherence to Antiretroviral Medications and Risk Reduction Behaviors in HIV Infected Women. AIDS Behav. 2011 Jul;15(5):885–896. doi: 10.1007/s10461-010-9865-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hovell MF, Sipan CL, Blumberg EJ, et al. Increasing Latino Adolescents' Adherence to Treatment for Latent Tuberculosis Infection: A Controlled Trial. Am J Public Health. 2003;93(11):1871–1877. doi: 10.2105/ajph.93.11.1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ingersoll KS, Farrell-Carnahan L, Cohen-Filipic J, et al. A Pilot Randomized Clinical Trial of Two Medication Adherence and Drug Use Interventions For HIV+ Crack Cocaine Users. Drug Alcohol Depend. 2011 Jul 1;116(1–3):177–187. doi: 10.1016/j.drugalcdep.2010.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Joseph CLM, Peterson E, Havstad S, et al. A Web-based, Tailored Asthma Management Program for Urban African-American High School Students. Am J Respir Crit Care Med. 2007;175:888–895. doi: 10.1164/rccm.200608-1244OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kopelowicz A, Zarate R, Gonzalez Smit V, Mintz J, Liberman RP. Disease Management in Latinos With Schizophrenia: A Family-Assisted, Skills Training Approach. Schizophr Bull. 2003;29(2):211–227. doi: 10.1093/oxfordjournals.schbul.a006999. [DOI] [PubMed] [Google Scholar]
- 26.Kopelowicz A, Zarate R, Wallace CJ, Liberman RP, Lopez SR, Mintz J. The Ability of Multifamily Groups to Improve Treatment Adherence in Mexican Americans With Schizophrenia. Arch Gen Psychiatry. 2012;69(3):265–273. doi: 10.1001/archgenpsychiatry.2011.135. [DOI] [PubMed] [Google Scholar]
- 27.Lai LL. Community pharmacy-based hypertension disease-management program in a Latino/Hispanic-American population. Consult Pharm. 2007;22:411–416. doi: 10.4140/tcp.n.2007.411. [DOI] [PubMed] [Google Scholar]
- 28.Ma M, Brown BR, Coleman M, Kibler JL, Loewenthal H, Mitty JA. The Feasibility of Modified Directly Observed Therapy for HIV-Seropositive African American Substance Users. AIDS Patient Care STDs. 2008;22(2):139–146. doi: 10.1089/apc.2007.0063. [DOI] [PubMed] [Google Scholar]
- 29.Migneault JP, Dedier JJ, Wright JA, et al. A Culturally Adapted Telecommunication System to Improve Physical Activity, Diet Quality, and Medication Adherence Among Hypertensive African-Americans: A Randomized Controlled Trial. Ann Behav Med. 2012;43:62–73. doi: 10.1007/s12160-011-9319-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nyamathi A, Nahid P, Berg J, et al. Efficacy of Nurse Case-Managed Intervention for Latent Tuberculosis Among Homeless Subsamples. Nurs Res. 2008;57(1):33–39. doi: 10.1097/01.NNR.0000280660.26879.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ogedegbe G, Chaplin W, Schoenthaler A, et al. A Practice-Based Trial of Motivational Interviewing and Adherence in Hypertensive African Americans. Am J Hypertension. 2008;21:1137–1143. doi: 10.1038/ajh.2008.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ogedegbe GO, Boutin-Foster C, Wells MT, et al. A Randomized Controlled Trial of Positive-Affect Intervention and Medication Adherence in Hypertensive African Americans. Arch Intern Med. 2012;172(4):322–326. doi: 10.1001/archinternmed.2011.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Otsuki M, Eakin MN, Rand CS, et al. Adherence Feedback to Improve Asthma Outcomes Among Inner-City Children: A Randomized Trial. Pediatrics. 2009;124:1513–1521. doi: 10.1542/peds.2008-2961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Powell-Cope GM, White J, Henkelman EJ, Turner BJ. Qualitative and Quantitative assessments of HAART adherence of substance-abusing women. AIDS Care. 2003;15(2):239–249. doi: 10.1080/0954012031000068380. [DOI] [PubMed] [Google Scholar]
- 35.Remien RH, Stirrat MJ, Dolezal C, et al. Couple-focused support to improve HIV medication adherence: a randomized controlled trial. AIDS. 2005;19:807–814. doi: 10.1097/01.aids.0000168975.44219.45. [DOI] [PubMed] [Google Scholar]
- 36.Resnick B, Shaughnessy M, Galik E, et al. Pilot testing of the PRAISEDD intervention among African American and low-income older adults. J Cardiovasc Nurs. 2009;24:352–361. doi: 10.1097/JCN.0b013e3181ac0301. [DOI] [PubMed] [Google Scholar]
- 37.Riekert KA, Borrelli B, Bilderback A, Rand CS. The development of a motivational interviewing intervention to promote medication adherence among inner-city, African-American adolescents with asthma. Patient Educ Couns. 2011;82:117–122. doi: 10.1016/j.pec.2010.03.005]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Robbins B, Rausch KJ, Garcia RI, Prestwood KM. Multicultural medication adherence: a comparative study. J Gerontol Nurs. 2004;30:25–32. doi: 10.3928/0098-9134-20040701-07. [DOI] [PubMed] [Google Scholar]
- 39.Rosenzweig M, Brufsky A, Rastogi P, Puhalla S, Simon J, Underwood S. The Attitudes, Communication, Treatment,and Support Intervention to Reduce Breast Cancer Treatment Disparity. Oncol Nurs Forum. 2011;38(1):85–89. doi: 10.1188/11.ONF.85-89. [DOI] [PubMed] [Google Scholar]
- 40.Rothschild SK, Martin MA, Swider SM, et al. The Mexican-American Trial of Community Health workers (MATCH): Design and baseline characteristics of a randomized controlled trial testing a culturally tailored community diabetes self-management intervention. Contemp Clin Trials. 2012;33:369–377. doi: 10.1016/j.cct.2011.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tesoriero J, French T, Weiss L, Waters M, Finkelstein R, Agins B. Stability of Adherence to Highly Active Antiretroviral Therapy Over Time Among Clients Enrolled in the Treatment Adherence Demonstration Project. J Acquir Immune Defic Syndr. 2003;33:484–493. doi: 10.1097/00126334-200308010-00009. [DOI] [PubMed] [Google Scholar]
- 42.Vivian EM. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy. 2002;22:1533–1540. doi: 10.1592/phco.22.17.1533.34127. [DOI] [PubMed] [Google Scholar]
- 43.Walker CC. An educational intervention for hypertension management in older African Americans. Ethnicity Dis. 2000;10:165–174. [PubMed] [Google Scholar]
- 44.Wells JR. Hemodialysis Knowledge and Medical Adherence in African Americans Diagnosed with End Stage Renal Disease: Results of an Educational Intervention. Nephrol Nurs J. 2011;38(2):155–163. doi: 10.1111/j.1365-2702.2006.01930.x. [DOI] [PubMed] [Google Scholar]
- 45.National Council on Patient Information and Education, author. Enhancing Prescription Medicine Adherence: A National Action Plan. 2007. [September 25, 2012]. Available at: http://www.talkaboutrx.org/documents/enhancing_prescription_medicine_adherence.pdf.
- 46.Peterson AM, Takiya L, Finley R. Meta-analysis of trials of interventions to improve medication adherence. Am J Health-Syst Pharm. 2003;60:657–665. doi: 10.1093/ajhp/60.7.657. [DOI] [PubMed] [Google Scholar]
- 47.Manias E, Williams A. Medication adherence in people of culturally and linguistically diverse backgrounds: a meta-analysis. Ann Pharmacother. 2010;44:964–982. doi: 10.1345/aph.1M572. [DOI] [PubMed] [Google Scholar]
- 48.Knafl GJ, Schoenthaler A, Ogedegbe G. Secondary analysis of electronically monitored medication adherence data for a cohort of hypertensive African-Americans. Patient Prefer Adherence. 2012;6:207–219. doi: 10.2147/PPA.S30582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Safren SA, Otto MW, Worth JL, et al. Two strategies to increase adherence to HIV antiretroviral medication: Life-Steps and medication monitoring. Behav Res Ther. 200;39:1151–1162. doi: 10.1016/s0005-7967(00)00091-7. [DOI] [PubMed] [Google Scholar]
- 50.Takiya LN, Peterson AM, Finley RS. Meta-analysis of interventions for medication adherence to antihypertensives. Ann Pharmacother. 2004;38:1617–1624. doi: 10.1345/aph.1D268. [DOI] [PubMed] [Google Scholar]